Diseases of the vulva
Dr. ishraq mohammedAnatomy:
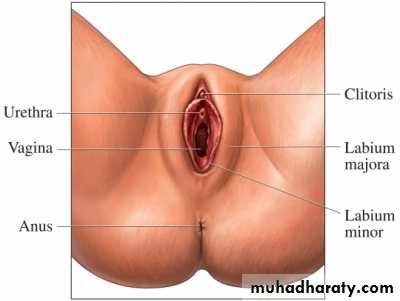
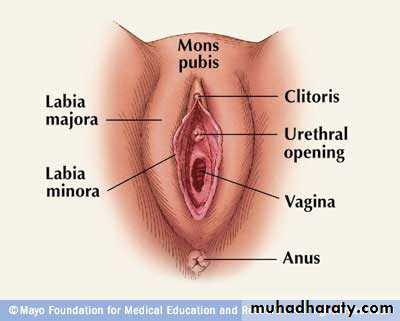
is the external genital organs of the female The vulva has many major and minor anatomical structures, including the labia majora, mons pubis, labia minora, clitoris, bulb of vestibule, vulval vestibule, greater and lesser vestibular glands, and the opening of the vagina. Its development occurs during several phases, chiefly during the fetal and pubertal periods of time.In human beings, major structures of the vulva are:[3]
the mons pubisthe labia, consisting of the labia majora and the labia minora
the external portion of the clitoris (Latin: Clitoral glans) and the clitoral hood
the vulval vestibule
the pudendal cleft
the frenulum labiorum pudendi or the fourchette
the opening (or urinary meatus) of the urethra
the opening (or introitus) of the vagina
the hymen and
Other structures:
the perineum
the sebaceous glands on labia majora
the vaginal glands:
Bartholin's glands
Paraurethral glands called Skene's glands
Assessment of vulval disease:
History: the duration of complaint, detail of onset & any precipitating factors, general skin problems , current method of skin care, which topical treatment are being used & the impact of the symptoms on sexual function.Examination: for evidence of systemic diseases or generalized skin condition. Pelvic & vaginal examination should be performed unless is too uncomfortable.
Investigations: it is important to take a biopsies whenever there is any doubt about the diagnosis.
Symptoms of benign vulval conditions:
Pruritus vulvae :Causes of pruritus vulvae can include the following.Infections. For example: thrush, threadworms, scabies, and some sexually transmitted infections.
Skin conditions may affect vulval skin. For example: eczema, psoriasis, lichen simplex, lichen planus and lichen sclerosus.
Sensitisation of the vulval skin to soaps, perfumes, deodorants, excessive sweat, condoms, wet wipes, textile dyes, detergents, fabric conditioners, sanitary wear, etc.
Urinary or faecal incontinence. This can make the skin of the vulva moist and irritated.
Menopause. Because of lower oestrogen levels, the vulval skin tends to become thinner and drier after the menopause, which can make it prone to itch.
Pregnancy can cause itch due to vulval engorgement. There is also an increased risk of vaginal discharge and thrush during pregnancy, which may cause itch.
Breast-feeding can cause itch due to low oestrogen levels.
Any cause of a generalised body itch may also cause itching of the vulva. For example, a generalised body itch may be a side-effect of some medicines or due to some blood disorders, thyroid problems or kidney or liver disease.
Diabetes can cause itch in the vulval area.
A cancer of the vulval skin is an uncommon cause.
Unknown cause. In some cases, no cause can be found.
Liver disease. uraemia.& low ferritin level.
What are the treatments for pruritus vulvae?
Treating the cause
Most of the time, when a cause can be found, the cause can be treated and pruritus vulvae improves. However, depending on the underlying cause, sometimes prolonged or repeated treatment may be needed. The treatment varies, depending on the cause. For example, identifying and stopping the use of anything that may be sensitising the vulval skin, antifungal cream for thrush, antibiotics for certain infections, steroid cream for various skin conditions, hormone cream or hormone replacement therapy (HRT) if the itch is related to the menopause. Your doctor will advise.
Moisturisers
Bland moisturisers (emollients) such as aqueous cream or emulsifying ointment can help to ease the itch, whatever the cause.
Sometimes soaps, perfumes, bubble baths, deodorants, scented creams, the dye in toilet tissue, etc, can sensitise (irritate) the delicate vulval skin. Don't use any of these on your vulva or in your bath water or shower non-coloured toilet tissue. An antihistamine medicine at bedtime may help if sleep is affected. Antihistamines do not have a great effect on the itch, but some cause drowsiness.
In addition, your doctor may advise that you use a mild steroid ointment such as hydrocortisone for a week or so. This often settles the itch within a few days. It may also help to break any itch-scratch cycle that has developed. However, you should not use steroid ointment regularly on the vulva as it can have a thinning effect on the skin with long-term use.
Vulval pain or burning: the cause is frequently elusive & treatment is empirical. Steroid cream or ointment will help some of these women, but a multidisciplinary approach is required for many . Surgery is rarely helpful.
Classification of vulval diorders:
Non-neoplastic disorders:Lichen sclerosus
Squamous cell hyperplasia
Other dermatoses
Vulval intraepithelial neoplasia:
Squamous VIN:VIN 1 mild dysplasia, VIN2 moderate dysplasia, VIN3 sever dysplasia or carcinoma in situ.
Non-squamous VIN:
Paget,s disease.
Lichen sclerosus:
Is the commonest condition found in elderly women complaining of vulvar itch. The cause is not known, but the condition is associated with autoimmune disorders. Although it most commonly affect the vulva & peri-anal skin. Lesions appear elsewhere. The lesion is white & the skin looks thin, with a crinkled surface. the contours of the vulva slowly disappear & labial adhesions form. The diagnosis usually made clinically but a biopsy should be performed whenever there is uncertainty. About 4per cent of women with LS develop invasive cancer. 9per cent of women show prevalence of auto-immune disease.
Treatment:
If the patients are asymptomatic, no treatment is required. Mild itching may be helped by 1per cent hydrocortisone ointment applied three times daily. More potent steroid may be required for short periods. some women benefit from 2per cent testosterone ointment, which should be applied twice or three times per day for 6weeks; thereafter the frequency can be reduced to once or twice a week. No place for vulvectomy due to high morbidity & high recurrence rate.Squamous cell hyperplasia:
Term applied to histological evidence of hyperplasia without any clinical evidence of the cause. Chronic rubbing of otherwise of otherwise normal skin(lichen simplex), psoriasis, condylomata acuminata & infection with candida albicans are among the diagnosis that must be excluded. this stipulation is likely to reduced to near zero the number of cases assigned to this category on clinical grounds.Other dermatoses:
The most common general disease causing itching of the vulva are diabetes, uraemia & liver failure.In allergic dermatitis, the skin usually red & swollen& may later become thickened. Secondary infection may occur.
Psoriasis, lichen planus & scabies may affect the vulva. In lichen planus, the lesion on the vulva is characteristically a purple-white papule with a shiny surface & regular outline.
Vaginal infection is the most common cause of vulval itching, particularly in younger women. Candidiasis & trichomoniasis are the most common cause . Human papilloma virus is not thought to cause pruritis vulvae.
Vulval ulcers:
Aphthous ulcersHerpes genitalis
Primary syphilis
Crohn,s disease
Behcet”s disease
LGV
Chancroid
Donovanosis
tuberculosis
Benign tumours:
Cystic tumours: bartholin”s cyst & abscess.Vaginal cyst
Solid tumour: the commonest are condylomata acuminata due to infection with HPV, usually type 6 &11,
Squamous papillomata, skin tag, lipoma, fibroma & very rarely endometriosis.
Premalignant conditions:
The histological features & terminology of VIN are analogous to those of CIN & VAIN.Natural history of VIN: 40percent of women with VIN are younger than 41years. Although histologically very similar to CIN & often occur in association with it, VIN has been said not to have the same malignant potential.
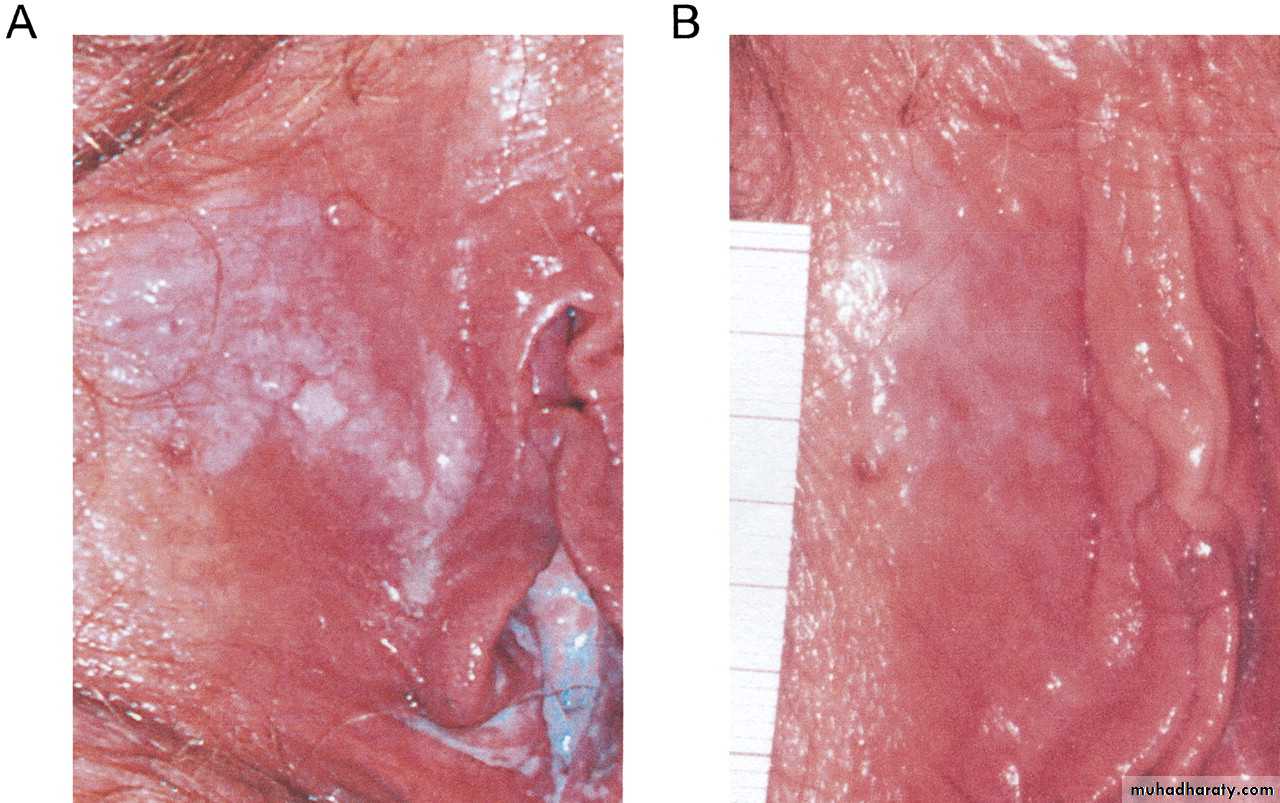
Diagnosis & assessment of VIN: often presented as pruritus , but 20-45 per cent are asymptomatic. The lesions are often raised above the surrounding skin & have a rough surface. The color is variable: white ,red dark brown. They are often multifocal. however, the full extent of the abnormalities is often not apparent until 5per cent acetic acid is applied (colposcopy) VIN turned white & mosaic or punctation may be visible. Adequate biopsy must be taken from abnormal area to rule out invasive disease.
Risks factor:
. Risk factors are similar to those for vulvar cancer of the warty or basaloid type, and include human papillomavirus (HPV) infection, cigarette smoking, and immunodeficiency or immunosuppression . Human papillomavirus — Almost 90 percent of all VIN lesions test positive for HPV [8]. HPV has been associated with both VIN and vulvar cancer of the warty and basaloid subtypes. Multifocal VIN and multicentric VIN are most often associated with high oncogenic risk HPV subtypes 16, 18, and 31 [9-12], and should be considered premalignant lesions.Treatment of VIN:
The goals of treatment are to prevent development of invasive vulvar cancer and relieve symptoms, while preserving normal vulvar anatomy and function. Treatment of VIN must be individualized based upon biopsy results, location and extent of disease, and the woman's symptoms. Management options include:
Wide local excision,Skinning vulvectomy, Laser ablation, Topical treatment
Excisional treatment has a diagnostic advantage over ablative or medical management modalities in women with VIN since an occult invasive squamous cell carcinoma is present in many of these women; the risk is particularly high in women over age 50 [4,9]. Removing the entire lesion for histopathological examination facilitates diagnosis of these cases.Medical — Conservative therapies aimed at preserving the vulvar anatomy have been attempted, particularly in younger patients. Careful colposcopic examination with biopsies to exclude invasive disease is mandatory prior to beginning treatment with any of these drugs. Imiquimod , Topical 5-fluorouracil , strong steroids applied twice or thrice daily for not more than 6 months because of the thinning of the skin that may result .
Assessment of the results of treatment should include a consideration of the length of follow up. Surgical excision is associated with crude recurrence rate of 15-43per cent. Close observation & re-biopsy are essential to detect invasive disease among those who relapse. Repeated treatment are commonly required.
In view of the mutilating nature of treatment, the high recurrence rate & the uncertainty about risk of invasion, there is a place for careful observation, especially of young women without sever symptoms. However, some of these untreated patients will develop cervical cancer, so the importance of close follow up must be emphasized to the patient & her general practitionar.
Paget”s disease:
This uncommon condition similar to that found in the breast. Pruritus is the presenting compliant. It is often presented as red, crusted plaque with sharp edges. The diagnosis must be made by a biopsy. In one third of cases there is adenocarcinoma in the apocrine glands , & concomitant genital malignancies are found in 15-25per cent. These are most commonly vulval or cervical ,but ovarian bladder endometrial , vaginal& urethral cancer have all been reported. The treatment is very wide local excision, usually including total vulvectomy . The specimen must be examined histologically, with great care to exclude an apocrine adenocarcinoma.Invasive disease of the vulva:
Uncommon but potentially curable disease.About 95per cent of cases are squamous , & melanoma is the commonest of the remainder. Little is known of the etiology of the vulval cancer.
Natural history: after local invasion into the underlying & surrounding tissue & into the vagina & the anus , vulval cancer spread, predominantly via the lymphatic system( inguinal, femoral in the groin then to the external iliac L.N). Drainage to both groins occur from midline structures- the perineum & the clitoris- but some contralateral spread may take place from other parts of the vulva. Only tumours with less than 1mm of invasion carry a sufficiently low risk of lymphatic spread to be considered microinvasive.
Staging: the FIGO staging of vulval cancer:
Ia confined to the vulva/ or perineum, 2cm or less maximal diameter. Groin nodes not palpable. Stromal invasion no greater than 1mm.Ib as for Ia but stromal invasion more than 1mm.
II confined to the vulva /or perineum, mpre than 2cm maximum diameter, groin nodes not palpable.
III extend beyond the vulva, vagina, lower urethra or anus, or unilateral regional lymph node metastasis.
IVa involve the mucosa of rectum or bladder; upper urethra; or pelvic bone; &/or bilateral regional L.N metastasis.
IVb any distant metastasis including pelvic L.N.
Diagnosis & assessment:
71per cent with invasive disease complain of irritation or pruritus, & 57per cent note a vulval mass or ulcer. 23per cent are complain of bleeding & irritation. Because of the multicentric nature of female lower genital tract cancer, inspection of the cervix& cervical cytology. The groin nodes must be palpable carefully & any suspicious nodes sampled by FNA. The CXR is always required, IVP, MRI of the pelvis may sometimes be helpful. Thorough examination under anesthesia & a full-thickness, generous biopsy are the most important investigations.
Treatment: surgery
Early stage vulval cancer:Primary lesion: the primary lesion should be excised with a 1cm disease-free margin, including the deep margin. In most early cancers, this can be achieved by a wide radical local excision & will allow for the preservation of non-involved structures. If the primary lesion is associated with a vulval maturation disorders , this will be removed as well.
Regional lymph node: depth of invasion is the best predictor of risk of nodal metastasis in vulvar cancer . In stage Ia, as the risk of nodal involvement with depth of invasion less than 1mm is virtually zero. Thee tumors are treated by wide local excision alone.
Lateral vulval tumors: the management of regional lymph nodes can be modified for patients ( i.e. those with the medial border at least 2cm lateral to the line drawn between the clitoris & the anus) require only ipsilateral inguinal node dissection. If the ipsilateral nodes are negative, the contralateral nodes are rarely involved. However, should these nodes be positive, a contralateral node dissection should be undertaken.
Inguinal node dissection:
Surgical dissection of inguinal nodes is considered mandatory in early-stage vulval cancer when depth of invasion is greater than 1mm. A full dissection of inguino-femoral lymph node. The routine removal of pelvic L.N in early of VC is not recommended. Another approach to reduce morbidity is the identification & removal of sentinel node(i.e. the first node to drain the vulval tumor) being identified &, if histologically normal, the remainder of inguinal L.N dissection should be omitted. The most reliable technique is probably a hybrid of intralesional injection of radiolabelled technetium combined with intralesion injection of blue dye at the time of surgery & scanning of the nodal tissue for the radioactive signal.Advanced vulval cancer:
Surgery to the primary lesion:The size & location of the tumor will influence the surgical approach to the primary lesion. The surgical goal is to remove the tumor with at least a 1cm disease-free margin. In the majority of cases, a triple incision technique can be employed. However, if there is evidence of skin bridge between the primary tumor & the inguinal node at the time of surgery, a radical vulvectomy with en-bloc inguinal node dissection should be considered. If extensive areas of vulval tissue need to be removed, reconstructive surgery with the use of skin graft or myocutaneous flaps may be required to achieve healing.
Management of inguinal nodes: en-bloc dissection should be undertaken . In cases in which the nodes are fixed or ulcerated, biopsy of these 0r FNA should be considered, followed by radiotherapy to the inguinal & pelvic LN ( the standard radiotherapy dose to the inguinal nodes may be inadequate to bring about a complete regression).
Neoadjuvant therapy:
Radiotherapy may be given pre-operatively to the primary lesions to allow for tumor shrinkage. This is particularly useful if the primary surgery would necessitate removal of the urethral or anal sphincters. A total maximum dose of 55Gy may be given with concurrent 5-fluorouracil. Subsequent tumor shrinkage may then enable the preservation of sphincters.Vulval cancer can be treated by primary radical radiotherapy if surgery is declined or not possible.
Adjuvant radiotherapy is recommended when surgical margins is inadequate (less than8mm) if re-excision might compromise function.
Radiotherapy to the groin & pelvic node sites is recommended if more than one node is involved or there is evidence of any extracapsular spread.
Radiotherapy may be used prior to surgery to attempt to reduce the morbidity & functional loss associated with surgery in large lesions.
Radiotherapy with concurrent chemotherapy may improve outcome, but as yet there are no data in support of this approach.
Treatment related morbidity:
Wound infection & wound breakdown.Lymphedema of the legs .
Psychological morbidity .
Morbidity associated with recurrent disease:
Recurrent disease affecting the vulva itself treated by further surgical excision &/ radiotherapy. Recurrence involving the inguinal lymph node or pelvic LN should be treated by radiotherapy. Most patients with groin recurrence die of disease.
Follow up of treated patients:
3 monthly for the first 2 years following treatment then 6 monthly for the following 3 years.
Thank you