Principles of Surgical Oncology
Dr. Khdair Al-RawaqLec Highlight
DefinitionsThe history of surgical oncology
The role of surgery in management of cancer, including :
• Prevention
• Screening
• Diagnosis
• Treatment
• Rehabilitation
• Palliative care
Future of Surgical Oncology
DefinitionsSurgical oncology, It is refered to the specific application of surgical principles to the oncologic setting. These principles have been derived by adapting standard surgical approaches to the unique situations that arise when treating cancer patients.
The surgeon is often the first specialist to see the patient with a solid malignancy, and, in the course of therapy, he or she may be called upon to provide diagnostic, therapeutic, palliative, and supportive care. In each of these areas, guiding paradigms that are unique to surgical oncology are employed.
Definitions
A surgical oncologist is a well-qualified surgeon who has obtained additional training and experience in the multidisciplinary approach to the prevention, diagnosis, treatment, and rehabilitation of cancer patients, and devotes a major portion of his or her professional practice to these activities and cancer research.”
Ancient History of Surgery for Cancer Treatment
1600 BC First recorded description of the surgical treatment of cancer (in Egypt)400 BC Hippocratesdescribes the stages of cancer and advises against surgery for terminal disease; he coins the terms “carcinoma”(crab-leg tumor) and “sarcoma”(fleshy tumor)
200 AD Galenidentifies cancer as a systemic disease (primary and metastasis)
Before 1850 Early heroic attempts to resect cancer
1850-1950 Development of standard surgical resection techniques1950-1960 Development of extended radical surgical procedures
Ancient History of Surgery for Cancer Treatment
Historical Eras of Surgery to Treat Cancer
1960-1980 Exploration of combined-modality treatment1980-2000 Multimodality therapy improves organ preservation and survival
2000-present Surgical practice incorporates improved understanding of the molecular basis of
Landmark Advances in Surgical Oncology
1775 Etiologic basis of cancer Percival Pott1809 Elective oophorectomy Ephraim McDowell
1829 Metastatic process Joseph Recamier
1846 Ether used as anesthesia John Collins Warren
1867 Carbolic acid used as antisepsis Joseph Lister
1873 Laryngectomy Albert Theodore Billroth
1878 Resection of rectal tumor Richard von Volkman
1880 Esophagectomy Albert Theodore Billroth
1881 Gastrectomy Albert Theodore Billroth
1890 Radical mastectomy William Stewart Halstead
1896 {Oophorectomy for breast cancer} G. T. Beatson
Landmark Advances in Surgical Oncology
1904 Radical prostatectomy
Hugh H. Young1906 Radical hysterectomy Ernest Wertheim
1908 Abdominoperineal resection
W. Ernest Miles
1909 Nobel prize for thyroid surgery
Theodore Emil Kocher
1910 Craniotomy
Harvey Cushing
Landmark Advances in Surgical Oncology
1912 Cordotomyfor the treatment of pain
E. Martin1913 Thoracic esophagectomy
Franz Torek
1927 Resection of pulmonary metastases
George Divis
1933 Pneumonectomy
Evarts Graham
1935 Pancreaticoduodenectomy
Allen O. Whipple
Landmark Advances in Surgical Oncology
1945 Adrenalectomy for prostate cancer
Charles B. Huggins
1957 Isolated limb perfusion
Oliver Creech
1958 First multicenter clinical trial
Bernard Fisher
1965 Hormone therapy for cancer
Charles Huggins
1971 Microvascular free-tissue transfer
Harry Buncke
Landmark Advances in Surgical Oncology
Surgery for Cancer Prevention
Role of Surgery in Cancer PreventionPre-cancerous lesions
Leukoplakia of the tongue
Thyroid gland in MENS II
Colon in FAP
•Organs at high risk of malignancy even where a pre-cancerous lesion has not been identified
Breast in cariers of deleterious BRCA mutations
Colon in HNPCC
Surgery for Cancer Screening
Role of Surgery in Cancer Screening
•Colonoscopy in colon cancer•Digital rectal examination in prostate cancer
•Clinical breast examination
Surgery for Diagnosis
Role of Surgery in DiagnosisHistory
Ascertain presence of risk factors
Evidence of metastases
Presence of co-morbid factors
Family and social history
Psychological assessment of patient
Ascertain patient’s social and economic resources
Ascertain patient’s expectation from therapy
Patient’s treatment preferences
Educate patient on diagnosis, treatment and follow-up, and correct mis-information
Investigations
•Knowledge of all available modalities of investigating particular case
•Microscopic diagnosis is compulsory
Role of Surgery in Diagnosis
BiopsySurgeon’s responsibilities:
•Selection of appropriate biopsy method and site
•Responsible that the tissue reach the pathologist timely and properly .
•Communicate the results to the patient, family, other physicians
•Provide initial prognosis and information on follow-up care
Types of Biopsy Methods
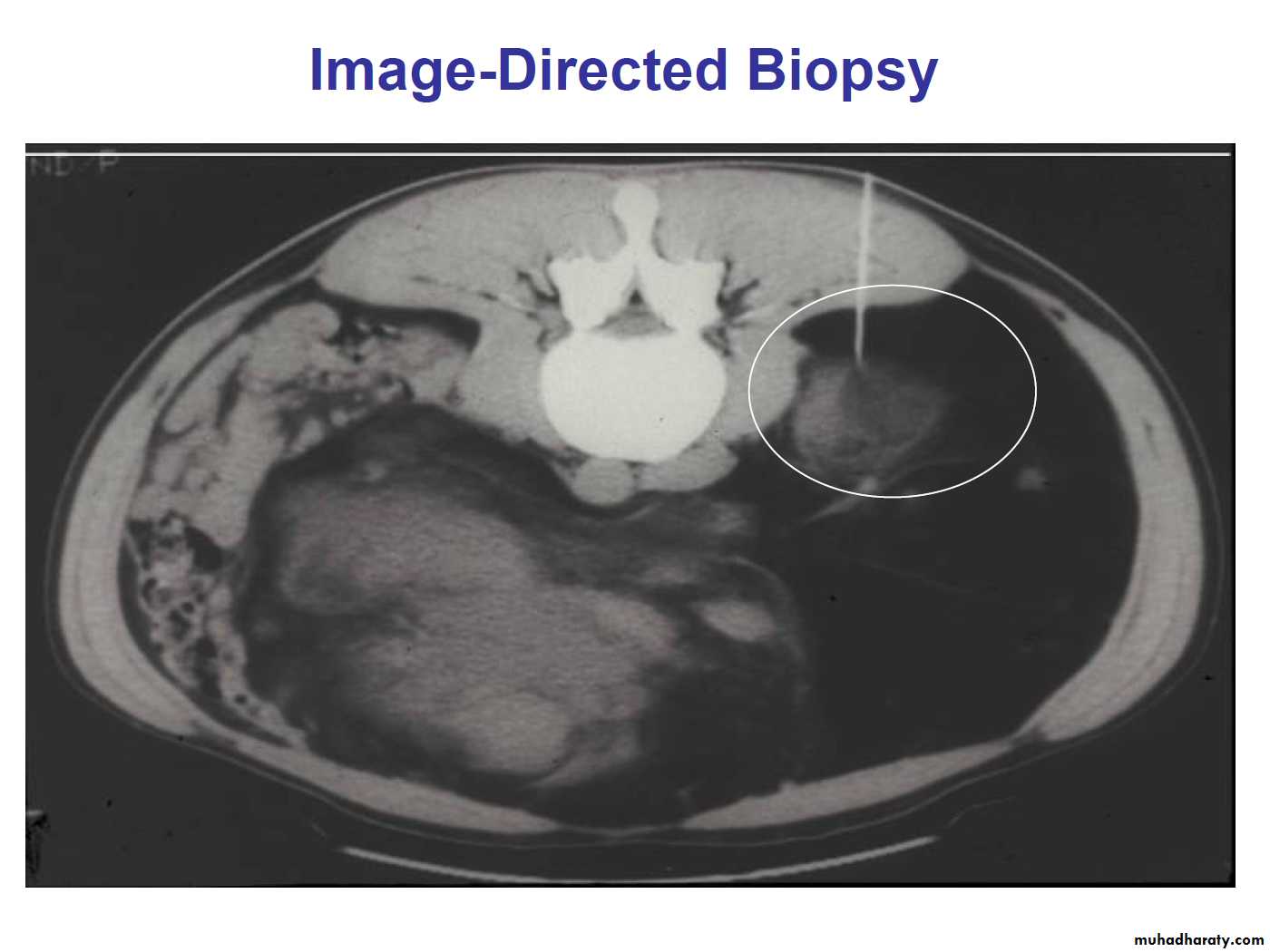
•Transcutaneous•Image-directed (with fine-needle aspiration or cutting needle)
–Ultrasonography
–Computerized tomography
–Magnetic resonance imaging
•Open incisional (A portion of the tumor)
•Open excisional (All tumor mass removed)
Types of tissue Biopsy
• Lymph node biopsylymphoma
metastatic carcinoma.
• Biopsy of a tissue-based mass
Lymphoma
The goal of biopsy in the patient with an abnormal lymph node and suspected lymphoma is to make the general diagnosis and to establish the lymphoma type and subtype. Additional analyses of the cells in the node, its internal architecture, and the subpopulations of cells are critical for subsequent treatment.Diagnosis of lymphoma should be made on a completely excised node that has been minimally manipulated
The use of needle aspiration does not consistently allow for the complete analyses. Eg. RS cell
can be performed as needed.
Carcinoma
The diagnosis of metastatic carcinoma often requires less tissue than is needed for lymphoma. Fine-needle aspiration (FNA), core biopsy, or subtotal removal of a single node will be adequate in this situation.For metastatic disease, the surgeon will use a combination of factors, such as location of the node, physical examination, and symptoms, to predict the site of primary disease. When this information is communicated to the pathologist, the pathologic evaluation can be focused on the most likely sites so as to obtain the highest diagnostic yield. The use of immunocytochemical analyses can be successful in defining the primary site, even on small amounts of tissue.
Sentinel node biopsy
TechniqueThe node or nodes that preferentially drain a particular primary tumor”basins” are identified by mapping and then surgically excised.
The mapping agents include radiolabeled materials and vital dyes that are specifically taken up by, and transported in, the lymphatic drainage systems. These mapping and localizing agents, used alone or in combination, are critical in defining the unique flow patterns to specific lymph node(s) and ambiguous drainage patterns (eg, a truncal melanoma that may drain to the axilla, supraclavicular, or inguinal spaces).
Biopsy of a tissue-based mass
Several principles must be considered
Mass in the aerodigestive tract In the aerodigestive tract, biopsy of a lesion should include a representative amount of tissue taken preferably from the periphery of the lesion, where the maximum amount of viable malignant cells will be present. Because the treatment of in situ and invasive diseases varies greatly, the biopsy must be of adequate depth to determine penetration of the tumors. This is particularly true for carcinomas of the oral cavity, pharynx, and larynx.
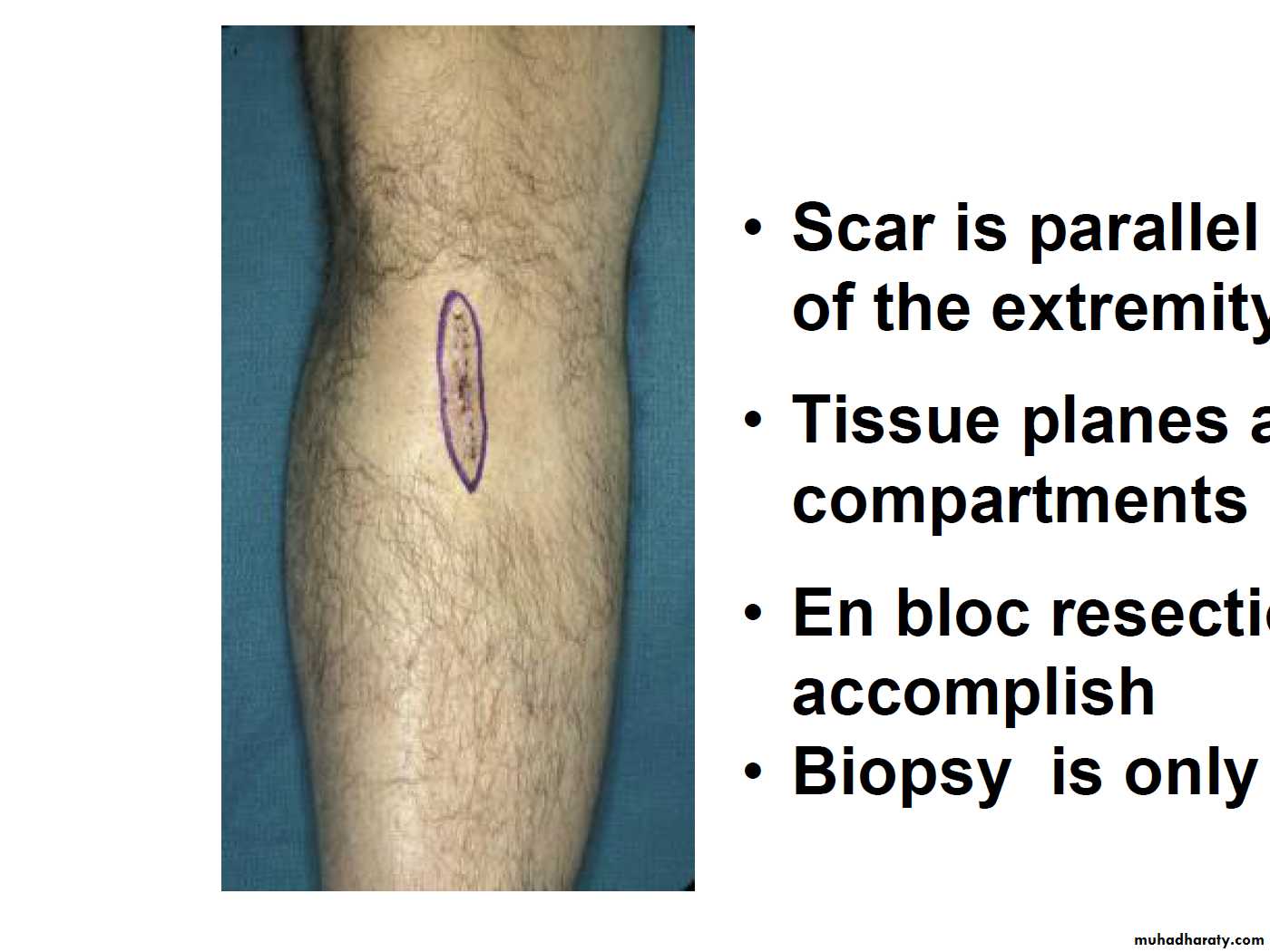
Mass in the trunk or extremities For soft-tissue or bony masses of the trunk or extremities, the biopsy technique should be selected on the basis of the planned subsequent tumor resection. The incision should be made along anatomic lines in the trunk or along the long axis of the extremity. When a sarcoma is suspected, FNA can establish the diagnosis of malignancy, but a core biopsy will likely be required to determine the histologic type and plan neoadjuvant therapy.
Breast mass
Although previously a common procedure, an open surgical biopsy of the breast is rarely indicated todayA core biopsy/FNA, performed either under image guidance (ultrasonography or mammography) or directly for palpable lesions, is the method of choice.
The core biopsy method establishes the histologic diagnosis, provides adequate tissue for analyses of hormone-receptor levels and other risk factors, causes little or no cosmetic damage, does not perturb sentinel node analyses, and does not require extended healing prior to the initiation of therapy. In addition, a small radioopaque clip can be placed in the tumor to guide the surgical extirpation.
Surgeon’s Tasks in Performing Biopsy
•Orient the specimen•Ensure the integrity of the tissue plane
•Ensure the adequacy of the tissue sample
•Be sure tissue reach the pathologist !
• Appropriate Open Biopsy
• •Scar is parallel to the long axis of the extremity• •Tissue planes and compartments are intact
• •En bloc resection will be easy to accomplish
• •Biopsy is only the first step
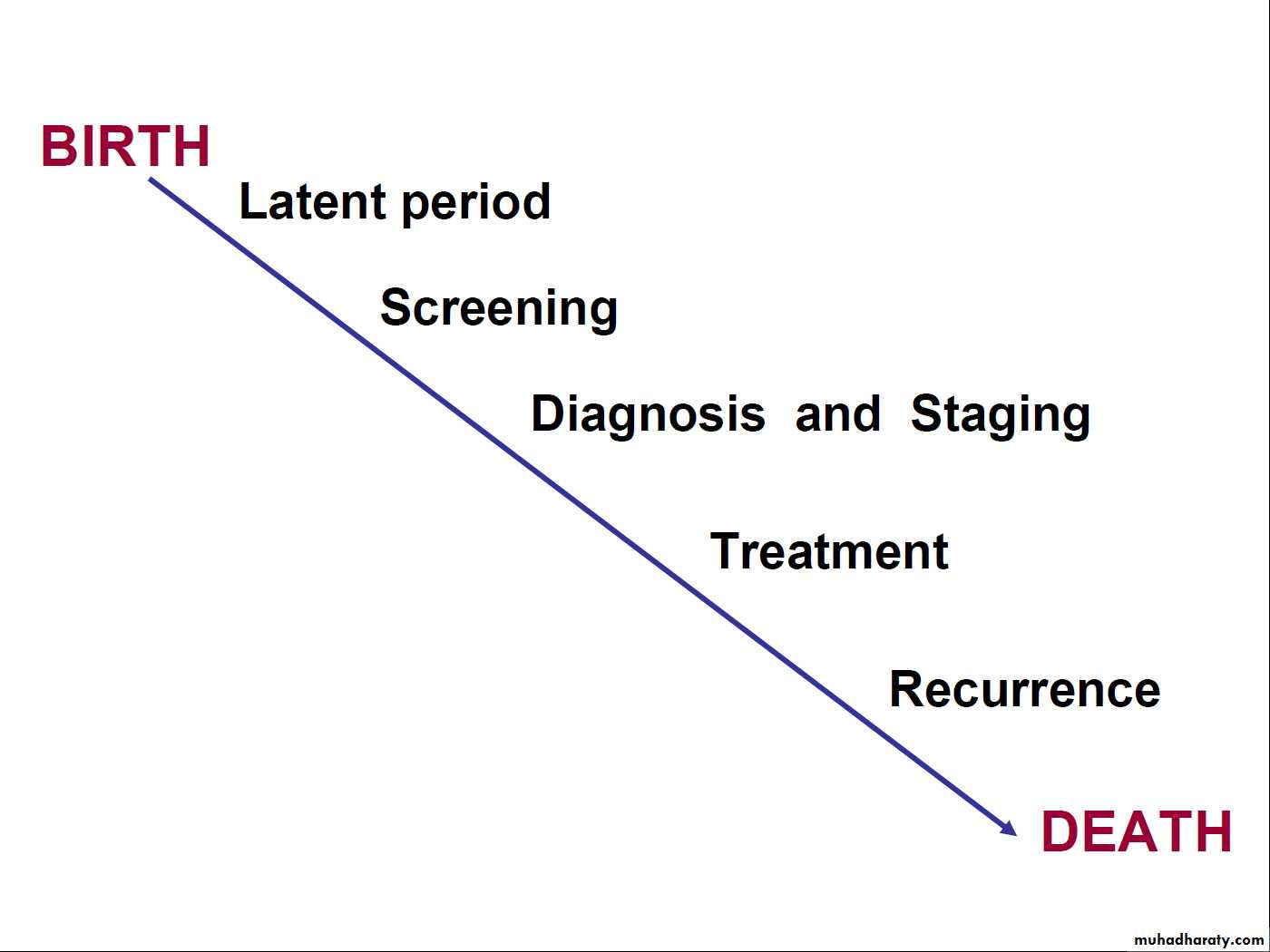
Surgery and Staging
•Classifies patients according to the degree of spread of cancer in order
•Guide selection of primary and adjuvant treatment
•Estimate prognosis
•Assist in evaluating result of treatment
•Facilitate exchange of information
•Contribute to continuing investigation of cancers
Types of staging
TNM most commonAJCC head & neck
FIGO Gyenicological Malig.
Duke GIT
Surgery forCancer Treatment
Role of Surgery in Cancer Care•Surgery
Zero-order kinetics—100% of cells at risk are killed with a single treatment
•Radiotherapy/Chemotherapy
First-order kinetics—only a portion of cells at risk are killed during treatment, which is followed by regrowth
Preoperative Assessment and Preparation
•Surgeon’s responsibility to assess the risk-to-benefit ratio and identify and correct underlying, relevanthealth problems .–Nutritional status
–Co-morbid medical conditions
–Hypertension
–Diabetes
–Congestive heart failure
–Liver or renal insufficiency
–Immunosuppresion
Types of surgery
•Local resection•Radical resection with en-bloc resection of lymph nodes
•Supra-radical resections
•Surgery for metastasis
•Surgical management of complications
•Vascular access surgery
Treatment
Principles of surgical resection of tumor
•Adequate margin of resection
•Prevention of tumor spillage
•Minimal manipulation
•Reconstruction
Metastasectomy
This is done when:•The primary tumor is controlled or can be controlled
•Metastasis is single or where multiple is localized
•Evidence that metastasectomy is associated clinical benefits
•Tumor doubling time is sufficiently long
•No significant co-morbid factor
Surgery
and RehabilitationRole of surgery in the rehabilitation of cancer patients
•Restoration of form•Restoration of function
•Care of ostomies
•Psychological treatment and support
•Maintenance and improvement of quality of life.
Surgery and Palliative care
Goals of Palliative Surgery
•Relieve symptoms for patients beyond cure when non-surgical measures are not feasible, not effective, or not expedient•Palliation means patient should be better at the completion of the procedure
“It is axiomatic that one cannot palliatively improve an asymptomatic patient using a scalpel.”
R. G. Martin, 1982
Palliative Improvement of Function and quality of life
•Adequate control of pain•Relief gastrointestinal and biliary obstruction
•Stop hemorrhage
•Supplement poor nutrition
•Airway obstruction
•Renal failure
•Rectal or urinary incontinence
Factors that influence outcome of treatment
• •Patient related factors• •Health care provider related factors
• •Environment related factors
Surgical Oncology in the Future
•Preemptive surgery in populations at genetic risk for the development of cancer
•Tissue and function
-preserving improvements
–Minimally invasive and robotic surgery
–Implantable monitors
–Treatment sensitizers
–Tissue-engineered, implantable “spare parts”
•Refinements in surgical practice will be driven by the underlying molecular basis of tumor biology