د.منى
\
radiology L4
Brain IMAGING TECHNIQUE
Imaging techniques
In most neurological disorders, plain films are either normal or the abnormalities are too non-specific
for the diagnosis to be made. Skull radiographs are rarely performed except as part of skeletal surveys
in suspected non-accidental injury or myeloma . Computed tomography (CT) and magnetic resonance
imaging (MRI) give vastly more information and one or the other investigation is indicated in
practically all patients with intracranial disease.
Computed tomography
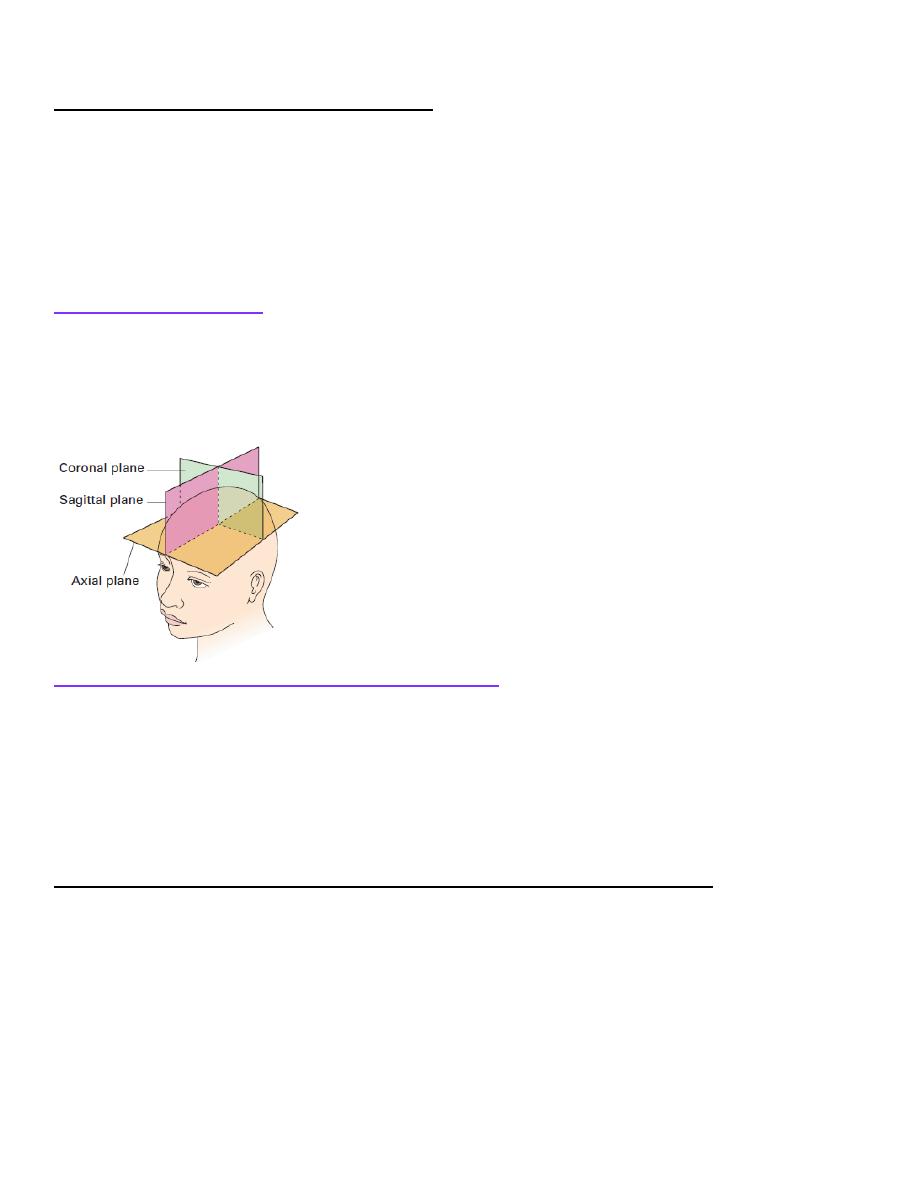
A routine CT examination of the brain involves making 20
–30 axial sections. The axial plane is also
the routine viewing projection but, if sufficiently thin, reconstructions can be made from the axial
sections, which then provide images in any other plane .However, to enable good differentiation of
grey and white matter, a slice thickness of 3
–5 mm is needed. The window settings are selected for
brain tissue or bone, depending on the structure being assessed
Contrast enhancement for computed tomography
The brain parenchyma does not normally enhance following an intravenous injection of contrast
medium due to the blood
–brain barrier (BBB) – the endothelial lining of cerebral vessels preventing
passage of solutes. Contrast enhancement of a brain lesion is therefore a consequence of breakdown of
the BBB such as with ischaemia, inflammation and neoplasms. Intracranial lesions (such as
meningiomas) supplied by the external carotid artery, which lacks a BBB, will often enhance avidly.
There is also no BBB in the pituitary, pineal and choroid plexuses, which will normally enhance.
Contrast is therefore only used routinely to evaluate vessels and extra-axial lesions or to increase the
conspicuity of brain lesions.
Intracranial enhancement on computed tomography and magnetic resonance imaging
Physiological
• Choroid
• Anterior pituitary gland
• Arteries
• Dural venous sinuses
Pathological
• Metastases
• Some primary gliomas
• Meningiomas
• Abscess
• Acute demyelination

د.منى
\
radiology L4
Computed tomography angiography
If thin slices are acquired following contrast administration
detailed reconstructions of the vessels can
be created in
multiple planes and with surface-shaded three-dimensional
images. CT angiography has
replaced conventional
angiography for the initial diagnosis of arterial
occlusions, aneurysms and
arteriovenous malformations
(AVMs). The venous phase of the angiogram can give information
on the
venous sinuses of the brain such as when
looking for thrombosis. Perfusion CT is a new technique
that
can quantify the passage of contrast through the brain
to evaluate the presence and extent of infarction
and ischaemia
in stroke patients who may be candidates for thrombolysis
treatment.
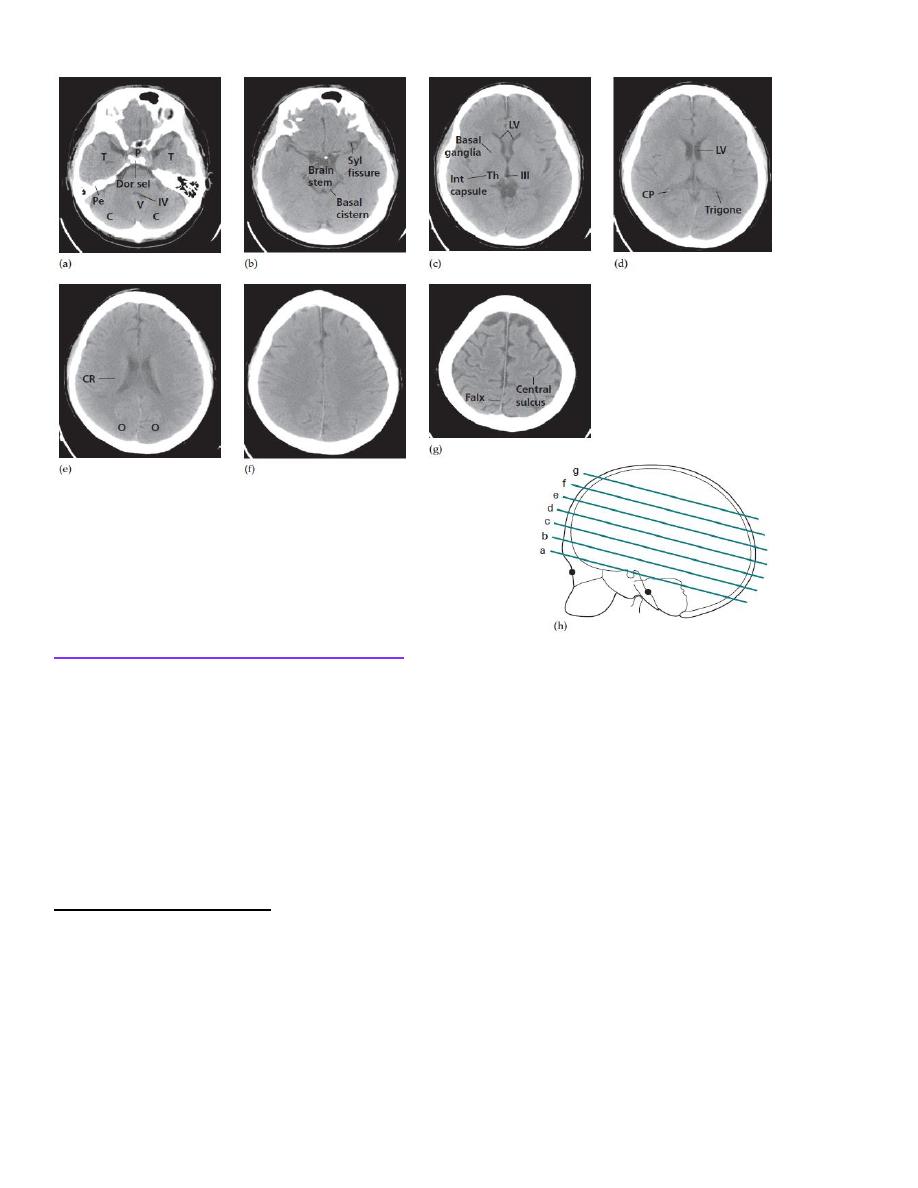
Normal head computed tomography
The
cerebrospinal fluid (CSF) is seen as water density within the ventricular system and subarachnoid
space surrounding
the brain. It is possible to distinguish the white and grey
matter of the brain due to
the higher fat content within myelinated white matter, which is therefore of lower attenuation.
The larger arteries at the base of the brain can usually be identified within the CSF-containing basal
cisterns.
Calcification is normally seen in the pineal gland and choroid plexus particularly in the lateral
ventricles.
Pathological calcification can be seen in abnormal vessels such as an AVM or aneurysm and some
types of brain tumour.
The supratentorial regions are usually well shown, but details of the posterior fossa may be obscured by
artefact from the surrounding bone.
د.منى
\
radiology L4
Abnormal head computed tomography
When an abnormality is seen, it is important to decide whether it has an intra-axial or extra-axial
location as the pathologies and therefore the differential diagnosis are very different. Intra-axial lesions
can involve the white and grey matter structures of the brain parenchyma, while extra-axial lesions may
involve the meninges, extracerebral spaces and skull vault. Specific diagnoses are suggested by
combining the clinical features with information about multiplicity, size, position and density of the
lesion.
The key signs of an abnormality on a CT scan are:
• abnormal tissue density
• mass effect
• enlargement of the ventricles.
Abnormal tissue density
Abnormal tissue may be of higher or lower density than the normal surrounding brain. High density is
seen withacute haemorrhage ,calcification and areas of contrast enhancement . Low density can be due
to cytotoxic oedema associated with infarcts, or to vasogenic oedema, which commonly surrounds
neoplasms, abcesses and other areas of inflammation.
Cytotoxic oedema will involve both the white and grey matter structures ,whereas vasogenic oedema is
limited to the white matter and characteristically shows finger-like projections into the subcortical
white matter in the gyri.
د.منى
\
radiology L4
Mass effect
The normally symmetrical lateral ventricles should be examined to see if they are displaced or
compressed. Shift of midline structures, such as the septum pellucidum, the third ventricle or the pineal
gland away from a lesion indicates a significant mass effect. Ventricular dilatation will occur if the
mass obstructs the flow of CSF. A mass effect may also show itself by effacing the basal cisterns, such
as when the suprasellar cistern is obscured by downward movement of the medial temporal lobes over
the tentorium cerebellum (uncal herniation )or the cerebellar tonsils through the foramen magnum.
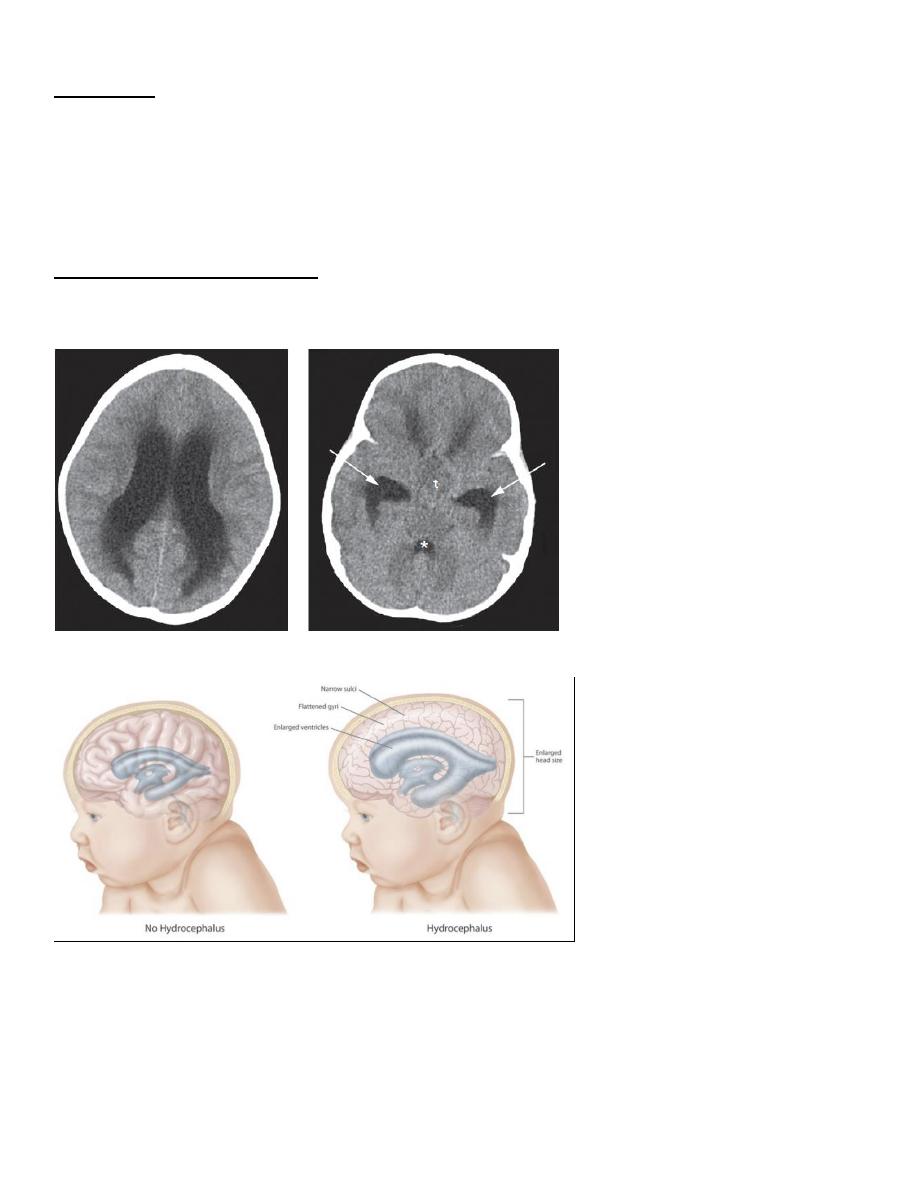
Enlargement of the ventricles
There are two basic mechanisms that cause the cerebral ventricles to enlarge:
• Obstruction to the CSF pathway, either within the ventricular system (obstructive hydrocephalus) or
over the surface of the brain
• Secondary to atrophy of the surrounding brain tissue
د.منى
\
radiology L4
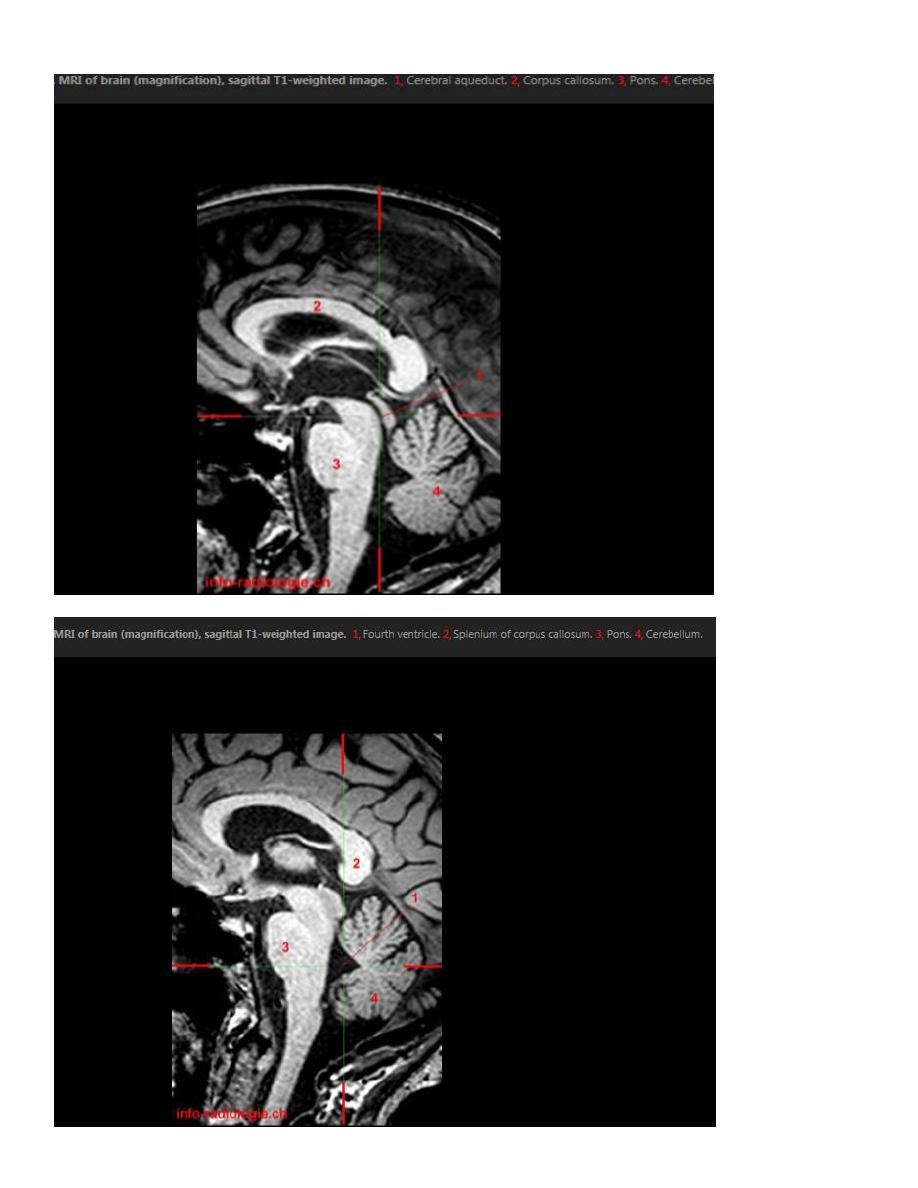
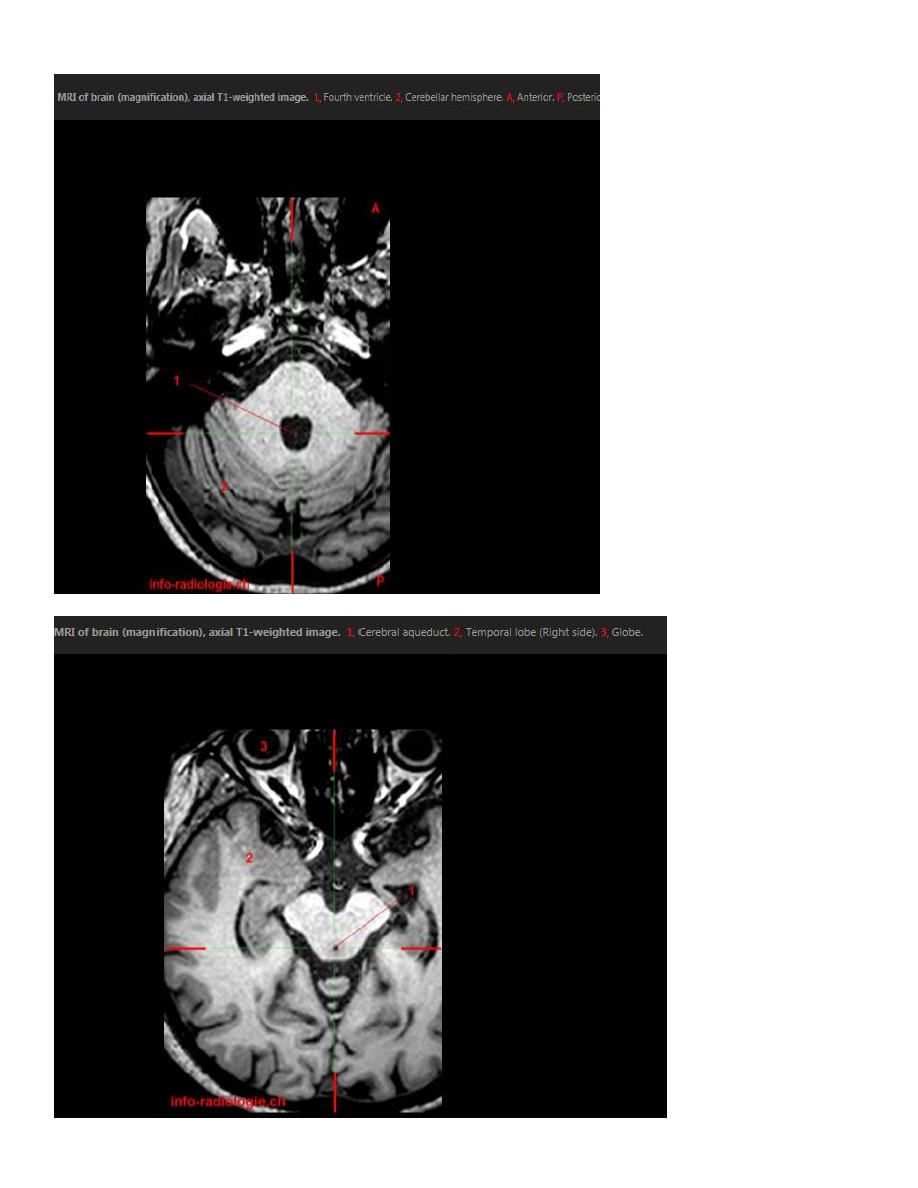
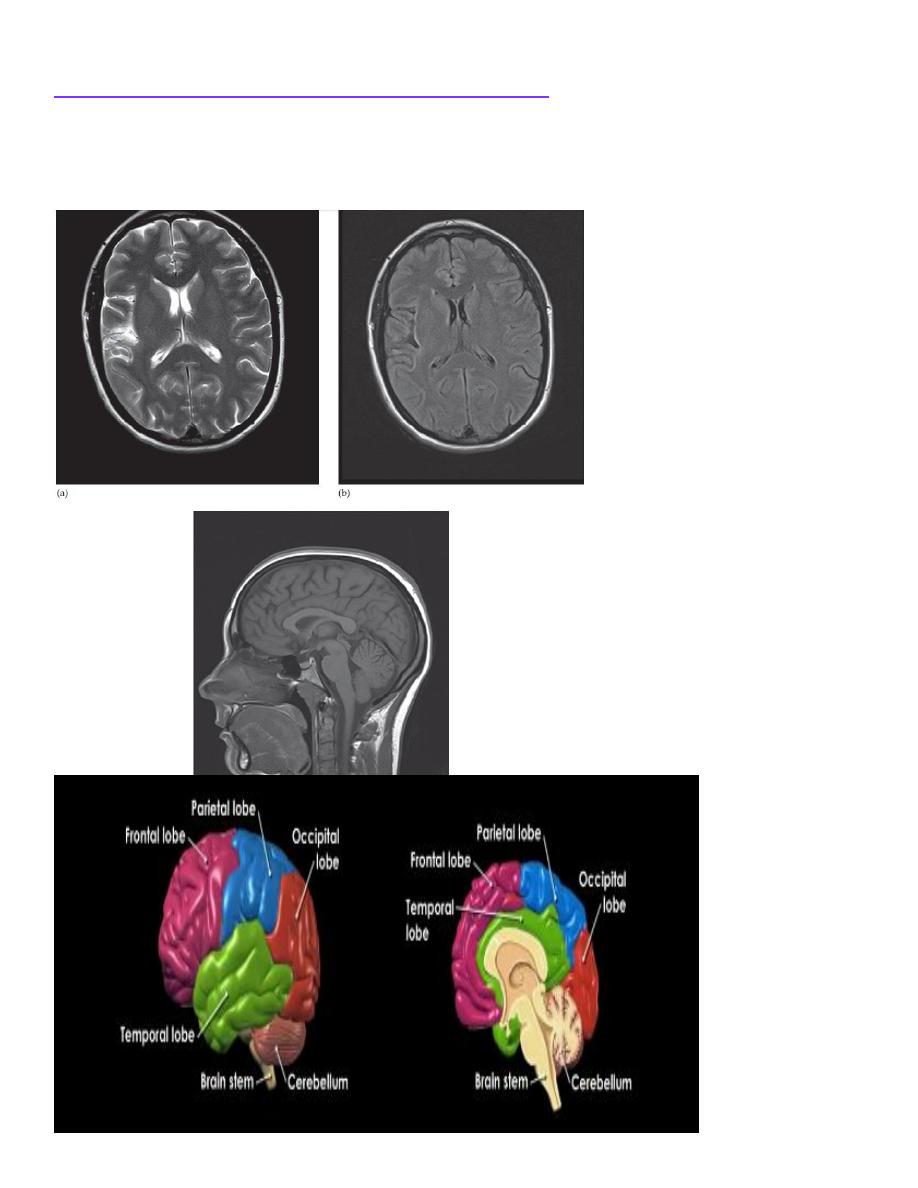
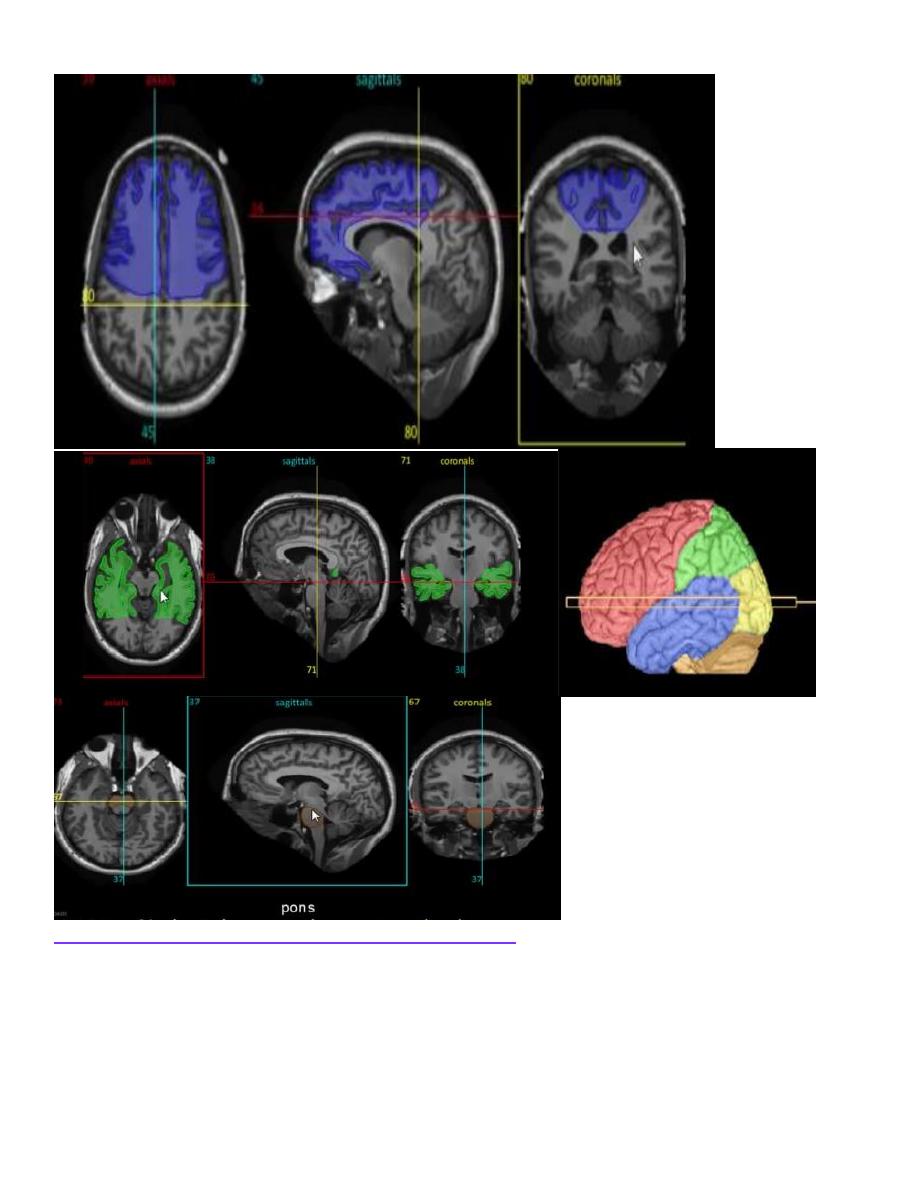
Magnetic resonance imaging
The advantage of brain MRI is its superior spatial and contrast resolution without the artifact problems
associated with local bone structures on CT. Therefore, the anatomy of the brain can be exquisitely
displayed and enables much better visualization of brain pathologies, particularly in areas such as
around the skull base for the pituitary gland and the posterior fossa which are poorly seen by CT. The
routine sequences used for MRI vary but usually include T1- and T2-weighted sequences in orthogonal
planes
A FLAIR (fluid attenuated inversion recovery) sequence is useful as the pulse sequence nulls the bright
signal from CSF, making brain pathology (usually T2 bright) more visible. Magnetic resonance can
also recognize flowing blood within larger arteries and veins, which can be examined without the need
for contrast medium to create intracranial angiograms .
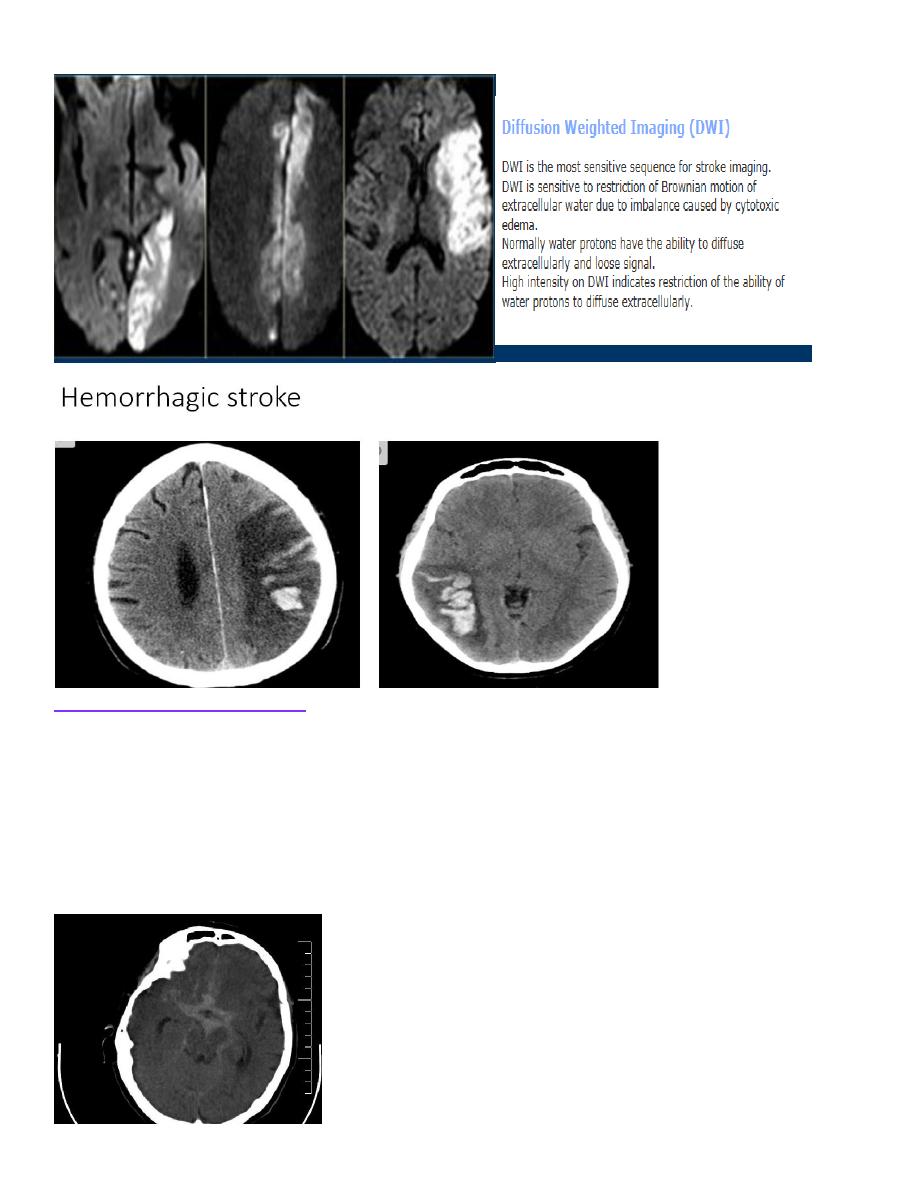
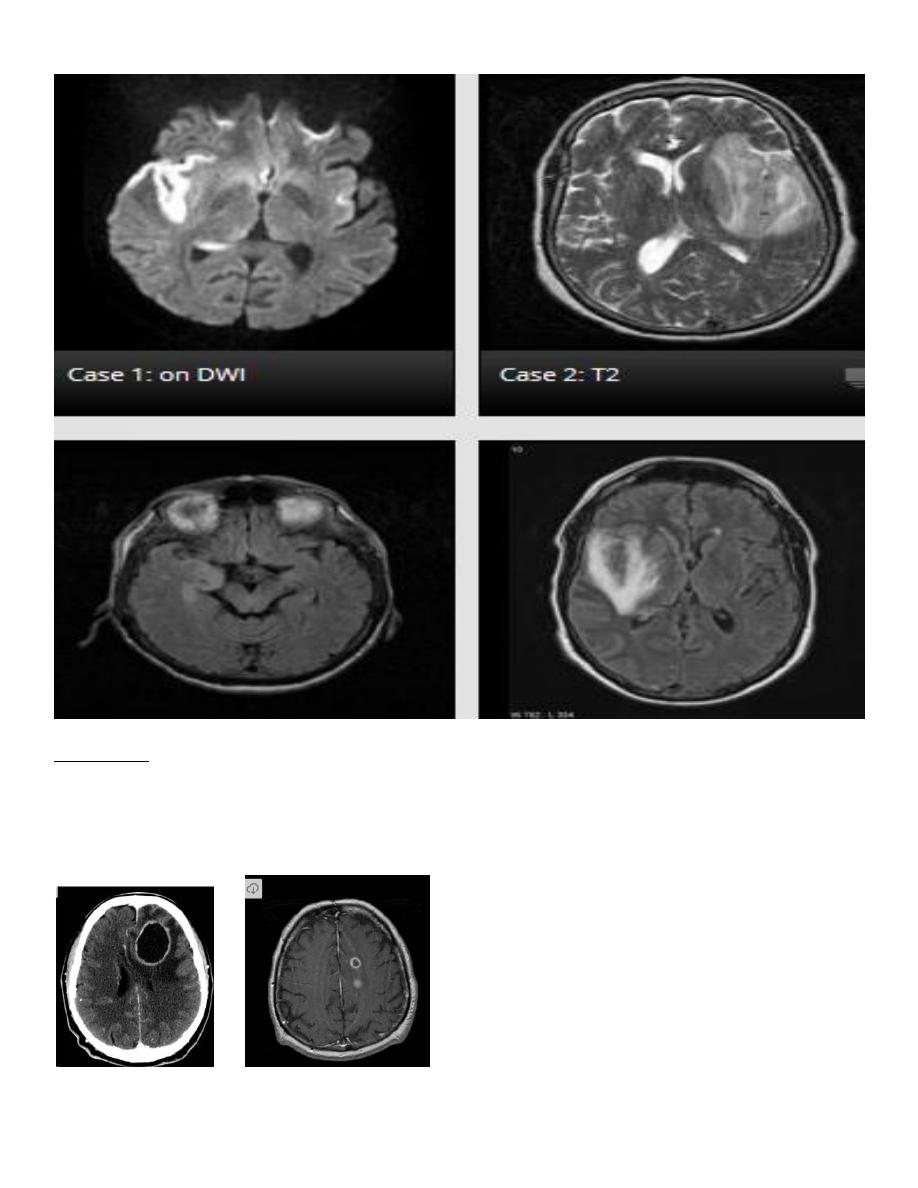
The diffusion-weighted imaging (DWI) sequence looks at the normally random movement of water
molecules in brain tissue and is extremely useful, particularly when the patient is suspected of having
an acute stroke. Within areas of cytotoxic oedema such as an infarct, the movement
of water molecules in the extracellular space is limited by the swollen, dying cells and this produces
bright signal, whereas the movement of water within vasogenic oedema is not limited (free) and does
not produce any signal change. The DWI scan becomes positive within minutes of an acute stroke
whereas CT abnormalities can take hours and will miss very small infarcts. Restricted diffusion within
a cystic mass is also relatively specific for pus within a pyogenic abscess.
The water molecules in normal axons making up the white matter are unlikely to traverse the myelin
sheath and therefore flow more rapidly in the direction of the axon bundle. An advance in diffusion
imaging uses this feature to demonstrate the location and orientation of the tracts connecting various
parts of the brain: an investigation known as diffusion tensor imaging or tractography, which may be
helpful for studying white matter pathways in disease and for surgical planning.
Functional MRI utilizes different techniques to measure the blood flow to parts of the brain which
changes depending on the neuronal activity in that location at the time of scanning. The patient is
usually scanned whilst performing various tasks such as memory recall and the scan produces a map of
brain activity superimposed on the anatomical location. The technique may be useful in understanding
brain function, particularly in psychiatric disorders The disadvantages of MRI compared with CT
include the limited visualization of calcification and lack of bone detail. Each sequence has to be
acquired separately so the overall scan time is much longer, during which the patient has to lie still, and
monitoring seriously ill patients within the scanner can be difficult. If intubated, the life support and
monitoring equipment must be MRI compatible. Any intracranial ferrous metal present such as
aneurysm clips or cochlear implants are absolute contraindications
.
د.منى
\
radiology L4
د.منى
\
radiology L4
د.منى
\
radiology L4
Contrast enhancement for magnetic resonance imaging
the gadolinium compounds used for MRI enhancement are excluded from the normal brain substance
by the BBB.
Breakdown of the BBB, such as by tumours or abscesses, means that contrast will accumulate within
these pathological processes and show high signal intensity (i.e. they appear white) on T1-weighted
images
د.منى
\
radiology L4
Abnormal magnetic resonance imaging of the brain
The range of normal anatomy and abnormalities that can be shown by MRI is very great. Fat,
haemorrhage, oedema, CSF and flowing blood all have characteristic signal intensities.
Thus, it is more often possible to make a specific diagnosis of an intracranial disorder with MRI than
with CT. MRI is the preferred investigation in intracranial sepsis, tumours, inflammatory diseases,
epilepsy and congenital malformations. Haemorrhage can be seen on MRI and the blood can be aged as
haematomas develop a specific signal pattern owing to the breakdown products of haemoglobin, such
as methaemaglobin or haemosiderin. These have different paramagnetic effects that profoundly alter
the MR signal in a way that can be recognized on T1- and T2-weighted scans
د.منى
\
radiology L4
Specific brain disorders
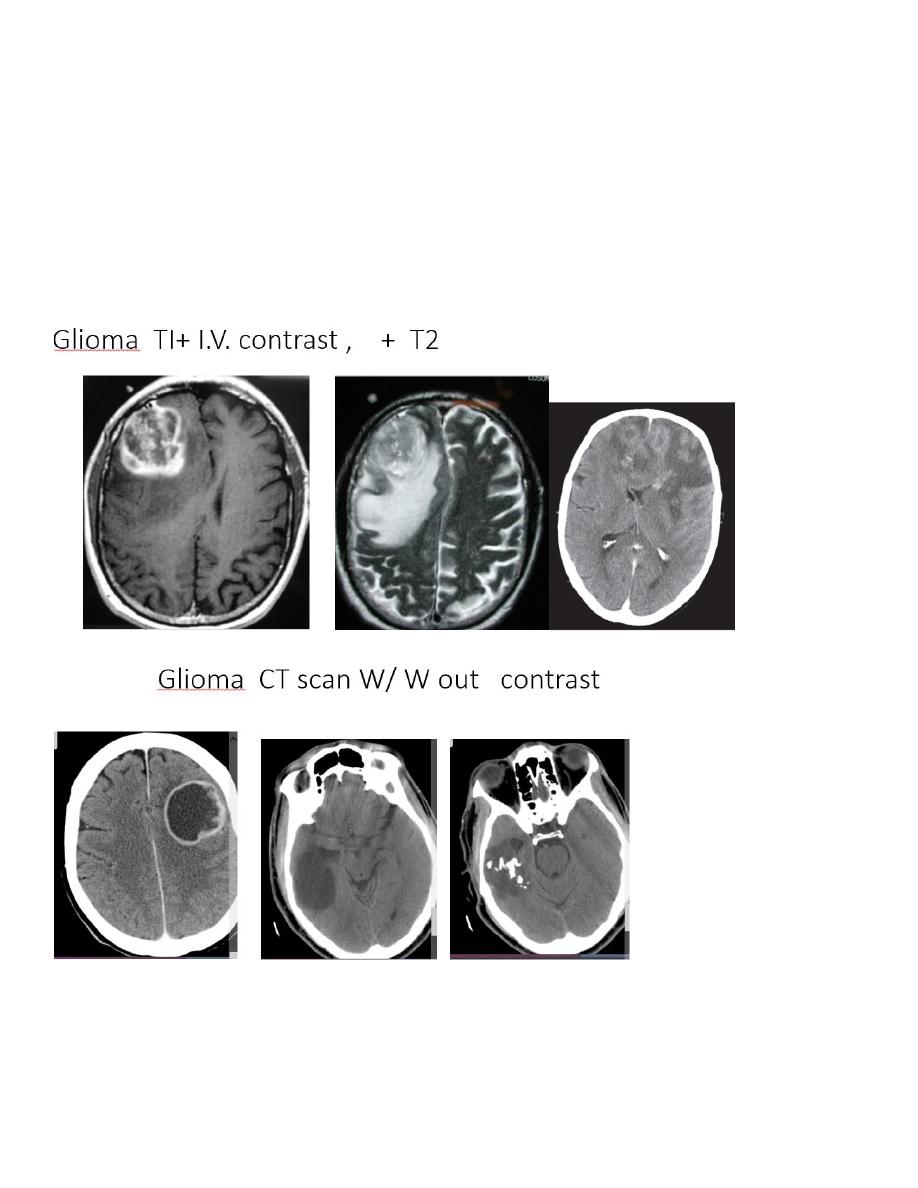
Glioma
Glioma is a non-specific term used to describe a group of tumours that arise from glial cells, which
normally support the brain neurons, such as astrocytes (astrocytoma is the commonest tumour type).
They range from low grade (e.g. childhood pilocytic astrocytoma) to high grade (e.g. glioblastoma
د.منى
\
radiology L4
multiforme). At CT, a glioma typically appears as a solitary, irregular, low attenuation lesion .Local
mass effect can usually be demonstrated although this can be minimal as the glioma is replacing rather
than expanding brain tissue. Gliomas may calcify
– particularly oligodendrogliomas. For accurate
assessment of gliomas, both pre and post contrast scans should be performed as enhancement can be
associated with a higher grade of malignancy.
The MRI features are similar to those of a mass, often with adjacent signal change. However, it is
important to realize that tumour cells will be present beyond the margin of any signal change seen
around a glioma. The mass may show a variety of signal intensities but, in general, the tumour is lower
in signal intensity than the normal brain on the T1-weighted images and higher in signal intensity
on the T2-weighted images. Calcification, though sometimes recognizable as absence of signal, is less
evident than it is with CT.
د.منى
\
radiology L4
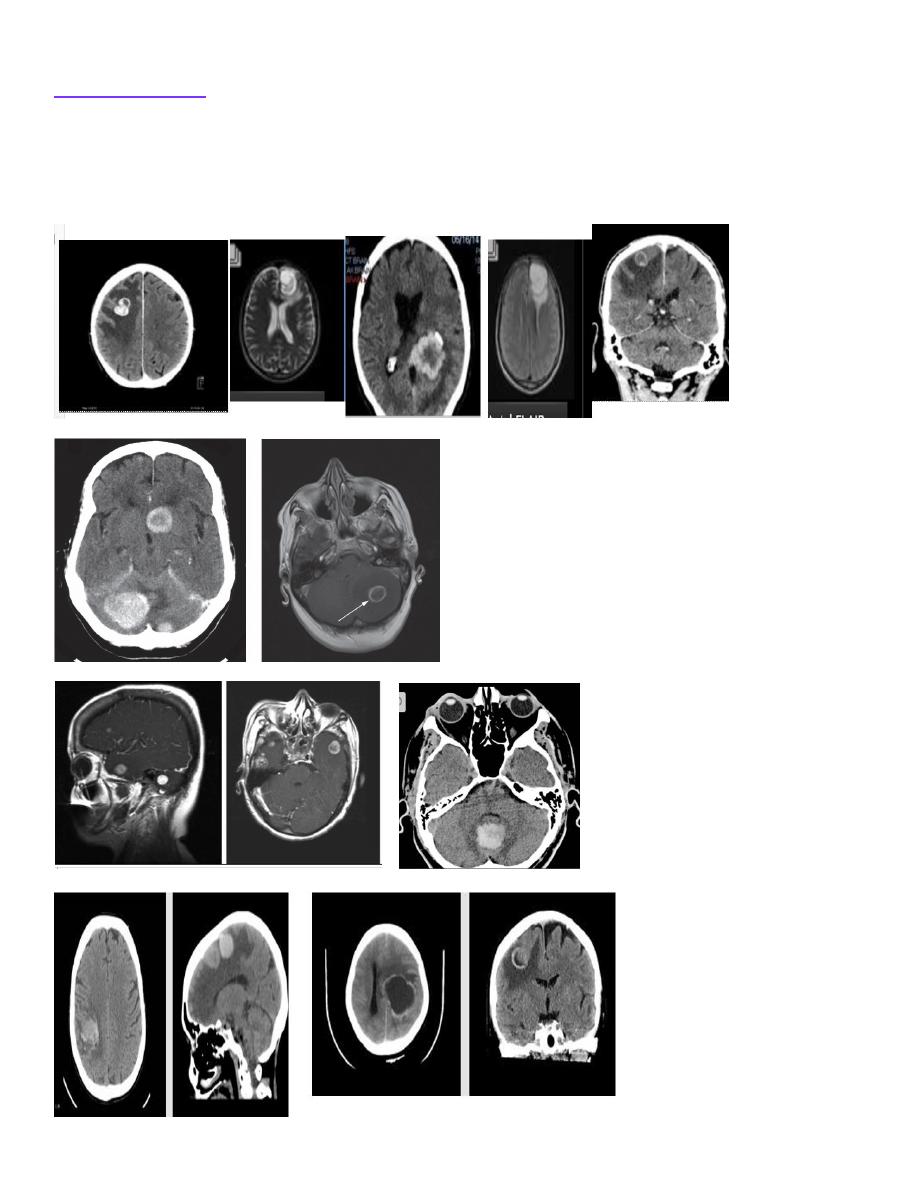
Brain metastases
Metastases in the brain are often low density on CT unless they are haemorrhagic. On CT and MRI,
they usually show contrast enhancement and are often surrounded by substantial oedema. Metastases
are typically multiple but a solitary metastasis can be indistinguishable from a primary intracerebral
brain tumour with either technique. A parenchymal lesion in the posterior fossa of an adult should be
considered to be a metastasis until proven otherwise.
د.منى
\
radiology L4
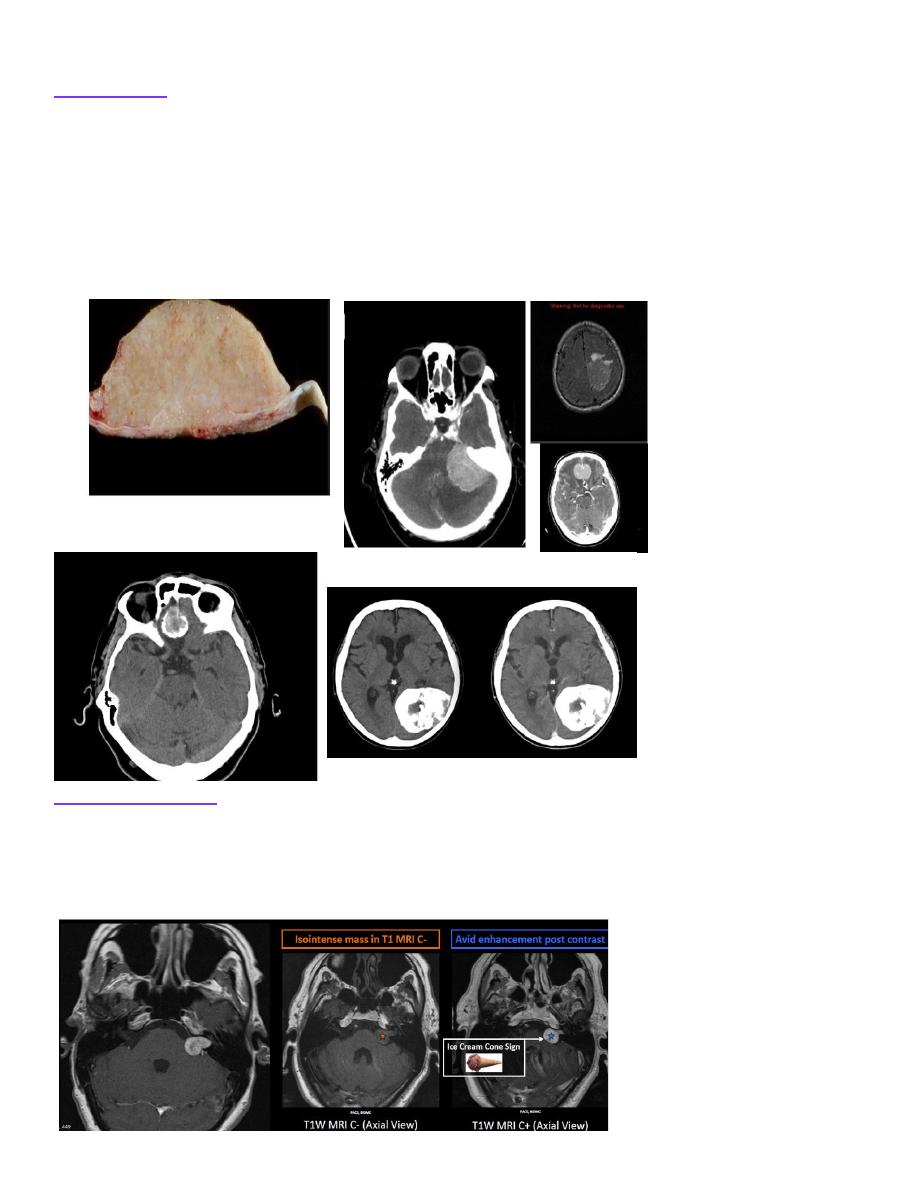
Meningioma
Meningiomas are the commonest non-glial intracranial tumour and arise from the meninges of the
vault, falx or tentorium. The commonest sites are the parasagittal region, over the cerebral convexities
and the sphenoid ridges. On an unenhanced CT scan, a meningioma is often denser than the brain
because of calcium within the lesion . Following intravenous contrast, the tumour shows marked
homogeneous enhancement (. Reactive sclerosis and blistering of the adjacent bone with thickening
and enhancement of the local dura may also be seen. The multiplanar imaging capability of MRI makes
it possible to predict the site of origin of the tumour with greater confidence than is usually possible
with CT. Once it can be ascertained that an enhancing tumour is extra-axial, by compressing the brain
from outside, the diagnosis of meningioma becomes highly likely.
Acoustic neuroma
The term
‘acoustic neuroma’ is a misnomer as they are schwannomas that arise from the vestibular
branch of the vestibulocochlear nerve. Vestibular schwannomas typically arise on the nerve within the
internal auditory canal and may extend out medially into the cerebellopontine angle . When large, they
can be recognized at CT or MRI. When small, they may only be identifiable with high resolution MRI
As schwann cells are not glial in origin, they enhance avidly.
د.منى
\
radiology L4
Stroke
Stroke is defined as a sudden, focal neurological deterioration due to a disturbance in the blood supply
to the brain. It is a common cause of hospital admission and has a high morbidity. The important
causes of stroke are:
• Cerebral infarction, which may be due to in situ thrombus or embolus from the proximal artery or
heart.
• Intracerebral haemorrhage.
• Subarachnoid haemorrhage.
Acute cerebral infarction and haemorrhage are often clinically similar, but it is important to distinguish
between these two conditions as subsequent investigation and treatment differ greatly. The acute
management of thromboembolic infarct is aimed at destroying the clot with thrombolysis, but this is
contraindicated in the presence of haemorrhage
– therefore CT is the best first test.
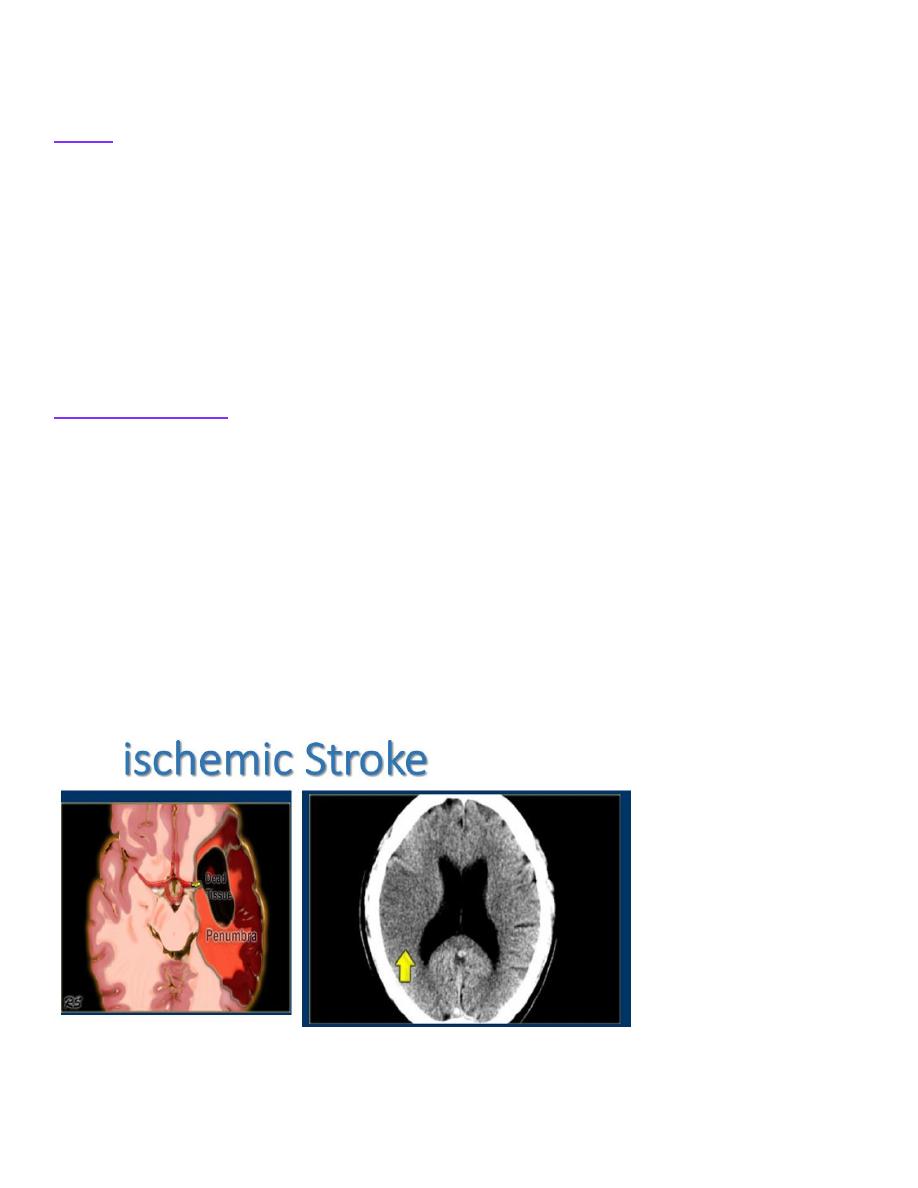
Cerebral infarction
There are four main outcomes of CT performed for an acute stroke:
• The presence of haemorrhage precludes thrombolysis treatment and is described below.
• Stroke mimics are conditions that present like stroke, such as a subdural haematoma or brain tumour,
for which different treatments are required.
• A normal scan either means the patient is not having a stroke (stroke mimic not identifiable by
imaging, such as hemiplegic migraine) or is at the very early stages of a stroke before the CT becomes
abnormal and therefore is an ideal candidate for thrombolysis.
• Then there are the early signs of a stroke seen on CT. The dense artery sign is high density clot
visualized within a major intracranial artery. Later, infarcted brain becomes lower attenuation which is
initially best seen in areas such as the lentiform nucleus and later may involve the whole vascular
territory. The infarct will gradually resolve, leaving an atrophic area of low attenuation gliosis.
Diffusion-weighted imaging is the most sensitive method for the early detection of an infarct and will
show changes within minutes of the onset . However, its use acutely is limited by scanning time,
availability and problems obtaining safety clearance.
د.منى
\
radiology L4
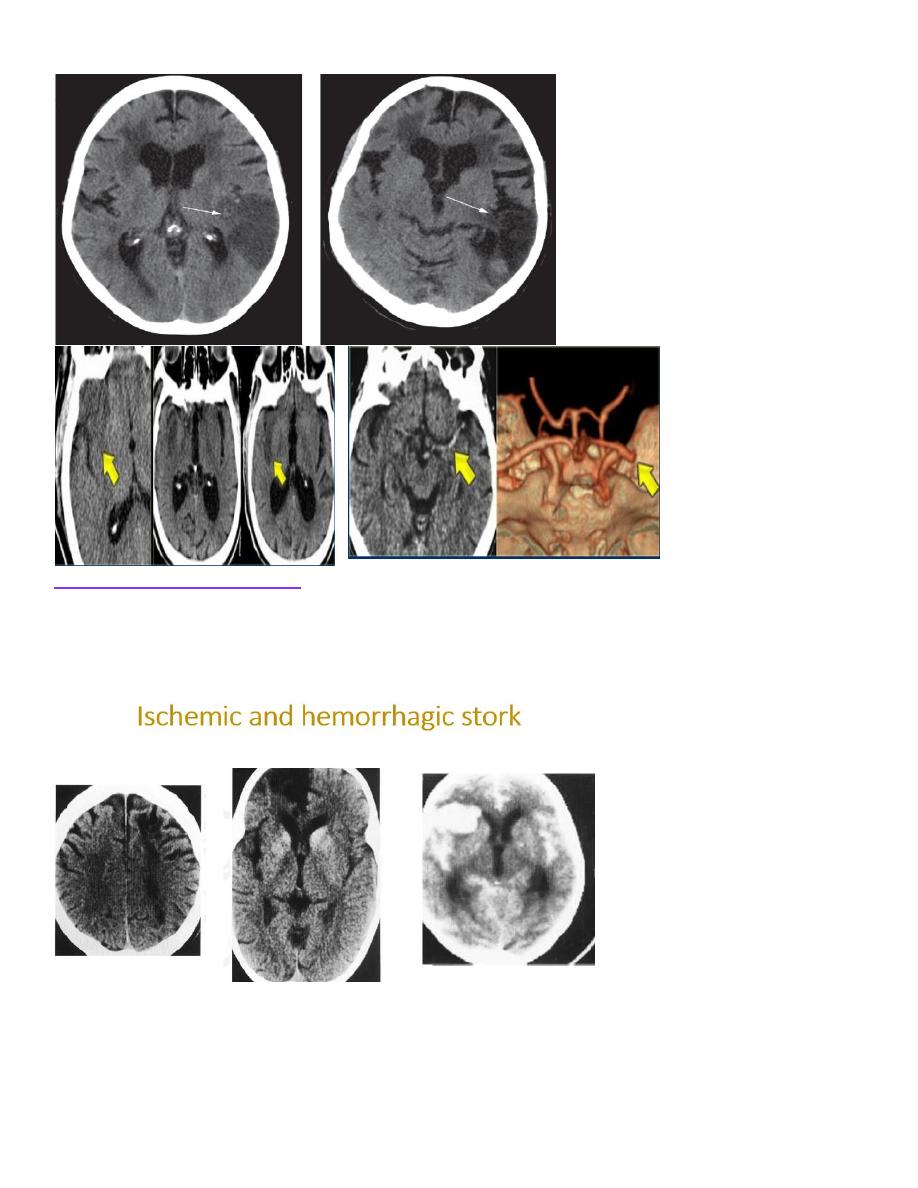
Intracerebral haemorrhage
Acute haemorrhage is seen on CT as high attenuation, frequently causing a mass effect .The initial high
density lessens over time, leaving a low density area indistinguishable from an infarct. MRI is useful in
the follow-up of intracerebral haemorrhages to exclude underlying vascular malformation or occult
metastasis, which may be obscured by the presence of blood. If no cause is identified, formal cerebral
angiography may be required to exclude a subtle vascular anomaly.
د.منى
\
radiology L4
د.منى
\
radiology L4
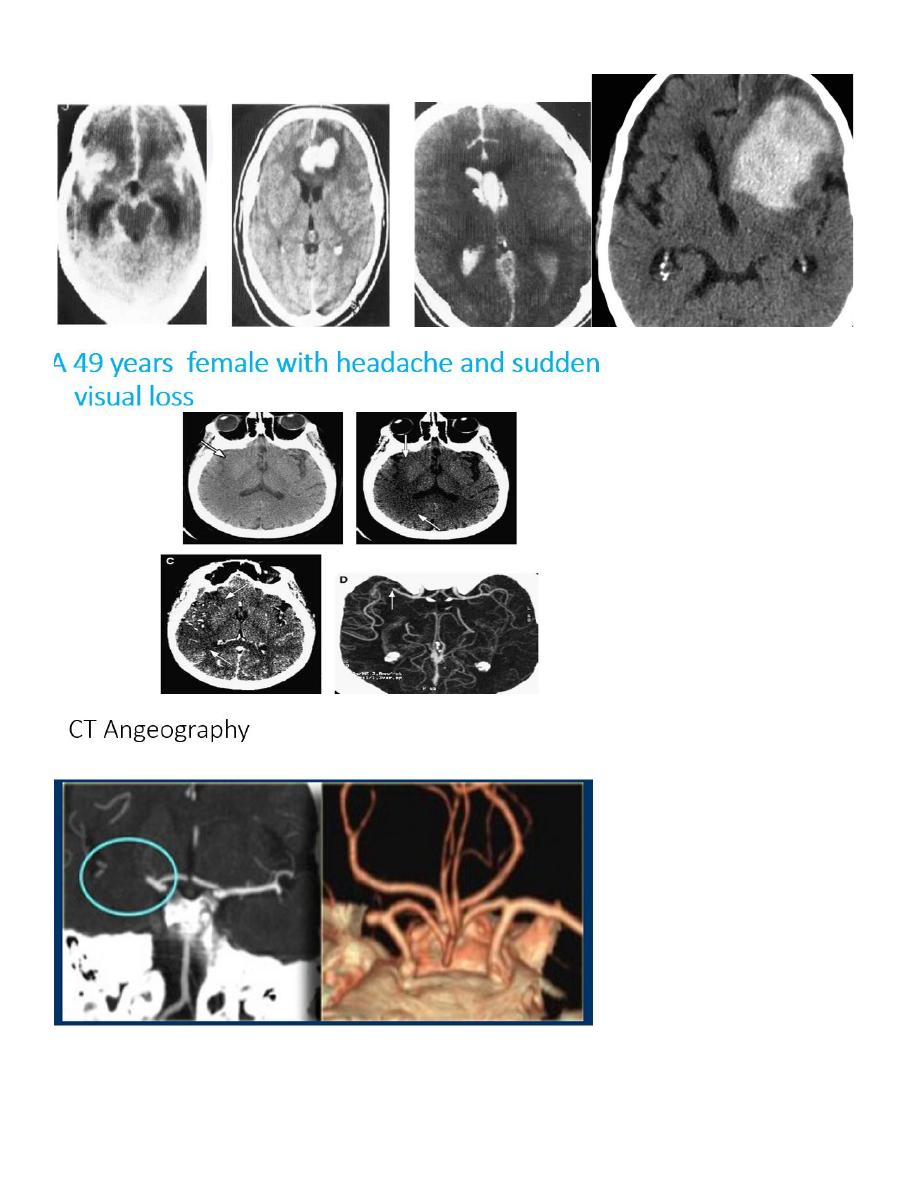
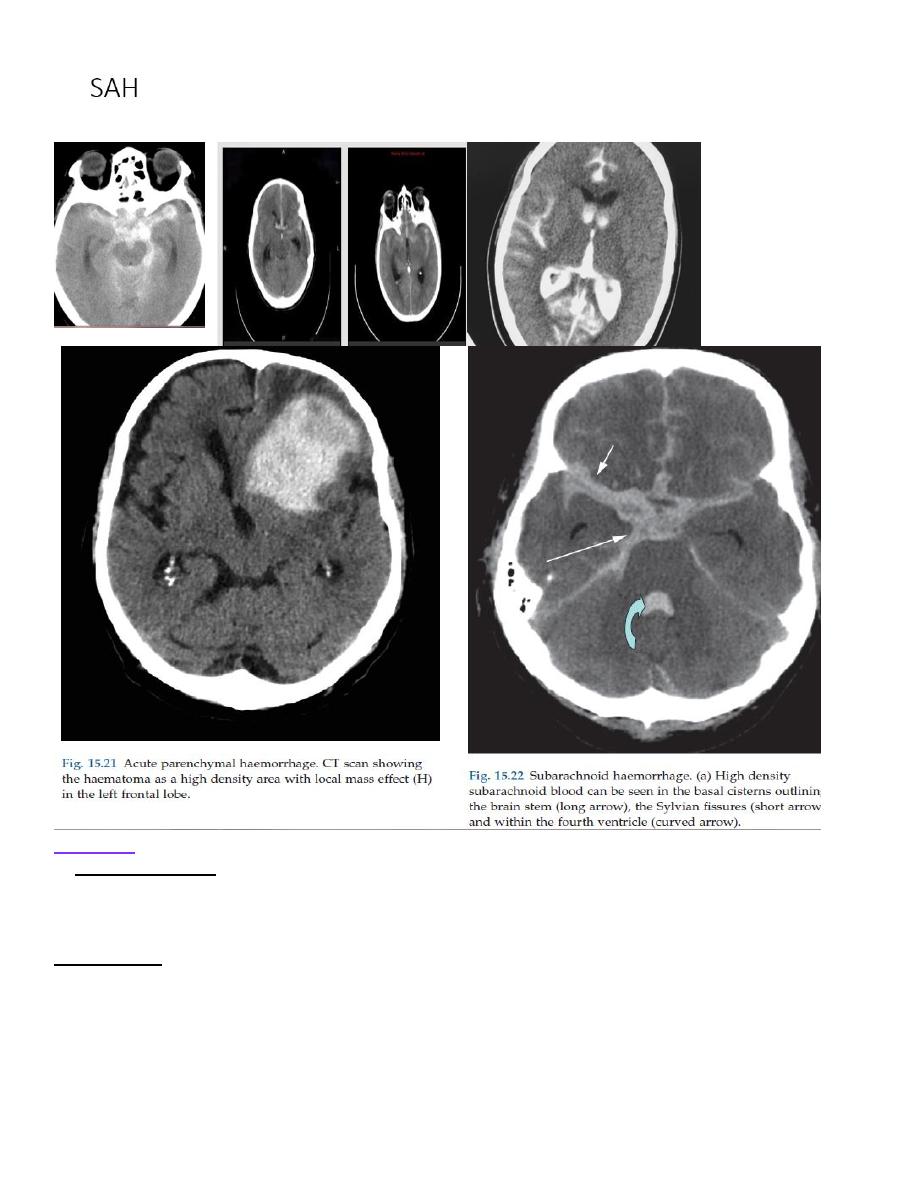
Subarachnoid haemorrhage
Spontaneous subarachnoid haemorrhage is usually due to a ruptured intracranial aneurysm or vascular
malformation. CT is the best initial investigation to diagnose a subarachnoid haemorrhage and to
demonstrate the site of bleeding. A subarachnoid haemorrhage is recognized by high density blood
outside the brain in the sulci, Sylvian fissures and basal cisterns. Subarachnoid haemorrhage on CT will
obviate the need for lumbar puncture and CSF examination, but sensitivity of CT decreases with time
after a haemorrhage and a normal examination does not exclude the diagnosis. CT angiography can be
used to demonstrate the aneurysm and to plan treatment by neurosurgical clipping or by interventional
radiological microcatheter techniques which occlude the aneurysm with metal coils. Ateriovenous
malformations may be coiled or embolized to reduce the size and risk of haemorrhage
د.منى
\
radiology L4
Infection
In acute meningitis CT and MRI are usually normal and antibiotics should start immediately and not
await the result of a scan. A lumbar puncture is frequently performed to obtain CSF to confirm the
diagnosis. A CT scan prior to lumbar puncture is only essential if there is evidence of raised
intracranial pressure, focal neurological signs or change in conscious level.
Encephalitis is caused by infection, usually viral. CT and MRI show unilateral or asymmetrical
bilateral, focal abnormal areas, often in a characteristic distribution appearing as low attenuation on CT
and high signal on a T2-weighted MRI scan. The commonest cause of viral encephalitis
is herpes simplex, which typically produces abnormalities in the medial temporal lobe, insular cortex
and inferior frontal lobes. These areas may contain areas of haemorrhage and enhancement.
د.منى
\
radiology L4
An abscess can be caused by bacterial, tuberculous, fungal or parasitic organisms. Necrosis and pus
formation occur in the centre of the abscess, which appears as low density on CT or fluid on MRI. The
wall of the abscess enhances with intravenous contrast and may be surrounded by oedema, giving an
appearance known as
‘ring enhancement’ . The pus within the centre of a pyogenic abscess will
typically demonstrate restricted diffusion.
د.منى
\
radiology L4
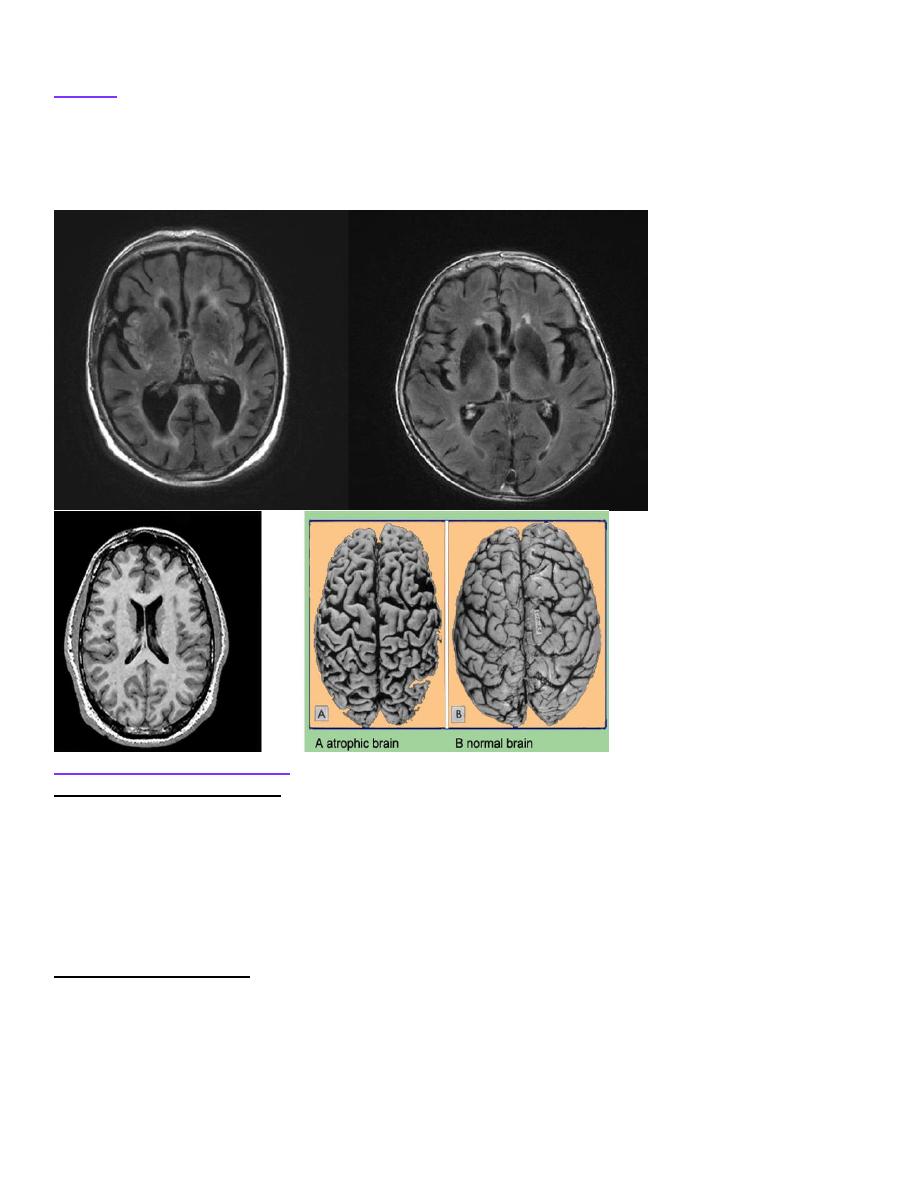
Ageing
Various changes can be seen on CT and MRI in elderly patients that often bear little correlation with
the clinical state of the patient. Atrophy of the brain occurs, resulting in dilatation of the ventricles and
widening of the cortical sulci. Small vessel atherosclerotic ischaemia can produce low attenuation areas
in the deep white matter on CT, normally seen in the periventricular regions, which are
T2=hyperintense on MRI.
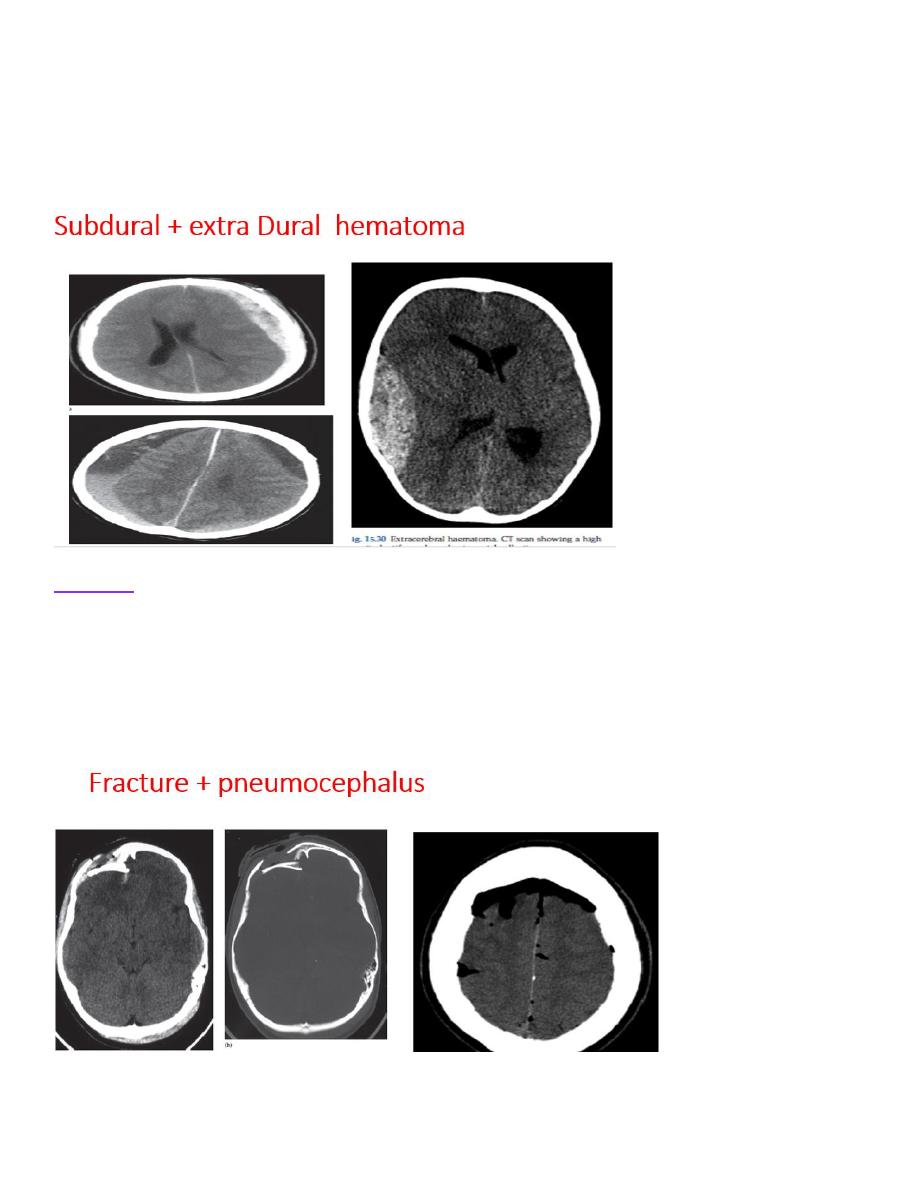
Extracerebral haematoma
Extracerebral haematomas comprise extradural and subdural haematomas, depending on the location
of the blood in relation to the dura mater layer of the meninges. An extradural haematoma is seen as a
lens-shaped, high density area situated over the surface of the cerebral hemisphere that does not cross
sutures as it lies below the periosteal layer of the skull . It is normally an arterial bleed from a
meningeal artery which was damaged by a skull fracture
– a common associated finding – and
therefore occurs at the site of head impact (coup injury). As it is an arterial bleed, an initial period of
lucidity is followed by rapid loss of consciousness as the intracranial pressure increases, requiring
emergency surgical evacuation.
A subdural haematoma is seen as a crescenteric collection of blood that conforms to the shape of the
underlying brain and occurs most commonly over the convexity of the brain where it is not limited by
any of the skull sutures, but can also extend along the falx and tentorium . It is normally a venous bleed
from the bridging veins which cross the subdural space and therefore is more commonly seen in
patients who have cerebral atrophy, making the veins more prone to injury. They often occur on the
side opposite to the head impact (contracoup injury) or may be bilateral following a shaking injury (as
seen in nonaccidental injury). Acutely, the blood is high density for 1
–2 weeks following injury;
د.منى
\
radiology L4
however, as the feeding system is low pressure, the haematoma may be clinically occult and become
chronic and consequently low (CSF) density after several weeks . In the intervening period,
haematomas pass through a phase of being isodense with the brain and are, therefore, less obvious on
CT scans. They should be suspected if there is any midline displacement or ventricular compression.
The displacement may not be obvious if the haematomas are bilateral, when effacement of the sulci
may be the only clue to their presence
Fracture
Fractures of the skull base or vault should be looked for on bone window settings . Fractures of the
skull vault should not be confused with normal sutures or vascular markings. Assessment should be
made of any significant depression of the fracture as these may require surgical elevation and are more
likely to be associated with underlying brain injury. If there is a penetrating skull injury or a fracture
involves the normally pneumatized paranasal sinuses, middle ears or mastoids, air may enter the
cranium and be seen on CT as locules of very low density gas . CT can also demonstrate fluid (blood)
in the sinuses and mastoid air cells or air in the orbits, suggesting a facial or skull base fracture.
Noor Rahman
