The shoulder and pectoral girdle
Dr.Ammr Talib Al-YassiriCollege of Medicine/Baghdad University
Learning outcomes
Rotator cuff disordersInstability of the shoulder
Disorders of the glenohumeraljoint
Disorders of the scapula
Rotator cuff disorders
The rotator cuff is made up of the lat. portions ofteres minor,
infraspinatus,
supraspinatus and
subscapularis
contraction of the individual muscles exerts a rotational pull on the proximal end of the humerus,
the main function of the conjoint structure is to draw the head of the humerus firmly into the glenoid socket and stabilize it there
The commonest cause of pain around the shoulder ‘rotator cuff syndrome’
supraspinatus impingement syndrome and tendinitisTears of the rotator cuff
Acute calcific tendinitis
Adhesive capsulitis (frozen shoulder)
Biceps tendinitis and/or rupture.
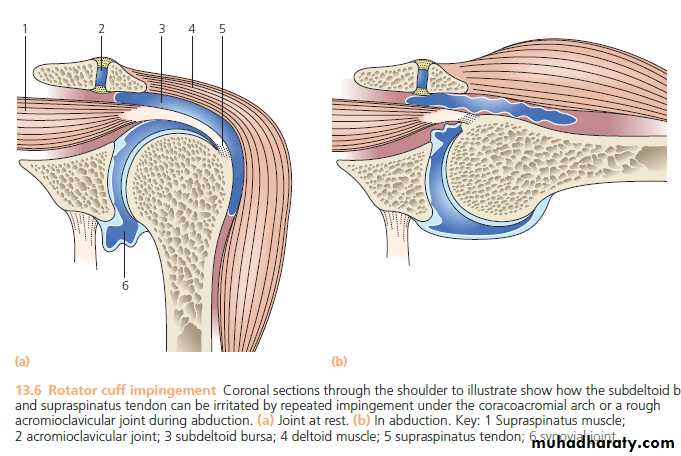
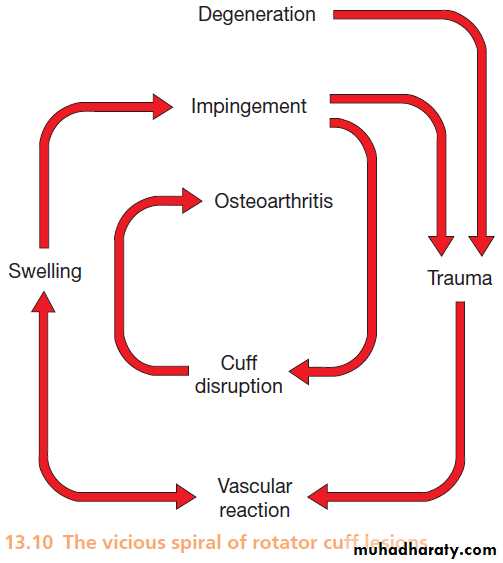
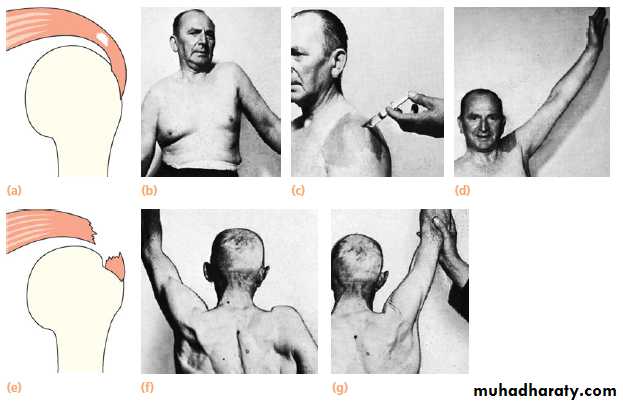
IMPINGEMENT SYNDROME, SUPRASPINATUS TENDINITIS AND CUFF DISRUPTIONPATHOLOGY
a painful disorder which is thought to arise from repetitive compression or rubbing of the tendons (mainly supraspinatus) under the coracoacromial arch.The impingement position(abduction, slight flexion and internal rotation)
The site of impingement ‘critical area’
supraspinatus tendinitis may also occur initially in response to severe repetitive stress
factors which may predispose to repetitive impingement are
osteoarthritic thickening of the acromioclavicular joint,
Swelling of the cuff or the subacromial bursa in inflammatory disorders such as gout or rheumatoid arthritis.
Variations of acromial morphology.
CLINICAL FEATURES
pain and/or weakness (over the front and lateral aspect of the shoulder during activities with the arm abducted and medially rotated)Tenderness
Three patterns are encountered:
Subacute tendinitis – the ‘painful arc syndrome’, due to vascular congestion, microscopic haemorrhage and oedema.
Chronic tendinitis – recurrent shoulder pain due to tendinitis and fibrosis.
Cuff disruption – recurrent pain, weakness and loss of movement due to tears in the rotator cuff.
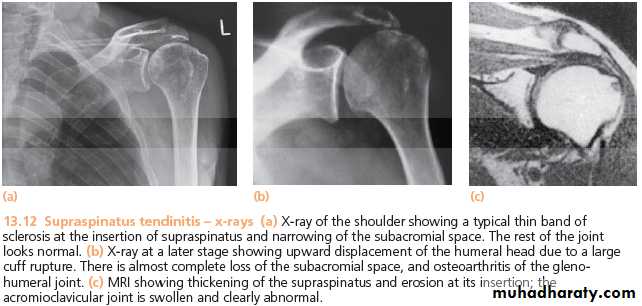
IMAGING FOR ROTATOR CUFF DISORDERS:
X-ray examinationnormal in the early stages
chronic tendinitis :
erosion, sclerosis or cyst formation at the site of cuff insertion
caudal tilt view
Osteoarthritis of the acromioclavicular joint
late cases :glenohumeral joint osteoarthritis
MRI
Ultrasonography
TREATMENT OF CUFF DISORDERS
Conservative treatment:avoiding the ‘impingement position’
Physiotherapy
A short course of non-steroidal anti-inflammatory tablets
If all these methods fail, the patient should be given one or two injections of depot corticosteroid into the subacromial space.
protective modifications of shoulder activity for at least 6 months.
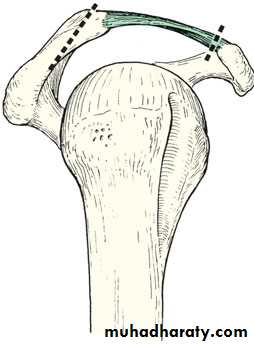
Surgical treatment
Indications
If symptoms do not subside after 3 months of conservative treatment
if they recur persistently after each period of treatment
The indication is more pressing if there are signs of a partial rotator cuff tear and in particular full thickness tear in a younger patient.
The object is to decompress the rotator cuff
Repair of the rotator cuff tear if it is indicated
chronic pain,
weakness of the shoulder and significant loss of function.
The younger and more active the patient, the greater is the justification for surgery
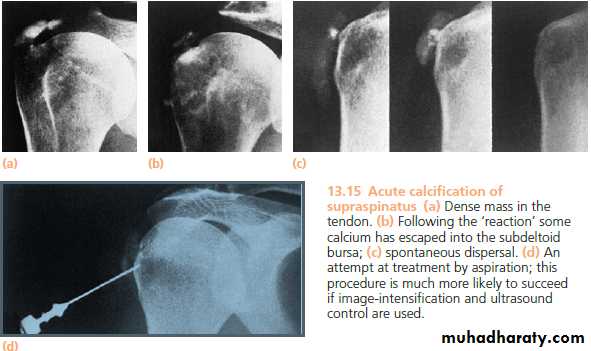
ACUTE CALCIFIC TENDINITIS
Acute shoulder pain may follow deposition of calcium hydroxyapatite crystals, usually in the ‘critical zone’ of the supraspinatus tendon.local ischaemia leads to fibrocartilaginous metaplasia and deposition of crystals by the chondrocytes.
Clinical features
30–50 year-olds
Aching agonizing climax After a few days, pain subsides
During the acute stage the arm is held immobile
the joint is usually too tender to permit palpation or movement.
X-RAYS
Calcification just above the greater tuberosity
Treatment
NON-OPERATIVE
TREATMENT
OPERATIVE
TREATMENT
LESIONS OF THE BICEPS TENDON
TendenitisC/F
usually occurs together with rotator cuff impingement
Tenderness
TREATMENT
Non operative
Operative
Rupture
C/F
usually accompanies rotator cuff disruption
aged over 50
Snap
Pain
Bruise
Lump
Treatment
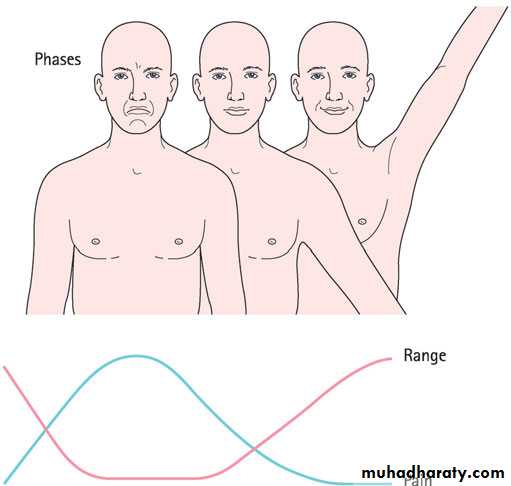
ADHESIVE CAPSULITIS (FROZEN SHOULDER)
progressive pain and stiffness of the shoulder which usually resolves spontaneously after about 18 months.The histological features are reminiscent of Dupuytren’s disease
active fibroblastic proliferation in the rotator interval, anterior capsule and coraco-humeral ligament.
The condition is particularly associated with
diabetes,
Dupuytren’s disease,
hyperlipidaemia,
hyperthyroidism,
cardiac disease
hemiplegia.
It occasionally appears after recovery from neurosurgery
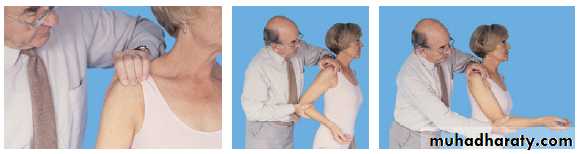
Clinical features
aged 40–60history of trauma
aching in the arm and shoulder
stiffness, untreated stiffness persists for another 6-12 months
slight wasting
tenderness is seldom marked
cardinal features is stubborn lack of movements in all directions.
X-rays are normal
Differential dignosis:
Infection.Post-traumatic stiffness
Diffuse stiffness
Reflex sympathetic dystrophy
Treatment
CONSERVATIVE TREATMENT
analgesics and anti-inflammatory
‘pendulum’ exercises
reassure
Manipulation under general anaesthesia +injection with methylprednisolone and lignocaine
injecting a large volume (50–200 mL) of sterile saline under pressure
SURGICAL TREATMENT: Arthroscopic capsular release
INSTABILITY OF THE SHOULDER
The shoulder achieves its uniquely wide range of movement at the cost of stabilityPathogenetic classification
shoulders become unstable because one of:
structural changes
unbalanced muscle recruitment
Three polar types of disorder can be identified:
Type I Traumatic structural instability.
Type II Atraumatic (or minimally traumatic) structural instability.
Type III Atraumatic non-structural instability (muscular dyskinesia)
TRAUMATIC ANTERIOR INSTABILITY– POLAR TYPE I
PATHOLOGY
commonest type (over 95 per cent)
usually follows an acute injury
• the classic Bankart lesion
• the Hill–Sachs lesion
• In other cases the labral tear and bone defect may be absent, althuogh the inferior gleno-humeral ligament will be stretched
• In patients over the age of 50, dislocation is often associated with tears of the rotator cuff.
Clinical features
young man or woman who gives a history of the shoulder ‘coming out’recurrent dislocation requiring treatment develops in about one-third of patients under the age of 30 and in about 20 per cent of older patients.
Recurrent subluxation a ‘catching’ sensation, followed by ‘numbness’ or ‘weakness’- the so called‘dead arm syndrome’ whenever the shoulder is used with the arm in the overhead position
On examination
apprehension test
Imaging
x-ray: The Hill–Sachs lesion (when it ispresent) is best shown by an anteroposterior x-ray with the shoulder internally rotated, or in the axillary view. Subluxation is seen in the axillary view.MRI or MR arthrography: bone lesions and labral tears.
Treatment
If dislocation recurs at long intervals, the patient may choose to put up with the inconvenience and simply try to avoid vulnerable positions of the shoulder.OPERATIVE TREATMENT
indications
frequent dislocation, especially if this is painful,
recurrent subluxation or a fear of dislocation sufficient to prevent participation in everyday activities, including sport.
Two types of operation are employed:
Anatomical repairsBankart procedure.
Non-anatomical repairs
Putti–Platt operation
Bristow–Laterjet operation
Kronberg and Brostrum
ATRAUMATIC OR MINIMALLY TRAUMATIC INSTABILITY – POLARTYPES II AND III
include entities such as the ‘loose shoulder’, multidirectional instability, voluntary dislocation and habitual dislocationATRAUMATIC STRUCTURAL INSTABILITY
acquired multidirectional instability
due either to
repetitive micro-trauma which has placed undue stress upon the soft tissues
or to rapid, forceful movements that contribute to the development of overall laxity of the joint;
occasionally a predisposing factor such as glenoid dysplasia is identified.
dislocation may occur in several different directions.
Treatment
REHABILITATIVE MEASURES Dedicated physiotherapy is focused on strengthening the muscles.
SURGICAL TREATMENT usually some type of capsular plication (which can be performed arthroscopically) or a capsular shift (by open operation).
ATRAUMATIC NON-STRUCTURAL INSTABILITY (ALTERED MUSCLE PATTERNING)
Each of the muscles moving and stabilizing the shoulder needs to be activated at a specific time in coordination with other protagonistic and antagonistic muscles. If this pattern is altered instability can occur.Muscle patterning instability usually occurs in younger patients who can voluntarily slip the shoulder out of joint as a trick movement (habitual),
Treatment follows much the same lines as for atraumatic structural instability but surgery should be avoided if possible.
POSTERIOR INSTABILITY
Almost always a posterior subluxationC/F:
takes the form of subluxation when the arm is used in flexion and internal rotation.
On examination,
the posterior drawer test
posterior apprehension test
TREATMENT
physiotherapy.
SURGERY : should be considered only if the primary abnormality is found to be structural
TYPES OF OPERATIONS:
1) Soft-tissue reconstructions are the mainstay of treatment.
2) Rarely glenoid osteotomy
3) In extreme cases a bony block to posterior translation of the humeral head is employed.
DISORDERS OF THE GLENOHUMERALJOINT
TUBERCULOSIS
Uncommon
starts as an osteitis but is rarely diagnosed until arthritis has supervened. This may proceed to abscess and sinus formation, but in some cases the tendency is to fibrosis and ankylosis.
Clinical features:
Adults are mainly affected.
Constant ache and stiffness lasting many months or years.
The striking feature is wasting of the muscles around the shoulder, especially the deltoid.
In neglected cases a sinus may be present over the shoulder or in the
axilla.
All movements are limited and painful.
X-rays show generalized rarefaction, usually with some erosion of the joint surfaces
Treatment: systemic treatment with antituberculous drugs, rest, If there are repeated flares, or if the articular surfaces are extensively destroyed, the joint should be arthrodesed.
RHEUMATOID ARTHRITIS
Most common arthropathy to affect the shoulder complex (90% of rheumatoid pt.)Pathology
The acromioclavicular joint : erosive arthritis
The gleno-humeral joint: synovitis, cartilage destruction and bone erosion
The subacromial bursa and the synovial sheath of the long head of biceps become inflamed and thickened; often this leads to rupture of the rotator cuff and the biceps tendon.
C/F:
generalized rheumatoid arthritis;
Pain and swelling;
the patient (usually a woman) increasing difficulty with simple tasks such as combing her hair or washing her back.
synovitis→ swelling and tenderness anteriorly, superiorly or in the axilla.
Tenosynovitis→features similar to those of cuff lesions
weakness and limitation of movement
Treatment:
general treatment of rheumatoid arthritis.
local treatment in the form of intra-articular injections of methylprednisolone
If synovitis persists, operative synovectomy is carried out; at the same time, cuff tears may be repaired.
Excision of the lateral end of the clavicle may relieve acromioclavicular pain.
total joint replacement with an unconstrained prosthesis
arthrodesis
OSTEOARTHRITIS
usually secondaryOften chondrocalcinosis is present
(‘Milwaukee shoulder’).
Clinical features:
aged 50–60
history of injury, shoulder dislocation or a previous painful arc syndrome.
movements are restricted in all directions.
X-rays
Treatment:
Analgesics and anti-inflammatory
exercises may improve mobility.
In advanced cases arthroplasty is justified
alternative is arthrodesis.
DISORDERS OF THE SCAPULA
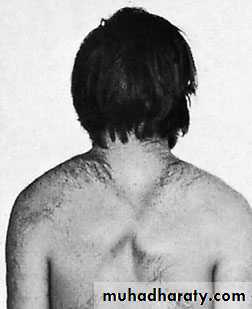
CONGENITAL ELEVATION OF THE SCAPULA
complete their descent from the neck by the third month of fetal life;
CLINICAL FEATURES
Sprengel’s deformity
Klippel–Feil syndrome
TREATMENT :
Mild cases are best left untreated.
Surgical treatment aims to decrease deformity and improve shoulder function.
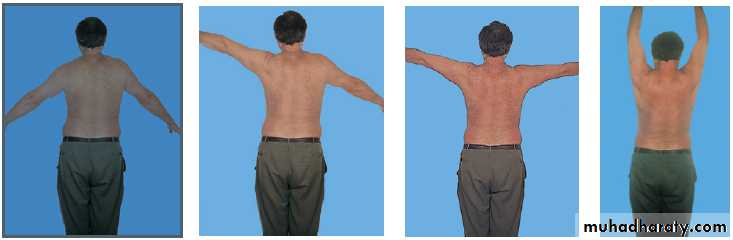
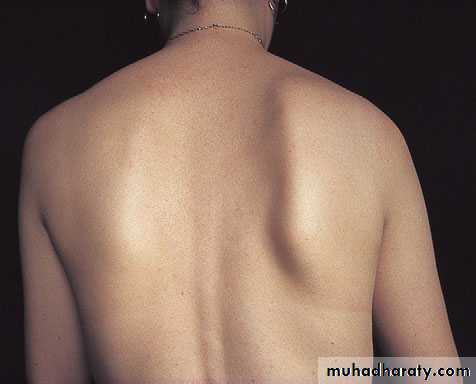
SCAPULAR INSTABILITY
Winging of the scapula is due to weakness of the serratus anterior muscle.There are several causes of weakness or paralysis of the serratus anterior muscle:
Neuralgic amyotrophy
Injury to the brachial plexus
Direct damage to the long thoracic nerve (e.g. during radical mastectomy)
fascioscapulohumeral muscular dystrophy.
Treatment: Disability is usually slight and is best accepted. However, if function is noticeably impaired, tendon transfer; or the scapula can be fixed to the rib-cage
references
Apley’s System of Orthopaedics and FracturesReview of Orthopedics, Miller
Campbell’s operative orthopaedics