Medicine Poisoning Dr. Haidar F. Abd
1 |
P a g e
Medicine Poisoning Dr. Haidar F. Abd
2 |
P a g e
Taking a history in poisoning
• What toxin(s) have been taken and how much?
• What time were they taken and by what route?
• Has alcohol or any drug of misuse been taken as well?
• Obtain details of the circumstances of the overdose from family, friends and ambulance
personnel
• Ask the general practitioner for background and details of prescribed medication
• Assess suicide risk (full psychiatric evaluation when patient has physically recovered)
• Capacity to make decisions about accepting or refusing treatment?
• Past medical history, drug history and allergies, social and family history?
• Record all information carefully
Medicine Poisoning Dr. Haidar F. Abd
3 |
P a g e
Patients who are seriously poisoned must be identified early so that appropriate management
is not delayed. Triage involves:
• immediate measurement of vital signs
• identifying the poison(s) involved and obtaining adequate information about them
• identifying patients at risk of further attempts at self-harm and removing any remaining
hazards from them.
• The Glasgow Coma Scale (GCS) is commonly employed to assess conscious level,
although it has not been specifically validated in poisoned patients.
• An electrocardiogram (ECG) should be performed and cardiac monitoring instituted in
all patients with cardiovascular features or where exposure to potentially cardiotoxic
substances is suspected.
• Patients who may need antidotes should be weighed when this is feasible, so that
appropriate doses can be prescribed.
• Substances that are unlikely to be toxic in humans should be identified so that
inappropriate admission and intervention are avoided

Medicine Poisoning Dr. Haidar F. Abd
4 |
P a g e
Substances of very low toxicity
• Writing/educational materials
• Decorating products
• Cleaning/bathroom products (except dishwasher tablets which are corrosive)
• Pharmaceuticals: oral contraceptives, most antibiotics (but not tetracyclines and
antituberculous drugs), H2-blockers, proton pump inhibitors, emollients and other skin
creams, baby lotion
• Miscellaneous: plasticine, silica gel, household plants, plant food
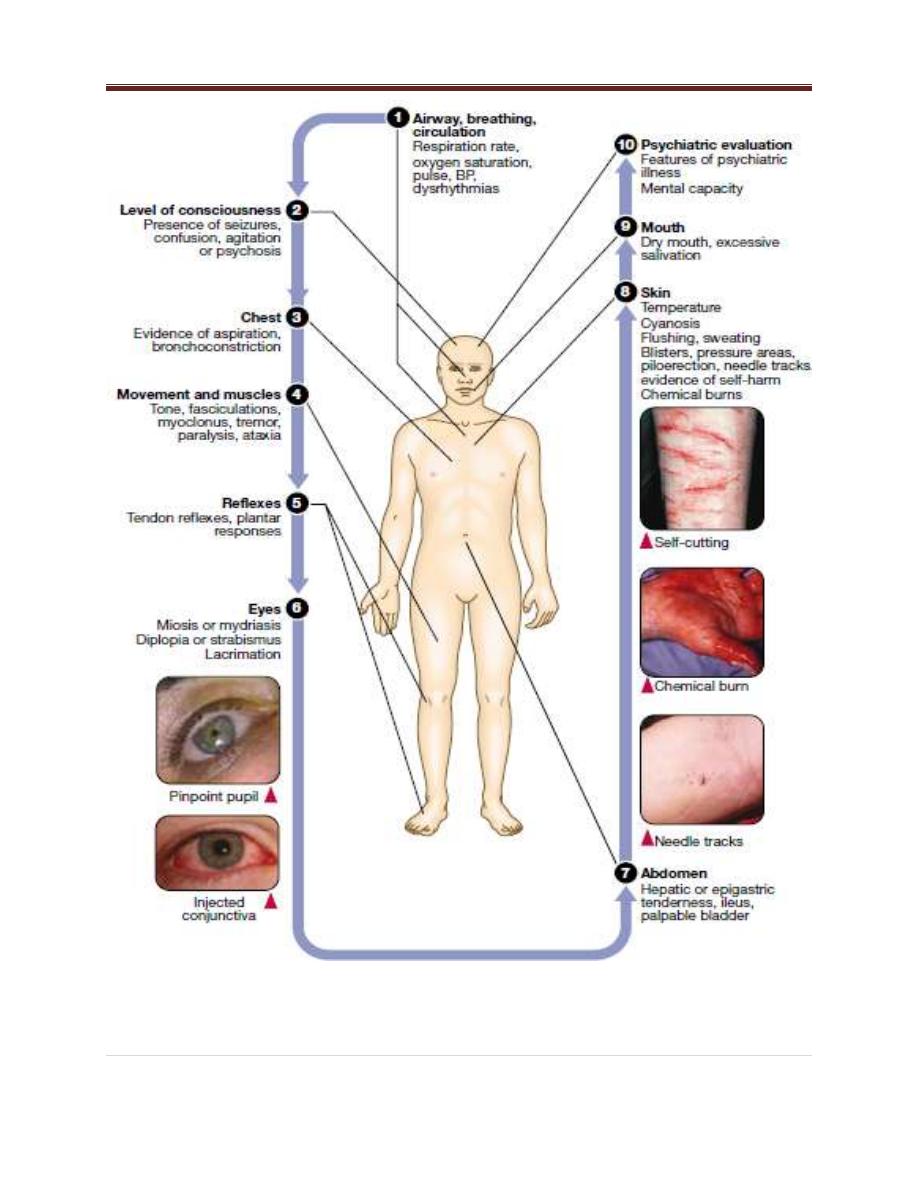
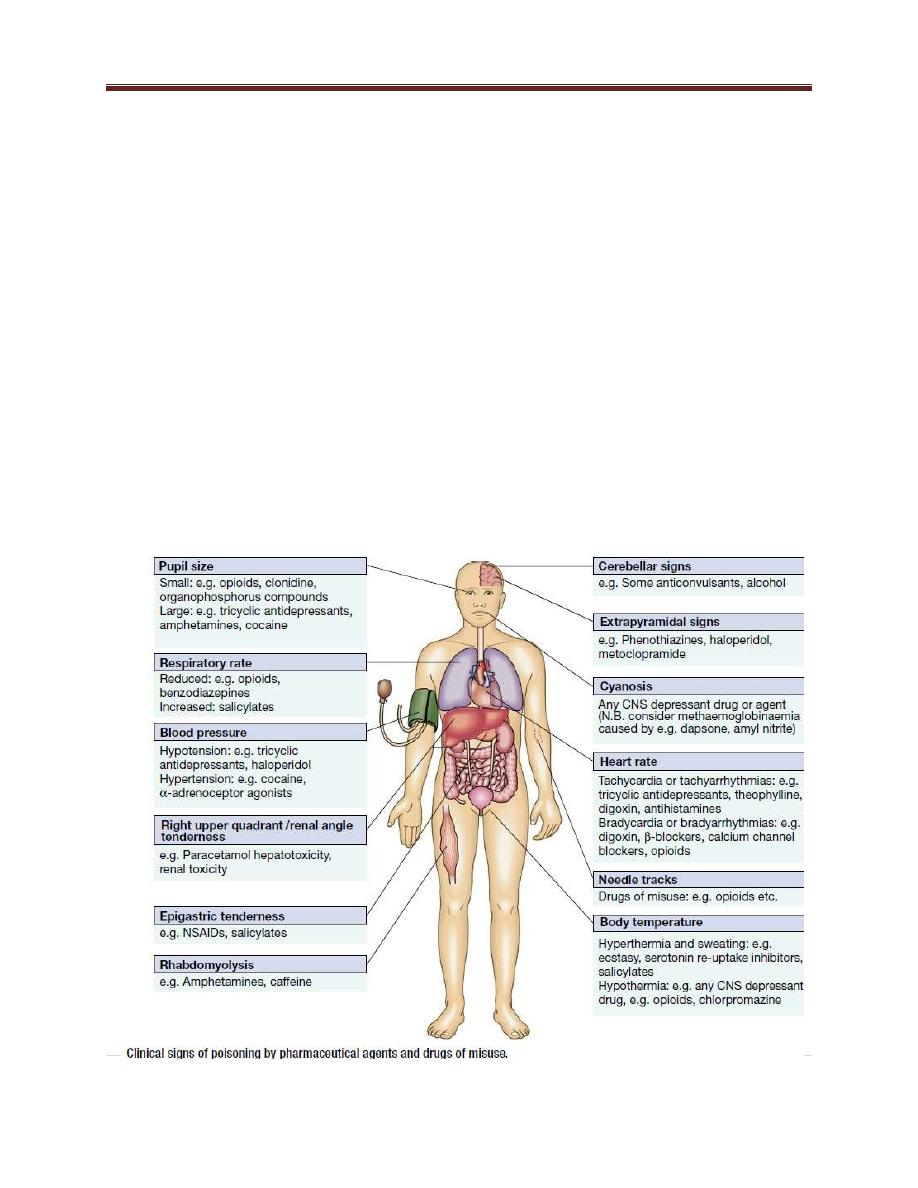
Clinical assessment and investigations
• The patient may have a cluster of clinical features ('toxidrome') suggestive of poisoning with a particular drug
type
• Poisoning is a common cause of coma, especially in younger people, but it is important to exclude other
potential causes.
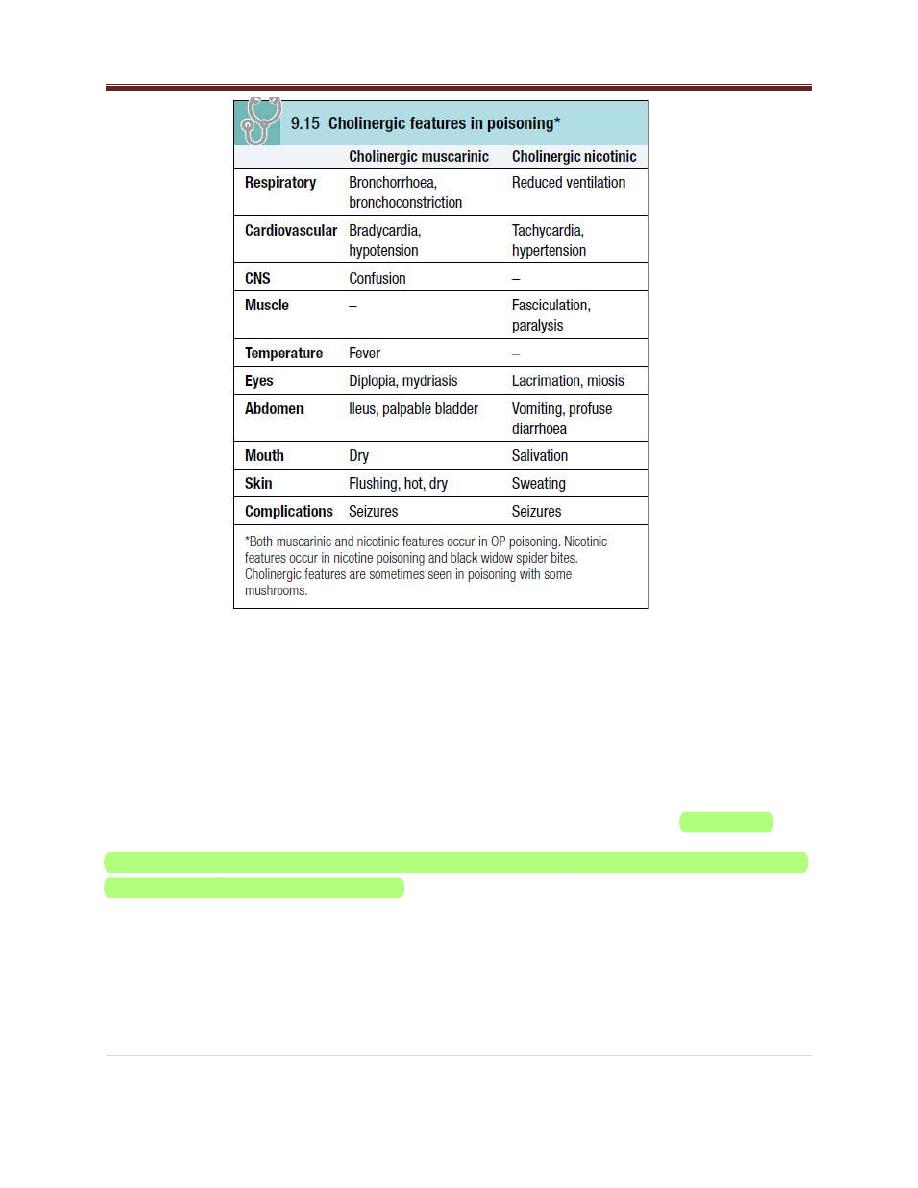
• Serotonin syndrome
• Anticholinergic
• Stimulant
• Sedative hypnotic
• Opioid
• Cholinergic muscarinic
• Cholinergic nicotinic
Psychiatric assessment
• Assess the risk of suicidal attempt
• The use or abuse of certain psychotropic materials
• Advice and treatment
Medicine Poisoning Dr. Haidar F. Abd
5 |
P a g e
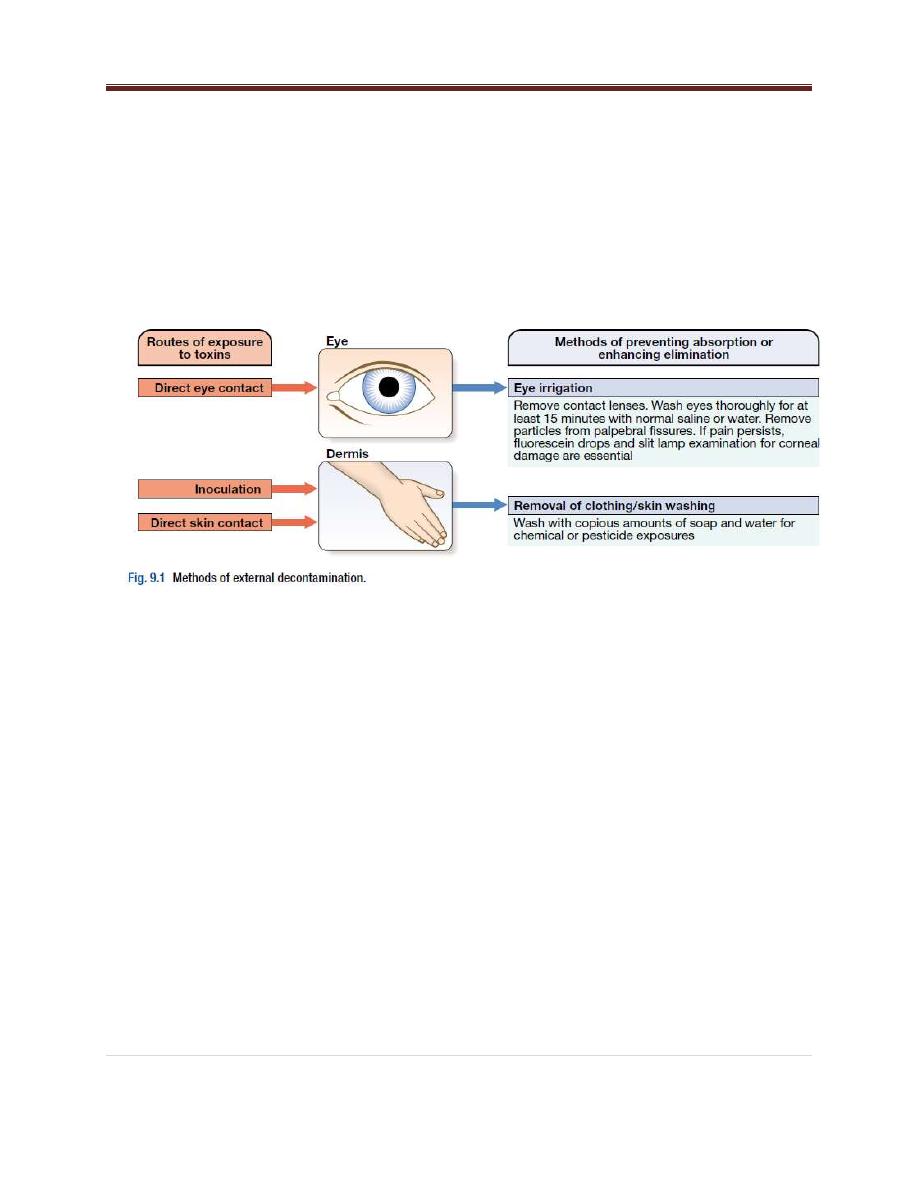
General management
• Patients presenting with eye or skin contamination should undergo appropriate local decontamination
procedures
• Gastrointestinal decontamination
• Patients who have ingested potentially life-threatening quantities of toxins may be considered for
gastrointestinal decontamination if poisoning has been recent.
• Induction of emesis using ipecacuanha is now never recommended.
Activated charcoal
• Given orally as slurry, activated charcoal absorbs toxins in the bowel as a result of its large surface area. If given
sufficiently early, it can prevent absorption of an important proportion of the ingested dose of toxin. However,
efficacy decreases with time and current guidelines do not advocate use more than 1 hour after overdose in most
circumstances
• However, use after a longer interval may be reasonable when a delayed-release preparation has been taken or
when gastric emptying may be delayed.
• Some toxins do not bind to activated charcoal so it will not affect their absorption.
• In patients with an impaired swallow or a reduced level of consciousness, the use of activated charcoal, even via a
nasogastric tube, carries a risk of aspiration pneumonitis.
• This risk can be reduced but not completely removed by protecting the airway with a cuffed endotracheal tube.
Substances poorly adsorbed by activated charcoal
medicines
Chemicals
1. Iron
2. Lithium
1. Acids*
2. Alkalis*
3. Ethanol
4. Ethylene glycol
5. Mercury
6. Methanol
7. Petroleum distillates*
* Gastric lavage contraindicated
Medicine Poisoning Dr. Haidar F. Abd
6 |
P a g e
Gastric aspiration and lavage
• Gastric aspiration and/or lavage is now very infrequently indicated in acute poisoning, as it is no more effective
than activated charcoal, and complications are common, especially aspiration. Use may be justified for life-
threatening overdoses of some substances that are not absorbed by activated charcoal
Whole bowel irrigation
• This is occasionally indicated to enhance the elimination of ingested packets or slow-release tablets that are not
absorbed by activated charcoal (e.g. iron, lithium), but use is controversial. It is performed by administration of
large quantities of polyethylene glycol and electrolyte solution (1-2 L/hr for an adult), often via a nasogastric
tube, until the rectal effluent is clear.
• Contraindications include inadequate airway protection, haemodynamic instability, gastrointestinal
haemorrhage, obstruction or ileus. Whole bowel irrigation does not cause osmotic changes but may
precipitate nausea and vomiting, abdominal pain and electrolyte disturbances.
Urinary alkalinisation
• Urinary excretion of weak acids and bases is affected by urinary pH, which changes the extent to which they are
ionised.
• Highly ionised molecules pass poorly through lipid membranes and therefore little tubular reabsorption occurs
and urinary excretion is increased.
• If the urine is alkalinised (pH > 7.5) by the administration of sodium bicarbonate (e.g. 1.5 L of 1.26% sodium
bicarbonate over 2 hrs), weak acids (e.g. salicylates, methotrexate and the herbicides 2,4-
dichlorophenoxyacetic acid and mecoprop) are highly ionised and so their urinary excretion is enhanced. This
technique should be distinguished from forced alkaline diuresis, in which large volumes of fluid with diuretic are
given in addition to alkalinisation.
• This is no longer used because of the risk of fluid overload.
• Urinary alkalinisation is currently recommended for patients with clinically significant salicylate poisoning when
the criteria for haemodialysis are not met (see below). It is also sometimes used for poisoning with
methotrexate. Complications include alkalaemia, hypokalaemia and occasionally alkalotic tetany (p. 444).
Hypocalcaemia is rare.

Medicine Poisoning Dr. Haidar F. Abd
7 |
P a g e
Haemodialysis and haemoperfusion
• These can enhance the elimination of poisons that have a small volume of distribution and a long half-life after
overdose, and are useful when the episode of poisoning is sufficiently severe to justify invasive elimination
methods.
• The toxin must be small enough to cross the dialysis membrane (haemodialysis) or must bind to activated
charcoal (haemoperfusion)
• Haemodialysis may also correct acid-base and metabolic disturbances associated with poisoning.
Poisons effectively eliminated by haemodialysis or
haemoperfusion
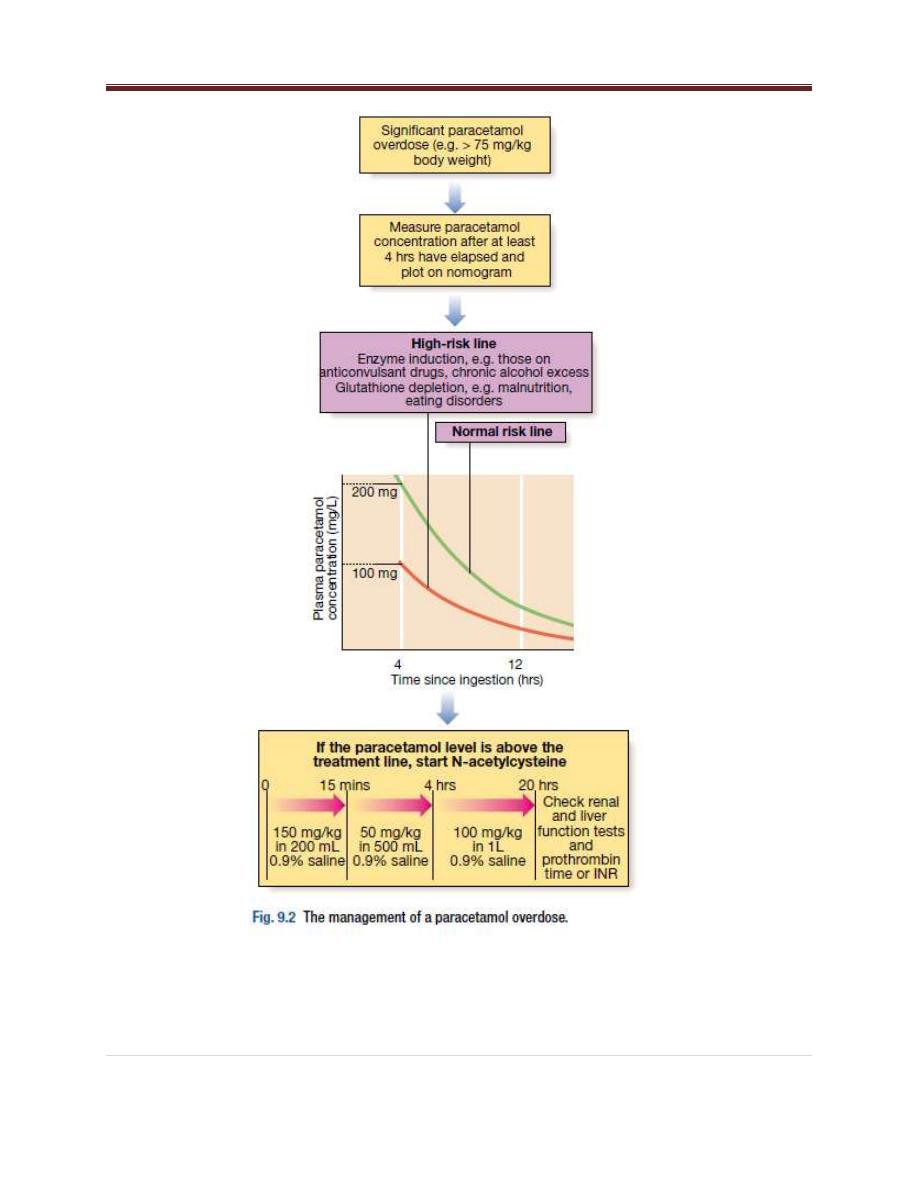
PARACETAMOL
• Paracetamol (acetaminophen) is the drug most commonly used in overdose in the UK.
• Toxicity results from formation of an intermediate reactive metabolite which binds
covalently to cellular proteins, causing cell death.
• This results in hepatic and occasionally renal failure.
• In therapeutic doses, the toxic intermediate metabolite is detoxified in reactions
requiring glutathione, but in overdose, glutathione reserves become exhausted.
Medicine Poisoning Dr. Haidar F. Abd
8 |
P a g e

Medicine Poisoning Dr. Haidar F. Abd
9 |
P a g e
Management
• Activated charcoal may be used in patients presenting within 1 hour.
• Antidotes for paracetamol act by replenishing hepatic glutathione. Acetylcysteine given
intravenously (or orally in some countries) is highly efficacious if administered within 8
hours of the overdose.
• However, since efficacy declines thereafter, administration should not be delayed in
patients presenting after 8 hours to await a paracetamol blood concentration result.
• The antidote can be stopped if the paracetamol concentration is shown to be below the
appropriate treatment line.
• The most important adverse effect of acetylcysteine is related to dose-related
histamine release, the 'anaphylactoid' reaction, which causes itching and urticaria, and
in severe cases, bronchospasm and hypotension.
• Most cases can be managed by temporary discontinuation of acetylcysteine and
administration of an antihistamine. An alternative antidote in paracetamol poisoning is
methionine 2.5 g orally 4-hourly to a total of four doses, but it is less effective, especially
after delayed presentation.
• If a patient presents more than 15 hours after ingestion, liver function tests,
prothrombin time (or international normalised ratio-INR), renal function tests and a
venous bicarbonate should be measured, the antidote started, and a poisons
information centre or local liver unit contacted for advice if results are abnormal.
• An arterial blood gas sample should be taken in patients with severe liver function
abnormalities; metabolic acidosis indicates severe poisoning.
• Liver transplantation should be considered in individuals who develop life-threatening
liver failure due to paracetamol poisoning
• If multiple ingestions of paracetamol have taken place over several hours or days (i.e. a
staggered overdose), acetylcysteine should be given when the paracetamol dose
exceeds 150 mg/kg body weight in any one 24-hour period or 75 mg/kg body weight in
'high-risk groups'

Medicine Poisoning Dr. Haidar F. Abd
10 |
P a g e
Salicylates (aspirin)
Clinical features
• Salicylate overdose commonly causes nausea, vomiting, sweating, tinnitus and deafness.
• Direct stimulation of the respiratory center produces hyperventilation and respiratory
alkalosis.
• Peripheral vasodilatation with bounding pulses and profuse sweating occurs in moderately
severe poisoning.
• Serious salicylate poisoning is associated with metabolic acidosis, hypoprothrombinaemia,
hyperglycaemia, hyperpyrexia, renal failure, pulmonary oedema, shock and cerebral
oedema.
• Agitation, confusion, coma and fits may occur, especially in children.
• Toxicity is enhanced by acidosis, which increases salicylate transfer across the blood-brain
barrier.
Management
• Activated charcoal should be administered if the patient presents early.
• Multiple doses of activated charcoal may enhance salicylate elimination but currently are
not routinely recommended.
• The plasma salicylate concentration should be measured at least 2 (in symptomatic
patients) or 4 hours (asymptomatic patients) after overdose and repeated in patients with
suspected serious poisoning, since concentrations may continue to rise some hours after
overdose.
• In adults, concentrations above 500 mg/L and 700 mg/L suggest serious and life-
threatening poisoning respectively, although clinical status is more important than the
salicylate concentration in assessing severity.
• Dehydration should be corrected carefully, as there is a risk of pulmonary oedema, and
metabolic acidosis should be identified and treated with intravenous sodium
Medicine Poisoning Dr. Haidar F. Abd
11 |
P a g e
bicarbonate (8.4%), once plasma potassium has been corrected. Urinary alkalinisation is
indicated for adult patients with salicylate concentrations above 500 mg/L.
• Haemodialysis is very effective at removing salicylate and correcting acid-base and fluid
balance abnormalities, and should be considered when serum concentrations are above
700 mg/L in adult patients with severe toxic features, or when there is renal failure,
pulmonary oedema, coma, convulsions or refractory acidosis.
Organophosphorus poisoning
Clinical features and management
OP poisoning causes an acute cholinergic phase, which may occasionally be followed by the
intermediate syndrome or organophosphate-induced delayed polyneuropathy (OPIDN). The
onset, severity and duration of poisoning depend on the route of exposure and agent involved.
Acute cholinergic syndrome
The acute cholinergic syndrome usually starts within a few minutes of exposure. Nicotinic or
muscarinic features may be present (Box 9.15). Vomiting and profuse diarrhoea are typical
following oral ingestion.
Bronchoconstriction, bronchorrhoea and salivation may cause severe respiratory compromise.
Miosis is characteristic and the presence of muscle fasciculations strongly suggests the
diagnosis, although this feature is often absent, even in serious poisoning. Subsequently, the
patient may develop generalised flaccid paralysis which can affect respiratory and ocular
muscles and result in respiratory failure. Ataxia, coma and convulsions may occur. In severe
poisoning, cardiac repolarization abnormalities and torsades de pointes may occur.
Other early complications of OP poisoning include extrapyramidal features, pancreatitis,
hepatic dysfunction and pyrexia.
Management
In the event of external contamination, further exposure should be prevented, contaminated
clothing and contact lenses removed, the skin washed with soap and water, and the eyes
irrigated. The airway should be cleared of excessive secretions and high-flow oxygen
administered.
Medicine Poisoning Dr. Haidar F. Abd
12 |
P a g e
Intravenous access should be obtained. Gastric lavage or activated charcoal may be considered
within 1 hour of ingestion. Convulsions should be treated as described in Box 9.11, p. 210. The
ECG, oxygen saturation, blood gases, temperature, urea and electrolytes, amylase and glucose
should be monitored closely.
Early use of sufficient doses of atropine is potentially life-saving in patients with severe toxicity.
Atropine reverses ACh-induced bronchospasm, bronchorrhoea bradycardia and hypotension.
When the diagnosis is uncertain, a marked increase in heart rate associated with skin flushing
after a 1 mg intravenous dose makes OP poisoning unlikely. In OP poisoning, atropine should be
administered in doses of 0.6–2 mg i.v., repeated every 10–25 mins until secretions are
controlled, the skin is dry and there is a sinus tachycardia. Large doses may be needed but
excessive doses may cause anticholinergic effects .
In patients requiring atropine, an oxime such as pralidoxime chloride (or obidoxime), if
available, should also be administered, as this may reverse or prevent muscle weakness,
convulsions or coma, especially if administered rapidly after exposure. The dose for an adult is 2
g i.v. over 4 mins, repeated 4–6-hourly. Oximes work by reactivating AChE that has not
undergone ‘ageing’ and are therefore less effective with dimethyl compounds and nerve
agents, especially soman. Oximes may provoke hypotension, especially if administered rapidly.
Ventilatory support should be instituted before the patient develops respiratory failure (p. 194).
Benzodiazepines may be used to reduce agitation and fasciculations, treat convulsions and
sedate patients during mechanical ventilation.
Exposure is confirmed by measurement of plasma (butyrylcholinesterase) or red blood cell
cholinesterase activity. These correlate poorly with the severity of clinical features, although
values are usually less than 10% in severe poisoning, 20–50% in moderate poisoning and > 50%
in subclinical poisoning.
The acute cholinergic phase usually lasts 48–72 hours, with most patients requiring intensive
cardiorespiratory support and monitoring.
to those of the head and neck, proximal limbs and the muscles of respiration, resulting in
ventilatory failure.
This ‘intermediate syndrome’ (IMS) generally develops quite rapidly between 1 and 4 days after
exposure, often after resolution of the acute cholinergic syndrome, and may last 2–3 weeks.
There is no specific treatment but supportive care, including maintenance of airway and
ventilation, is important.
Medicine Poisoning Dr. Haidar F. Abd
13 |
P a g e
Organophosphate-induced delayed polyneuropathy (OPIDN)
This is a rare complication that usually occurs 2–3 weeks after acute exposure. It is a mixed
sensory/motor polyneuropathy, especially affecting long myelinated neurons, and appears to
result from inhibition of enzymes other than AChE. It is a feature of poisoning with some OPs
(e.g. trichlorocresylphosphate), while others, including nerve agents, are not thought to have
this effect. Early clinical features are muscle cramps followed by numbness and paraesthesiae,
proceeding to flaccid paralysis of the lower and subsequently the upper limbs. Paralysis of
the lower limbs is associated with foot drop and a highstepping gait, progressing to paraplegia.
Paralysis of the arms leads to wrist drop. Sensory loss may also be present but is variable.
Initially, tendon reflexes are reduced or lost, but later mild spasticity may develop.
There is no specific therapy for OPIDN. Regular physiotherapy may limit deformity caused by
musclewasting.
Recovery is often incomplete and may be limited to the hands and feet, although substantial
functional recovery after 1–2 years may occur, especially in younger patients.
Medicine Poisoning Dr. Haidar F. Abd
14 |
P a g e
Naloxone ---------- opioid
Digoxin ------------- dg antibody
Benzodiazepine -------------
B- blocker -------------- isoprotenol
Warfarin -------------
vit. K
Heparin ----------------- protamine sulfate
Case ///
very import
. /// gardener had been insecticides ---- cholinergic effect ----
stimulation muscarinic receptor ------ increase salivation and lacrimation ---- air way
obstruction --- bradycardia .??
Q1// diagnosis ??
Organo phosphorus poisoning
Q2// main treatment ??
atropine
give frequent dose .
By:
براء محمد جاسم
المهمات
التي ذكرها الدكتور في المحاضرة
ـك
انت هذهـ
ر محاضرة . في مناهج الطب الباطني والمواد جميعاـخا
.
وهذه
... اخر محاضرة اقوم بطباعتها النتهاء منهج الطب المقرر
بعد خسمة سنوا
ت مضت والحمد
. هلل
Thanks' For all
I wish you the best
2015/5/7
