1
2015 – 2016
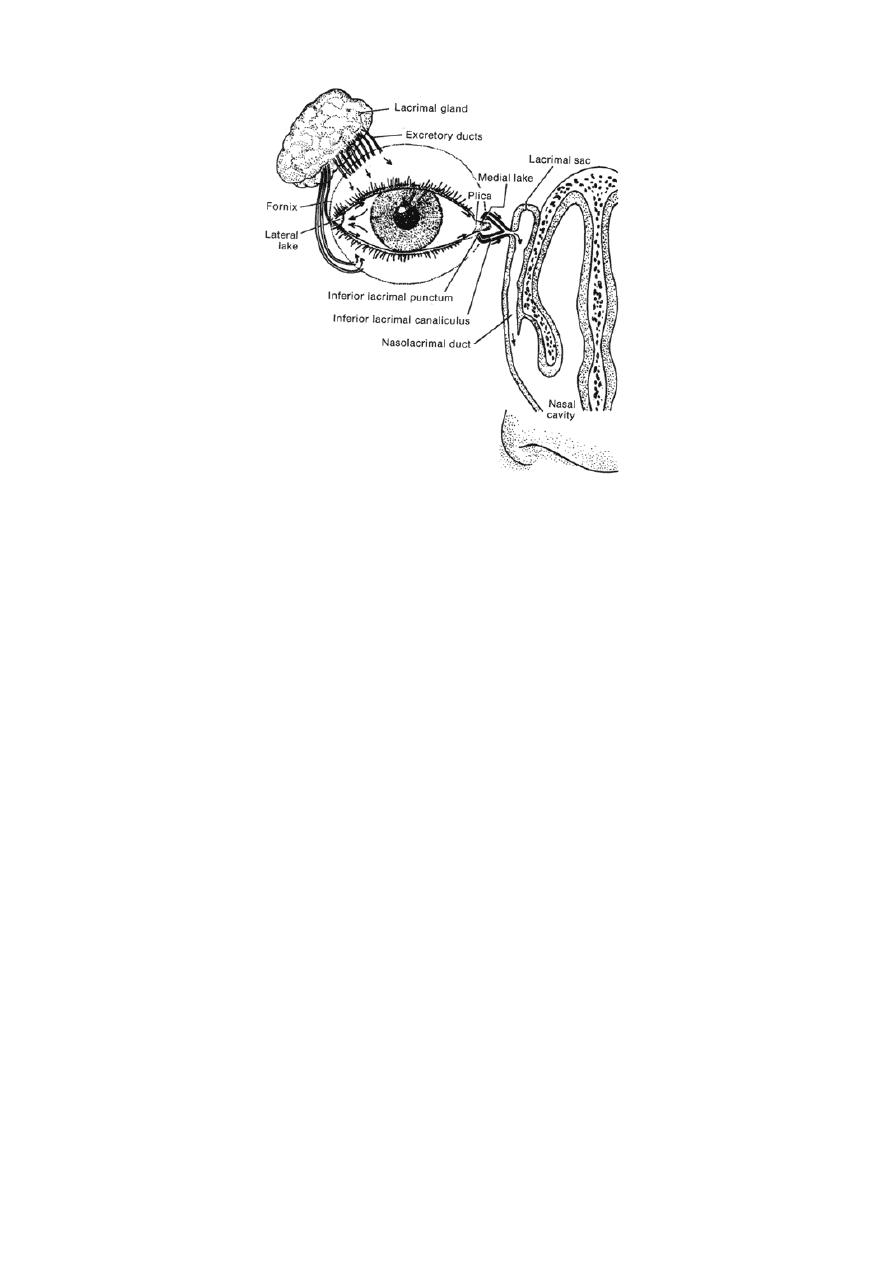
The lacrimal apparatus
The lacrimal system consists of:
1- Secretory portion: Comprises the following:
a- The lacrimal gland: Which is divided into palpebral (Aqueoussecretion)
(near the temporal aspect of upper eyelid) and orbital
(near the eyeball) lobes, and it is situated in the upper
temporal angle of the orbit.
b- Accessory lacrimal glands: glands of Krause and glands of wolfring.
c- Meibomian glands.
d- Glands of Zeis. (For oily secretion)
e- Sweat glands of Möll.
f- Goblet cells of conjunctiva.
g- Glands of Manz. (For mucin secretion)
h- Glands of Henle.
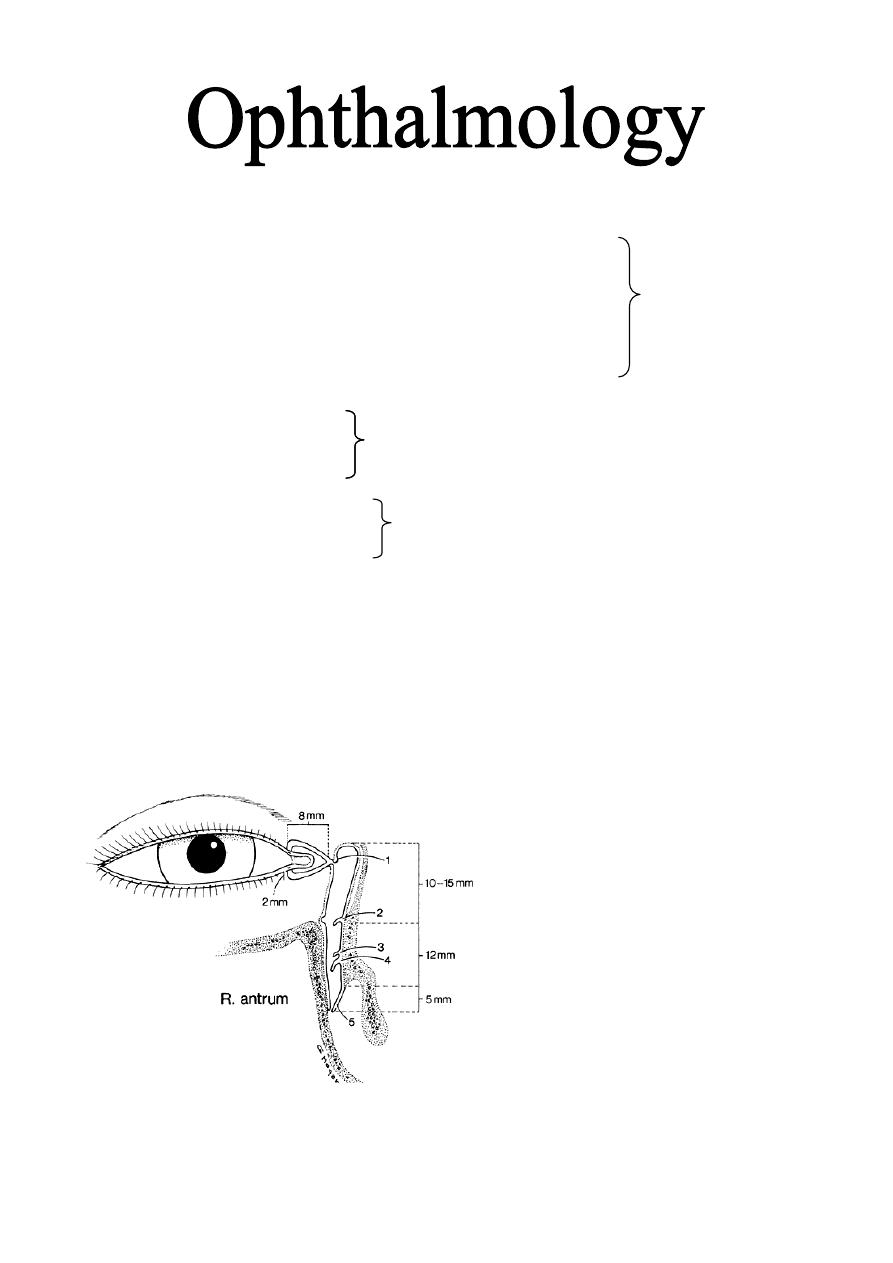
2- Drainage portion: Consists of:
a- Two puncti on the eyelid margins, one upper and one lower.
b- Vertical canaliculi (Ampullae): 2 mm in length.
c- Horizontal canaliculi: 8 mm.
d- The lacrimal sac: 10 mm long.
e- The nasolacrimal duct: 12 mm, ends into valve of Hasner in the inferior
meatous of the lateral nasal wall.
Dr. Najah
طب بغداد
Lecture: 14

2
The tear film
The pre-corneal tear film has three layers:
1- Superficial oily layer: Its main advantage is to prevent evaporation.
2- Middle aqueous layer: the thickest layer. Its functions mention below.*
3- Inner mucin layer: Immediately adjacent to cornea: it covered corneal
surface and converted it from hydrophobic into hydrophilic so the aqueous
layer adherent to it.
Functions of tear:*
1- Forms and maintains a smooth refracting surface over the cornea.
2- Maintains a moist environment for the conjunctival and corneal epithelium,
as dryness of the cornea and conjunctiva causes sloughing of their epithelium
and it may ends with corneal ulcer.
3- Bactericidal properties, as it has lysozymes and Igs (IgA).
4- Lubricates the lids.
5- Transports metabolic products (especially CO2 & O2) for cornea as it is an
avascular structure, so the tear film transports these nutrients from the
atmosphere to the cornea and vice versa.
6- Provides a pathway for WBCs in case of injury (enhances the migration of
WBCs).
7- Dilutes and washes away noxious stimuli.
Physiology of tear:
1- Tear flow along the upper and lower marginal stripe and enter the upper and
lower canaliculi by capillarity (capillary action) and suction. 70% of tear pass
through the lower punctum and 30% through the upper punctum because of
gravity.
2- With each blink, there is contraction of palpebral part of orbicularis oculi
that compress the ampullae, shorten the horizontal canaliculi. Contraction of
lacrimalis part of orbicularis oculi cause expansion of lacrimal sac so that
creating negative pressure, which sucks the tear in to sac.
3- When the eyes are open, the muscle relax so the sac collapses and a positive
pressure is created which forces the tears down into the nose (plus the gravity
effect).
Causes of excessive watering:
1- Lacrimation:
Caused by reflex over-production of tear from stimulation of the
ophthalmic branch of the trigeminal nerve by irritation of the cornea and
conjunctiva, and it is initiated also due to emotional stimulation. Lacrimation
is usually associated with symptoms of underlying cause and treatment is
usually medical (e.g. conjunctivitis, keratitis, and ect).

3
2- Epiphora (Obstructive epiphora):
Caused by mechanical obstruction of tear drainage, it is characterized by
excessive watering which is exacerbated by a cold atmosphere and is least in a
warm dry atmosphere (due to evaporation). Treatment in most cases is by
surgery.
3- Lacrimal pump failure:
There is no reflex over-production, and no mechanical obstruction, but
occurs secondary to lower lid laxity (aging) and weakness of orbicularis oculi
muscle (e.g. facial nerve palsy).
Treatment: is also surgical but more difficult than obstructive epiphora.
`
Diseases of lacrimal glands
1- Acute dacryoadenitis:
Is an uncommon inflammation of the lacrimal gland that usually
accompanies systemic diseases, e.g. mumps and infectious mononucleosis
(IMN).
Purulent infection may be secondary to extension of inflammation from the
eyelids or the conjunctiva.
Signs and symptoms:
a- Pain and discomfort in the upper outer position of the orbit.
b- Mechanical blepharoptosis due to lid swelling.
c- Eversion of the upper eyelid indicates a swollen and reddened gland.
Treatment:
Usually self-limited, but we use antibiotics if there is purulent discharge.
2- Chronic dacryoadenitis:
Is a proliferative inflammation of the lacrimal gland that occurs in a variety
of disorders; sarcoidosis, sjögren's syndrome, leukaemia, lymphoma,
amyloidosis, TB, syphilis and foreign body granuloma.
Signs and symptoms:
a- Painless enlargement of the lacrimal gland.
b- Eversion of the upper lid shows enlargement of the gland, but there is no
congestion.
Treatment: Directed towards the cause.
Diseases of the lacrimal passages
Dacryocystitis: Is an acute or chronic inflammation of the lacrimal sac. The
cause is obstruction of the lacrimal sac or nasolacrimal duct followed by
microbial infection.

4
1- Acute dacryocystitis:
Is a suppurative inflammation of the lacrimal sac associated with cellulitis of
the overlying tissues (tissues medial to the medial canthus).
Signs and symptoms:
Acute onset of painful swelling, tenderness overlying the lacrimal sac
combined with widespread cellulitis and associated constitutional symptoms.
Treatment:
- Local hot compresses and systemic antibiotics.
- Incision and drainage if there is abscess formation (incision and drainage
may end with fistula formation, so avoiding this procedure is a must unless
there is large abscess which is not responded to antibiotics).
2- Chronic dacryocystitis:
Occurs due to obstruction of nasolacrimal duct and it is seen most frequently
in middle life.
Signs and symptoms:
- Epiphora which may be associated with a chronic or recurrent conjunctivitis
(due to stagnation of tears in the lacrimal gland).
- Painless swelling at the inner canthus.
- In some cases a swelling is absent although pressure over the sac results in
reflux of mucopurulent material through the canaliculi.
Treatment: Dacryocystorhinostomy (DCR).
DCR can be done by three surgical ways:
1- External Traditional DCR:
A 15-30 mm incision is made on the side of the nose and some bone is removed to
make a connection between the lacrimal sac and middle meatous of the nose. Tubes
are left behind to prevent the fistula from becoming closed and are removed after a
few months.
2- Endoscopic Endonasal DCR:
The operation can also be performed endoscopically through the nose where an
opening is fashioned in the lacrimal sac from within the nose. The advantages include
lesser peri-operative morbidity, and no scar. Data suggests a slightly lower success
rate than the "traditional" technique.
With the advent of nasal endoscopes, endoscopic dacryocystorhinostomy is becoming
popular. In this procedure, a nasal endoscope is used to visualise the lacrimal sac
through the nasal cavity. The bone covering the lacrimal sac is nibbled out. The
medial wall of the sac is incised or excised, facilitating drainage of tears into the
nasal cavity. This procedure avoids scarring.

5
3- Endoscopic Laser DCR:
Endoscopic laser dacryocystorhinostomy (DCR) enables an obstructed lacrimal sac to
be opened through an intranasal approach, avoiding the need for a skin incision. The
holmium:yttrium aluminum garnet (holmium:YAG) or diode laser is well-suited for
this procedure because of its properties of fiberoptic delivery, effective bone cutting,
and precise soft-tissue coagulation. Endoscopic laser DCR appears to be a safe and
effective procedure which should be considered as an alternative to external DCR for
the surgical treatment of nasolacrimal duct obstruction. The success rate is less than
above 2 procedures because of the smaller bone ostium which can be formed.
Lacrimal drainage obstruction
1- Punctal stenosis (with epiphora):
Causes:
a- Idiopathic: usually in elderly people (the most common cause).
b- Herpes simplex lid infection.
c- Irritation.
d- Trachoma.
e-Cicatricial conjunctivitis.
Treatment:
Initial treatment: Dilatation by special probe.
2- Canalicular obstruction:
Causes:
a- Idiopathic fibrosis (most common).
b- Chronic dacryocystitis.
c- Herpes simplex lid infection.
d- Cicatricial conjunctivitis.
e- Systemic use of 5-fluorourcil.
Treatment:
Partial obstruction: Intubation of the canalicular for six months.
Complete obstruction: DCR or CDCR (Conjunctival DCR), insertion of luster
jones tube from conjunctival sac to the lacrimal sac with DCR.
3- Acquired nasolacrimal obstruction:
Causes:
a- idiopathic stenosis (most common cause).
b- Naso-orbital trauma.
c- Irradiation.
d- Wegener's granulomatosis.
e- Nasopharyngeal tumor.
Treatment: DCR.
6
4- Congenital nasolacrimal duct obstruction:
At birth, the lower end of the nasolacrimal duct (NLD) is frequently non-
canalized (near the valve of hasner), but this is of no clinical significance in
most neonates because it canalizes spontaneously soon after birth. Sometime,
the occlusion is continues and result in:
Signs:
a- Epiphora.
b- Gentle pressure of the lacrimal sac causes reflex of purulent material from
the puncti.
c- occasionally, acute dacryocystitis might result.
Differential diagnosis of watery eye (lacrimation and epiphora) in neonates:
a- congenital drainage system obstruction.
b- Ophthalmia neonatorum. (neonatal conjunctivitis)
c- Congenital glaucoma. (very important to be remember)
Treatment:
a- Massage: of the NLD, so increase the hydrostatic pressure and thereby
ruptures the membranous obstruction. This is done as ten strokes applied four
times daily.
b- Probing: overcomes the obstructive membrane at Hasner's valve. It should
not be performed until the age of 12-18 months because spontaneous
canalization occurs in about 95% of cases.
Postoperative antibiotic and steroid drops are used four times daily for one
week, if after six weeks there is no improvement, the probing should be
repeated.
90% are cured by the first trial of probing and further 6% by the second.
Failure of surgery is due to congenital alteration of NLD anatomy or
congenitally absent.
Cases with persistent symptoms in spite of two satisfactory probing can be
treated by DCR at preschool age.
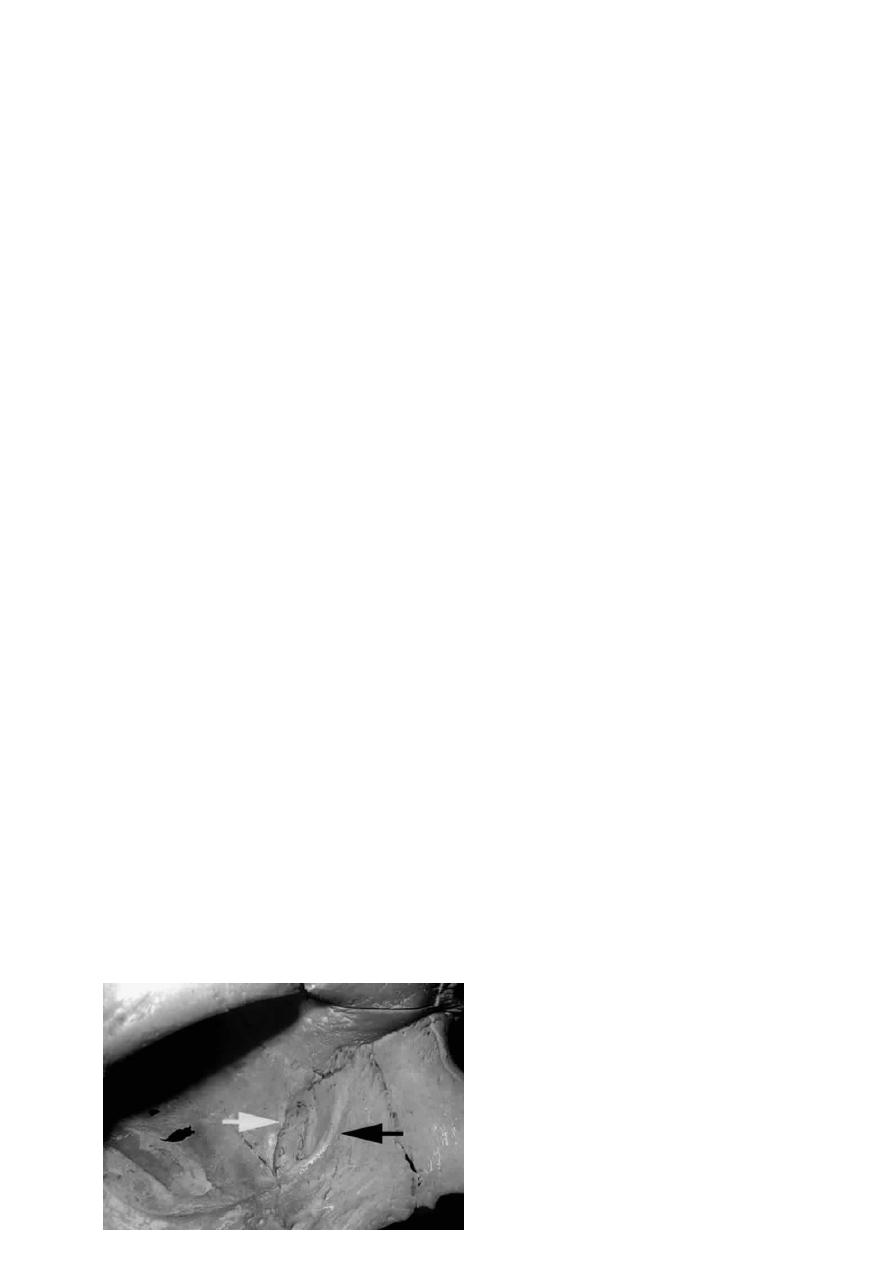
The black arrow points to
anterior crest of the lacrimal fossa,
this crest is part of frontal process of
the maxillary bone which forms the
anterior part of this fossa, while the
white arrow points to the posterior
7
crest which is a part of the lacrimal bone. The posterior part of the lacrimal
fossa is formed by the lacrimal bone, and between the maxillary and lacrimal
bones there is the maxillary-lacrimal suture.
Dry eye (Keratoconjunctivitis Sicca "KCS"):
Absent or reduced tears cause keratinization of corneal and conjunctival
epithelium and possibly marked corneal scarring and opacification, usually both
eyes are affected.
Symptoms:
- Burning sensation.
- Feeling of dryness (the patient himself told you that his eyes are dry).
- Continuous foreign body sensation.
- Mucus discharge (as the aqueous part is affected).
- Transient blurring and vision (as it Forms and maintains a smooth refracting
surface over the cornea).
- Itching.
- Photophobia.
Causes of dry eyes:
1- Atrophy and fibrosis of lacrimal gland tissue as a result of a destructive
infiltration by mononuclear cells, usually associated with systemic diseases.
a- Pure KCS: Involving lacrimal gland alone (dry eye only and nothing else).
b- Primary sjögren's syndrome: Dry eye associated with dry mouth.
c- Secondary sjögren's syndrome: dry eye and mouth associated with
systemic disease, most common one is rheumatoid arthritis, and other
diseases are SLE, systemic sclerosis, hashimoto thyroiditis and primary
biliary cirrhosis.
2- Miscellaneous causes:
a- Destruction of lacrimal tissue by tumors, sarcoidosis.
b- Meibomian gland dysfunction.
c- Absence of lacrimal gland which is either congenital or due to surgical
removal (due to involvement by tumor).
d- Blockage of the excretory ductules (due to burns, drugs, diseases …etc,
that cause blockage of these excretory ducts. Excretory ducts are about six
ducts open in the supero-lateral part of conjunctival fornix and 2 ducts open at
the infero-lateral part of conjunctival fornix). This blockage duo to severe
conjunctival scarring.
8
Treatment of dry eye:
Supplementation of tears with the use of tear substitutes is the mainstay of therapy
for dry eyes. A variety of tear substitutes are available. The preservatives found in
artificial tears can be toxic to the ocular surface, so the introduction of preservative-
free artificial tears has provided a major improvement in treatment. These products
contain electrolytes and buffering agents and are usually either isotonic or slightly
hypotonic. Recently, several formulations have been introduced that have
“transiently preserved” agents. These preservatives are inactivated on contact with
the tear film.
Because of their duration in the conjunctival sac, ointments or gels as a lubricating
agent can be very useful. Sustained-release inserts and gels. And there are other
measures that are not used routinely.
From all these wide varieties of tear substitutes eye drops and gels, the
patient can choice one which is most appropriate to relief the symptoms by a
method of trials and errors.



