
AFTER MID
TOTAL LEC: 12
Dermatology
Bacterial Skin Infections
DR. BASMAN LEC: 3
Dr. Basman


Bacterial skin infections
Overview over bacterial skin infections
The skin provides a remarkably good barrier against bacterial infections. Although many
bacteria come in contact with or reside on the skin, they are normally unable to establish an
infection. When bacterial skin infections do occur, they can range in size from a tiny spot to
the entire body surface.
Many types of bacteria can infect the skin. The most common
are Staphylococcus and Streptococcus. Skin infections caused by less common bacteria may
develop in people while hospitalized or living in a nursing home.
Some people are at particular risk of developing skin infections. For example, people with
diabetes are likely to have poor blood flow, especially to the hands and feet, and the high
levels of sugar (glucose) in their blood decrease the ability of white blood cells to fight
infections. People who are older, who have human immunodeficiency virus (HIV) or AIDS or
other immune disorders, or hepatitis, and who are undergoing chemotherapy or treatment
with other drugs that suppress the immune system are at higher risk as well because they
have a weakened immune system. Skin that is inflamed or damaged by sunburn, scratching,
or other trauma is more likely to become infected. In fact, any break in the skin predisposes a
person to infection.
Prevention involves keeping the skin undamaged and clean. When the skin is cut or
scraped, the injury should be washed with soap and water and covered with a sterile
bandage. Petrolatum may be applied to open areas to keep the tissue moist and to try to
prevent bacterial invasion. Doctors recommend that people do not use antibiotic ointments
(prescription or nonprescription) on uninfected minor wounds because of the risk of
developing an allergy to the antibiotic.
Most common bacterial skin infections
Folliculitis:
Folliculitis is an infection of a hair follicle. It looks like a tiny red or white pimple at the base of
a hair. There may be only one infected follicle or many. Each infected follicle is itchy or slightly
painful, but the person otherwise does not feel sick. Its usually caused by staphy or strept ..
but can be caused also by gram negative rods like pseudomonas.
Treatment by topical antibiotics like tetracycline , gentamycin or fucidic acid.
!
Skin abscesses:
Skin abscesses are warm, painful, pus-filled pockets of infection below the skin surface that
may occur on any body surface. Abscesses may be one to several inches in diameter. By
staph ,strept and gram negative rods.
Treatment needs surgical drainage along with systemic and topical antibiotics.
Furuncles
(boils) are tender, smaller, more superficial abscesses that by definition involve a hair follicle
and the surrounding tissue. Furuncles are common on the neck, breasts, face, and buttocks.
They are uncomfortable and may be painful when closely attached to underlying structures
(for example, on the nose, ear, or fingers). Usually by staph or strept.
Carbuncles
are multiple furuncles that are connected to one another below the skin surface. If not
treated, abscesses often come to a head and rupture, discharging a creamy white or pink
fluid. Bacteria may spread from the abscess to infect the surrounding tissue and lymph
nodes. The person may have a fever and feel generally sick.
The conditions usually caused by staph and commomly around the neck . more common in
diabetic and debilitated patients.
Treatment require surgical debridment and heavy systemic antibiotic therapy
!
Cellulitis
is a spreading bacterial infection of the skin and the tissues immediately beneath the skin.
Cellulitis may be caused by many different bacteria. The most common are those of
the Streptococcusand Staphylococcus species. Streptococci spread rapidly in the skin
because they produce enzymes that hinder the ability of the tissue to confine the infection.
Cellulitis that is caused by Staphylococcusbacteria usually occurs in open wounds and pus-
filled pockets (abscesses). Many other bacteria can cause cellulitis. Recently, a strain
of Staphylococcus that is resistant to previously effective antibiotics has become a more
common cause. This strain is called methicillin-resistant Staphylococcus aureus(MRSA).
Bacteria usually enter through small breaks in the skin that result from scrapes, punctures,
surgery, burns, fungal infections (such as athlete's foot), and skin disorders. Areas of the skin
that become swollen with fluid (edema) are especially vulnerable. However, cellulitis can also
occur in skin that is not obviously injured.
Symptoms
Cellulitis most commonly develops on the legs but may occur anywhere. Cellulitis usually
only affects one side, such as one hand or one leg. The first symptoms are redness, pain, and
tenderness over an area of skin. These symptoms are caused both by the bacteria
themselves and by the body's attempts to fight the infection. The infected skin becomes hot
and swollen and may look slightly pitted, like an orange peel. Fluid-filled blisters, which may
be small (vesicles) or large (bullae), sometimes appear on the infected skin. The borders of
the affected area are not distinct.
Most people with cellulitis feel only mildly ill, but some may have a fever, chills, rapid heart
rate, headache, low blood pressure, and confusion.
As the infection spreads, nearby lymph nodes may become enlarged and tender
(lymphadenitis) and the lymphatic vessels may become inflamed (lymphangitis)
Diagnosis
A doctor usually diagnoses cellulitis based on its appearance and symptoms. Laboratory
identification of the bacteria from skin, blood, pus, or tissue specimens (called a culture)
usually is not necessary unless a person is seriously ill or has a weakened immune system or
the infection is not responding to drug therapy.

Prognosis
Most cellulitis resolves quickly with antibiotic therapy. Occasionally, people develop
abscesses. Serious but rare complications include severe skin infections that rapidly destroy
tissue (called necrotizing skin infections) and spread of bacteria through the blood
(bacteremia). When cellulitis affects the same site repeatedly, especially the leg, lymphatic
vessels may be damaged, causing permanent swelling of the affected tissue.
Treatment
Prompt treatment with antibiotics can prevent the infection from spreading rapidly and
reaching the blood and internal organs. Antibiotics that are effective against both streptococci
and staphylococci (such as dicloxacillin or cephalexin If doctors suspect methicillin-
resistant Staphylococcus aureus infection, treatment may include antibiotics such
as trimethoprim or doxycycline
)
Also, the affected part of the body is kept immobile and elevated to help reduce swelling.
Cool, wet dressings applied to the infected area may relieve discomfort. Disorders that
increase risk of developing cellulitis in the future (for example, athlete's foot) are treated.
Symptoms of cellulitis usually disappear after a few days of antibiotic therapy. Abscesses are
cut open and drained.
Erysipelas
is a superficial form of cellulitis typically caused by streptococci.
Erysipelas causes a shiny, painful, red, raised patch on the skin. The edges have
distinct borders and do not blend into the nearby normal skin. The patch feels warm
and firm to the touch. It occurs most frequently on the legs and face. People often
have a high fever, chills, and a general feeling of illness (malaise).
Doctors base the diagnosis on the characteristic appearance of the rash.
Antibiotics given by mouth, such as penicillin, can cure the infection. For a severe
infection, intravenous penicillin is needed. Cold packs and drugs for pain may relieve
discomfort. Fungal foot infections may be an entry site for infection and may require
treatment with antifungal drugs to prevent recurrence.
Impetigo
is a skin infection, caused by Staphylococcus aureus, Streptococcus pyogenes, or both,
that leads to the formation of scabby, yellow-crusted sores and, sometimes, small blisters
filled with yellow fluid.
Impetigo is common. It affects mostly children. Impetigo can occur anywhere on the body
but most commonly occurs on the face, arms, and legs. The blisters that may form (bullous
impetigo) vary in size and can last for days to weeks. Impetigo often affects normal skin but
may follow an injury or a condition that causes a break in the skin, such as a fungal infection,
sunburn, or an insect bite. Poor hygiene and a moist environment are also risk factors. Some
people have staphylococci or streptococci bacteria living in their nose without causing
disease (they are considered nasal carriers). These nasal bacteria may cause repeat
infection in the person and sometimes in others.
Impetigo is itchy and slightly painful. The itching often leads to extensive scratching,
particularly in children, which serves to spread the infection. Impetigo is very contagious—
both to other areas of the person's own skin and to other people. Impetigo typically causes
clusters of tiny blisters that rupture and develop a honey-colored crust over the sores. Bullous
impetigo is similar except that the sores typically enlarge rapidly to form larger blisters. The
blisters burst and expose larger bases, which become covered with honey-colored varnish or
crust.
Doctors base the diagnosis on the appearance of the rash. In people who have repeated
infections, a swab of the nose is taken and sent to the laboratory to determine whether they
are a nasal carrier of staphylococci or streptococci.
The infected area should be washed gently with soap and water several times a day to
remove any crusts. Small areas are treated with antibiotic ointments or creams applied
directly to the skin (topically). If large areas are involved or are not cured with topical
antibiotics, an antibiotic taken by mouth may be needed. People who are nasal carriers are
treated with topical antibiotics applied to the nasal passages.
!

Lymphangitis
is infection of one or more lymphatic vessels, usually caused by streptococci.
Streptococci bacteria usually enter the lymphatic vessels from a scrape or wound in an
arm or a leg. Often, a streptococcal infection in the skin and the tissues just beneath the skin
(cellulitis) spreads to the lymph vessels. Occasionally, staphylococci or other bacteria are the
cause.
Red, irregular, warm, tender streaks develop on the skin in the affected arm or leg. The
streaks usually stretch from the infected area toward a group of lymph nodes, such as those
in the groin or armpit. The lymph nodes become enlarged and feel tender.
Common symptoms include a fever, shaking chills, a rapid heart rate, and a headache.
Sometimes these symptoms occur before the red streaks appear.
The diagnosis of lymphangitis is based on its typical appearance. A blood test usually
shows that the number of white blood cells has increased to fight the infection.
Most people recover quickly with antibiotics that kill staphylococci and streptococci, such
asdicloxacillin oxacillin
.
Staphylococcal scalded skin syndrome
is a reaction to a staphylococcal skin infection in which the skin blisters and peels off as
though burned.
Certain types of staphylococci bacteria secrete toxic substances that cause the top layer of
the epidermis to split from the rest of the skin. Because the toxin spreads throughout the
body, staphylococcal infection of a small area of skin may result in peeling over the entire
body. Staphylococcal scalded skin syndrome occurs almost exclusively in infants and children
under the age of 6.
Symptoms
Symptoms begin with an isolated, crusted sore that may look like impetigo . In
newborns, the infection may appear in the diaper area or around the stump of the umbilical
cord. In older children, the face is the typical site of infection. In adults, the infection may
begin anywhere. In all people with this disorder, the skin around the crusted sore becomes
scarlet in color within 24 hours. These areas are painful. The skin may be extremely tender
and have a wrinkled tissue paper–like consistency. Then, other large areas of skin distant
from the initial infection, frequently areas of friction, such as skinfolds, and on the buttocks,
hands, and feet, redden and develop blisters that break easily.
The top layer of the skin then begins peeling off, often in large sheets, with even slight
touching or gentle pushing. The peeled areas look scalded. Within 2 to 3 days, the entire skin
surface may be involved, and the person becomes very ill with a fever, chills, and weakness.
Diagnosis
A diagnosis is made by the appearance of skin peeling after an apparent staphylococcal
infection. If no signs of staphylococcal infection are observed, doctors often do a biopsy, in
which a small piece of skin is removed and sent to the laboratory to be tested.
prognosis and Treatment
With prompt diagnosis and treatment, staphylococcal scalded skin syndrome rarely causes
death. The topmost layer of the skin is quickly replaced, and healing usually occurs within 5 to
7 days after start of treatment.
Treatment is with antibiotics given by vein and later by mouth. Doctors give people who have
a widespread infection and oozing sores the same treatment they give to people who have
been burned . Skin moisturizers (emollients) may be used to help protect the skin after it has
healed.
Erythrasma
is infection of the top layers of the skin caused by the bacterium Corynebacterium
minutissimum.
Erythrasma affects mostly adults, especially those with diabetes and those living in the
tropics. Erythrasma is most common in the foot, where it causes scaling, cracking, and
breakdown of the skin between the 4th and 5th toes. This infection is also common in the
groin, where it causes irregularly shaped pink or brown patches and fine scaling especially
where the thighs touch the scrotum (in men). The armpits, skinfolds under the breasts or on
the abdomen, and the area between the vaginal opening and the anus (perineum) are prone
to this infection, particularly among people with diabetes and among obese middle-aged
women. In some people, the infection spreads to the torso and anal area.
.An antibiotic given by mouth, such as erythromycin or tetracycline
can eliminate the infection. Antibacterial soaps, such as chlorhexidine, may also help. Drugs
applied directly to the affected area (topically), such as erythromycin.
Mycobacterial skin infections
Cutaneous tuberculosis
Cutaneous tuberculosis (TB) is essentially an invasion of the skin by
Mycobacterium tuberculosis, the same bacteria that cause TB of the lungs
(pulmonary TB). Cutaneous TB is a relatively uncommon form of extrapulmonary
TB (TB infection of other organs and tissues).
THE DIAGNOSIS IS USUALLY MADE OR CONFIRMED BY
ARE EPITHELIOID GRANULOMAS WITH OR WITHOUT CASEATION.
Treatment
Patients with pulmonary or extrapulmonary TB disease need to be treated with
antitubercular drugs. This usually involves a combination of antibiotics
(isoniazid,
, pyrazinamide and ethambutol) given over a period of
several months and sometimes years.
Occasionally surgical excision of localised cutaneous TB is recommended.
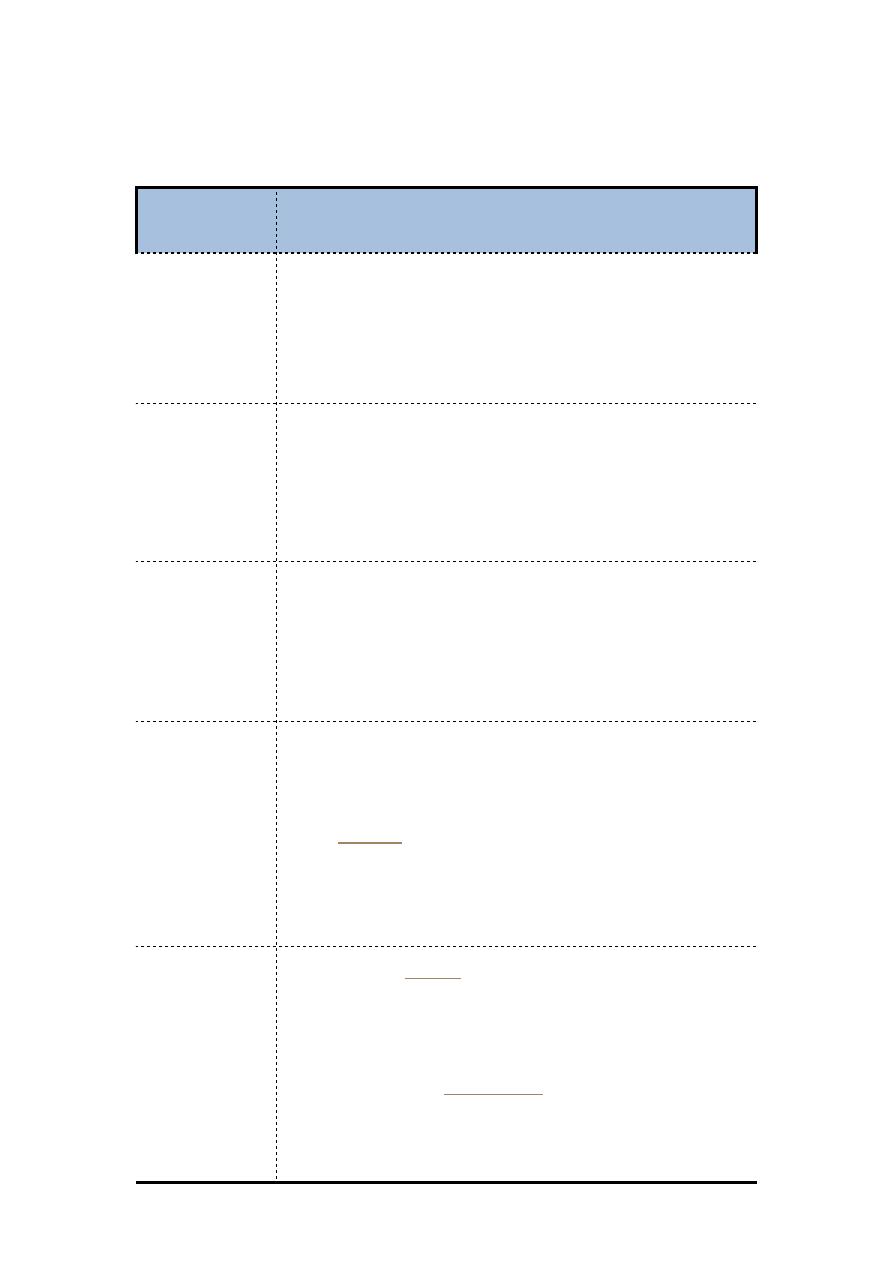
Types of cutaneous TB
Types of
cutaneous TB
Features
TB verrucosa cutis
♣
Occurs after direct inoculation of TB into the skin in someone who
previously
♣
infected with mycobacteria
♣
Presents as a purplish or brownish-red warty growth
♣
Lesions most often occur on the knees, elbows, hands, feet and buttocks
♣
Lesions may persist for years but can clear up even without treatment
Lupus vulgaris
♣
Persistent and progressive form of cutaneous TB
♣
Small sharply defined reddish-brown lesions with a gelatinous
consistency
♣
(called apple-jelly nodules)
♣
Lesions persist for years, leading to disfigurement and sometimes skin
cancer
Scrofuloderma
♣
Skin lesions result from direct extension of underlying TB infection of
lymph nodes, bone or joints
♣
Often associated with TB of the lungs
♣
Firm, painless lesions that eventually ulcerate with a granular base
♣
May heal even without treatment but this takes years and leaves
unsightly scars
Miliary TB
♣
Chronic TB infection that has spread from the primary infection (usually
in the lungs) to other organs and tissues via the bloodstream
♣
Skin lesions are small (millet-sized) red spots that develop into ulcers
and
♣
♣
More likely in immunocompromised patients, eg HIV, AIDS, cancer
♣
The patient is generally sick
♣
Prognosis is poor (many patients die even if diagnosed and treated)
Tuberculoid
♣
Generalised
in patients with moderate or high degree of
immunity to TB because of previous infection
♣
Usually in good health with no identifiable focus of active TB in skin or
elsewhere
♣
Erythema induratum (Bazin disease) presents as recurring nodules or
lumps on the back of the legs (mostly women) that may ulcerate and
scar. It is a type of
♣
Papulonecrotic tuberculid results in crops of recurrent crusted skin
papules on knees, elbows, buttocks or lower trunk that heal with scarring
after about 6 weeks.



