Myocarditis
Acute inflammatory condition that can have an infectious, toxic or autoimmune etiology.Viral infections are the most common causes, such as Coxsackie and influenza A and B viruses.
Myocarditis may occur several weeks after the initial viral symptoms and susceptibility is increased by corticosteroid treatment , immunosuppression, radiation, previous myocardial damage and exercise.
The clinical picture ranges from a symptomless disorder , sometimes recognized by the presence of an inappropriate tachycardia or abnormal ECG, to fulminant heart failure.
Myocarditis may be heralded by an influenza like illness.
Diagnosis
- ECG changes are common but non-specific .
- Biochemical markers of myocardial injury (e.g. troponin I and T, creatine kinase) are elevated.
- Echocardiography may reveal left ventricular dysfunction , and if the diagnosis is uncertain it can be confirmed by endomyocardial biopsy.
In most patients, the disease is self-limiting and only supportive therapy is available.
the immediate prognosis is excellent .
In most cases
Clinical Features
Cardiomyopathy
Definition
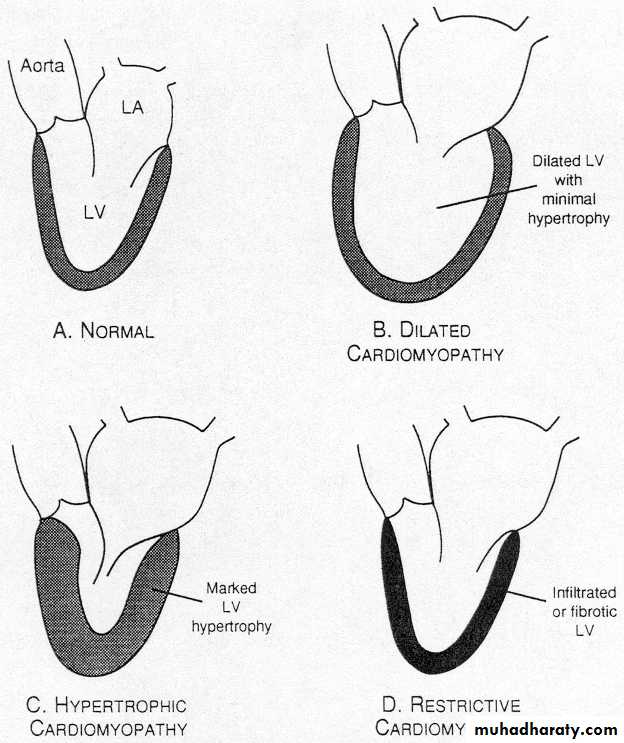
Cardiomyopathies are group of diseases primarily affecting the myocardium and characterized by myocardial dysfunction that is not the result of coronary atherosclerosis, hypertension, valvular dysfunction and pericardial abnormalities.Types
Dilated CMPHypertrophic CMP
Restrictive CMP
Arrhythmogenic right ventricular cardiomyopathy.
Obliterative cardiomyopathy.
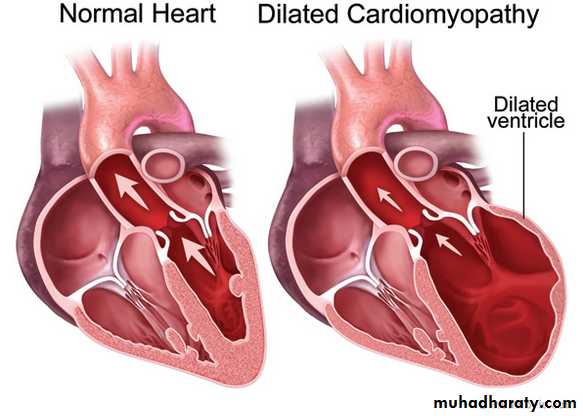
Dilated (congestive) CMP
Heart is enlarged and both ventricles are dilated.
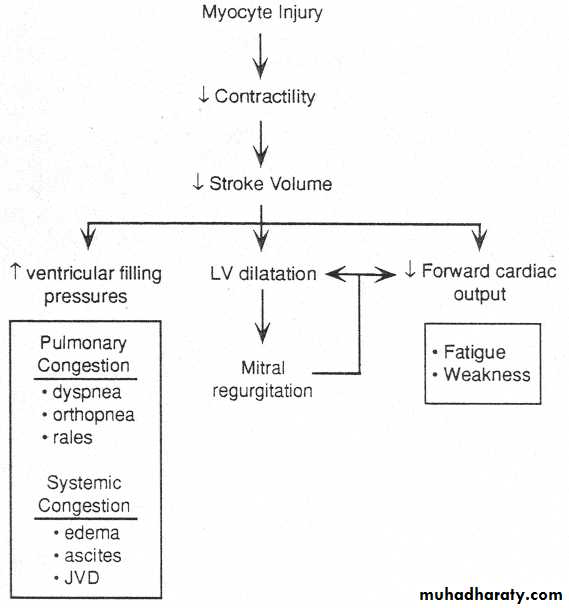
Myocardial contractility is diminished and cardiac output is reduced.
Pathophysiology
• The pathogenesis is not clear
EtiologyIdiopathic
Familial (almost 20 %)
Alcoholism (accounts for 15 to 40% of all cases )
Collagen vascular disease (SLE, rheumatoid
Postmyocarditis
Peripartum (last trimester of pregnancy or 5 m postpartum)
Toxins (cobalt, lead, phosphorus
Antiretroviral agents (zidovudine, didanosine, zalcitabine
Infections: viral HIV, Coxsachivirus B, toxoplasmosis
Hematologic (e.g., sickle cell anemia, hemochromatosis)
Ischemic
Nutritional (beri-beri)
Irradiation
Symptoms
Asymptomatic
Dyspnea on exertion
Orthopnea, paroxysmal nocturnal dyspnea
Fatigue
Palpitations
Systemic and pulmonary embolism
Chest pain
Signs
Resting tachycardiaRaised JVP
Small pulse pressure
Pulmonary rales, hepatomegaly, peripheral edema
S3, S4
MR,TR
Complications
Congestive heart failureArrhythmias ( brady or tachy)
Thromboembolism
Sudden cardiac death
Investigations
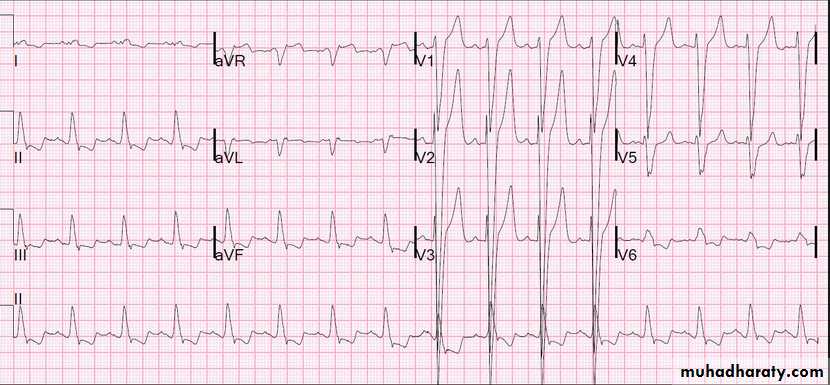
Electrocardiogram( ECG)
LBBB
LVH with ST-T changes
Arrhythmias (sinus tachycardia, AF, PVC, VT)
ECG
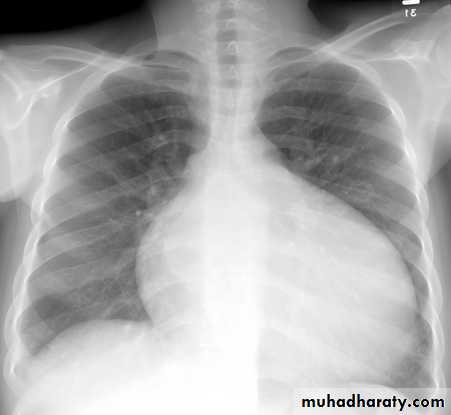
Chest X-Ray: cardiomegaly and pulmonary congestion
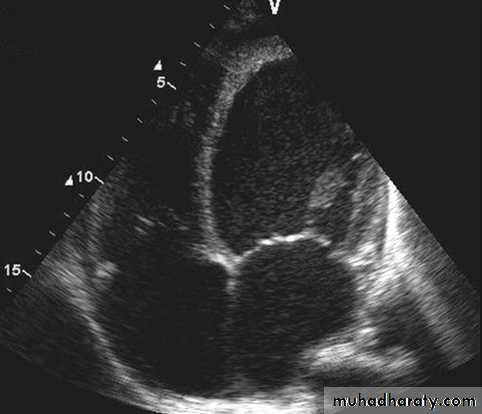
Echocardiogram: Chamber enlargement and global hypokinesisCXR
ECHO
Percutaneous
Cardiac cath: Contrast left ventriculogram, coronary angiogramEndomyocardial biopsy: The role of endomyocardial biopsy in patients with dilated cardiomyopathy is not well defined.
Goals of therapy
Treat underlying disease (SLE, alcoholism , hemochromatosis).Treat HF with sodium restriction, diuretics, ACE inhibitors , nitrates, β-blockers, spironolactone, and digitalis .
Limit activity when CHF is present.
Prevent thromboembolism with oral anticoagulants in all patients with Af and history thromboembolism.
Surgical treatment
Patients with dilated cardiomyopathy (left ventricular EF <25%) and associated coronary atherosclerosis (angina, ECG changes, reversible defects on thallium scan) may benefit from surgical revascularization (CABG).Consider heart transplant for young patients (younger than 60 years of age) who are no longer responsive to medical therapy.
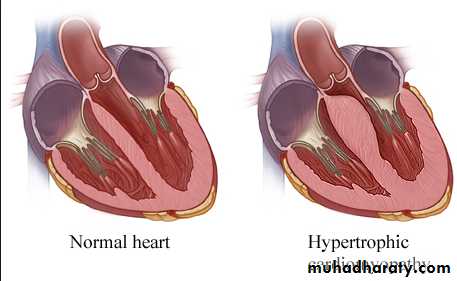
This is the most common form of cardiomyopathyGenetic disorder, usually with autosomal dominant transmission
• Hypertrophic cardiomyopathy
Types
Obstructive 25 %Non obstructive
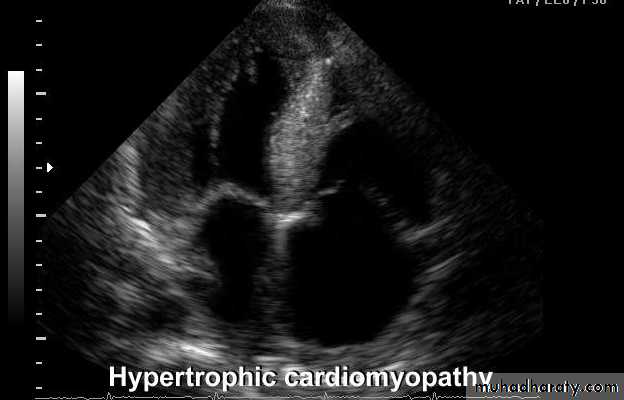
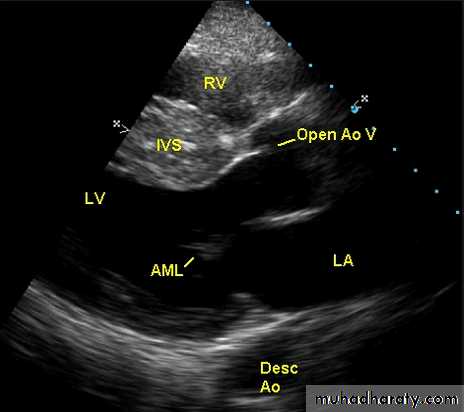
The hypertrophy may be generalised or confined largely to the interventricular septum (asymmetric septal hypertrophy or other regions (e.g. apical hypertrophic cardiomyopathy)
Microscopically
HCM is characterized by myocyte disarray in which there is loss of the normal parallel arrangement of cardiomyocytes, cells instead forming circles or whorls around foci of connective tissue. The myofibrillar architecture within cells is also disrupted (myofibrillar disarray).Pathophysiology
Dynamic LV outflow tract obstruction ( atleast >30 mm, usually > 50mm Hg)Diastolic dysfunction
Myocardial ischemia
Mitral regurgitation
Arrhythmias
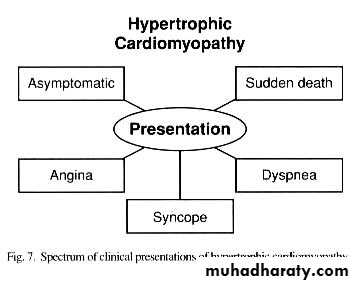
Signs
Apex localized, sustainedDouble apex beat
Palpable S4
Prominent “a” wave
Rapid upstroke carotid pulse, “jerky” bifid (spike-and-dome pulse)
Harsh systolic ejection murmur at base
MR: systolic murmur
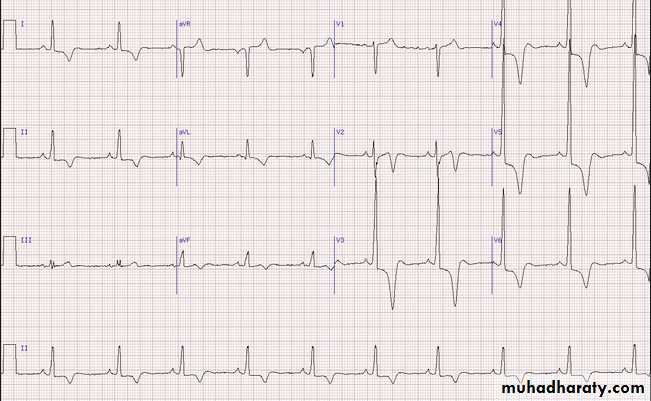
ECG
LA enlargement,Pathologic Q waves, most commonly in the inferolateral leads.
Voltage criteria for LVH
ECG 1
ECHO Echocardiography is diagnostic
Treatment
All first degree relatives: screening…echocardiography/genetic counseling
Avoid competitive athletics
Symptomatic
Beta blockers or calcium channel blockers
Antiarrythmic drugs
Disopyramide or amoidarone
Invasive treatment
High risk or non responders to medical treatmentICD ( high risk patients)
DDD pacemaker
Alcohol septal ablation
Surgery Myectomy
Restrictive Cardiomyopathy (RCMP)
DefinitionRestrictive cardiomyopathy is characterized by decreased ventricular compliance(stiff ventricles), usually secondary to infiltration of the myocardium.
These patients have impaired ventricular filling and reduced diastolic volume, normal systolic function, and normal or near-normal myocardial thickness.
• Amyloidosis is the most common cause in the UK,
• although other forms of infiltration (e.g. glycogen storage diseases) and a familial form of restrictive cardiomyopathy do occur.
• Diagnosis can be very difficult and requires complex Doppler echocardiography, CT or MRI, and endomyocardial biopsy.
• Treatment is symptomatic but the prognosis is usually poor and transplantation may be indicated.
Arrhythmogenic right ventricular
cardiomyopathyIn this condition, patches of the right ventricular myocardium are replaced with fibrous and fatty tissue .
It is inherited as an autosomal dominant trait .
The dominant clinical problems are ventricular arrhythmias, sudden death and right-sided cardiac failure.
The ECG typically shows a slightly broadened QRS complex and inverted T waves in the right precordial leads.
MRI is a useful diagnostic tool and is often used to screen the first-degree relatives of affected individuals.
Patients at high risk of sudden death can be offered an ICD.