Radiotherapy – an overview
Dr.Khdhair Al-RawaqRadiotherapy – (medicine) ‘…the treatment of disease (especially cancer) by exposure to radiation from a radioactive source or substance’
History and development of the use of radiation in medicine
What is cancer and what causes it?
Different types of radiotherapy – external beam, brachytherapy and unsealed sources
Example patients and future advances
The past
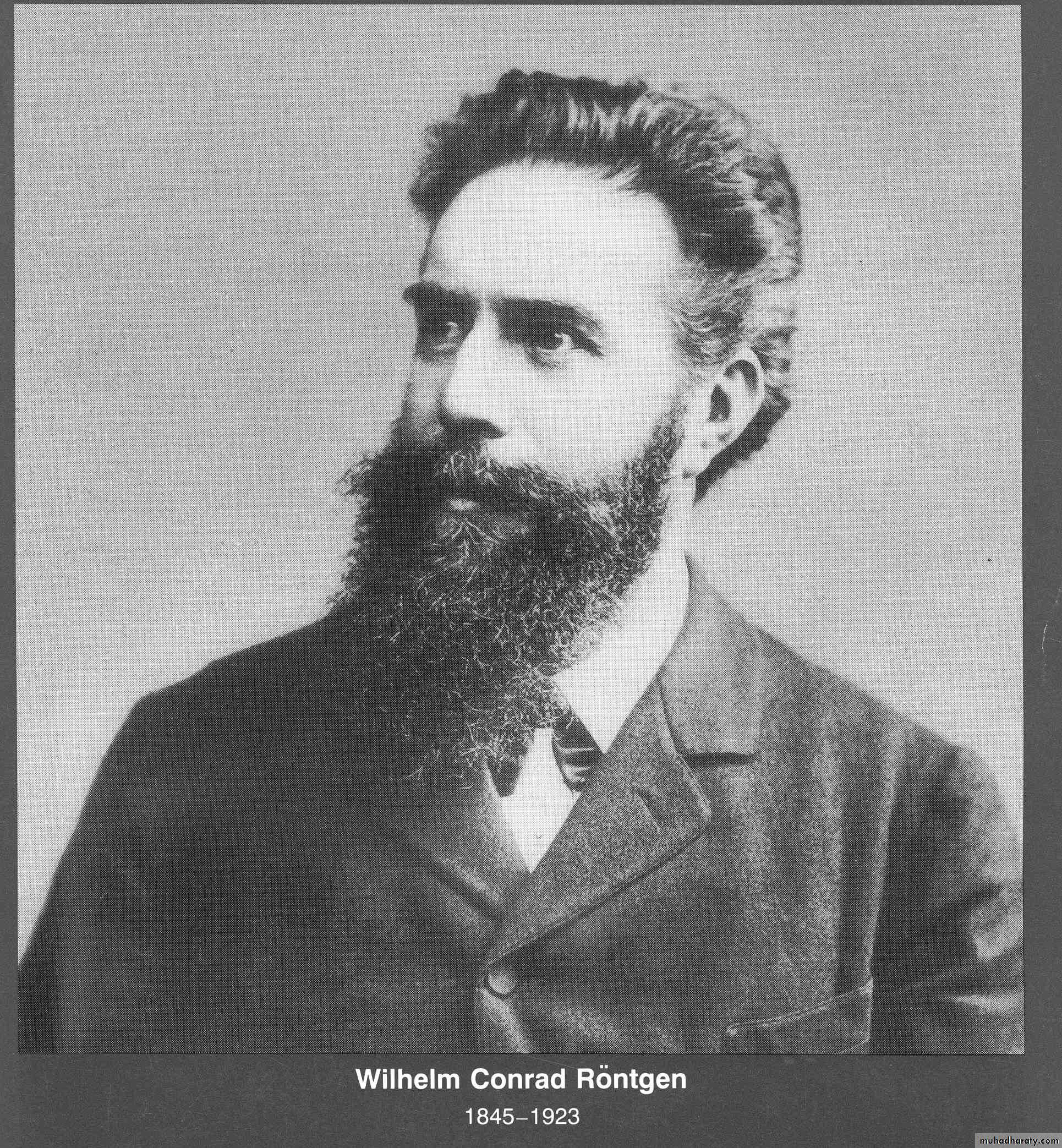
William Conrad Roentgen (1845-1923)
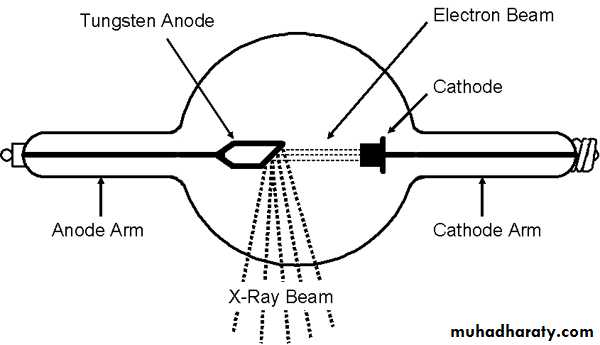
Discovered x-rays in 1895 which revolutionised the field of physics and medicineWilliam Crookes (1832-1919).
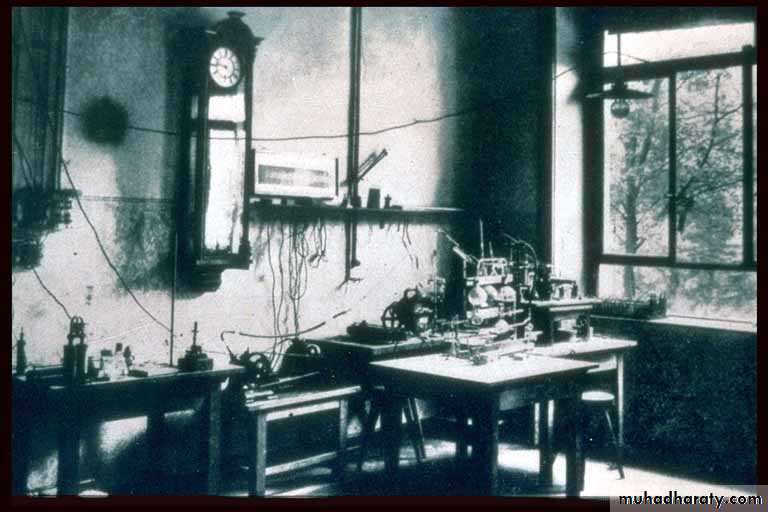
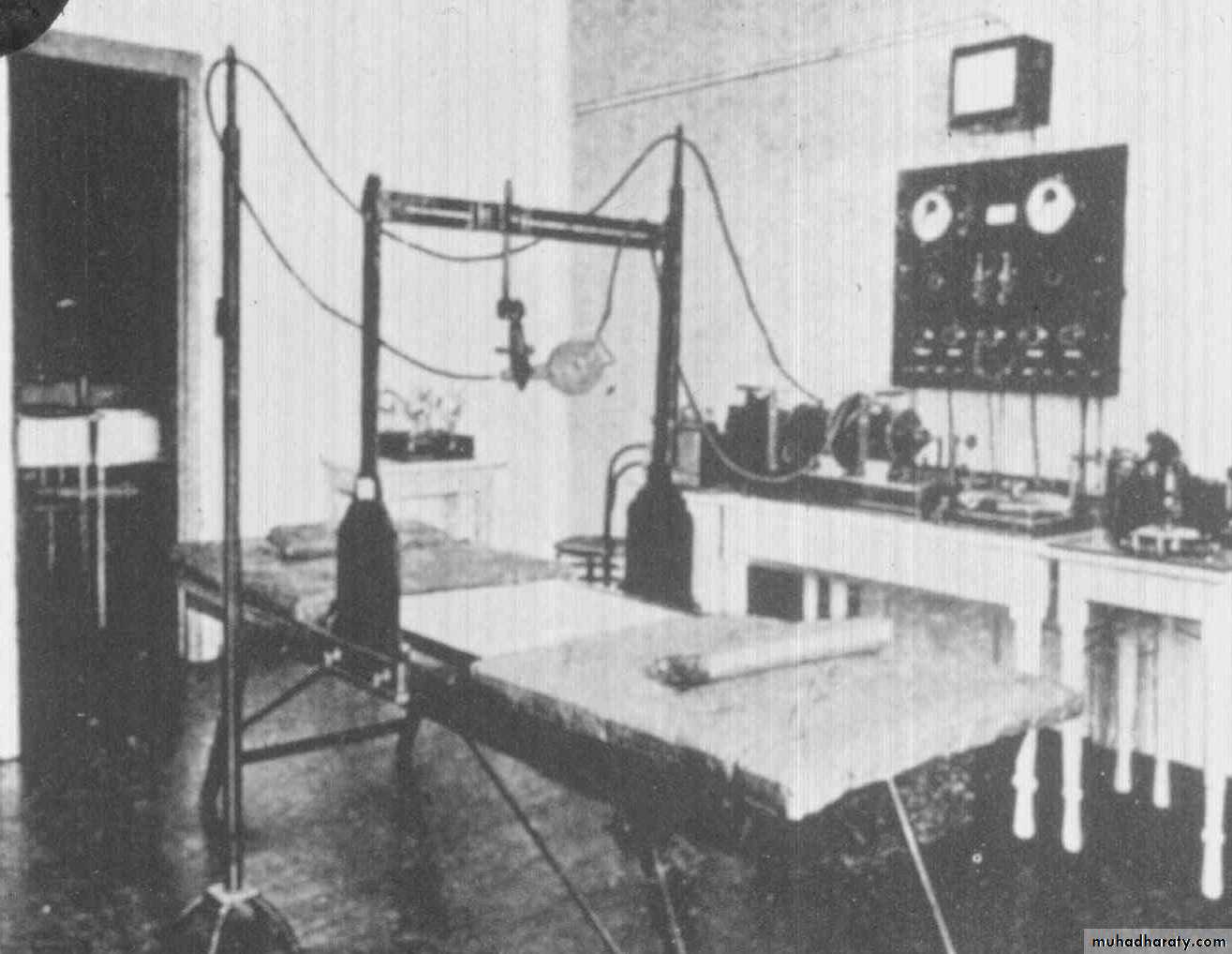
The Crookes tube – investigated behaviour of cathode rays in evacuated glass tubesRoentgen’s Laboratory in Wurzburg. Working with shrouded Crookes tubes, noticed a barium screen across the room glowing. The birth of the x-ray.
Radiograph of Frau Roentgen’s left hand
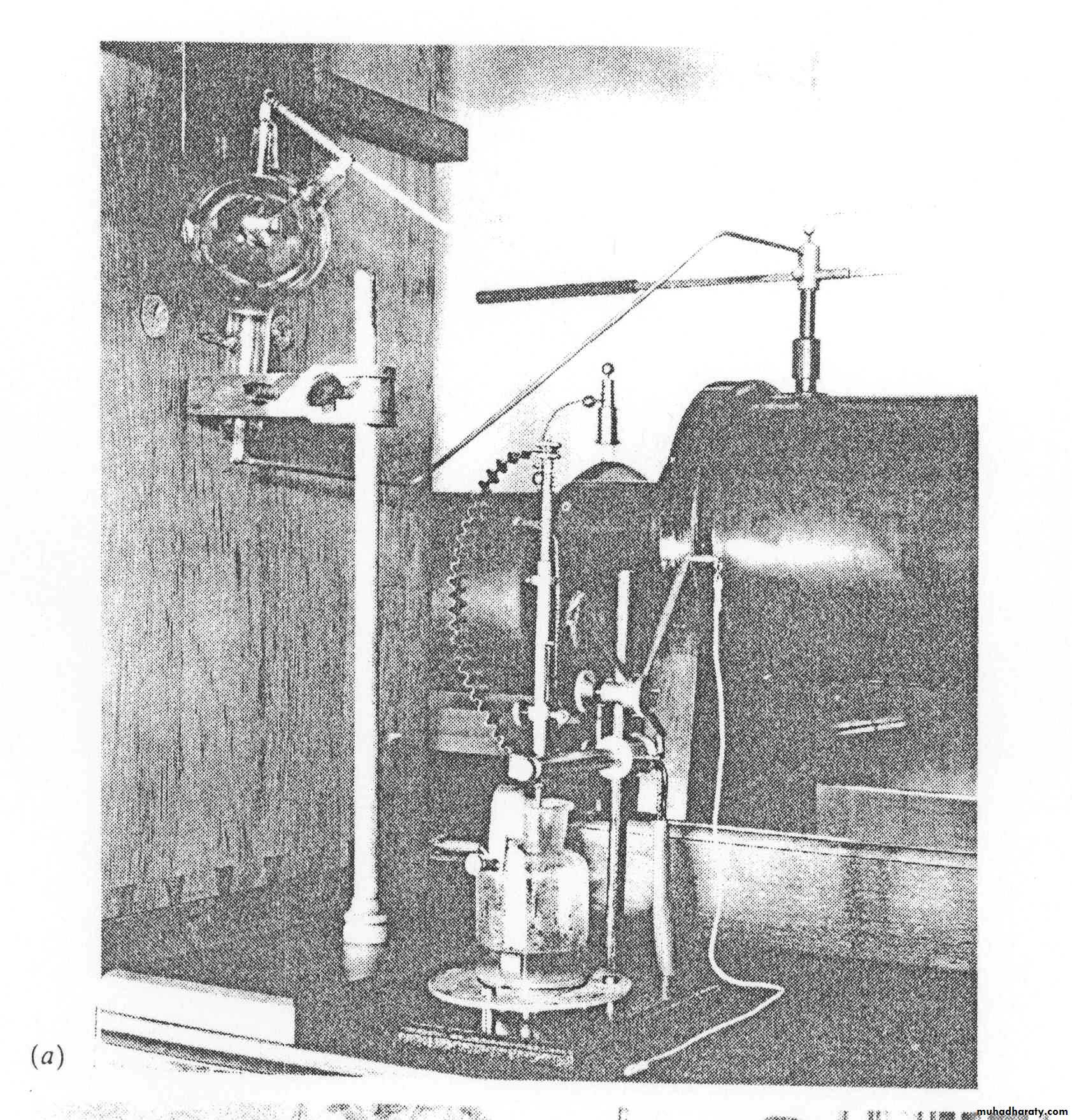
Roentgen’s x-ray apparatus.
Note the lack of any shielding around the Crookes tube.Henri Becquerel (1852-1908)
Marie Curie (1867-1934)Ernest Rutherford (1871-1937)
Early departments
Glasgow Royal Infirmary (1903).
Using a platinum target, x-rays could be focussed thus making useful radiographs possibleEarly radiotherapy for breast cancer (1903).
The Coolidge x-ray tube (1920).
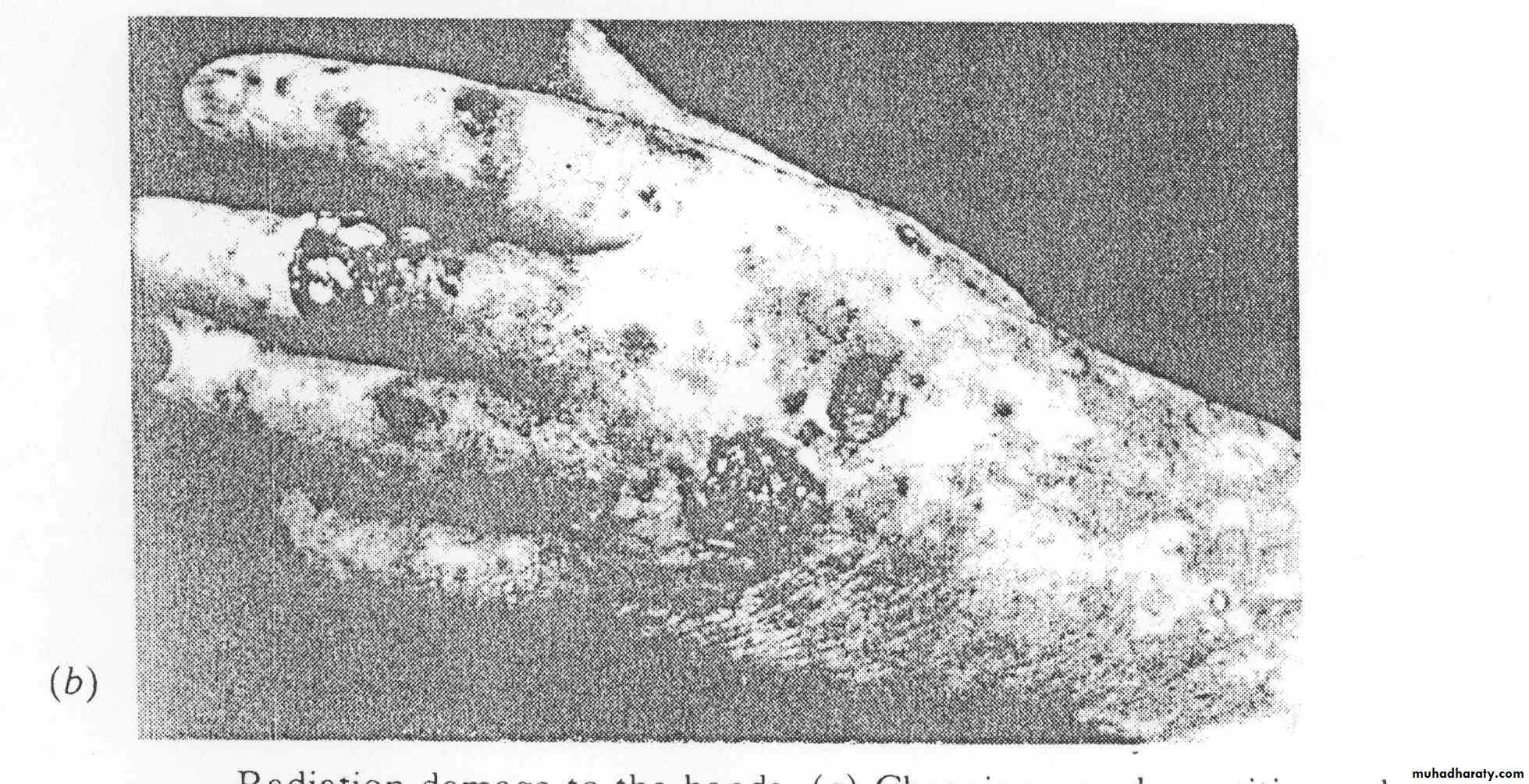
The basic design is the same todayRadiation damage
Radiation-induced ulceration of a physician who used x-rays for 8 years. In the early days little was known about the dangers of radiation.
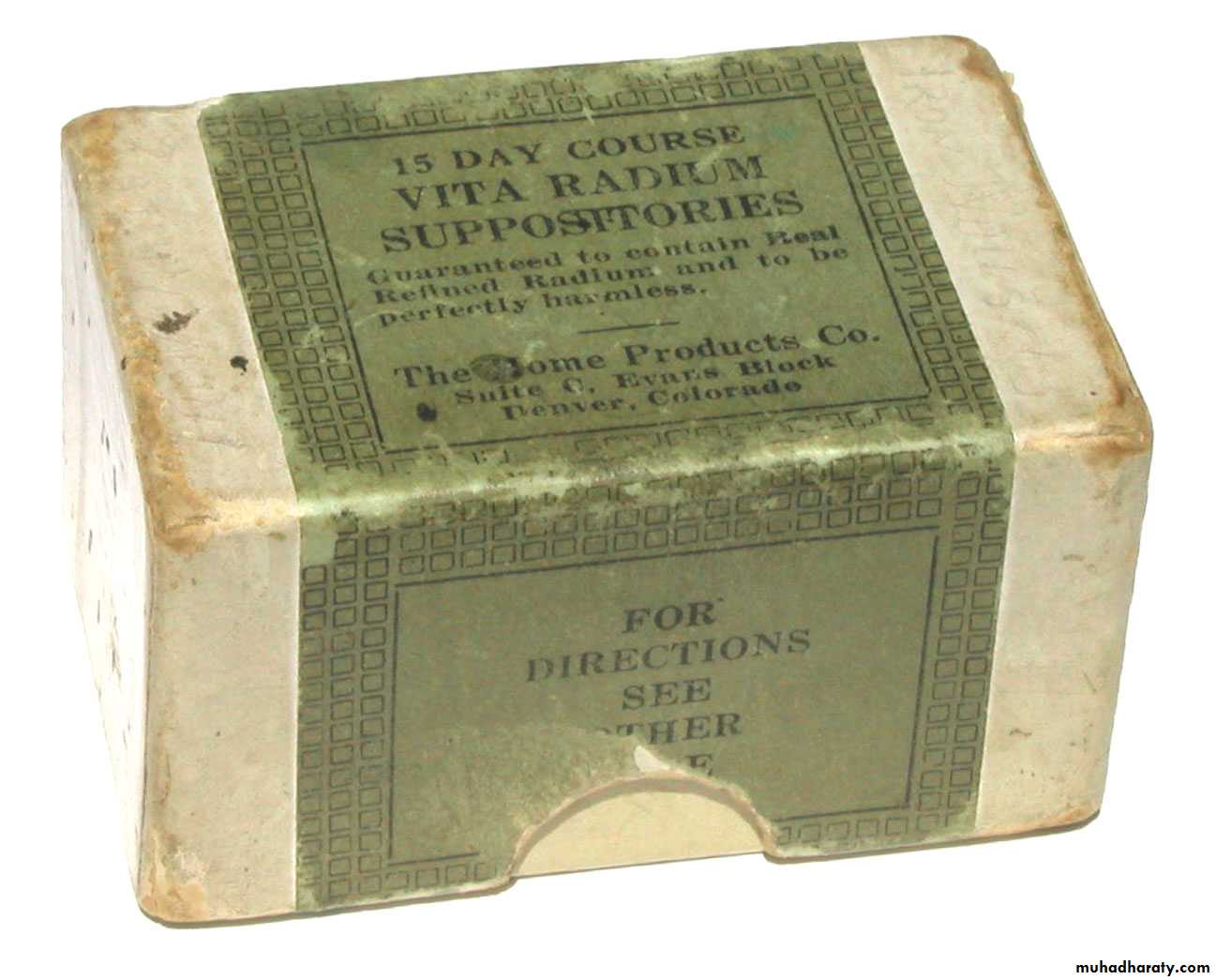
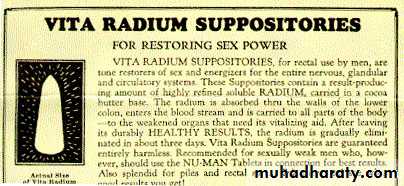
Quack cures
The ‘Tricho System’ (early 1920s) was one of a number of systems which used x-rays to remove unwanted hair
The ‘curative’ properties of spa water was thought to be due to radon gas, hence the invention of handy devices for home use
‘Radithor’ (1928)
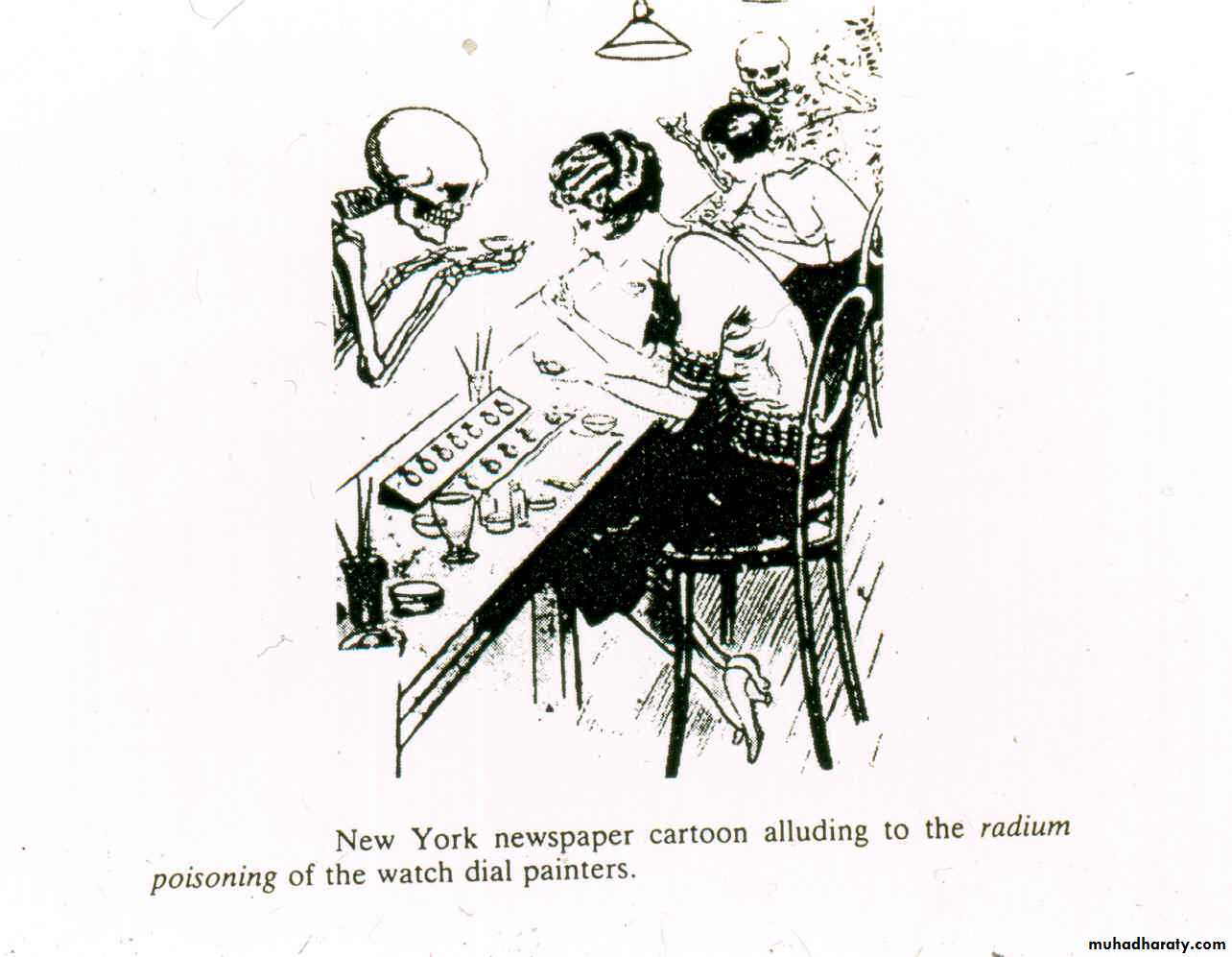
The truth starts to sink in…….
‘New York newspaper cartoon alluding to the ‘radium poisoning’ of the watch dial painters (1924)
(1930)
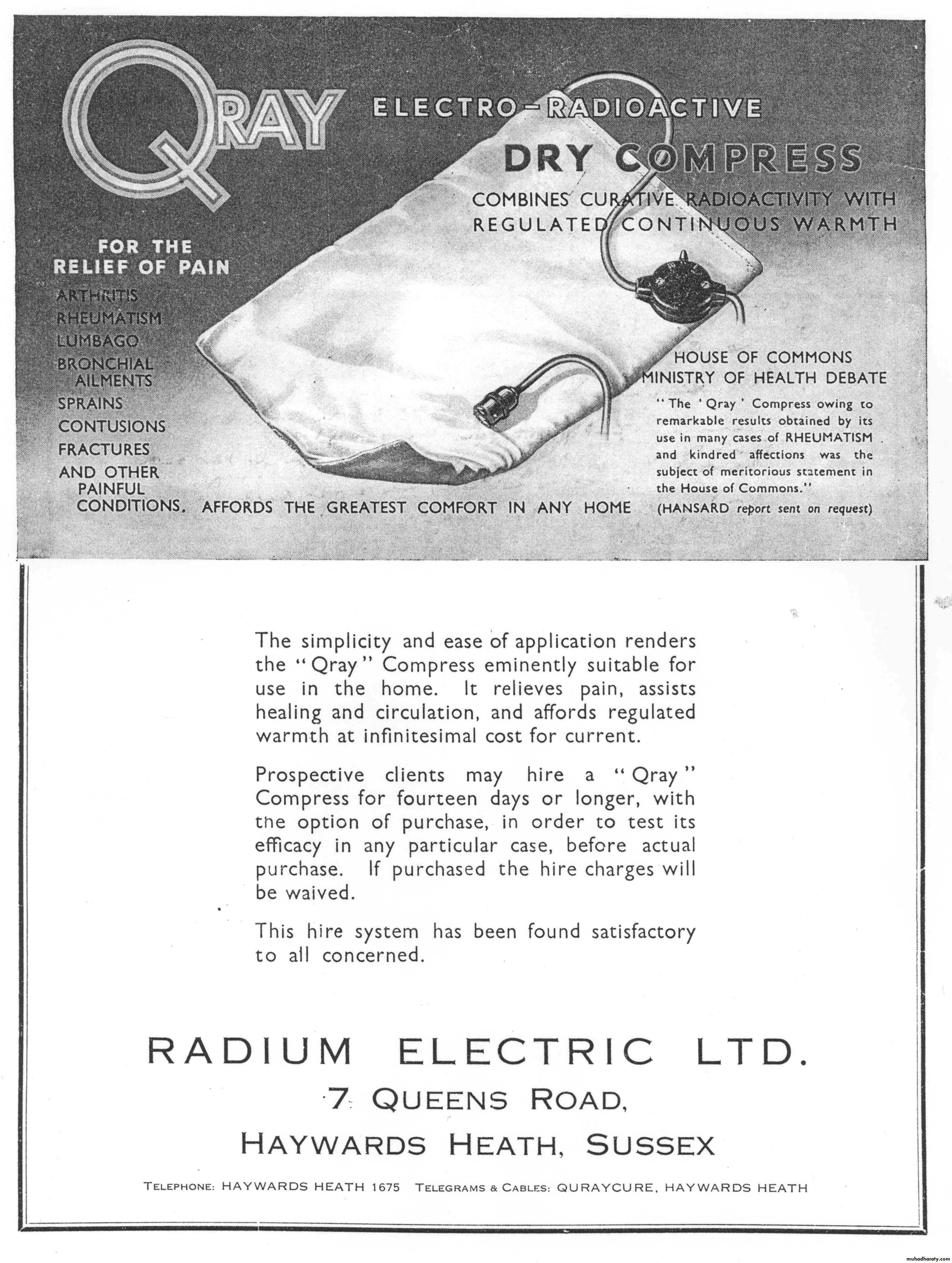
Advert for the ‘Qray Compress – invaluable in the treatment of bronchitis, colics, fractures, gout, insomnia, lumbago, shock, strains, etc’
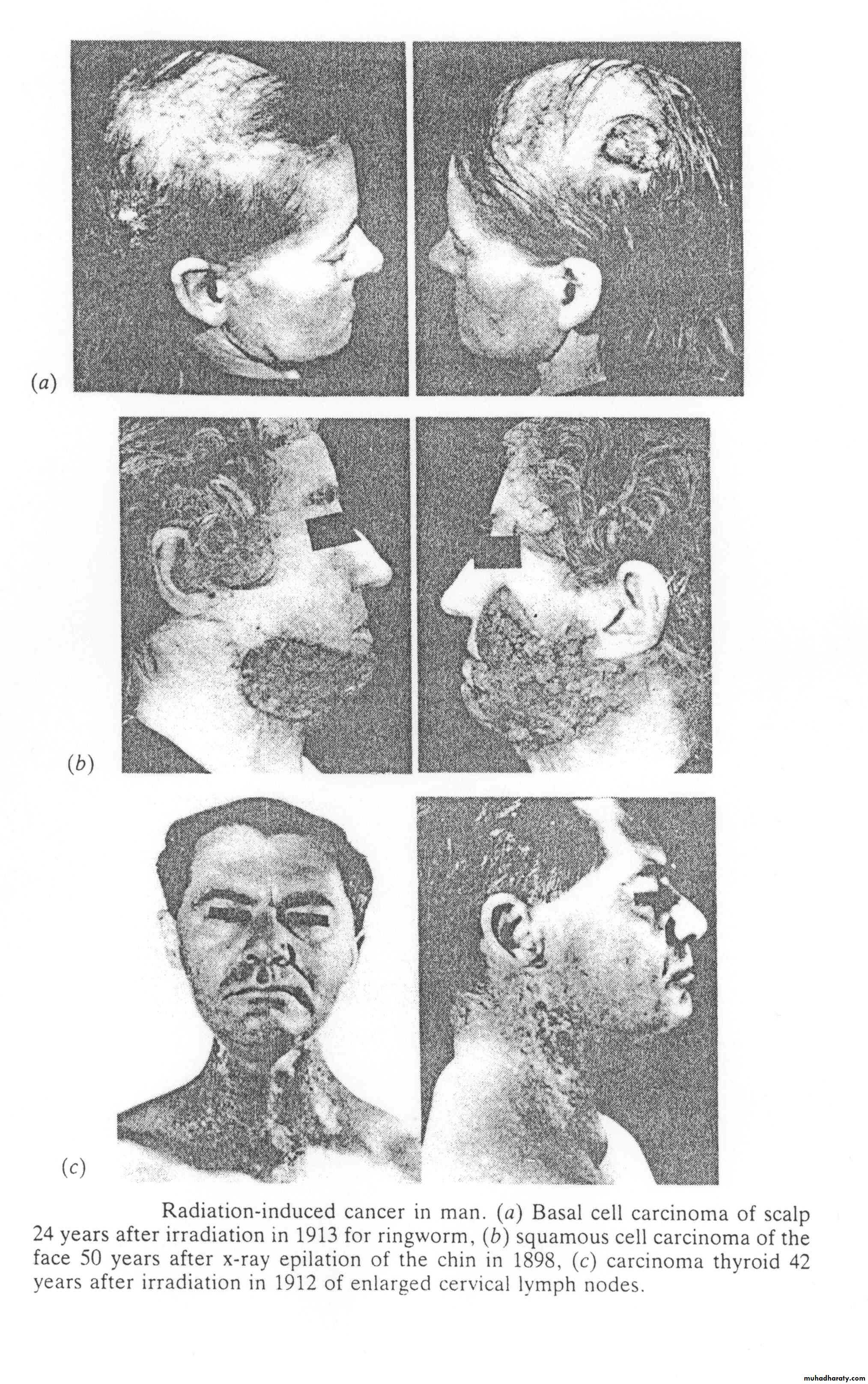
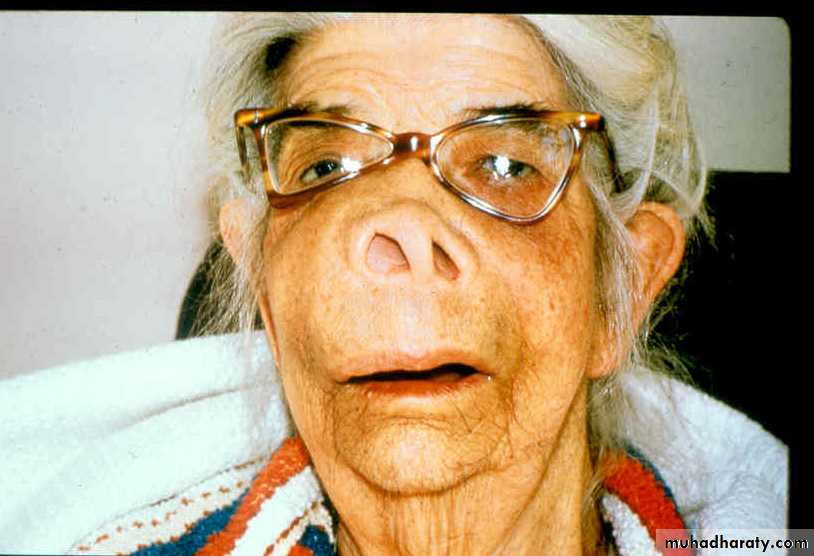
Radiation-induced cancers
Basal cell carcinoma of scalp 24 years after treatment for ringworm
Squamous cell carcinoma 50 years after x-ray treatment of facial hair
Thyroid carcinoma 42 years after treatment in 1912 for enlarged lymph nodes
Radiotherapy from the 1920s
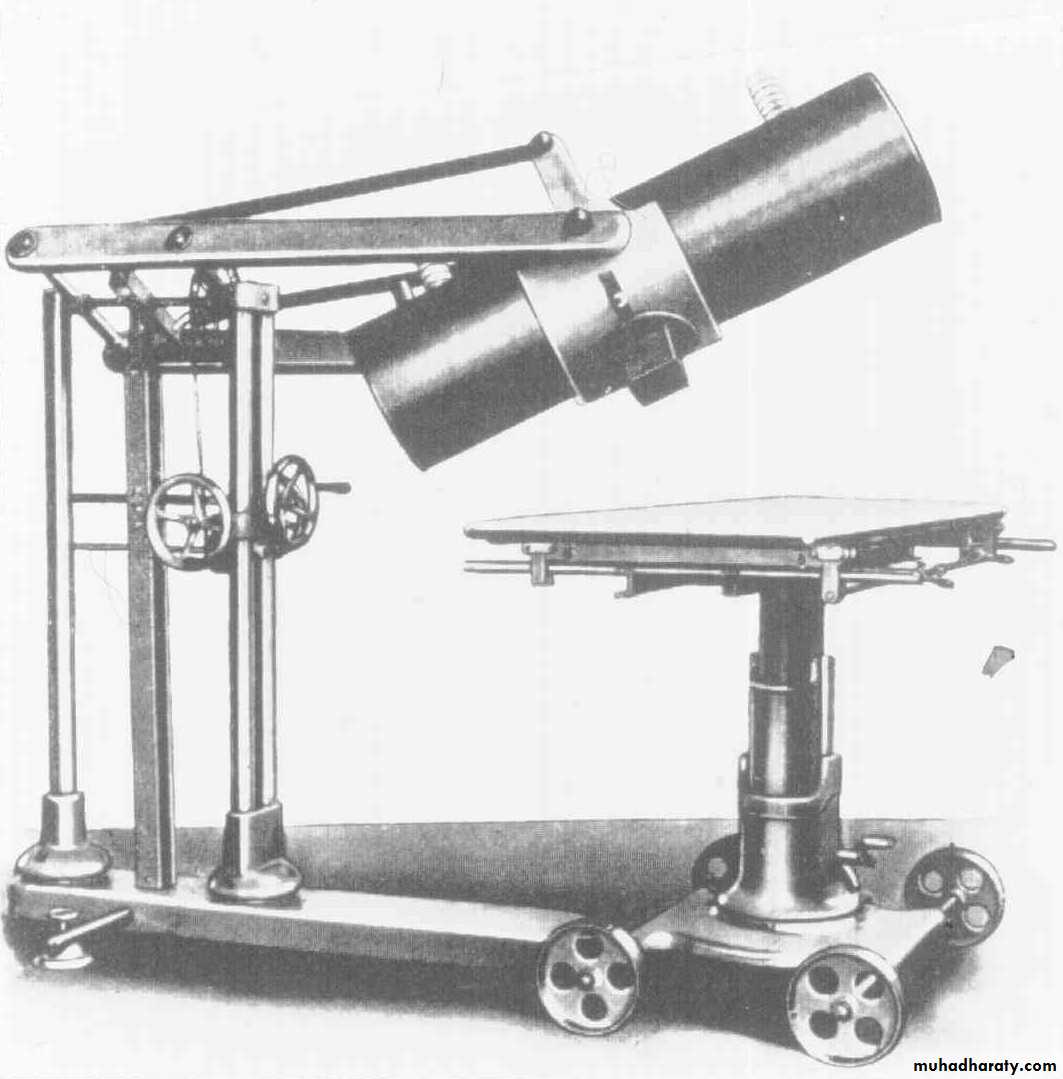
Deep x-ray therapy unit from the mid 1920s
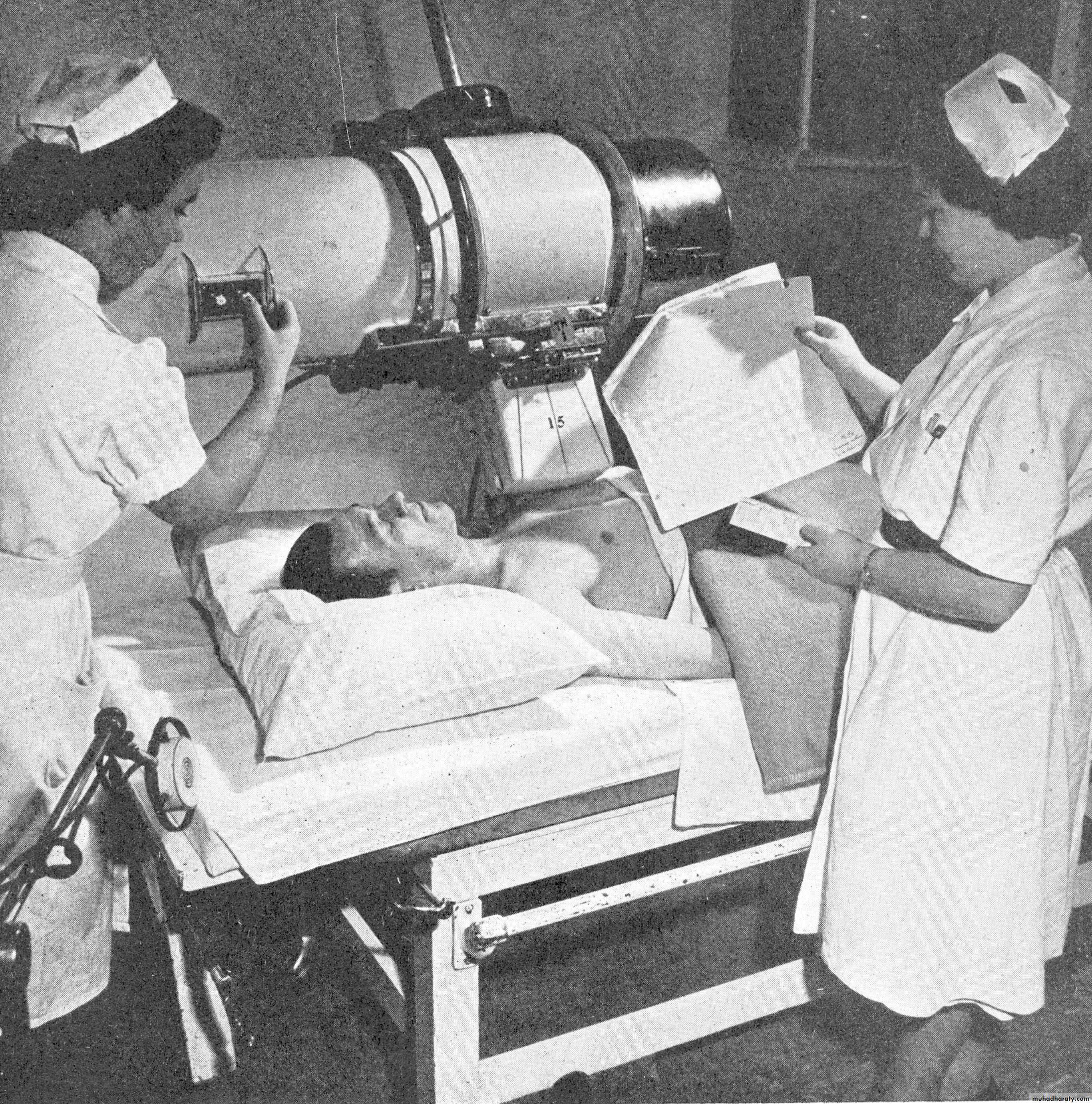
Middlesex Hospital (1950)
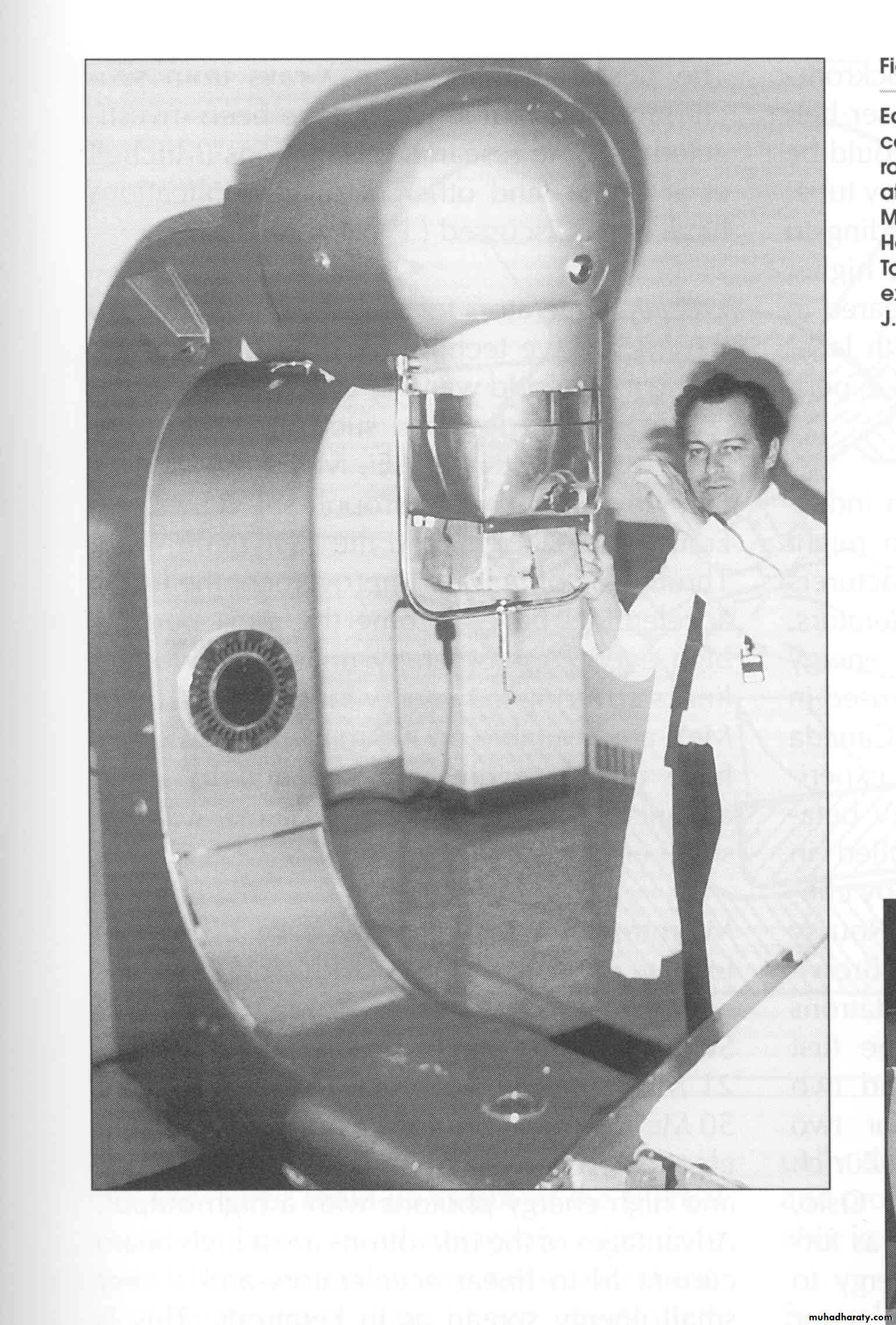
The Metropolitan Vickers Deep X-ray Unit (250kV)Early Cobalt Teletherapy Unit from the 1950s
Toronto, Canada‘Mobaltron’ Cobalt Unit (1972)
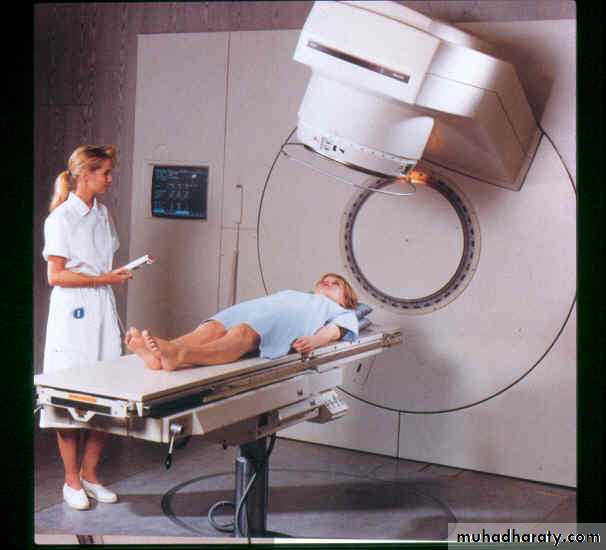
PortsmouthAn ‘SL75’ linear accelerator (1998)
What is cancer?1 in 4 deaths per year are cancer related
Subtle (or dramatic) changes in DNA coding lead to loss of normal cell mechanisms – differentiation, proliferation, adhesion and apoptosis
Balance between population loss and gain is uncoupled, leading to excessive proliferation – a tumour – and subsequent local invasion and metastasis
Everyone has a cancer at some point – controlled by normal defence mechanisms
Typical small basal cell ca
SCC above kneeStage 3 breast tumour
Extensive tumour upper palateThe causes of cancer
Genetic – oncogene over-expression, loss of tumour suppressor genes, various syndromesChemical – smoking, asbestos, dyes, soot, oils, chrome, arsenic, alcohol, diet?
Physical – solar radiation (UV), ionising radiation (radon, medical), heat, trauma
Viral – human papilloma virus (cervix), T-cell types (HIV), hepatitis B
Immune – AIDS, transplant patients
Endocrine – long-term oestrogen exposure?
To treat or not to treat?
Not every patient with cancer would benefit from active treatment (surgery, radiotherapy, chemotherapy, hormonal)Treatment should always have a positive benefit for the patient but the outcome is not always predictable
Balancing the probability of improving patient’s condition, whether by palliative symptom control or radical cure, against the discomfort caused, the disturbance to lifestyle and the risk of induced cancer
Radical and palliative
Radical – treatment given with the intent of long-term control or cure
Palliative – improves quality of life or treats symptoms with no implied impact on survival
Sometimes difficult to define aims in these terms
Adjuvant – prophylactic use of local or systemic treatment, following a radical approach, to prevent recurrence (chemo, hormonal)
Physics of Radiotherapy
Both electromagnetic and particulate radiation is used in radiotherapyElectromagnetic radiation (photons) for external beam are generated in x-ray tubes or linear accelerators
Particulates (electrons, protons, neutrons) are either generated artificially or are emitted following radioactive decay processes
The electromagnetic spectrum
Ionisation and absorbed dosePhotons interact with atomic structure (ionisation) – shell electrons and more photons are scattered
The ‘free’ electrons are stopped quickly, releasing their energy into tissue
Ionised DNA and free radicals cause cell damage – repair commences
Severe damage is not repaired and cell dies
The amount of energy delivered to and retained in tissue is called the ‘absorbed dose’
Unit of absorbed dose is the Gray1 Gray = 1 Joule/kg
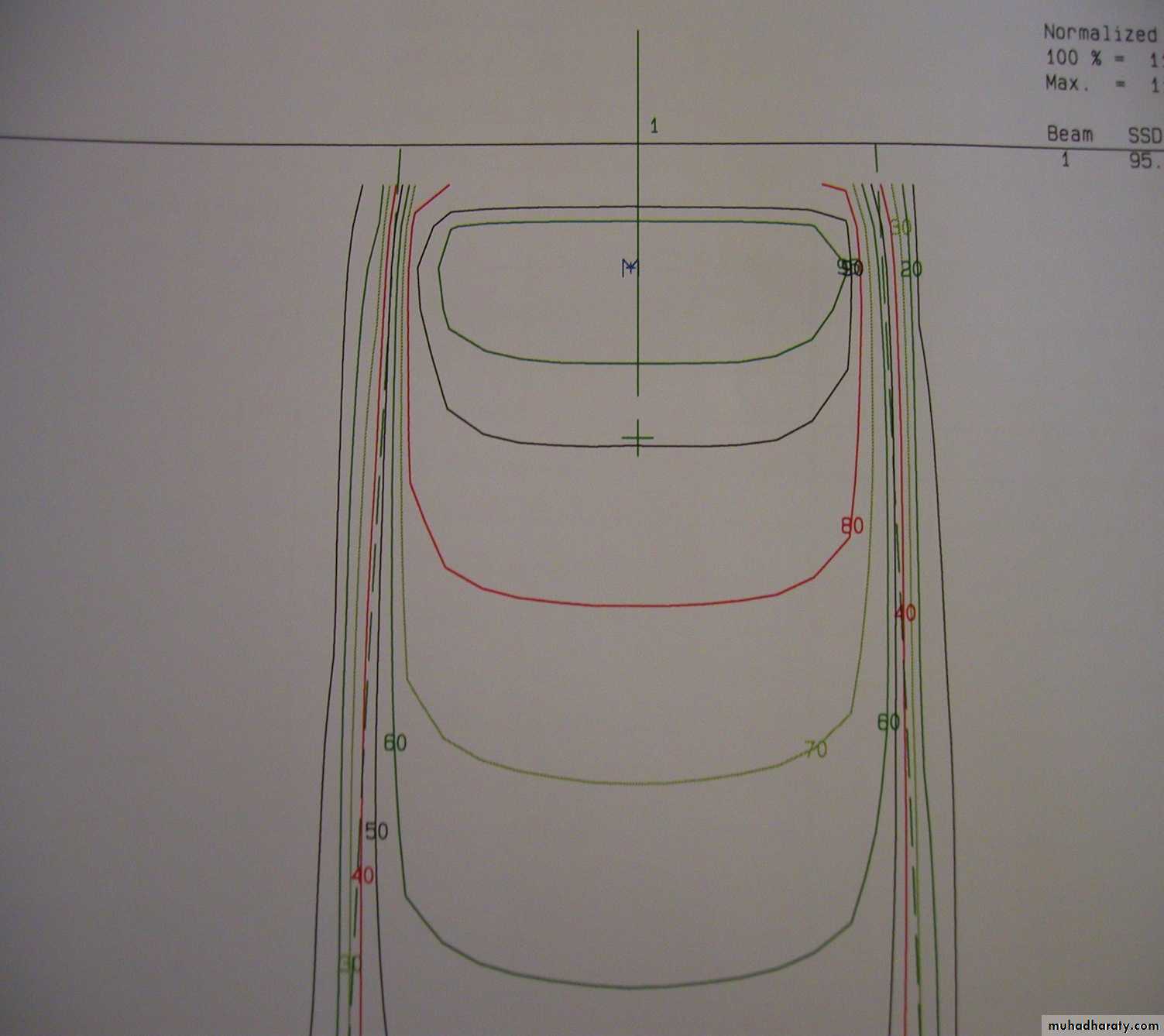
Absorbed dose decreases with depth – the depth dose curve
Increase photon beam energy = increase in depth dose
Typical depth dose curve
10 X 10 cm field10MV photons
The Linear Accelerator
How does it work - fractionation
High energy radiation damages or destroys both normal and tumour cellsIn most cases, normal cell repair mechanisms are slightly more efficient than those of tumour cells
Radical treatment doses are delivered in small daily fractions over several weeks
Fractionation and survival
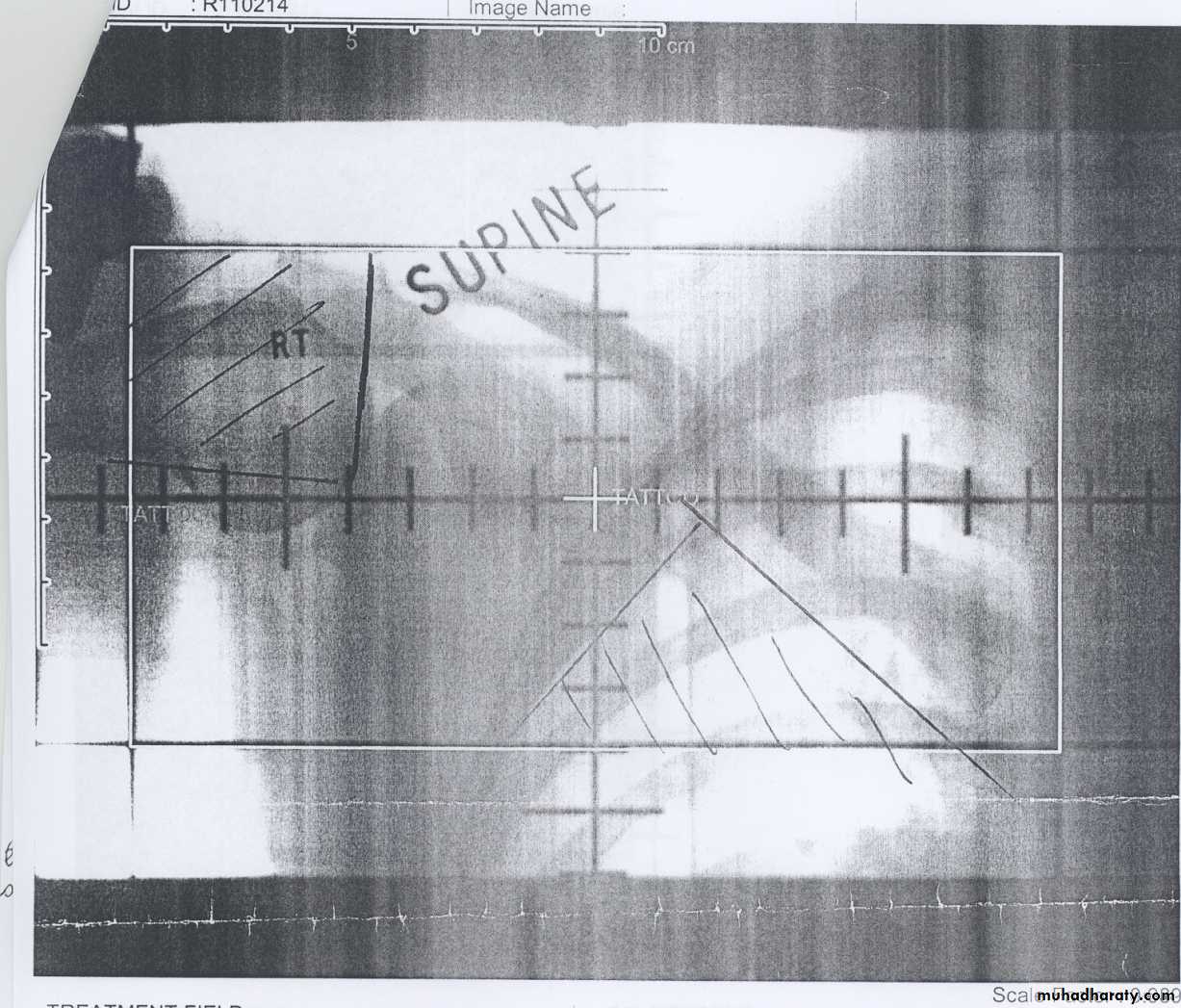
Delivering the dosePalliative treatments – simple single or opposed fields using visual marking or x-rays
(bony pain, advanced lung tumours, large brain tumours, obstruction, haemorrhage)
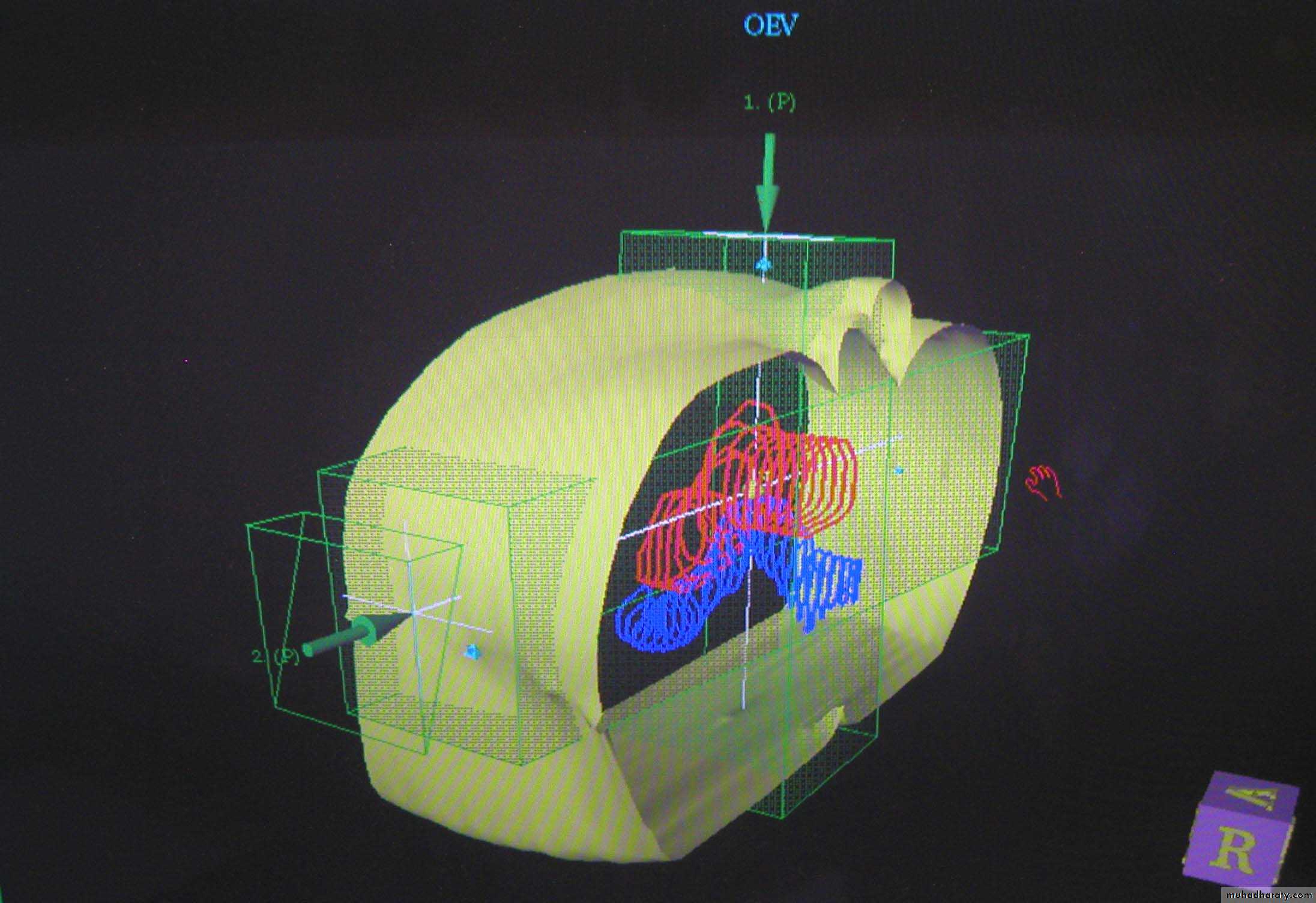
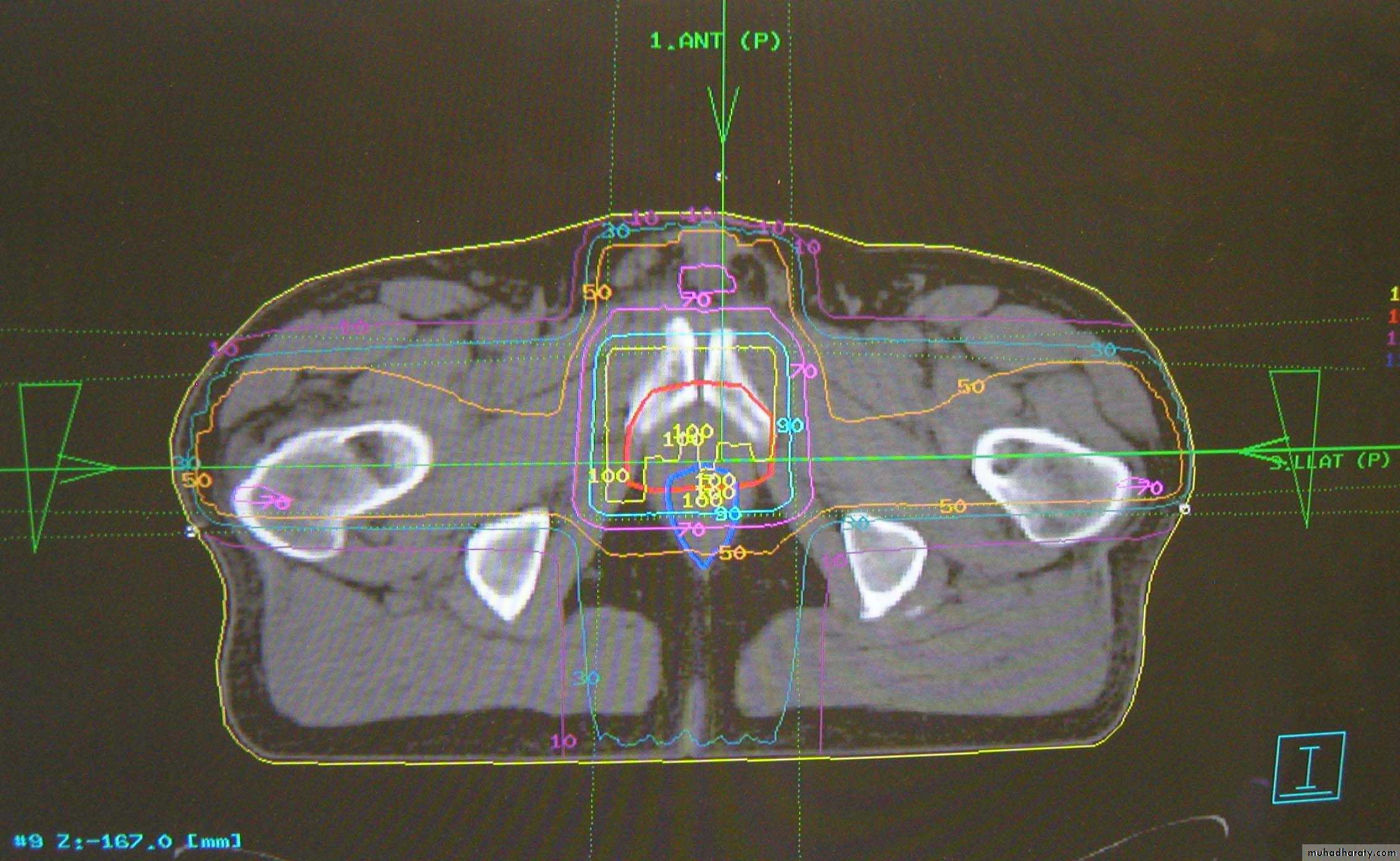
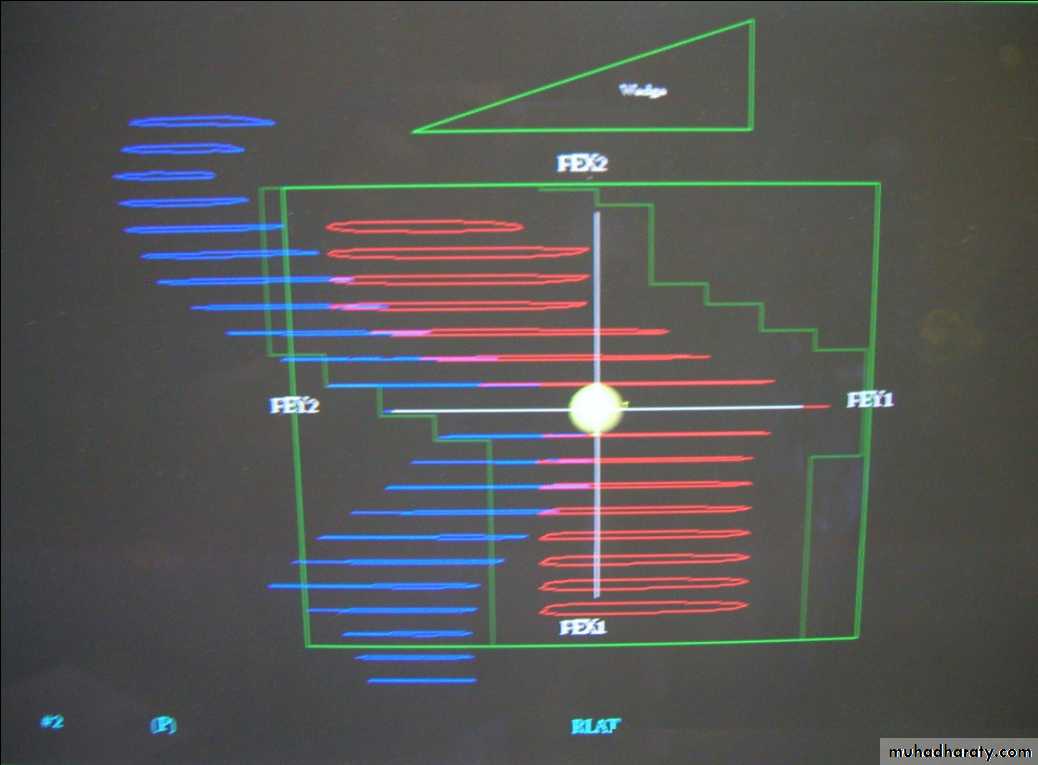
Radical treatments – complex multi-field treatment plans using image sets and customised field shapes
(prostate, bladder, head & neck sites, radical brain tumours, early breast)
It’s all about accuracy
Need to deliver a high, even dose to the tumour, whilst avoiding normal and sensitive tissue
Localisation of tumour volume is very important
Many diagnostic procedures available:
Diagnostic x-rays
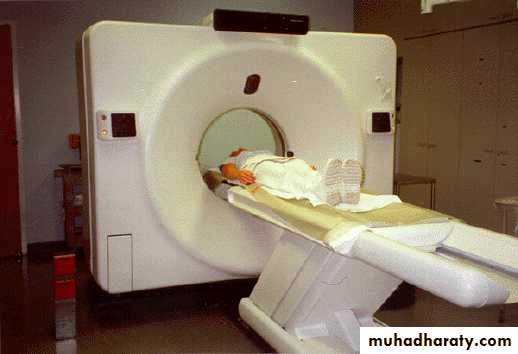
CT (Computerised Tomography)
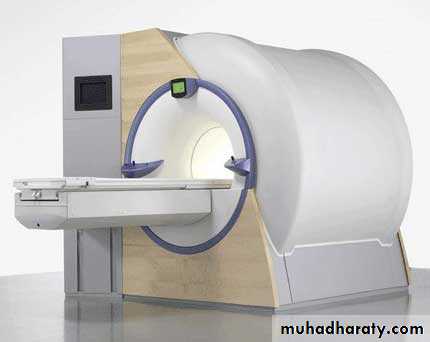
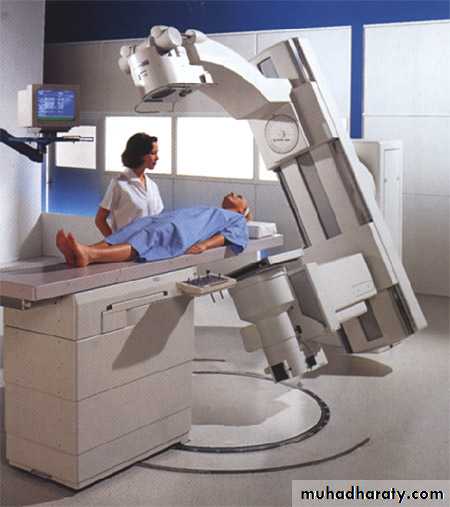
Radiotherapy simulatorMRI (Magnetic Resonance Imaging)
It’s all about accuracy
• Need to deliver a high, even dose to the tumour, whilst avoiding normal and sensitive tissue• Localisation of tumour volume is very important
• Many diagnostic procedures available
• Images from CT and MR scanners sent directly to planning system
• Planner designs the treatment plan
3D Conformal prostate plan with MLC
Multileaf collimator (MLC) array
The future – IMRT, IGRT
The patient pathway
Referral (GP)
New Patient Clinic (MDT)
Radiotherapy
Histology
Other tests
?
?
Simulation
MRICT
Planning
TreatmentFollow-up (3-5yrs)
Physics
MouldroomSide effects of radiotherapy
Toxicity divided into early or acute (during treatment) and late or chronic (months or years after treatment)
Early effects include skin erythema, diarrhoea, hair loss, sickness
Late effects include fibrosis (lung, skin, bladder), perforation and fistula, myelitis causing paraplegia, induced cancer
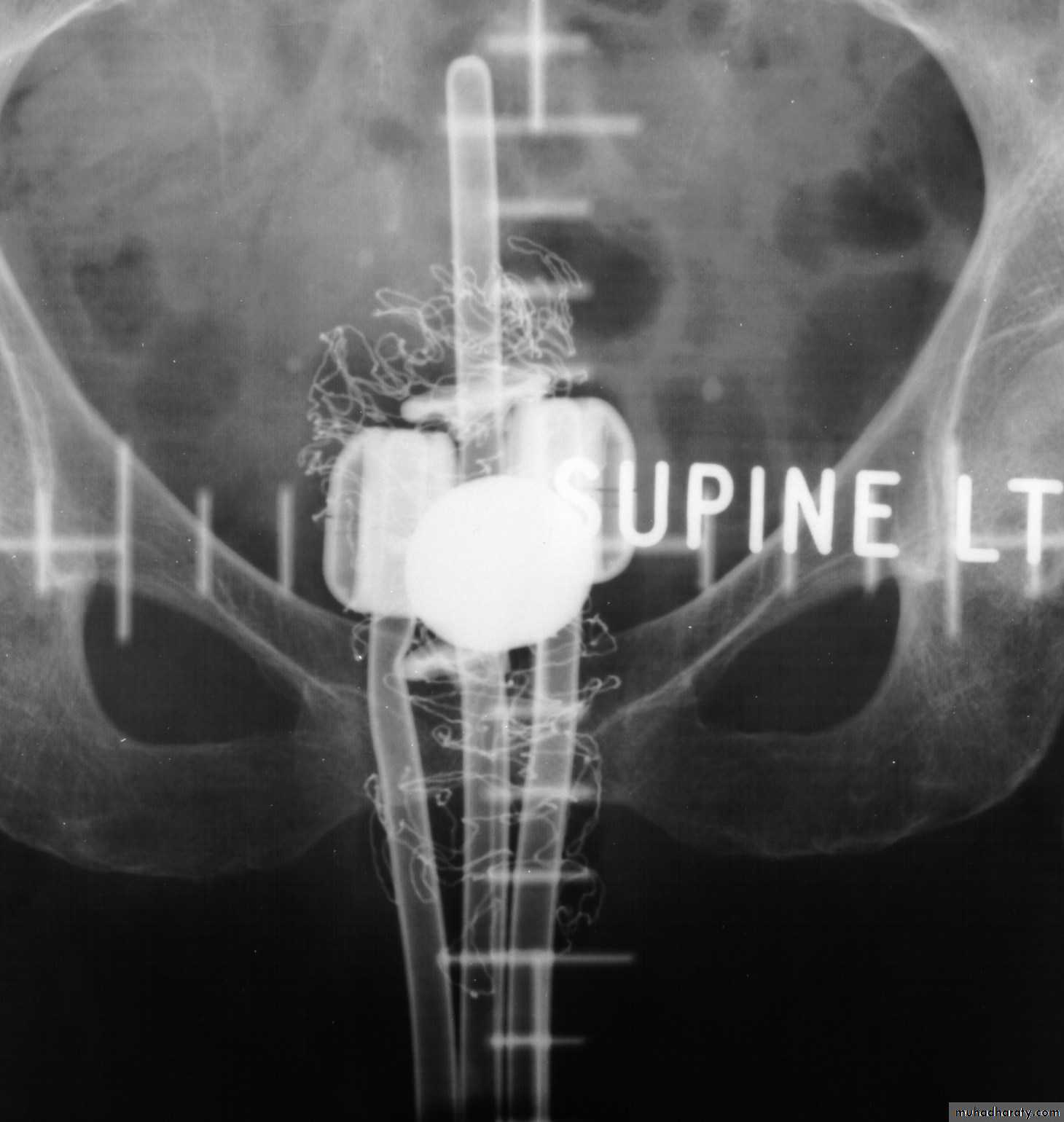
Brachytherapy
The use of sealed radioactive sources placed on or within tissueSealed source – the isotope is encapsulated and secure under high degree of physical or chemical stress
High dose rates near source with rapid fall-off at distance
Interstitial, intracavitary, surface application
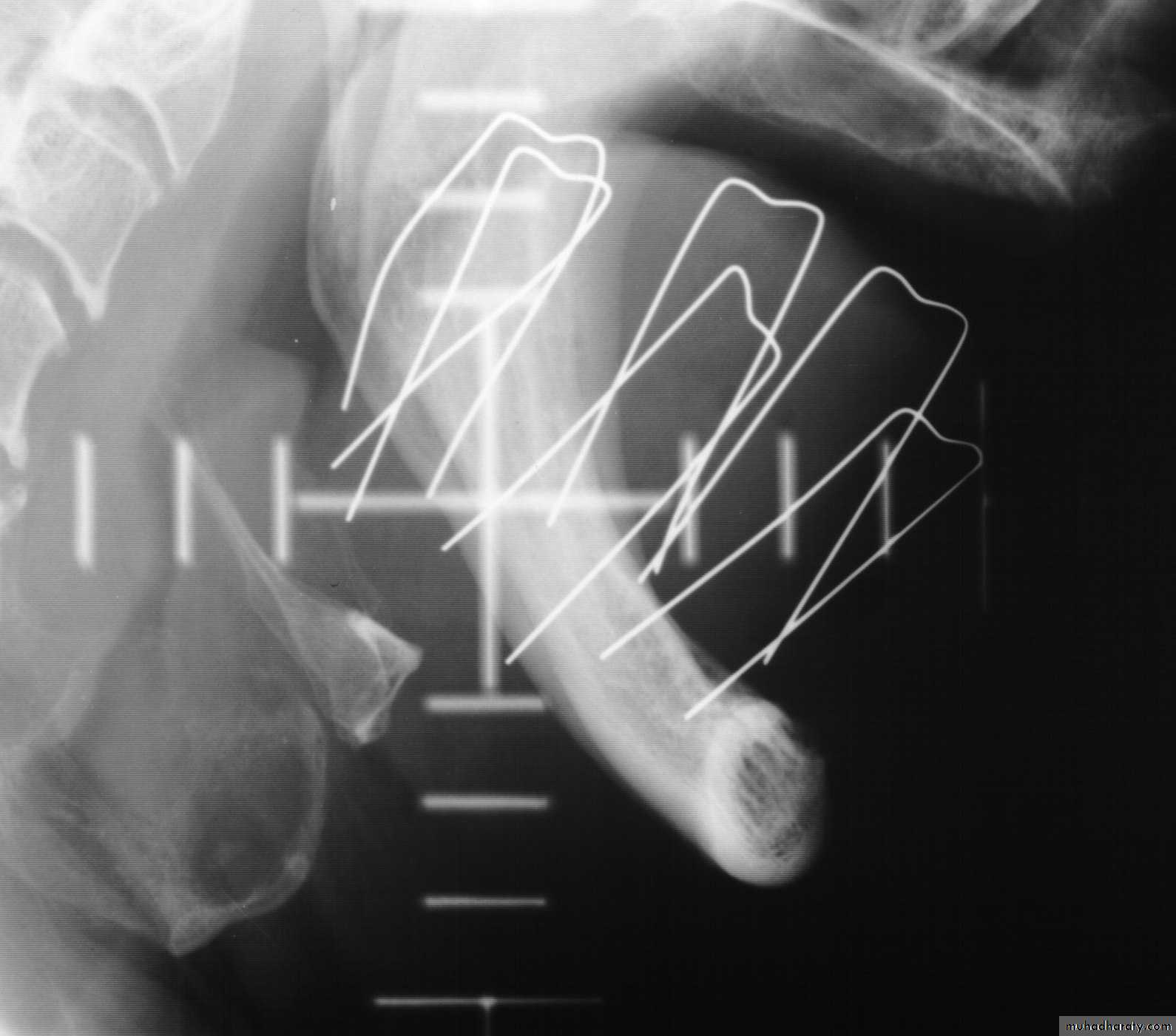
Interstitial treatments
192Ir (Iridium)Breast, anal and vaginal implants using iridium wire in steel needles
Tongue implants using hairpins
• 198Au (Gold) and 125I (Iodine)
• Seeds, for tongue and prostate. Permanent implant.•
Intracavitary treatments
• 137Cs (Ceasium)• Cervix & vagina using afterloaded source trains in plastic applicators.
• 192Ir (Iridium)
• The Microselectron - small, active source driven into applicatorsSurface applicators
• Use of surface applicators (or moulds) has diminished with the onset of electron treatments• 90Sr (Stontium) still used in some centres for low-energy beta treatment of opthalmic corneal vasularization
Unsealed sources
Isotope administered in liquid or colloid formMainly beta emitters
Systemic or targetted - relies on the chemical preference of target organ in uptake
131I (Iodine) in saline for thyroid tumours
89Sr (Strontium) as a chloride for bone deposits
32P (Phosphate) for polycythaemia vera
Radiation synovectomy, radiolabelled antobodies
Does it work?