The elbow and forearm
Dr. Ammar Talib Al-YassiriCollege of Medicine/Baghdad University
Congenital disorders
Acquired deformitiesOsreochondritis dissecans
Loose bodies
Tuberculosis
Rheumatoid arthritis
Tennis &golfer’s elbow
Bursitis
stiffness
objectives
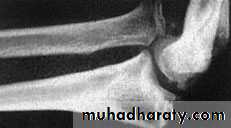
CONGENITAL DISLOCATION OF THE RADIAL HEADMay be anterior or posterior and is usually bilateral
Lump
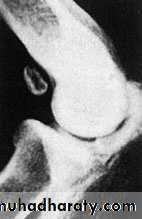
X-rays: show that the dislocated radial head is dome-shaped
Treatment:
Function is usually surprisingly good (need no treatment
If the lump limits elbow flexion it can be excised
CONGENITAL DISORDERS
CONGENITAL SYNOSTOSIS
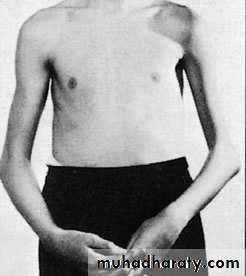
Proximal radio-ulnar synostosis causes loss of rotation,The elbow flexion is maintained
the inconvenience is often only moderate.
Surgery to regain rotation rarely succeeds.
A rotational osteotomy can give a more suitable angle of pronation–supination.
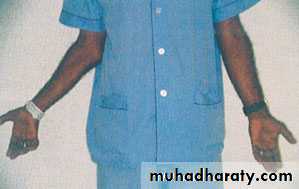
CUBITUS VALGUS
The normal carrying angle of the elbow is 5–15 degrees of valgus, anything more than this is regarded as a valgus deformitycommonest cause is longstanding non-union of a fractured lateral condyle
marked prominence of the medial condylar outline
The importance of cubitus valgus is the liability to delayed ulnar palsy
deformity no treatment, but for delayed ulnar palsy the nerve should be transposed to the front of the elbow.
ACQUIRED DEFORMITIES
CUBITUS VARUS (‘GUN-STOCK’ DEFORMITY)
most obvious when the elbow is extended and the arms are elevated.The most common cause is malunion of a supracondylar fracture
can be corrected by a wedge osteotomy of the lower humerus but this is best left until skeletal maturity.
capitulum is one of the common sites
due to repeated stress following prolonged or unaccustomed activityC/F:
a young male adolescent
aching
swelling,
signs of an effusion,
tenderness
slight limitation of movement.
intermittent locking
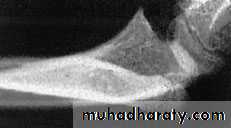
X-rays: may show fragmentation or, at a much later stage, flattening of the capitulum.
Treatment: symptomatic. However, if the fragment has separated, it should be removed. A large loose fragment which is often still partly attached can be pinned back.
OSTEOCHONDRITIS DISSECANS
due to:
Acute trauma (an osteocartilaginous fracture);Osteochondritis dissecans
synovial chondromatosis(a cluster of mainly cartilaginous ‘pebbles’)
osteoarthritis
C/F:
sudden locking and unlocking of the joint.
Symptoms of osteoarthritis
x-rays may reveal the loose body or bodies
Treatment: If loose bodies are troublesome, they should be removed
LOOSE BODIES
The elbow is affected in about 10%
Clinical features:The onset is insidious
Long hx of aching and stiffness.
The most striking physical sign is the marked Wasting
the joint is held flexed, looks swollen, and feels warm and diffusely tender; movement is considerably limited
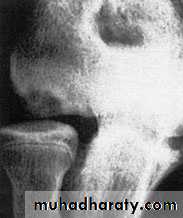
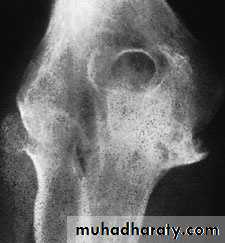
X-rays:
peri-articular osteoporosis and joint erosion.
subchondral cystic lesions.
Treatment:
General antituberculous treatment
rested until the acute symptoms subside.
movement is encouraged.
Late residual effects may justify excisional or replacement arthroplasty or (rarely) arthrodesis.
TUBERCULOSIS
The elbow is involved in more than 50 %
bilateralClinical features:
pain and tenderness,
Later the entire elbow may be swollen.
Movements are restricted
if bone destruction is marked, the joint becomes unstable.
X-ray: bone erosion, with gradual destruction of the radial head and widening of the trochlear notch of the ulna
Treatment:
general treatment,
the elbow should be splinted
Local injections of corticosteroid preparations may reduce pain and swelling
OPERATIVE TREATMENT: If synovitis persists – and more particularly if this is associated with erosion of the radial head – synovectomy with excision of the radial head is worthwhile. Progressive bone destruction and instability may call for arthroplasty
RHEUMATOID ARTHRITIS
olecranon bursa is a favourite site for gout.
C/F: :In an acute attack the area rapidly becomes painful, swollen and inflamed.DDX:
cellulitis
joint infection
IX:
serum uric acid
the bursal aspirate will contain urate crystals
Treatment: high dosage anti-inflammatory
pseudogout, due to the deposition of CPPD
GOUT AND PSEUDOGOUT
uncommon
Secondary to a previous fracture or ligamentous injury, loose bodies in the joint, longstanding occupational stress, inflammatory arthritis or gout.Clinical features:
pain and stiffness,
local tenderness,
thickening of the joint,
crepitus and restriction of movement.
ulnar nerve palsy.
X-rays: shows narrowing of the joint space with sclerosis and osteophytes. One or more loose bodies may be seen;
Treatment:
NSAID
Loose bodies, should be removed.
ulnar nerve transposition
joint replacement
OSTEOARTHRITIS
common
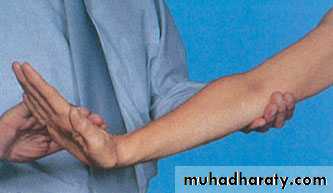
forceful repetitive wrist extensionPathology:
the extensor carpi radialis tendon
small tears, fibrocartilaginous metaplasia, microscopic calcification and a painful vascular reaction in the tendon fibres close to the lateral epicondyle.
C/F:
active individual of 30 or 40years.
Pain
aggravated by movements such as pouring out tea, turning a stiff doorhandle, shaking hands or lifting with the forearm pronated.
localized tenderness
Pain can be reproduced by passively stretching the wrist extensors or actively by having the patient extend the wrist with the elbow straight.
X-ray: is usually normal, but occasionally shows calcification at the tendon origin
TENNIS ELBOW (LATERAL EPICONDALGIA)
Treatment:
90 per cent of ‘tennis elbows’ will resolve spontaneously within 6–12 months.restrict, those activities which cause pain.
The role of physiotherapy and manipulation is uncertain.
Injection of the tender area with corticosteroid and local anesthetic relieves pain but is not curative.
OPERATIVE TREATMENT: The origin of the common extensor muscle is detached from the lateral epicondyle
similar to tennis elbow but about three times less common.
the flexor-pronator origin is affected.associated ulnar nerve neuropathy.
A medial collateral ligament injury should be excluded.
Treatment is the same as for lateral epicondylitis
outcome of surgery seems less predictable. The abnormal tissue at the flexor–pronator origin is excised,
GOLFER’S ELBOW (MEDIALEPICONDYLITIS)
The olecranon bursa sometimes becomes enlarged as a result of• continual pressure or friction; this used to be called ‘student’s elbow’. If the enlargement is a nuisance the fluid may be aspirated.
• The commonest non-traumatic cause is gout; there may be a sizeable lump with calcification on x-ray.
• In rheumatoid arthritis, also, the bursa may become enlarged, and sometimes nodules can be felt in the lump or just distal to it over the proximal ulna.
In both conditions other joints are likely to be affected as well.
A chronically enlarged bursa may prove a severe nuisance and need to be excised. However, wound healing can be a problem.
BURSITIS
may be due to
• congenital abnormalities (various types of synostosis, or arthrogryposis)• infection
• inflammatory arthritis
• osteoarthritis
• Post-traumatic
STIFFNESS OF THE ELBOW
The causes: are either
extrinsic (e.g. soft-tissue contracture or heterotopic bone formation),intrinsic (e.g. intra-articular adhesions and articular incongruity),
or a combination of these.
Most of the activities of daily living can be managed with flexion from 30 to 130 degrees and pronation and supination of 50 degrees each.
NON-OPERATIVE TREATMENT
Prevention by early active movement through a functional range.
serial splintage
POST-TRAUMATIC STIFFNESS
OPERATIVE TREATMENT:
The indication is failure to regain a functional range of movement at 12 months
The objectives are determined by the type of pathology.
Heterotopic bone can be excised.
Capsular release or capsulectomy (open or arthroscopic),
fixing of ununited fractures or correction of malunited fractures.
Post-traumatic radio-ulnar synostos is treated by resection when the synostosis has matured (this takes about one year) followed by diligent physiotherapy
Apley’s System of Orthopaedics and Fractures
Review of Orthopedics, MillerCampbell’s operative orthopaedics