
AFTER MID
TOTAL LEC: 13
Dermatology
Psoriasis
DR. SABEEH LEC: 1
Dr. Sabeeh


Dermatology
Dr. Sabeeh, Lec 1
February 24, 2016
Psoriasis
الصدفية
Objectives :
• Discuss definition and epidemiology of psoriasis
• Explain causes and aggravating factors of psoriasis
• Describe clinical signs of psoriasis
• List topical and systemic treatment options including side effects
Psoriasis
Psoriasis is a genetic, immunologically-mediated systemic disease primarily
affecting skin and joints.
It is a chronic, incurable, debilitating disease that profoundly affects the
quality of life of patients and their families.
How common is Psoriasis?
2% of population,
Racial variation,
Affects men and women equally,
Two age groups of onset —> Late teens to early 20s.
Aetiology :
Genetic, environmental and immunological.
1. Family history (30%)
70% concordance MZ twins.
20 % DZ twins.
HLA - CW6.
2. Environmental Factors
Triggering factors :
External factors may provoke psoriatic lesion
✴Physical trauma (Koebner s phenomenon1872)
✴Infections 1- Strep. tonsillitis 2- Viral HIV.
✴Climate and sun lights
✴Stress
LEC : 1
!1
✴Drugs
Antimalarial, B-bloker, Lithium
Withdrawal of systemic steroid (so important)
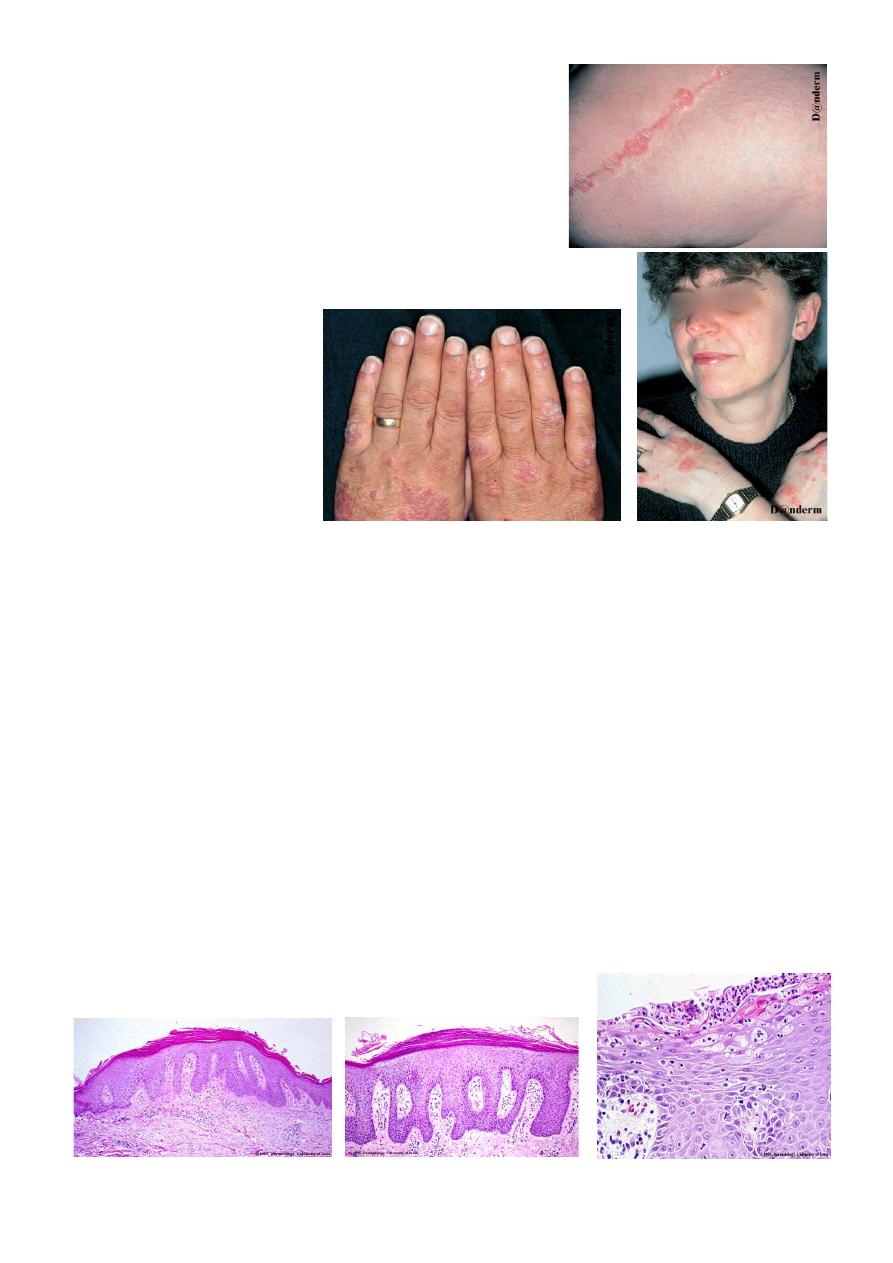
Koebner’s phenomenon
( as shown in the pictures )
• Production of the same lesion after trauma
• Lichen planus, vitiligo, viral warts, behchet disease,
• 25% of patients,
• poor prognosis,
• Reverse K phenomenon.
3. Immunological Factors
Evidence
• Cyclosporin immunosupressor.
• Bone marrow transplant of psoriatic donor.
• Activated T-lymphocyte increase number in dermis producing interluekin 12 and 17.
• And tumor necrosis fator TNF.
Pathophysiology :
• Rapid turn over of cell proliferation of the basal cell layer excessive but controlled
3 days.
• Two fold increase in proliferative cell population.
Immune system
Increase activation of T cells
Histopathology :
LEC : 1
!2
* Sunlight exposure
1.
2.
3.

Auspitz sign :
(so important)
• Silvery scale.
• Membrane like layer.
• Pin point bleeding.
Types of Psoriasis :
Chronic plaque psoriasis (90%).
(most common)
Palmoplantar psoriasis.
Flexural psoriasis.
Guttate psoriasis.
(good prognosis)
Erythrodermic psoriasis.
Pustular psoriasis.
Clinical types :
1. Psoriasis vulgaris
or
chronic plaque psoriasis
commonest, *any age,
*young, *extensor.
2. Guttate Psoriasis :
*children, *strept., *small papule, *red scaly,
• Treatment : treat infection.
LEC : 1
!3
Guttate Ps
( cont. )
• More common in children / adolescents.
• Acute streptococcal infection.
• Rain drop-like lesions.
• Self-resolving (months).
• May precede chronic psoriasis.
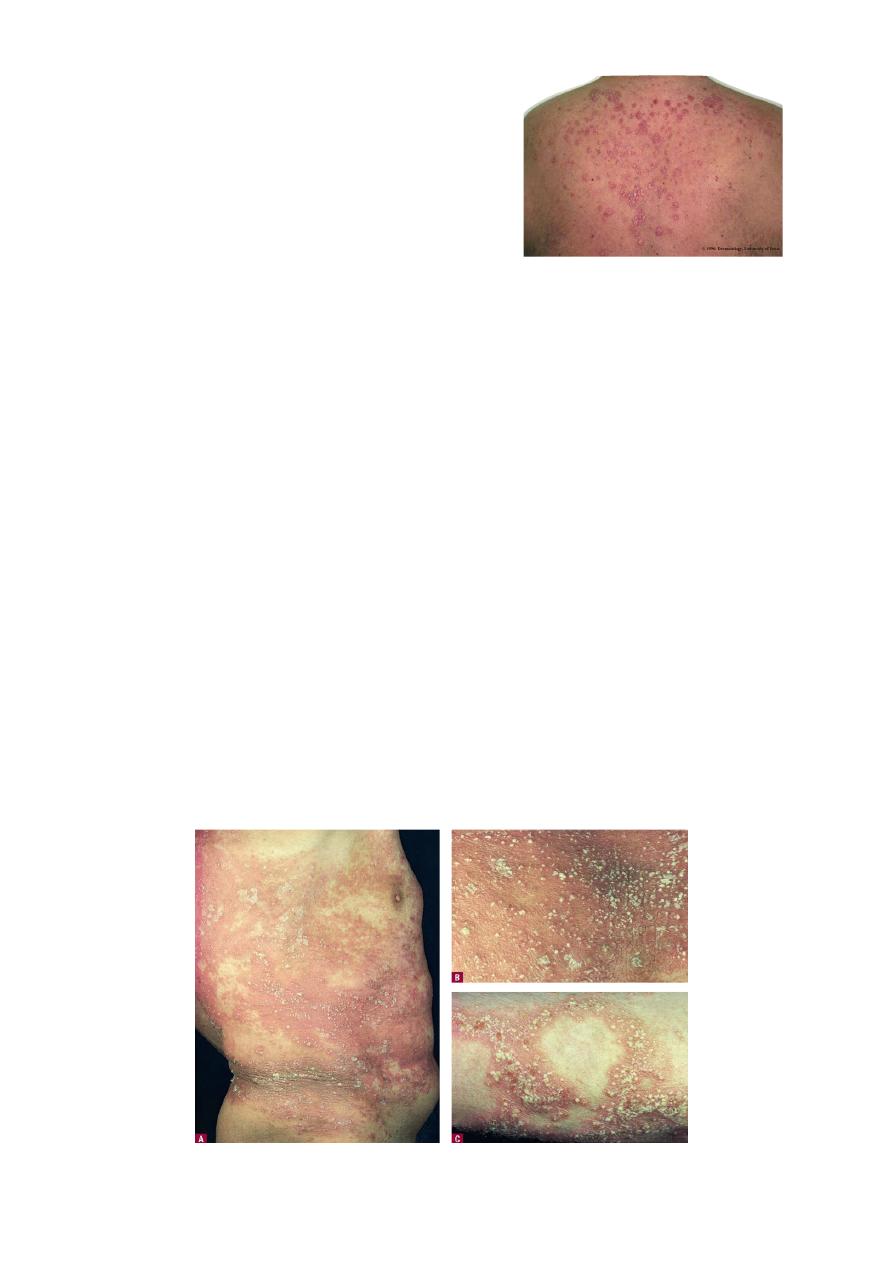
3. Pustular psoriasis :
Localised Palmoplantar
•
Commoner in females
• Adults
• Associated with smoking
• Distinct from ordinary psoriasis
• Symmetrical
Generalised Palmoplantar
• Rare.
• Acute generalised pustular psoriasis (von Zumbusch).
• Can occur with ordinary psoriasis.
• Precipitated by steroid withdrawal.
• Sheets of pustules, background erythema.
• May be systemically unwell.
✦ In generalised pustular clinical type of psoriasis
Site involved
—> *trunk, *extremities, *nail, *palm, *sole.
Can develop
—> *toxic fever, *leucocytosis, *loss of appetite.
The following drugs are used for treatment of pustular Ps. *etretinate,
*dapsone.
LEC : 1
!4
Generalised Pustular Ps.

4. Erythrodermic psoriasis :
Erythroderma – more than 90% body surface area.
• Uncommon.
• Most likely preceding history of psoriasis.
• May not have other features psoriasis.
• May be systemically ill.
✦ Erythrodermic or Exfoliative psoriasis
• Whole body, Face.
• Other CAUSES of erythroderma *eczema, *drugs, *malignancies,
*ichthyosis.
• Metabolic changes : hypoprotienemia, Iron deficiency anemia, vitamins
deficiency, hypothermia, hyperkinetic condition may lead to heart
failure, electrolyte disturbance.
5. Flexural psoriasis :
• Axilla, groin.
• Diffuse erythematous oozy, affecting the vault.
• Differentiate from tinea —> *active border, *clear vault, *+ve scraping.
6. Psoriatic arthritis
½ have HLA B-27
sero –ve RF ANF
with or without skin lesions
• Poly arthitis, rheumatoid like.
• Mono arthritis, like pyogenic arthritis.
• Axial skeleton, ankyloing spondylitis like.
• Arthritis mutilans, complete destruction of small joints of hand.
LEC : 1
!5

Psoriasis - Nails
•
Nail pitting.
•
Onycholysis.
•
Subungal hyperkeratosis.
Prognosis
!
Bad
early onset, +ve family history, generalized, koebner +ve.
✔
Good
guttate, reverse koebner.
Management Psoriasis
• Education
• Topical treatment
• Phototherapy
• Systemic treatment
1
st
Line : Topical treatment
• Emollients e.g. E45
• Vitamin D3 analogues (e.g.Calcipotriol)
• Topical corticosteroids
• Keratolytics e.g. 5% Salicylic acid
• Coal tar
• Dithranol (Short contact, dithrocream)
LEC : 1
!6
Onycholysis
subungal
hyperkeratosis
Onycholysis
Pitting

• Emollients
Reduces scale and dryness
Thick preparations can give folliculitis
• Vitamin D analogues
Calcipotriol
Irritation / hypercalcaemia
• Topical steroids
Skin atrophy
• Coal tar
Messy, folliculitis, irritation
• Dithranol
Irritation, stains skin
2
nd
Line : Phototherapy
• UVB (narrowband UVB)
• UVA plus tablets (8 methoxy
p
soralen)
=
P
UVA
Side effects
1- Erythema / pruritis.
2-Nausea (PUVA). 3-L/T – Skin cancer
* Management of erythrodermic psoriasis and generalised pustular psoriasis
• Admit.
• supportive treatment with careful monitoring of BP, temperature and urine output.
• Emollients and mild topical steroids.
• Consider systemic treatment.
3
rd
Line : Systemic treatment
* Mode of Action
• Methotrexate
Folic acid antagonist.
Selective inhibition of rapidly dividing cells.
• Ciclosporin
Suppression of T lymphocytes.
Blocks production of lymphokines.
• Acitretin
Vitamin A derivative.
Suppresses DNA synthesis and cell differentiation.
LEC : 1
!7

* Side effects
• Methotrexate
Teratogenicity, nausea and GI upset.
Liver fibrosis, marrow suppression.
LFT and CBP.
• Ciclosporin
Hypertrichosis, gym hypertrophy, tingling peripheries, carcinogenesis.
Hypertension, nephrotoxicity.
*
Blood pressure, blood urea serum creatinine.
• Acitretin
Teratogenic, dry skin and lips.
Hyperlipidaemia, hepatotoxicity.
*
Fasting lipids, LFTs.
Biological therapy
• Target T lymphocyte
• Target TNF
What is the prevalence of psoriasis in the western world?
A. 8%
B. 15%
C. 2%
What % of patients with psoriasis have a positive family history?
A. 10%
B. 30%
C. 70%
How could you treat Psoriasis on the face?
A. Mild steroid
B. Vitamin D analogues
C. Coal tar
D. Dithranol
What is the most common type of psoriasis?
A. Chronic plaque psoriasis
B. Palmoplantar psoriasis
C. Flexural psoriasis
D. Guttate psoriasis
E. Pustular psoriasis
LEC : 1
!8



