0
Mustafa Hatim Kadhim
Baghdad University
Al-kindy college of medicine
Third Stage
2013 - 2014
Practical Medicine
1
History Taking
Personal Data
Name
Age
Residency
Occupation
Marital Status
Date of Admission (DOA)
Chief Complaint:
What brought patient to hospital? (In patient's own words)
Duration: hours, days, weeks and months or years.
History of the present illness:
Story of the disease in chronological way using medical
terms (medical Language.) elaborate more on the system
(s) involved.
Systemic review – Systematic inquiry
General health:
Well-being, Appetite, Weight change, Energy, Sleep, Mood
Cardiovascular system
Chest pain on exertion (angina)
Breathlessness
Lying flat (Orthopnoea)
At night (Paroxysmal nochrnal dyspnoea)
On minimal exertion – record how much
Palpitation
Pain in legs on walking (claudication)
Ankle swelling
Respiratory system:
Shortness of breath (exercise tolerance)
Cough
Wheeze
Sputum Production (colour, amount)
Blood in Sputum (hemoptysis)
Chest pain (due to inspiration or Coughing)
Gastrointestinal system:
Mouth (oral ulcers, dental problem)
Difficulty swallowing (dysphagia- distinguish from
pain on swallowing, odynophagia)
Nausea and Vomiting
Vomiting blood (haematemesis)
Indigestion
Heartburn
Abdominal pain
Change in bowel habit
Change in color of stools (Pale dark, tarry black, fresh
blood)
Genitourinary system:
Pain passing urine (dysuria) frequency
Passing urine (at night nocturia)
Blood in the urine (haematuria)
Sexual partners- Unprotected intercourse
Men if appropriate:
Prostatic symptoms including difficulty
Starting - hesitancy
Poor stream or flow
Terminal drippling
Incontinence
Urethral discharge
Libido
Erectile difficulties
Women:
Last menstrual period (consider pregnancy)
Timing and regularity of periods
Length of periods
Abnormal bleeding
Vaginal discharge
Contraception
If appropriate
Libido
Pain during intercourse (dysparonia)
Incontinence (stress and urge)
Nervous system:
Headaches
Dizziness (vertigo or light – headed)
Faints
Fits
Altered sensation (numbness or tingling "Paresthesia")
Weakness
Visual disturbance
Hearing problems (deafness, tinnitus)
Musculoskeletal:
Joint pain, stiffness or swelling
Mobility
Falls
Endocrine:
Heat or cold intolerance
Change in sweating
Excessive thirst (polydipsia)
Practical Medicine
2
Other
Bleeding or bruising
Skin rash
Past History:
There is often a relationship between past medical history
and the presenting problem.
Drug History:
Ask about prescribed drugs and any other
Medications your patient is taking.
Family History:
Obtain the family history by asking open – ended questions,
e.g Are there any illness that run in your family?
Pedigree chart
Social History:
Focus on the relevant issues
Occupational History:
You should take a full occupational history from all patients
Travel History:
Travel related illness
Sexual History:
If it is relevant
When you think you have got all the information from the
patient and before you examine the patient :
Briefly summarize what the patient has told you.
Reflects this back to the patient. This allows the patient to
Correct anything you have misunderstood
Add anything that may have been forgotten
Tell the patient what you are going to do next.
_____________________________________
You are learning to be able to understand, diagnose
and help people. For most of us this is the reason we
became doctors.
NOTE
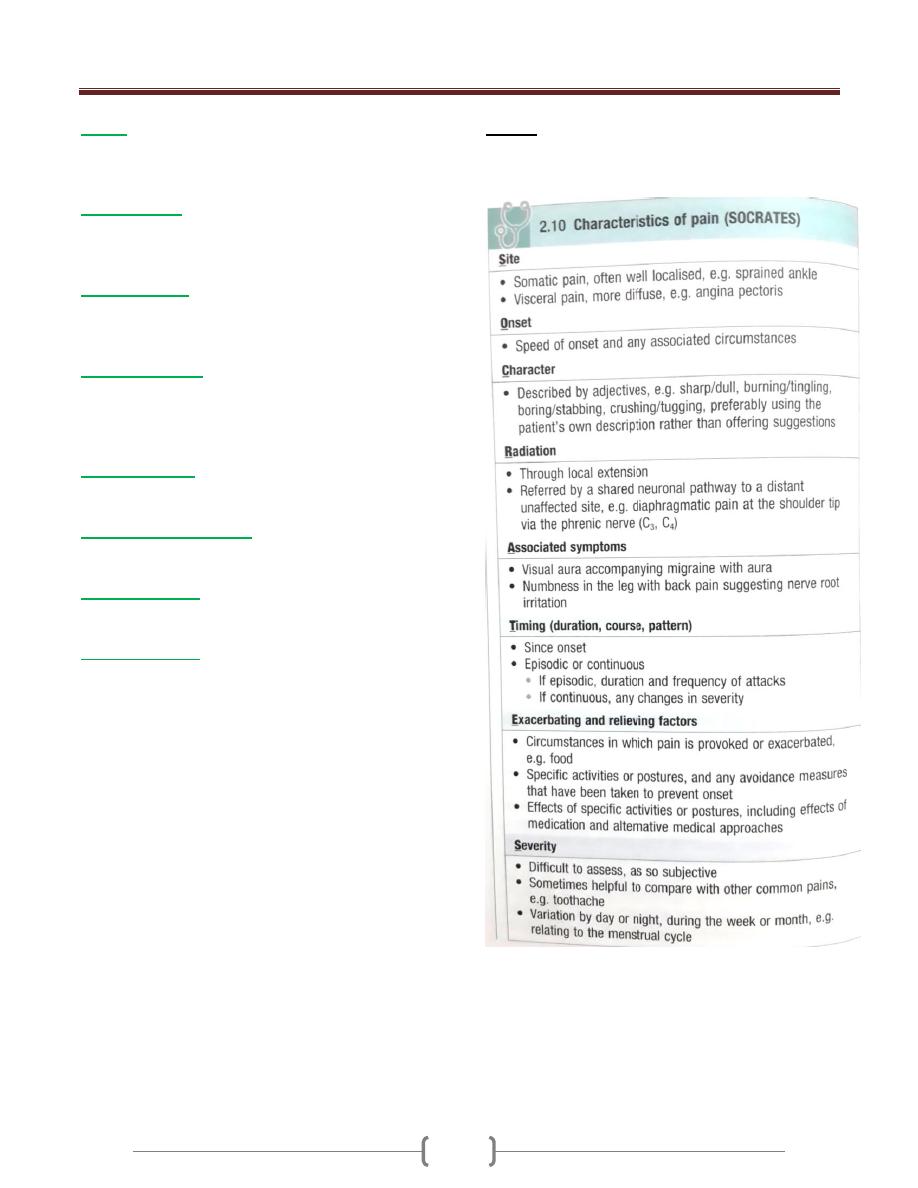
If there is pain in the history you must ask about the
characteristics of pain (SOCRATES)
