0
Mustafa Hatim Kadhim
Baghdad University
Al-kindy college of medicine
Third Stage
2013 - 2014
1
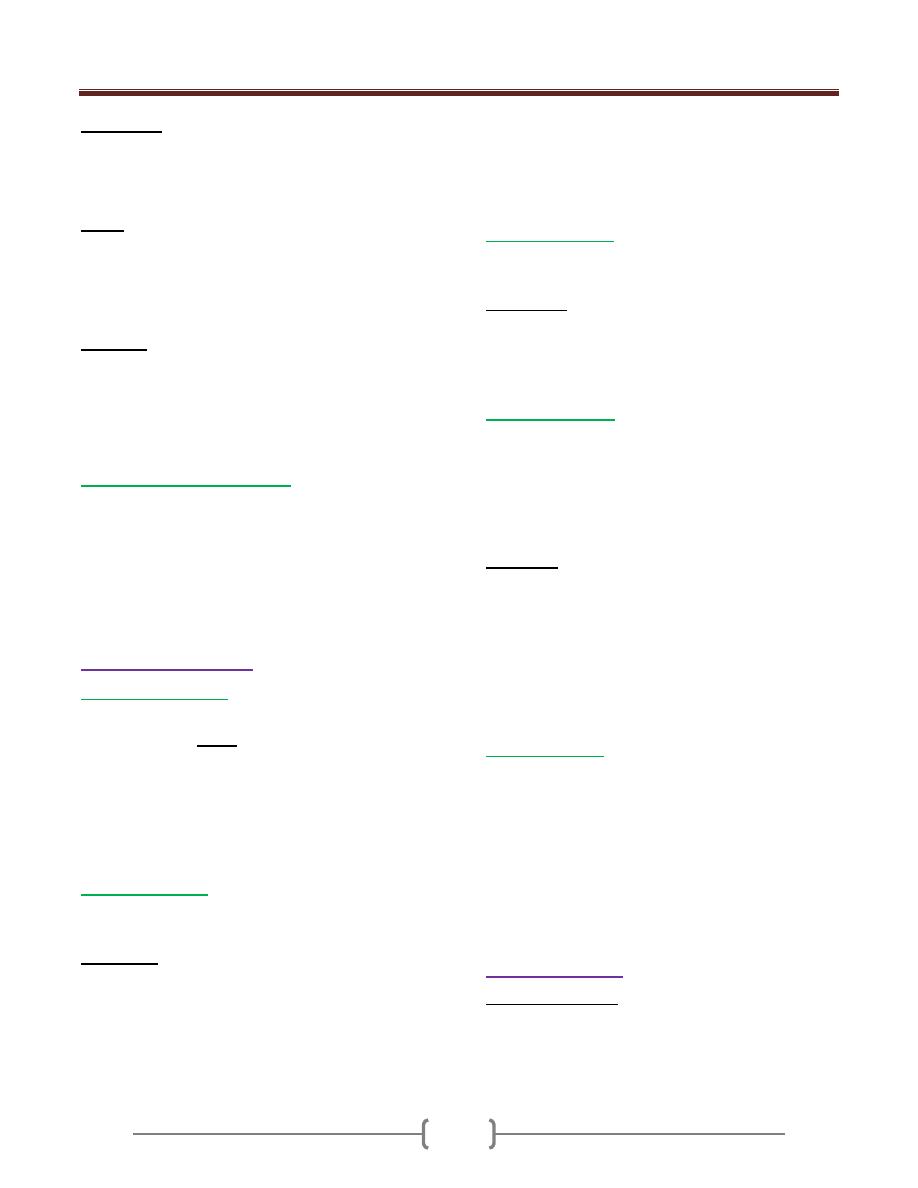
List of contents
الفصل االول
Lecture
number
Lecture name
Doctor name
Page
number
1
Introduction
دكتور زهير
3-6
2
The body response to trauma
دكتور
ليث نايف
7-11
3+4
Wounds, tissue repair and scars
دكتور
عماد
12-19
5+6
Hemorrhage & Shock
دكتور
عبد الهادي
20-23
7
Blood Transfusion
دكتور
توفيق
24-30
8+9
Fluid electrolytes & Acid-Base
balance
دكتور
رائد
31-48
10+11
Operating Room Sterilization
& Sterile precautions
دكتور
حميد
49-51
12+13
Burn
دكتور
احمد كمال
52-55
الفصل الثاني
Lecture
number
Lecture name
Doctor name
Page
number
1
Wound infection
دكتور
ممتاز
57-58
2+3
Cyst, Ulcer, sinuses & Fistulas
دكتور
ابتسام
59-62
4+5+6
Oncology
دكتور زهير
63-66
7+8
Artificial nutritional support
دكتور
ليث نايف
67-75
9
Vascular Surgery
دكتور
مثنى
العسل
77-78

2
Lecture 1 - Introduction to Surgery
3
Surgical diagnosis depends on: Sound knowledge of:
Anatomy
Physiology
Pathology
Specific history & clinical examination
Radiology
Surgical history
History of the chief complaint is the key step in surgical
diagnosis.
There is no standard surgical history of each disease as
the disease may present with certain symptoms and the
other patient present with the other or part of it as their
symptoms may take time to appear or never appear.
There are 2 types of surgical history:
1) Outpatient or emergency room history; Specific complaint
of the patient is pinpointed.
Objective: is to obtain diagnosis on which treatment is
ordered.
2) Clerking history: is the history of the patients who was
admitted for an elective surgery.
Objective: is to assess that the treatment planned is
correctly indicated & to ensure that the patient is suitable
for that operation
Outpatient or emergency room history:
You may ask
When the symptom started.
How it has progressed.
Whether there are any associated symptoms.
Whether the symptoms are improving or getting worse.
What relieve & what aggravate the symptoms.
What were the effects of the drugs which were taken.
History of previous illnesses, concurrent illnesses.
Drug therapy.
Allergies.
Complications related to anesthesia.
Clerking history
The clerking history centers on direct questioning of the
patient about specific points related to the complaint.
Examples:
1) Ask about signs of prostatism in patients with benign
prostatic hypertrophy to compare them with postoperative
state to assess the effect of the surgical procedure.
2) In a patient who was referred by a physician :
Ask about the indications for surgery.
The surgeon's decision whether or not the patient will
benefit from the operation.
These are particularly important in patients with non-
malignant condition where continued medical
treatment is an option.
Clinical Examination
Examine the whole patient particularly before operation.
The examination should be as thorough as in a routine
medical examination.
In examining a specific surgical structure one should
follow an accurate clinical description for example in :
Diagnosis of lump:
1) Site, size, shape, surface, consistency , mobility.
2) Important physical signs these includes:
Thrill, sign of compression, sign of indentation, sign of
aneurysm (pulsatile masses).
Ulcer:
Site, size, shape, floor, base, edge &surrounding tissues.
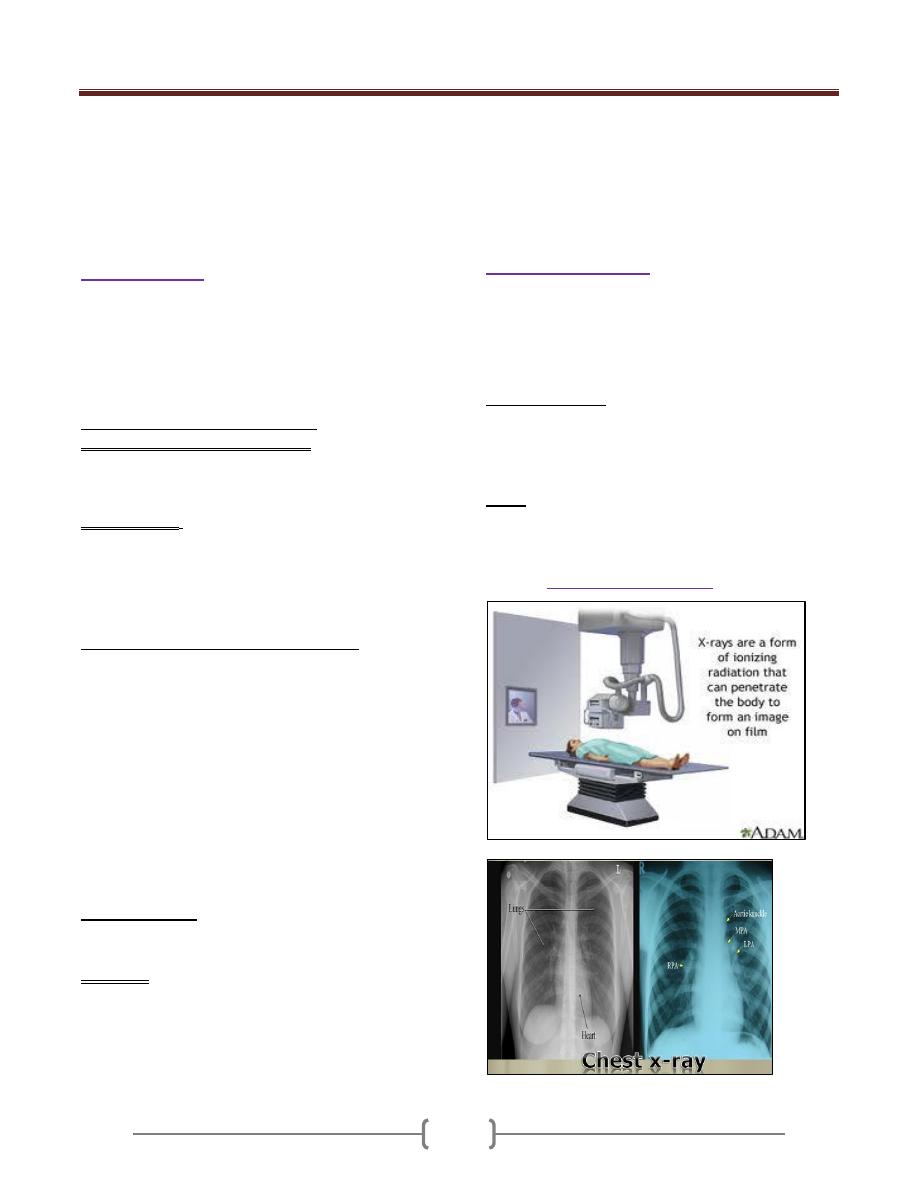
Confirmation of the diagnosis could be done by:
(Diagnostic
Radiology or imaging
)
Lecture 1 - Introduction to Surgery
4
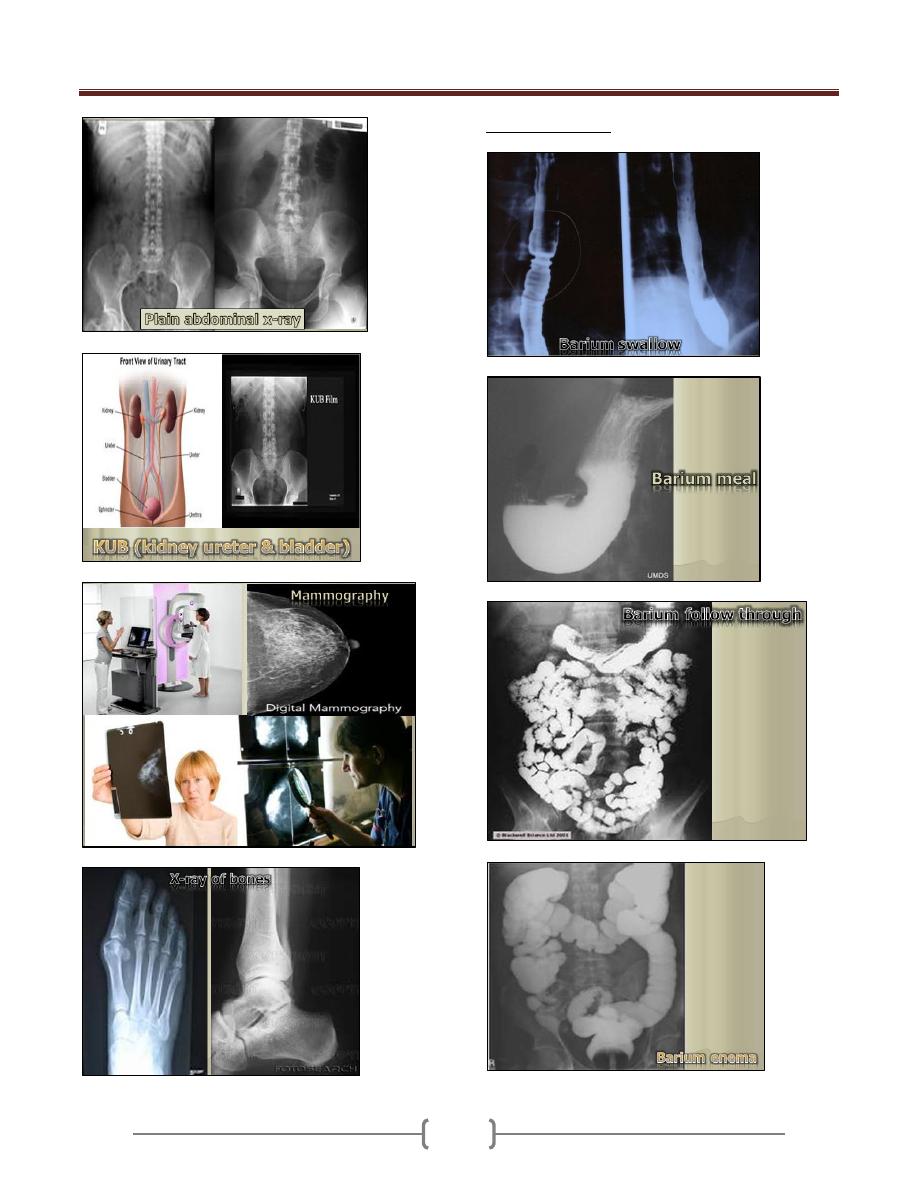
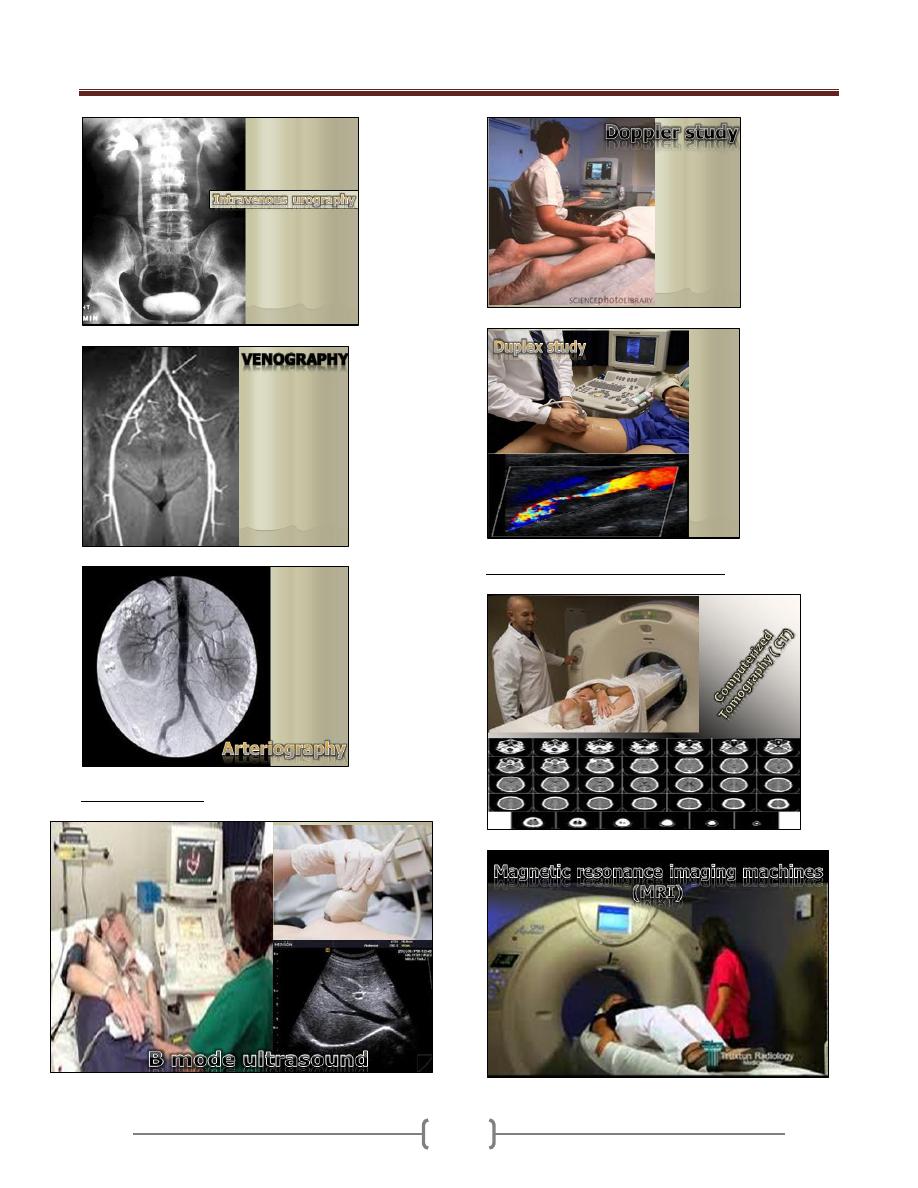
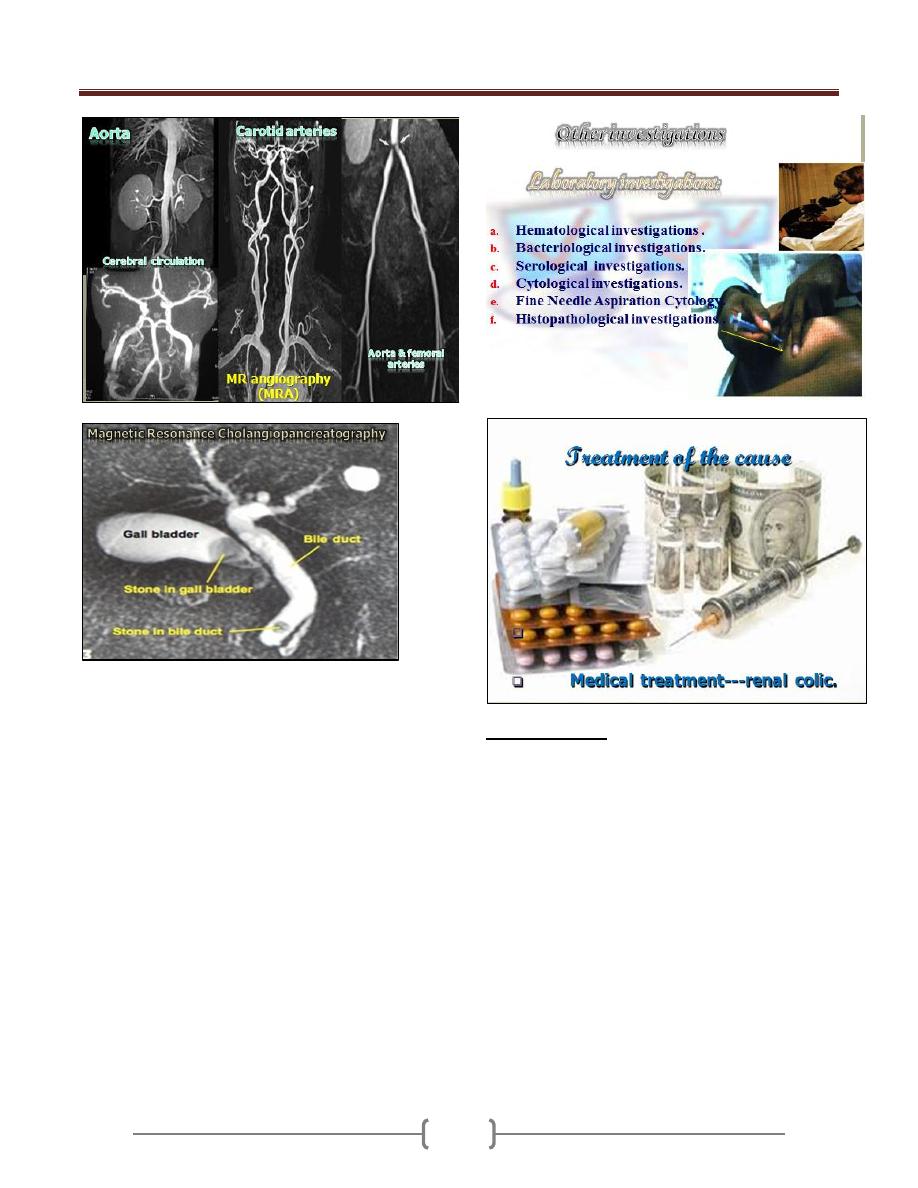
B. Contrast Studies
Lecture 1 - Introduction to Surgery
5
Ultrasound Studies
Advanced Radiological investigations
Lecture 1 - Introduction to Surgery
6
Surgical treatment
Appendectomy
Cholecystectomy
Drainag e of an abscess
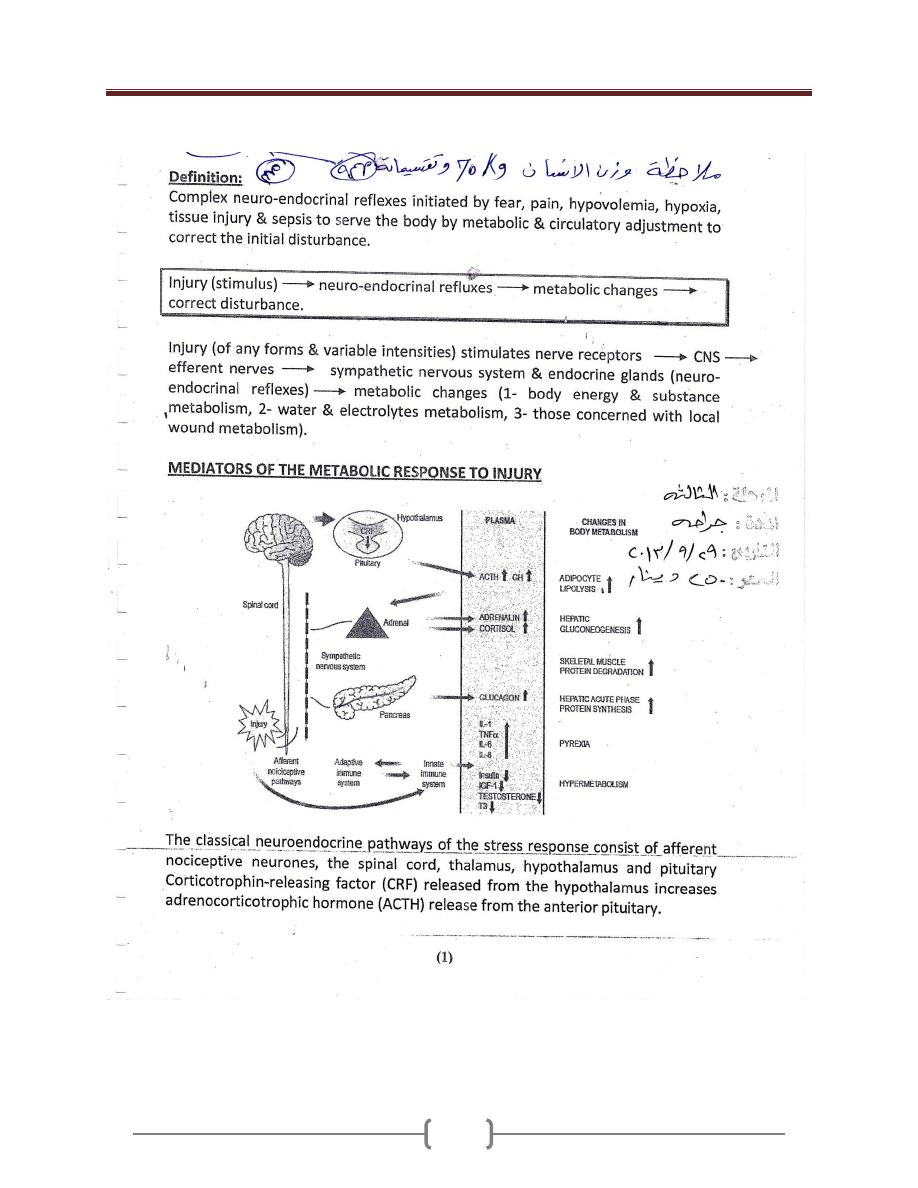
Lecture 2 – Body Response to trauma
7
Lecture 2 – Body Response to trauma
8
Lecture 2 – Body Response to trauma
9
Lecture 2 – Body Response to trauma
10
Lecture 2 – Body Response to trauma
11
Lecture 3+4 - Wounds, tissue repair and scars
12
Lecture 3+4 - Wounds, tissue repair and scars
13

Lecture 3+4 - Wounds, tissue repair and scars
14
Lecture 3+4 - Wounds, tissue repair and scars
15
Lecture 3+4 - Wounds, tissue repair and scars
16
Lecture 3+4 - Wounds, tissue repair and scars
17
Lecture 3+4 - Wounds, tissue repair and scars
18
Lecture 3+4 - Wounds, tissue repair and scars
19
Lecture 5+6 – Hemorrhage & Shock
20
Hemorrhage
Haemorrhage or bleeding is the loss of blood from the
circulatory system. It must be recognized & managed
aggressively to avoid multiple organ failure & death. It
must be treated first by arresting it, then other measures
like fluid resuscitation & blood transfusion.
Pathophysiology
Haemorrhage may lead to hypovolaemic shock
(hypoperfusion), the following events may occur:
Cellular anaerobic metabolism with lactic acidosis
(this acidosis causes coagulopathy & further
haemorrhage).
Ischaemic endothelial cells activate anti-coagulant
pathways & further haemorrhage.
Underperfused muscles are unable to generate heat so
hypothermia results which affects coagulation &
results in further haemorrhage.
These events result in a vicious cycle leading to
physiological exhaustion & death.
Medical therapy has a tendency to worsen the conditio
Intravenous fluids & blood are cold, so causes
hypothermia.
Many crystalloid fluids are acidic (normal saline has a
PH of 6.7).
Surgery causes heat loss (by opening body cavities) &
causes further haemorrhage.
Types of haemorrhage
1) Revealed & concealed haemorrhage :
Revealed haemorrhage: Obvious external haemorrhage.
eg. bleeding from open arterial wound, haematemesis
from DU.
Concealed haemorrhage: It is contained within body
cavity. It must be diagnosed & treated early, eg.
Abdominal (peritoneal & retroperitoneal), thoracic, &
pelvic bleeding due to trauma. Non-traumatic cause eg.
ruptured aortic aneurysm, occult GI bleeding.
2) Primary, reactionary, & secondary haemorrhage:
Primary hemorrhage: Occurring immediately as a result
of injury or surgery.
Reactionary (Delayed) haemorrhage : Occurring within
24 hours. Usually caused by dislodgement of clot (by
resuscitation, vasodilatation, normalization of BP) or due
to a slippage of a ligature.
Secondary haemorrhage: It usually occurs within 7 – 14
days after injury. It is precipitated by infection, pressure
necrosis (such as from a drain), or malignancy.
3) Surgical & non-surgical haemorrhage
Surgical haemorrhage: Result from direct injury; it is
amenable to surgical control.
Non-surgical haemorrhage: Result from oozing from
raw surfaces due to coagulopathy. It requires correction of
coagulation abnormalities or packing.
Hemorrhag is broken down into 4 classes by the
American College of Surgeons' Advanced Trauma Life
Support
1) Class I Hemorrhage involves up to 15% of blood
volume. There is typically no change in vital signs and
fluid resuscitation is not usually necessary.
2) Class II Hemorrhage involves 15-30% of total blood
volume. A patient is often tachycardic (rapid heartbeat)
with a narrowing of the difference between the systolic
and diastolic blood pressures. The body attempts to
compensate with peripheral vasoconstriction. Skin may
start to look pale and be cool to the touch. Volume
resuscitation with crystalloids (Saline solution or Lactated
Ringer's solution) is all that is typically required. Blood
transfusion is not typically required.
3) Class III Hemorrhage involves loss of 30-40% of
circulating blood volume. The patient's blood pressure
drops, the heart rate increases, peripheral perfusion, such
as capillary refill worsens, and the mental status worsens.
Fluid resuscitation with crystalloid and blood transfusion
are usually necessary.
4) Class IV Hemorrhage involves loss of >40% of
circulating blood volume. The limit of the body's
compensation is reached and aggressive resuscitation is
required to prevent death
Lecture 5+6 – Hemorrhage & Shock
21
Management of haemorrhage
1) Identify haemorrhage: Revealed haemorrhage may be
obvious but the diagnosis of concealed haemorrhage may
be difficult. Any shock should be assumed to be
hypovolaemic until proved otherwise & the cause should
be assumed haemorrhage until this has been excluded.
2) Immediate resuscitation:
Direct pressure should be placed over the site of external
haemorrhage .
Airway & breathing should be assessed & controlled.
Large- bore intravenous access should be instituted &
blood drawn for cross- matching.
Intravenous fluids should be given, & when the blood is
available it should be given according to the degree of
haemorrhage.
3) Identify the site of haemorrhage:
This is important to define the next step in haemorrhage
control (operation, endoscopic control,
angioembolization).
• History: Previous episodes, known aneurysm, drugs
(steroidal & nonsteroidal anti-inflammatory).
• Physical examination: Nature of blood : fresh, melaena,
external signs of injury, abdominal tenderness.
• Investigations: Must be appropriate to the patients
physiological condition, & unnecessary investigations
must be avoided. Chest & pelvic radiography, abdominal
ultrasound, diagnostic peritoneal aspiration.
4) haemorrhage control:
Control must be achieved rapidly by moving the patient
rapidly to a place of haemorrhage control (theater,
angiography or endoscopy suites). Patient needs
lifesaving procedure so surgery may need to be limited to
the minimum necessary to stop bleeding & control sepsis.
More definitive repairs can be delayed until the patient is
physiologically capable of sustaining the procedure
(Damage control surgery).
Shock
Shock is the most important cause of death among
surgical patients.
Definition: It is a systemic state of low tissue perfusion,
which is inadequate for normal cellular respiration.
Pathophysiology
1) Cellular
Tissue perfusion is reduced,
cells are deprived of oxygen
anaerobic metabolism occurs
Liberation of lactic acid (instead of carbon dioxide)
causes systemic metabolic acidosis .
As glucose within the cells exhausted anaerobic
respiration ceases
failure of sodium potassium pump in the cell membrane
& intracellular organelles.
Intracellular lysosomes release autodigestive enzymes &
cell lysis ensues.
Intracellular contents including potassium are released
into the blood stream causing hyperkalaemia.
2) Microvascular
Tissue ischemia activate immune & coagulation
systems.
Hypoxia & acidosis activate complement & prime
neutrophils resulting in the generation of oxygen free
radicals & cytokine release.
These lead to injury to capillary endothelial cells &
further activation of the immune & coagulation
systems.
The damaged endothelium becomes leaky, so fluid
leaks & tissue oedema ensues, exacerbating cellular
hypoxia.
3) Systemic
a) Cardiovascular: Decreased preload & afterload cause
compensatory baroreceptor response which leads to
increased sympathetic activity & release of
catecholamines into the circulation which results in
tachycardia & systemic vasoconstriction (except in sepsis)
Lecture 5+6 – Hemorrhage & Shock
22
b) Respiratory: The metabolic acidosis & increased
sympathetic activity result in an increased respiratory rate
& minute ventilation to increase the excretion of carbon
dioxide & this produces compensatory respiratory
alkalosis.
c) Renal: Decreased perfusion pressure in the kidney leads
to reduced filtration at the glomerulus & a decreased urine
output.
The renin-angiotensin-aldosterone axis is stimulated
resulting in further vasoconstriction & increased sodium
& water reabsorption by the kidney.
d) Endocrine: Antidiuretic hormon (vasopressin) is released
from hypothalamus & results in vasoconstriction & water
reabsorption in the renal collecting system.
Cortisol is also released from the adrenal cortex causes
sodium & water reabsorption & sensitising the cells to
catecholamines.
4) Ischemia-perfusion syndrome
Systemic hypo-perfusion causes tissue hypoxia which
activates complement, neutrophils, & microvascular
thrombi which cause further endothelial damage to
organs such as the lungs & kidneys.
The acid & potassium load cause myocardial
depression, vascular dilatation & further hypotension.
These events cause multiple organ failure.
Classification of shock
1) Hypovolemic shock:
It is the most common form of shock, caused by reduced
circulating volume due to
a) haemorrhagic causes
b) Non-haemorrhagic causes: poor fluid intake, excessive
fluid loss because of vomiting, diarrhea, urinary loss
(as in diabetes), evaporation & third- spacing (fluid is
lost into GIT & interstitial spaces as in bowel
obstruction or pancreatitis.
2) Cardigenic shock
It is due to primary failure of the heart to pump blood to
the tissues.
It occurs in:
a) myocardial infarction
b) dysrhythmias
c) valvular heart disease
d) blunt myocardial injury
e) cardiomyopathy
f) Myocardial depression: results from endogenous
factors released in sepsis & pancreatitis or exogenous
factors such as drugs.
3) Obstructive shock
Mechanical obstruction of cardiac filling causes reduction
of preload & fall in cardiac output.
It occurs in :
a) cardiac tamponade
b) tension pneumothorax
c) massive pulmonary embolism
d) Air embolism.
4) Distributive shock
There is abnormally high cardiac output with
vasodilatation & hypotension. There is maldistribution of
blood flow at a microvascular level with arteriovenous
shunting & dysfunction of the cellular utilization of
oxygen. The peripheries are worm & capillary refill is
brisk despite profound shock.
It occurs in
a) Septic shock: caused by release of endotoxins &
acivation of cellular & humoral components of the
immune system.
b) Anaphylaxis: vasodilatation is caused by histamine
release.
c) Spinal cord injury (neurogenic shock): caused by
failure of sympathetic outflow & adequate vascular
tone.
5)
Endocrine shock
: It occurs in:
a) hypo- & hyperthyroidism
b) Adrenal insufficiency.
In hypothyroidism there is disordered vascular & cardiac
responsiveness to circulating catecholamines so cardiac
output falls & there may be associated cardiomyopathy.
Hyperthyroidism may cause a high- output cardiac failure.
In adrenal insufficiency there is hypovolaemia & poor
response to circulating & exogenous catecholamines, it
occurs in Addisons disease, & systemic sepsis.
Severity of shock:
1) Compensated shock: There is a compensatory
cardiovascular & endocrine response to maintain adequate
blood flow to the most vital organs (brain, heart, lungs, &
kidneys) & reducing perfusion to the skin, muscles, &
Lecture 5+6 – Hemorrhage & Shock
23
GIT. Apart from tachycardia & cool peripheries
(vasoconstriction) there may be no other clinical signs of
hypovolaemia. Loss of 15% of the circulating blood
volume is within normal compensatory mechanism.
Blood pressure is only falls after 30-40% of circulating
volume has been lost.
2) Decompensation: Further loss of circulating volume
causes progressive cardiovascular, respiratory, & renal
decompensation.
3) Mild shock: Initially there is tachycardia, tachypnoea &
mild reduction in urine output with mild anxiety. Blood
pressure is maintained although there is a decrease in
pulse pressure. The peripheries are cold & sweaty with
prolonged capillary refill times (except in septic
distributive shock).
4) Moderate shock: As shock progresses, renal
compensatory mechanisms fail, renal perfusion falls &
urine output decreases below 0.5 ml/kg/h. There is further
tachycardia & blood pressure starts to fall. Patients
become drowsy & mildly confused.
5) Severe shock: There is profound tachycardia &
hypotension. Urine output falls to zero & patients are
unconscious with labored respiration.
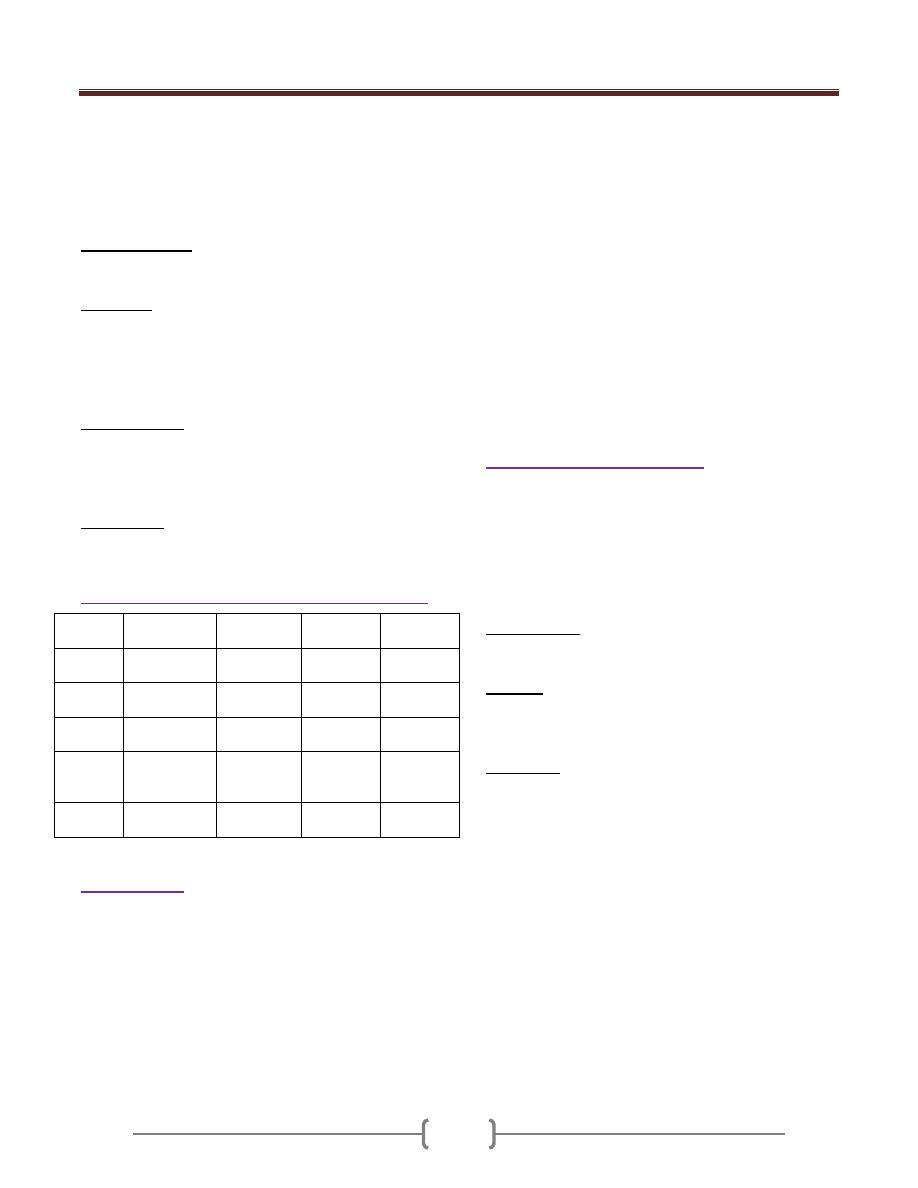
Cardiovascular and metabolic characteristics of shock
Hypovolaemia
Cardiogenic
Obstructive
Distributive
Cardiac
output
Low
Low
Low
High
Vascular
resistance
High
High
High
Low
Venous
pressure
Low
High
High
Low
Mixed
venous
saturation
Low
Low
Low
High
Base
deficit
High
High
High
High
Resuscitation
Should be rapid.
If there is doubt about the cause of shock it is safer to
assume the cause is hypovolaemia & begins with fluid
resuscitation followed by an assessment of the response.
If the general condition of the patient permits, rapid
clinical examination is performed.
In patients who are actively bleeding the resuscitation
should proceed parallel with surgery.
1) Ensure a patent airway & adequate oxygenation &
ventilation.
2) Intravenous access (with short wide- bore catheter) &
blood sample aspirated for cross-matching & blood
should be requested.
3) Intravenous administration of the available fluids
(crystalloid or colloid) while waiting blood Blood
transfusion should be done as early as possible.
4) Vasopressor agents (phenylephrine, noradrenaline) are
used in distributive shock in which there is peripheral
vasodilatation with hypotension despite high cardiac
output.
In cardiogenic shock or when myocardial depression
complicates a shock state inotropic therapy may be
needed to increase cardiac output & therefore oxygen
delivery. The inodilator dobutamine is the drug of choice.
Management of septic shock
1) Admission to intensive care unit of hospital.
2) Care of airway and breathing. Giving oxygen, and may
need mechanical ventilation.
3) Intravenous fluid (Crystalloid or colloid).
4) Antibiotic.
5) Taking history when the condition of patient permits.
6) Control of diabetes.
7) Investigations: Hb, WBC count, RBS, S. electrolytes, B.
urea, S. creatinin. Blood, urine and pus culture may be
needed. Chest X-ray.
8) Surgery: Drainage of pus, gangrene of limb may need
amputation.
9) Care of intravenous line (canula), intercostal tube and
Foley catheter if present.
10) Monitoring
a) Pulse rate, blood pressure, respiratory rate and
temperature
b) Oxygen saturation monitoring
c) Hourly urine output measurement. The best measures
of organ perfusion & the best monitor of the adequacy
of shock therapy remain the urine output.
d) CVP monitoring
e) Electrocardiogram
f) Cardiac output monitoring
g) Level of consciousness (is an important marker of
cerebral perfusion although it is a poor marker of
adequacy of resuscitation).
h) Measures of S. electrolytes and acid base balance.
Lecture 7 - Blood transfusion & blood products
24
Blood transfusion
is the process of transferring blood or
blood-based products from one person (donor) into the
circulatory system of another (recepient). Blood
transfusions can be life-saving in some situations, such as
massive blood loss due to trauma
Blood is made up of various parts, including red blood
cells, white blood cells, platelets, and plasma.
Every person has one of the following blood types: A, B,
AB, or O. Also, every person's blood is either Rh-
positive or Rh-negative. So, if you have type A blood,
it's either A positive or A negative.
The blood used in a transfusion must work with your
blood type. If it doesn't, antibodies (proteins) in your
blood attack the new blood and cause a reaction.
Type O blood is safe for almost everyone. People who
have this blood type are called universal donors. Type O
blood is used for emergencies when there's no time to test
a person's blood type.
People who have type AB blood are called universal
recipients. This means they can get any type of blood.
If you have Rh-positive blood, you can get Rh-positive or
Rh-negative blood. But if you have Rh-negative blood,
you should only get Rh-negative blood.
The indication for B.T. in surgical practice are;
1) 1-Trauma in which there have been severs blood loss.
2) 2-Haemorrhage from pathological lesions, ex.from GIT.
3) 3-Following severe burns, there may be associated
hemolysis
4) 4-Pre-operatively in cases of chronic anaemia in which
surgery is indicated urgently.
5) 5-During major operative procedures in which a certain
amount of blood loss is inevitable, ex.
abdominal operations & cardiovascular operations.
6) 6-Post-operatively in a patient who has become severly
anaemic.
7) 7-To arrest hemorrhage or as a prophylactic measure prior
to surgery in patient with a haemorrhigic state
ex.thrombocytopenia, haemophilia or liver disease.
Preparation of blood products for transfusion
Its important that blood donor should be fit, No evidence
of infection especially hepatitis & HIV infection.
Donated Blood is collected in a sterile bag, with a needle
& plastic tube attached in a complete, closed sterile unit.
15 G needle is introduced into the median cubital vein &
410 ml of blood is aspirated into the bag containing 75 ml
of anticoagulant (citrate,phosphate,dextrose;CPD).blood
can be stored for up to 42 days
During collection, the blood is constantly mixed with the
anticoagulant to prevent clotting.
All blood should be stored in special blood bank
refrigerator at 4C +/-2C.
Prolong storage may cause the following changes;
Leakage of intracellular K
Reduced level 2,3-DPG
Degeneration of functional granulocytes and platelets
Deterioration of clotting V and VIII
Ammonia concentration rises
Decrease in PH
Decrease in RBC deformability and viability
Component separation:
Red cells, plasma and platelets are separated into different
containers and stored in appropriate conditions so that
their use can be adapted to the patient's specific needs.
Red cells work as oxygen transporters, plasma is used as a
supplement of coagulation factors, and platelets are
transfused when their number is very scarce or their
function severely impaired. Blood components are usually
prepared by centrifugation.
Leukoreduction, also known as Leukodepletion is the
removal of white blood cells from the blood product by
filtration. Leukoreduced blood is less likely to cause
alloimmunization (development of antibodies against
specific blood types), and less likely to cause febrile
transfusion reactions.
Blood fractions
Some fractions are more appropriate than whole blood for
some clinical conditions.
1) packed red cells
Advisable in patients with chronic anaemia, elderly, small
children & patients in whom large volume of fluid may
cause cardiac failure. Packed RC is obtained by letting the
blood sediment & removing the plasma or by
centrifugation of whole blood for 15-30minutes.
2) platelet-rich plasma
Suitable for patient with thrombocytopenia.Prepared by
centrifugation of freshly donated blood for 15-30min.
3) platelet-concentrate
For patients with thrombocytopenia.Prepared by
centrifugation of platelet-rich plasma for 15-20 min.
4) plasma
By centrifugation of whole blood
Lecture 7 - Blood transfusion & blood products
25
5) human albumin 4.5%
Repeated fractionation of blood by organic fluids
followed by heat treatment result in this plasma fraction
which is rich in protein.Albumin may be stored for
several months at 4C & are suitable for protein
replacement ex. In severe burns
6) Fresh-frozen plasma (FFP).
Plasma removed from fresh blood within 4 hrs , rapidly
frozen by immersing in a solid Co2 & ethyl alcohol
mixture.This stored at -40 to -50C.Its good source for all
the coagulation factors, albumin & Ig.
Its indicated for surgical patient with abnormal
coagulation due to severe liver failure.Intial dose 12-15
ml/kg (one unit contain200-250ml).It should not be used
as a plasma expander in hypovolemia.
7) Cryoprecipitate.
By thawing FFP at 4C, removing supernatant plasma.The
cryoprecipitate is a very rich source of factorVIII. Its
stored at -40C,its good for haemophilic patients, also
good source of fibrinogen in patient with
hypofibrinogenemia
8) factorVIII&IX concentrate.
These are available in freeze dried form
9) Fibrinogen.
By liquid fractionation of plasma & stored in a dried form
. Used for patients with DIC or congenital
afibrinogenemia, however it carries a high risk of
hepatitis.
10) SAG-Mannitol blood.
All plasma is removed & is replaced with 100 ml of
crystalloid solution containing; Nacl, Adenine, Glucose &
Mannitol. This maintains good cell viability, but contain
no protein (albumin).
Blood grouping & cross-match.
RBCs have many different Ag on their surface.2 main
groups of major importance;
A. Ag of the ABO blood groups;
These are strongly antigenic & are associated with
naturally occurring Abs in the serum.4 different ABO cell
groups;
Red cell group serum contains;
A Anti-B Antibody
B Anti-A Antibody
AB No ABO Antibody
O Anti-A&Anti-B Antibody
B. Ags of the rhesus blood groups
The important Ag in this group is Rh (D) which is
strongly Antigenic & is present in 85% of the population
& Abs to the D Ag are not naturally present in the
remaining 15% but their formation may be stimulated by
the transfusion of Rh +ve.
Such acquired Abs are capable during pregnancy of
crossing the placenta& may cause severe hemolytic
anaemia & even death (hydropes fetalis) in a Rh +ve fetus
in utero.
Incompatibility
If Abs present in the recipients serum are incompatible
with the donors cells ,a transfusion reaction will result
because of agglutination & hemolysis of the donated
cells,leading in sever cases to acute tubular necrosis &
renal failure.So for this reason all transfusion should be
preceeded by;
1-ABO & Rh grouping of the recipient & donor cells , so
that only ABO&Rh(D) compatible blood is given
2-Direct matching of the recipients serum with the donor
cells to confirm compatibility
Blood grouping & cross-matching take 1 hr. If emergency
, blood volume may be restored by
saline,gelatin(ex,haemaccel),dextran or human albumin
4.5%.Alternatively O-ve should be given.
Giving blood.
1) Selection & preparation of the site
2) Checking of the donor blood; compatibility label ,
patients name, hospital reference , ward & blood group
3) Insertion of needle or cannula
4) Giving written instruction, ex, rate of flow. In emergency
it may be necessary to increase rate of flow,its preferable
to give one or two unit in 30 min using a pressure cuff
around a plastic bag of blood
Warming blood.
During rapid major blood transfusion,the blood must be
warmed before reaching the patient by blood warming
unit to reduce the risk of cardiac arrest.
Autotransfusion
Transfusion of patients own blood,ex. In ruptured ectopic
pregnancy when blood is collected from peritoneal cavity
& put in sterile container to give to the patient after
filtering it.
Lecture 7 - Blood transfusion & blood products
26
Complications of BT
A. Immune complications
1) Hemolytic
i. acute
ii. delayed
2) non-hemolytic
i. febrile
ii. urticarial
iii. anaphylactic
iv. pulmonary oedema (non-cardiogenic)
v. graft vs. host
vi. purpura
vii. immune suppression
B. non-immune complications
1) complications associated with massive B.T
i. coagulopathy
ii. citrate toxicity
iii. hypothermia
iv. acid-base disturbance
v. change in serum K concentration
vi. iron accumilation
vii. volume overload
2) infectious complications
i. hepatitis
ii. AIDS
iii. Other viral agents(CMV,EBV,HTLV)
iv. Parasites&bacteria
3) Other complications
i. thrombophlebitis
ii. air embolism
A.
Immune Complication
These are primarily due to the sensitization of the
recipient to donor blood cells (either red or white),
platelets or plasma proteins. Less commonly, the
transfused cells or serum may mount an immune response
against the recipient
1) Hemolytic reactions
Usually involve the destruction of transfused blood cells
by the recipient's antibodies. Less commonly, the
transfused antibodies can cause hemolysis of the
recipient's blood cells. There are acute (also known as
intravascular) hemolytic reactions and delayed (also
known as extravascular) hemolytic reactions.
i. acute hemolytic reactions
The majority of hemolytic reaction are caused by
transfusion of ABO incompatible blood.,eg group A,B or
AB cells to agroup O patient. Most hemolytic reaction are
the result of human error such as error in labeling or
checking the specimen
This type of reaction has been reported to occur
approximately 1 in 25,000 transfusions but it is often very
severe and accounts for over 50% of reported deaths
related to transfusion. The severity of the reaction often
depends in the amount of blood given.
Non-immune hemolysis of RBCs in the blood container
or during administration can occur due to physical
disruption (temperature changes, mechanical
forces,non-isotonic fluid)
The pt. develops chills, fever, nausea chest pain and
flank pain,pain along iv line hypotension, dark urine,
uncontrolled bleeding due to DIC in awake pt.. In
anasthetized pt., you should look for rise in temperature,
unexplained tachycardia, hypotension, hemoglobin
urea, oozing in the surgical field,DIC, shock and renal
shutdown.
Management of acute hemolytic reaction
These patients usually require ICU support and therapy
includes vigorous treatment of hypotension and
maintenance of renal blood flow The unit should be re-
checked. Blood from the recipient patient should be
drawn to test for hemoglobin in plasma, repeat
compatibility testing and coagulation tests. A foley
catheter should be placed to check for hemoglobin in the
urine. Osmotic diuresis with mannitol(or frusemide) and
fluids should be utilized (low-dose dopamine may help
renal function and support blood pressure).dialysis may
be necessary. With rapid blood loss, platelets and fresh
frozen plasma may be indicated.
Prevention:
Proper identification of the pt. from sample collection
through the blood admimistration, proper labeling of
samples and products is essential. Prevention on non-
immune hemolysis requires adherence to proper handling,
storage and administration of blood products
ii. Delayed hemolytic reactions
Pts may develop Abs to red cells Ags (Ab. To non-D Ag
of the Rh system or to the kell,duffy or kidd Ags).
Antibodies can occur naturally, or may arise as a
consequence of previous transfusion or pregnancy. .
Following a normal, compatible transfusion there is a 1-
1.6% chance of developing antibodies to these foreign
antibodies (alloimmunisation). This takes weeks or
months to happen - and by that time, the original
Lecture 7 - Blood transfusion & blood products
27
transfused cells have already been cleared. Re-exposure to
the same foreign antigen can then cause an immune
response.
Most delayed haemolytic reactions produce few
symptoms and may go unrecognised, however, there may
be malaise, jaundice, fever, a fall in Hematocrit despite
transfusion, and an increase in unconjucated bilirubin.
Diagnosis may be facilitated by the direct coombs test
which can detect the presence of antibodies on the RBC
membrane
Alloimmunisation to the D andK (Kell) antigens is
prevented by the provision of Rh(D) negative and Kell
negative blood for Rh(D) negative, kell negative pts. This
is important for females with child-bearing potential as
these antibodies can cause sever hemolytic disease of the
newborn during pregnancy
2) Non-hemolytic reaction
Are Due to sensitization of the recipient to donor WBC,
platelets, or plasma proteins. These reactions include;
i. Febrile Reactions
Cause: Fever and chills during transfusion without
evidence of hemolysis are thought to be caused by
recipient antibodies reacting with white cell antigens or
white cell fragments in the blood product or due to
cytokines which accumulate in the blood product during
storage. Fever occurs more commonly with platelet
transfusion (10-30%) than red cell transfusion (1-2%).It is
important to distinguish from fever due to the patient's
underlying disease or infection (check pretransfusion
temperature). Fever may be the initial symptom in a more
serious reaction such as bacterial contamination or
haemolytic reaction.
Management: Symptomatic, paracetamol
If the fever is accompanied by significant changes in
blood pressure or other signs and symptoms, the
transfusion should be ceased and investigated.
Prevention: A proportion of patients who have febrile
reactions will have similar reactions to subsequent
transfusions. Many are prevented by leucocyte filtration
(either bedside or pre-storage).
ii. Urticarial (allergic)reactions
Are characterized by erythema, hives and itching
without fever. on rare occasions it may be associated with
laryngeal oedema and bronchospasm. Again, this is a
relatively common reaction and occurs in about 1% of all
transfusions. It is thought to be due to sensitization
against plasma proteins. The use of packed red blood cells
rather than whole blood has decreased the likelihood of
this problem.
Management; If urticaria occurs in isolation (without
fever and other signs), slow the rate or temporarily stop
transfusion. If symptoms are bothersome, consider
administering an antihistamine before restarting the
transfusion. If associated with other symptoms, cease the
transfusion and proceed with investigation.
iii. Anaphylactic reactions
Are rare and occur in about 1 of 150,000 transfusions.
These are severe reactions that can occur with very small
amounts of blood (a few milliliters). Typically, these
reactions occur in pts with IgA deficiency who have anti-
IgA antibodies. These antibodies react to transfusions
containing IgA.
Anaphylactic and anaphylactoid reactions have signs of
cardiovascular instability including hypotension,
tachycardia, loss of consciousness, cardiac arrhythmia,
shock and cardiac arrest. Sometime respiratory
involvement with dyspnea and stridor are prominent.
IgA deficiency occurs in 1 of 600-800 patients in the
general population. Patients with known IgA deficiency
should receive washed packed red blood cells, or IgA free
blood units
Management by immediately stop transfusion,
supportive care including airway management may be
required. Adrenaline may be indicated. Usually given as
1;1000 solution s.c,i.m or slow i.v.,fluids and
corticosteroids
iv. Transfusion-related acute lung injury
Some pts can develop acute hypoxemia and non-
cardiogenic pulmonary oedema and present with a
picture that looks like adult respiratory distress syndrome
(ARDS) developing within 2-8 hrs hours after a
transfusion. This is a rare (1 in 5000) but serious
complication that is thought to be secondary to cytokines
in the transfused product or from interaction between
donar antileucocyte antibodies with the patient white cells
antigens (or vice versa) causing them to aggregate in the
pulmonary circulation. Subsequent damage to the
alveolocapillary membrane triggers the syndrome.
Treatment involves symptomatic support for respiratory
distress includes oxygen administration and may require
Lecture 7 - Blood transfusion & blood products
28
intubation and mechanical ventilation . symptoms
generally resolves over 24-48 hours.
v. Graft versus Host disease
This seen exclusively in immunocompromised patients
when donor lymphocytes proliferate and damage target
organs especially bone marrow, skin, liver and
gastrointestinal tract. The clinical syndrome comprises
fever, skin rash, pancytopenia, abnormal liver function
and diarrhoea and is fatal in over 80% of cases. The usual
onset is 8-10 days post transfusion, with a longer interval
between transfusion and onset of symptoms in infants.
Prevention: Gamma irradiation of cellular blood products
(whole blood, red blood cells, platelets, granulocytes) for
at risk patients.(pts with hodgkins disease, aplastic
anaemia, AIDS, cytotoxic drugs)
vi. Post-transfusion purpura
is common with the development of platelet antibodies.
The external purpura signal a reaction that may lead to
profound thrombocytopenia which usually occurs about
one week post transfusion. Plasmapheresis is the
recommended treatment.
vii. Immune suppression
is a debatable complication. The transfusion of leukocyte-
containing blood products appears to be
immunosuppressive causing a decrease in Natural Killer
cell function, decreased phagocytosis and decreased
helper to suppressor cell ratios.
The effect was first seen in renal transplant patients in
whom preoperative blood transfusions appeared to
improve graft survival.
B.
Non-Immune Complications
1) complications associated with massive B.T
Massive Transfusion is usually defined as the need to
transfuse a volume of blood equivalent or exceeding the
patients own volume in a less than a 24-hours period or
replacement of more than one blood volume in 24 hours
or more than 50% of blood volume in 4 hours.(adult
blood volume is approximately 70 ml/kg, in children over
1 months old is approximately 80 ml/kg.
Massive transfusion occurs in settings such as severe
trauma, ruptured aortic aneurysm, surgery and obstetrics
complications.
i. Coagulopathy
Is common with massive transfusion. The most common
cause of bleeding following a large volume transfusion is
dilutional thrombocytopenia(each 10-12 units can
produce a 50% fall in the platelet count, thus, significant
thrombocytopenia can be seen).
Alteration in clotting system may occur, it can be
preexisting or induced coagulopathy. Its usually related to
the effects of acidosis and hypothermia. Acidosis
interfere with the assembly of coagulation factor
complexes involving calcium. Hypothermia reduces the
enzymatic activity of plasma coagulation proteins and
prevent platelets activation
ii. Citrate toxicity
Citrate is the anticoagulant used in blood products. It is
usually rapidly metabolised by the liver. Rapid
administration of large quantities of stored blood(one unit
over five minutes or so ) may cause hypocalcaemia and
hypomagnesaemia when citrate binds calcium and
magnesium. This can result in myocardial depression or
coagulopathy.
Patients most at risk are those with liver disease or
dysfunction or neonates with immature liver function
having rapid large volume transfusion.
Management: Slowing or temporarily stopping the
transfusion allows citrate to be metabolised. Replacement
therapy with intravenous calcium administration may be
required if there is clinical(transient tetany, hypotensiov)
or ECG or lab evidence of hypocalcemia or
hypomagnesaemia
iii. Hypothermia
Rapid infusion of large volumes of stored blood
contributes to hypothermia. Infants are particularly at risk
during exchange or massive transfusion.
Prevention and Management: Appropriately maintained
blood warmers should be used during massive or
exchange transfusion
iv.
v. Acid-Base imbalance
can be seen after massive transfusion. The most common
abnormality is a metabolic alkalosis. Patients may
initially be acidotic because the blood load itself is acidic
and there may be a prevailing lactic acidosis from
hypoperfusion. However, once normal perfusion is
restored, any metabolic acidosis resolves and the citrate
and lactate are then converted to bicarbonate in the liver.
Lecture 7 - Blood transfusion & blood products
29
vi. Potassium Effects
Serum potassium can rise as blood is given. The
potassium concentration in stored blood increases steadily
with time (stored red cells leak potassium proportionally
throughout their storage)..
hyperkalaemia can occur during rapid, large volume
transfusion of older red cell units in small infants and
children.
Prevention: Blood less than 7 days old is generally used
for rapid large volume transfusion in small infants (eg
cardiac surgery,exchange transfusion)
vii. Iron accumulation
Iron accumulation is a predictable consequence of chronic
RBC transfusion. Organ toxicity begins when
reticuloendothelial sites of iron storage become saturated.
Liver and endocrine dysfunction creates significant
morbidity and the most serious complication is
cardiotoxicity which causes arrhythmias, and congestive
heart failure. Patients receiving chronic transfusion
usually have their iron status monitored and managed by
their physician.
Management and Prevention: Iron chelation therapy is
usually commenced early in the course of chronic
transfusion therapy
viii. Volume overload
Pts with cardiopulmonary disease and infants are at risk
of volume overload especially during rapid transfusion of
large volume of blood
Management; : Stop the transfusion, administer oxygen
and diuretics as required.its advisable in chronic anaemia
to give packed RC in addition to diuretic.The transfusion
should be given slowly(one unit over 4-6hrs).
2) Infectious complications
Hepatitis May be transmitted from donor & cause sever
hepatitis , usually 3 mths after transfusion. it should be
avoided by screening of the blood donor.
AIDS is a feared disease but the actual risk is quite low.
All blood is tested for the anti-HIV-1 antibody which is a
marker for infectivity. Unfortunately, there is a 6-8 week
period required for a person to develop the antibody after
they are infected with HIV and therefore infectious units
can go undetected
CMV and EBV are usually the cause of only
asymptomatic infection or mild systemic illness.
Unfortunately, some of these people become
asymptomatic carriers of the viruses and the white blood
cells in blood units are capable of transmitting either
virus.
Immunocompromised and immunosuppressed
patients are particularly susceptible to CMV and should
receive CMV negative units only.
Parasitic diseases
Reported to be transmitted via blood transfusion include
malaria, toxoplasmosis, and Chagas' disease.
Bacterial Contamination
Bacteria may be introduced into the pack at the time of
blood collection from sources such as donor skin, donor
bacteraemia or equipment used during blood collection or
processing.or it may results from faulty storage,especially
when donor blood being Left in a warm room for some
hrs before transfusion
Bacteria may multiply during storage. Gram positive and
Gram negative organisms have been implicated. Platelets
are more frequently implicated than red cells.
Symptoms: Very high fever, rigors, profound
hypotension, nausea and/or diarrhoea.
Management: Immediately stop the transfusion and
notify the hospital blood bank.
After initial supportive care, blood cultures should be
taken and broad-spectrum
antimicrobials commenced. Laboratory investigation will
include culture of the blood pack.
Prevention: Inspect blood products prior to transfusion.
Some but not all bacterially contaminated products can be
recognised (clots, clumps, or abnormal colour).
Maintaining appropriate cold storage of red cells in a
monitored blood bank refrigerator is important.
Transfusions should not proceed beyond the
recommended infusion time (4 hours).
Blood substitutes
1) Albumin
Human albumin can be used while cross-matching is
being performed.2-3 units are given IV over 30min.Its
valuable in burns & hypovolemia. Its prepared from
human plasma & heat treated so that neither hepatitis nor
Lecture 7 - Blood transfusion & blood products
30
HIV can be transmitted.Shelf life is one year at room
temp. but 5-yr at 2-8C
Human albumin(4.5%) is valuable in burn&hypovolemia.
Human albumin(20%) concentrated salt poor used in
sever hypoalbuminemia with salt&water overload ex.
Liver failure with ascitis.
2) 2-Dextrans
These are polysaccharide polymers of varying molecular
wt.ex.dextran70 & dextran40.
It produce an osmotic pressure similar to that of
plasma.They induce roulex of the red cells,thus interfere
with blood grouping&cross-matching,so the need of
blood sample before hand.It interfere with platelets
function & may cause an abnormal bleeding,so its
recommended that total volune of dextran should not
exceed 1000ml.It may also cause;
anaphylactic reaction.dextran may also cause;
- simple haemodilution of clotting factors
- Reduced factorVIII activity
- Increased fibrinogen activity
- Increased fibrinolysis
- Reduced clotting strength
- Impairment of platelets function
3) Gelatin(ex.Haemaccel,Gelofusin)
Used commonly as plasma expander.Up to 1000ml of 3.4-
4% solution givenIV.It has low rate of anaphylactic
reaction
4) Hydroxyethyl starches
Many types;Haptostarches,Pentastarches,Tetrastarches.It
has low incidence of anaphylactic reaction.It may cause
intractable itching,coagulopathy may occur due to
reduction in factor VIII& platelets
\
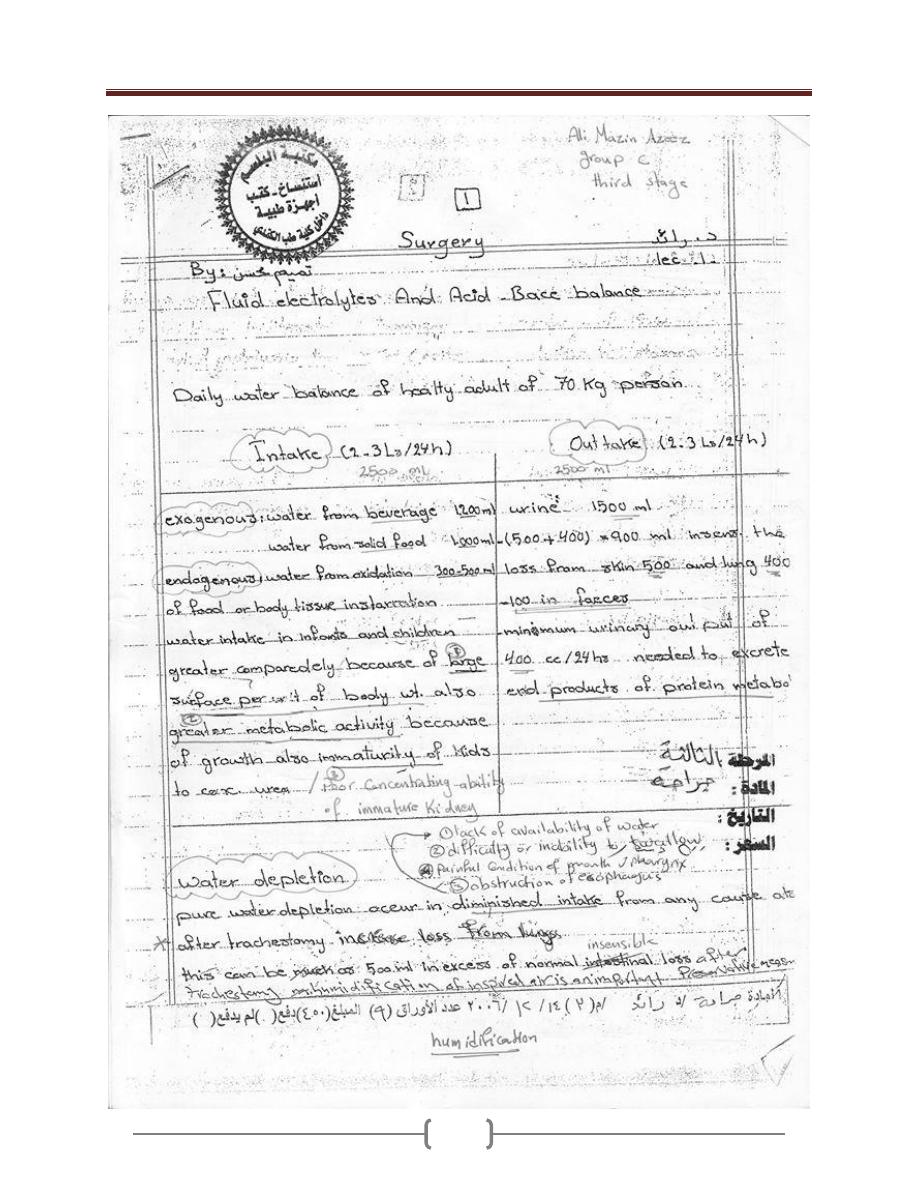
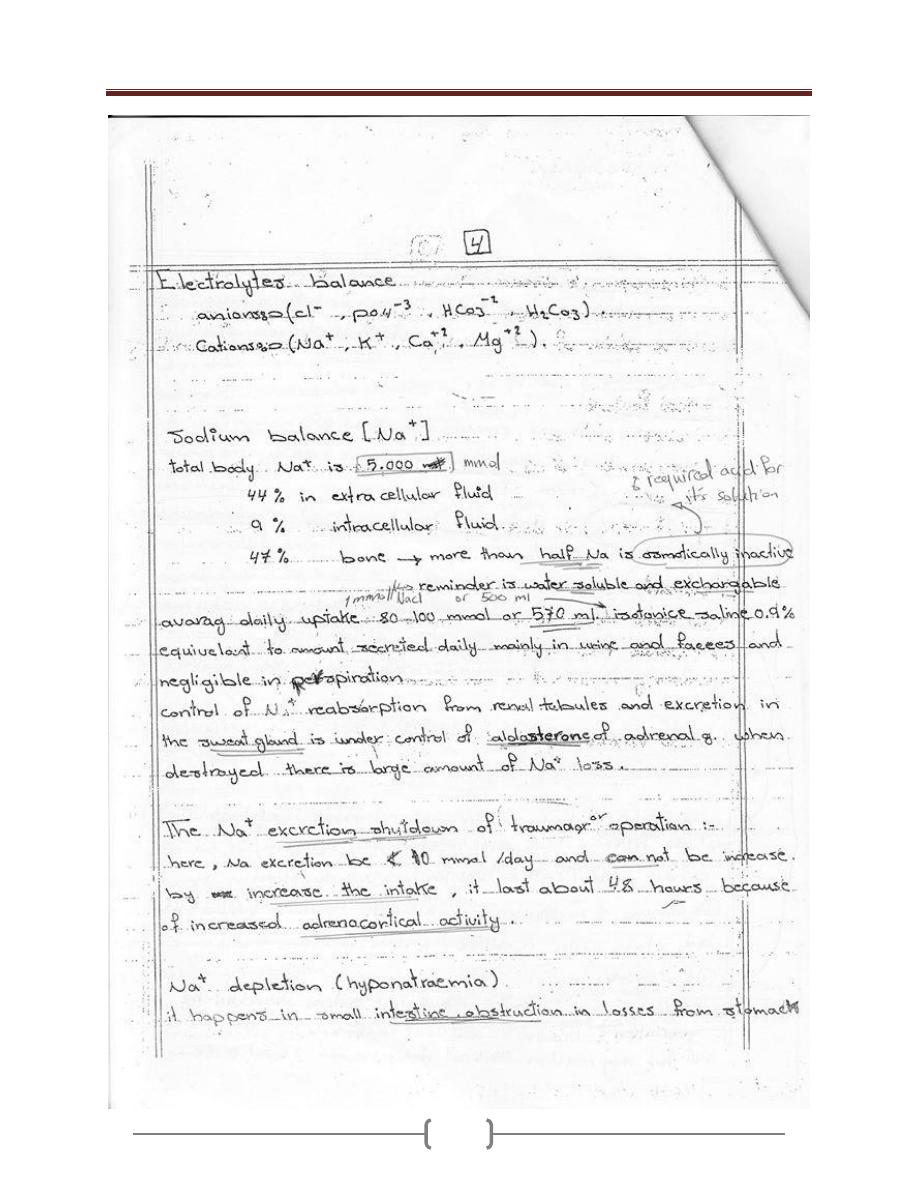
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
31
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
32
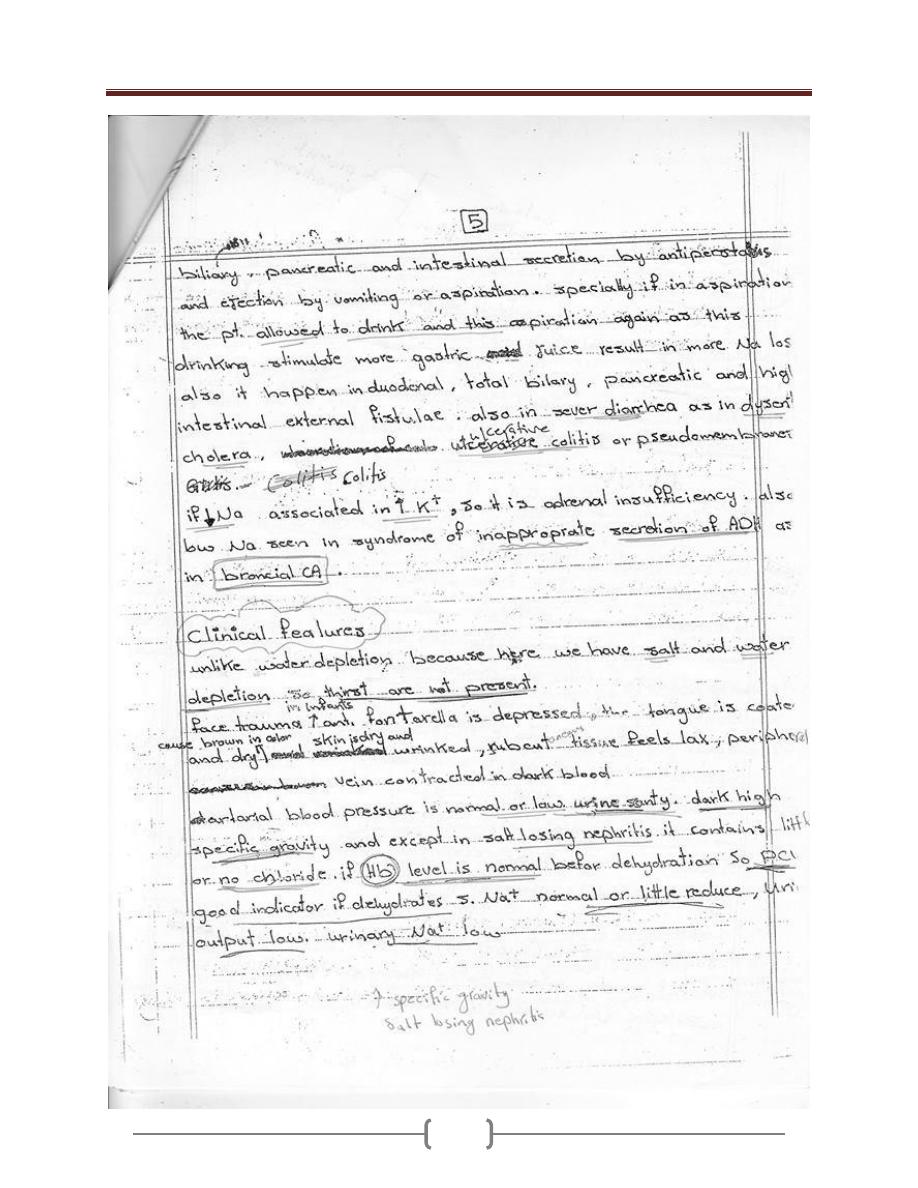
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
33
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
34
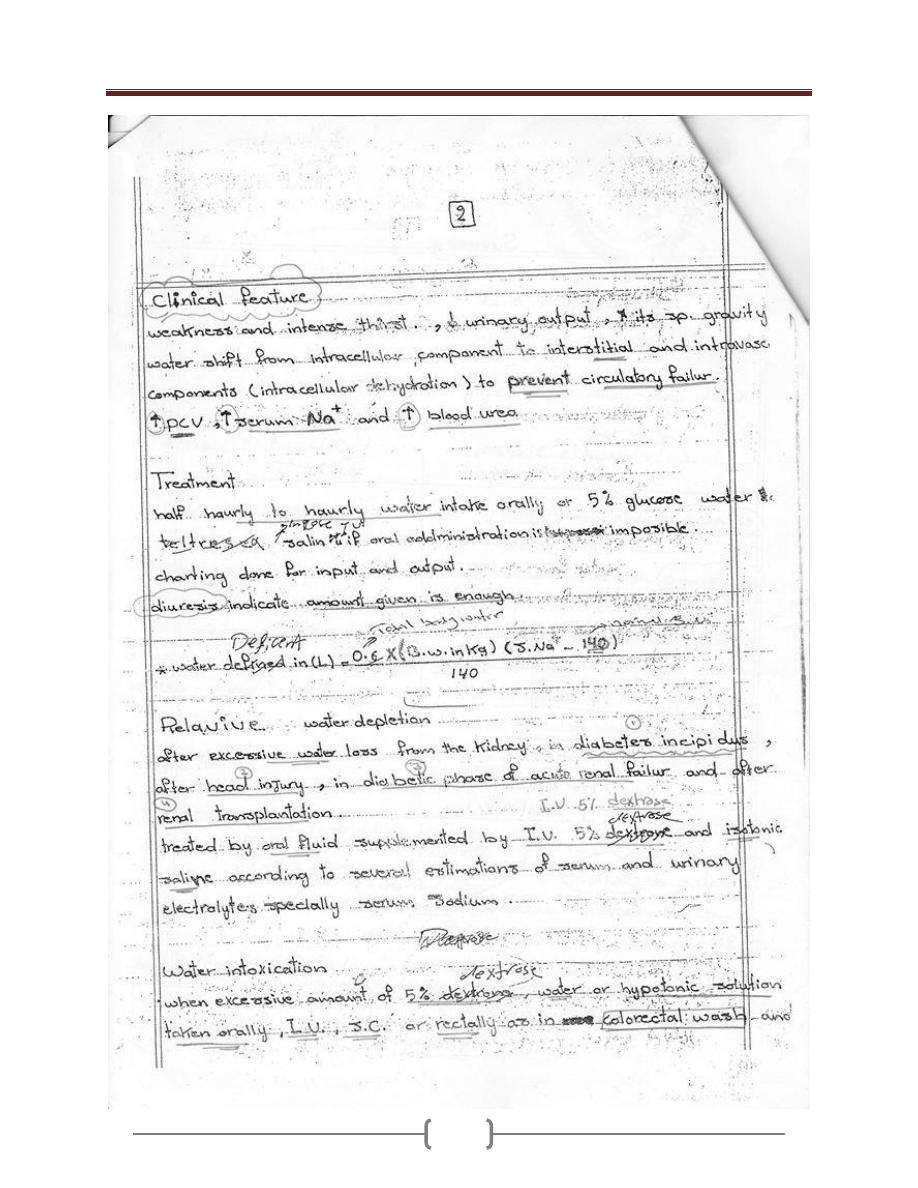
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
35
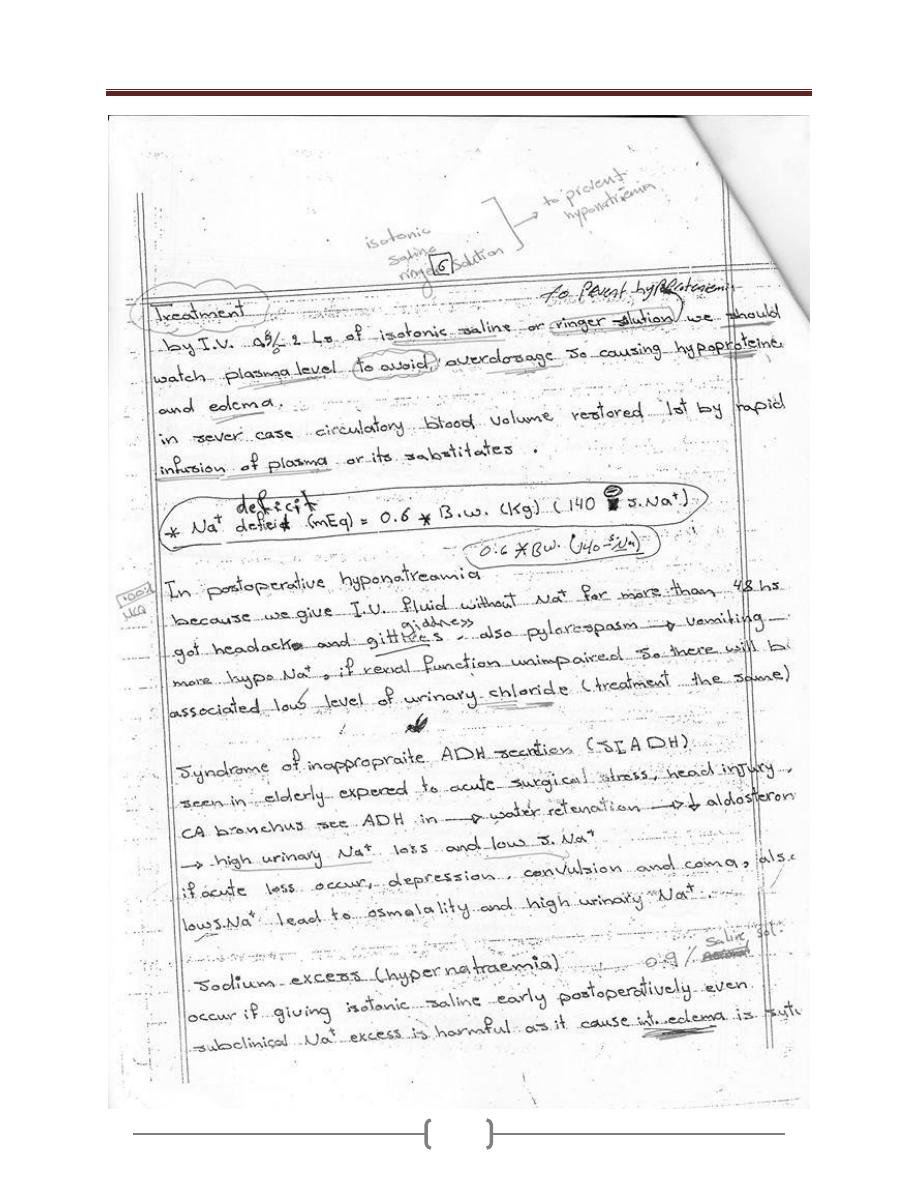
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
36
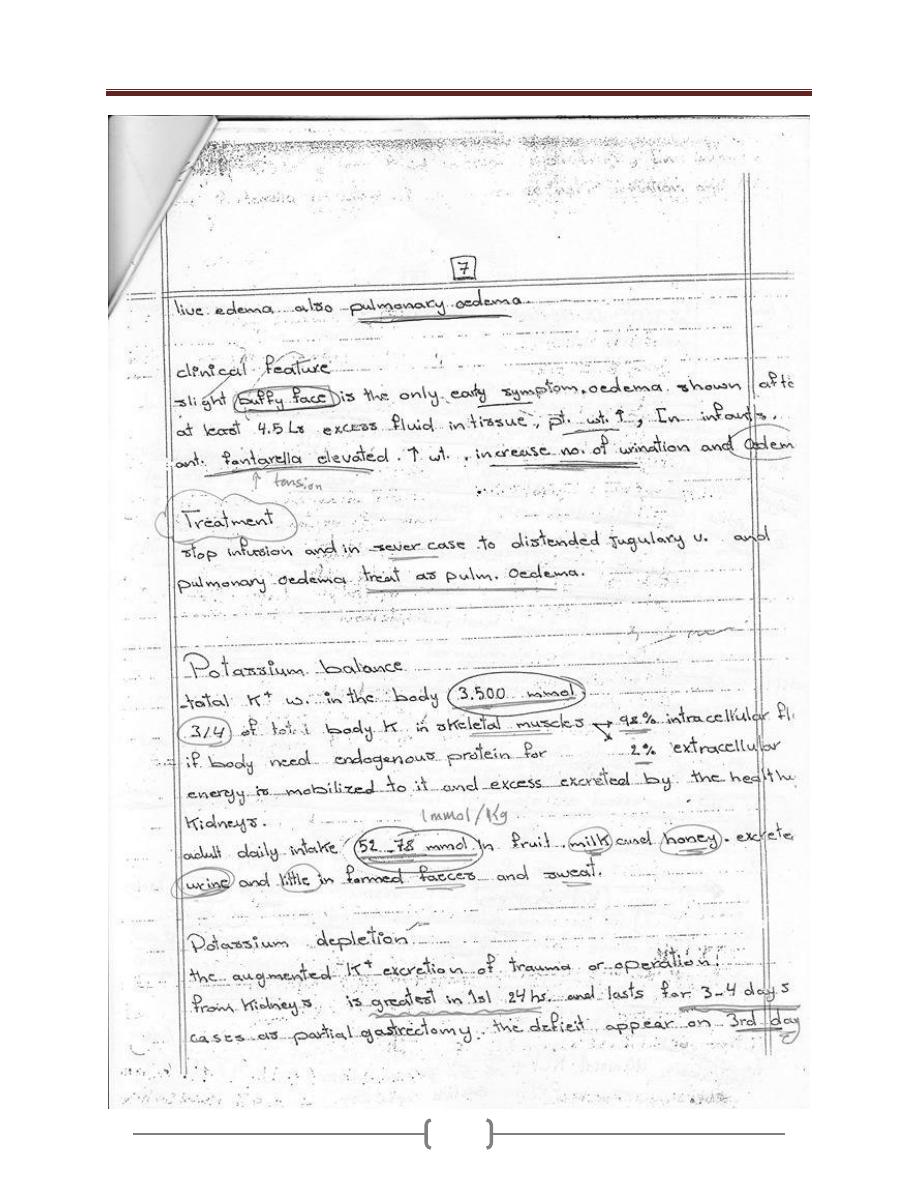
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
37
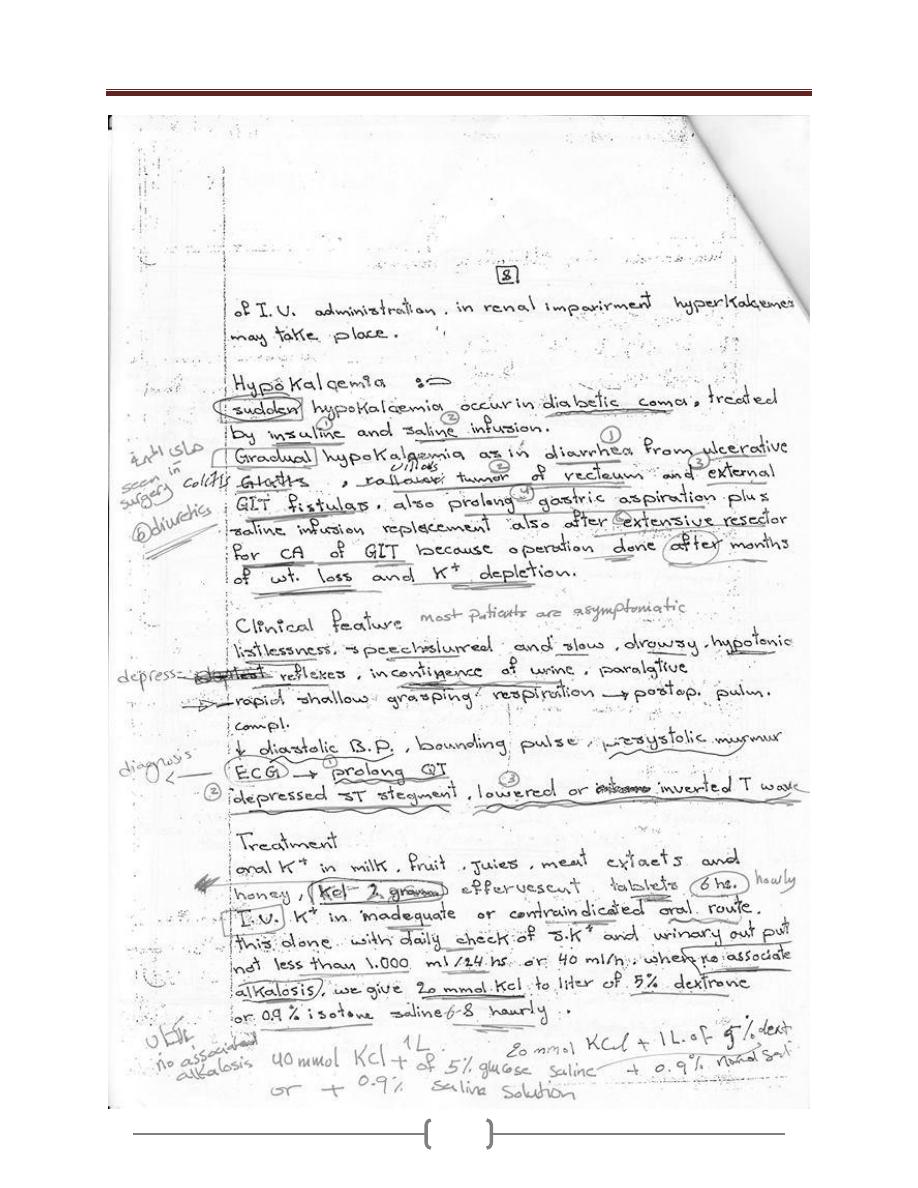
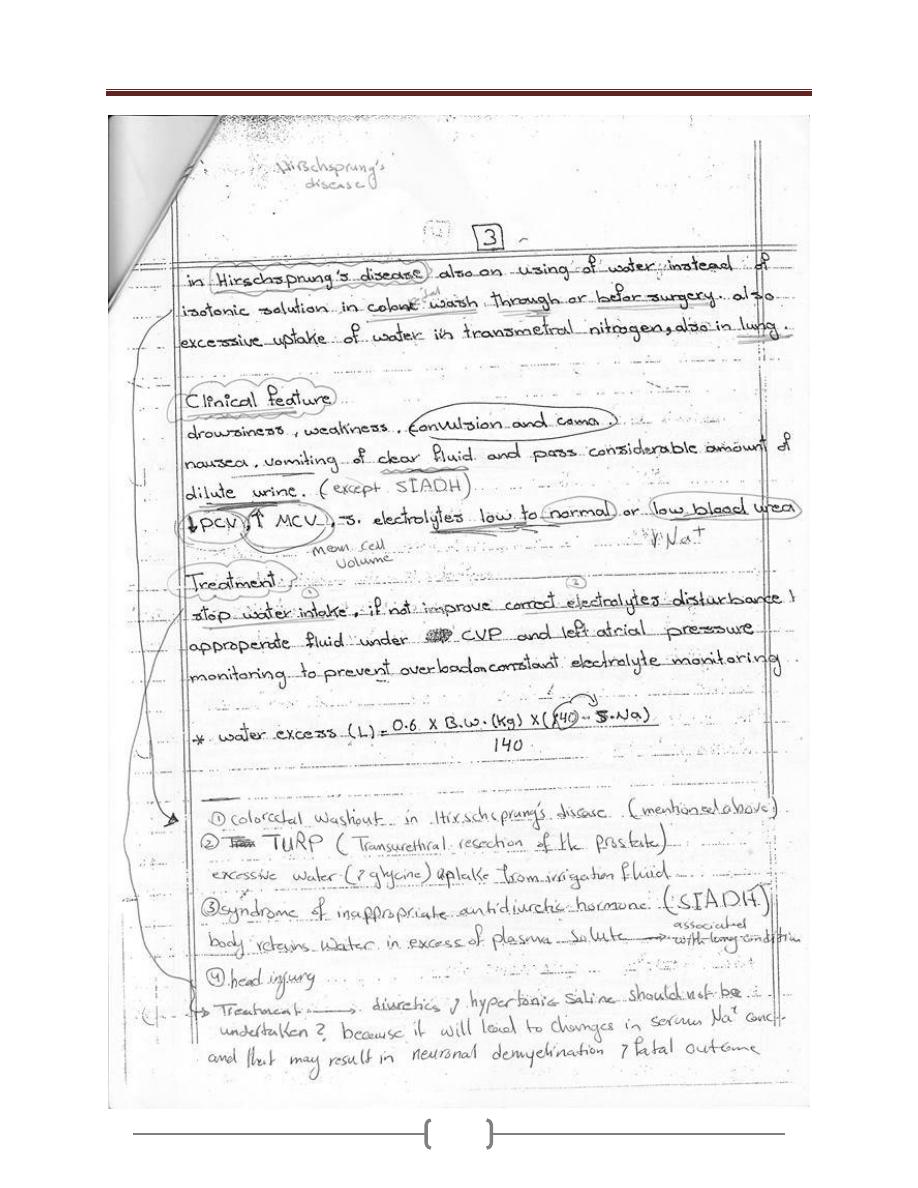
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
38
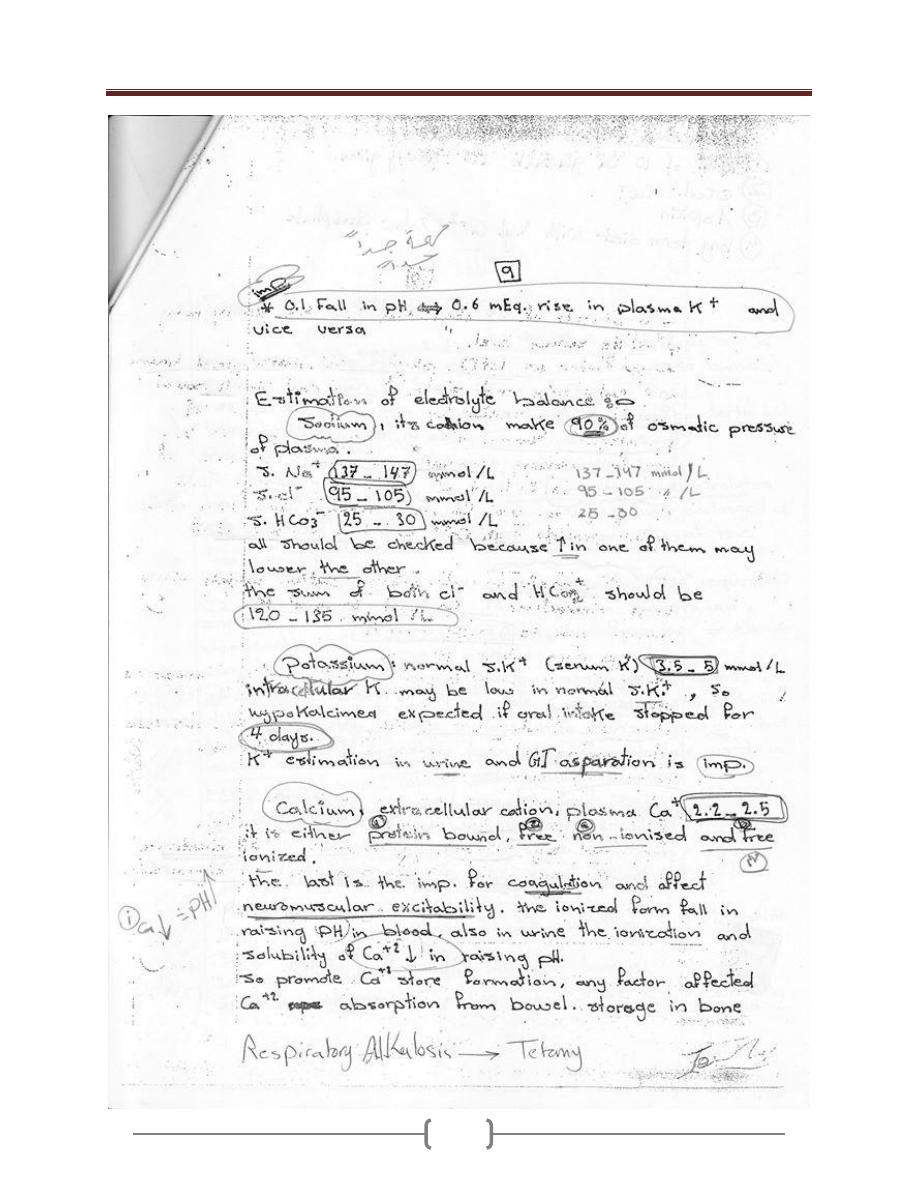
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
39
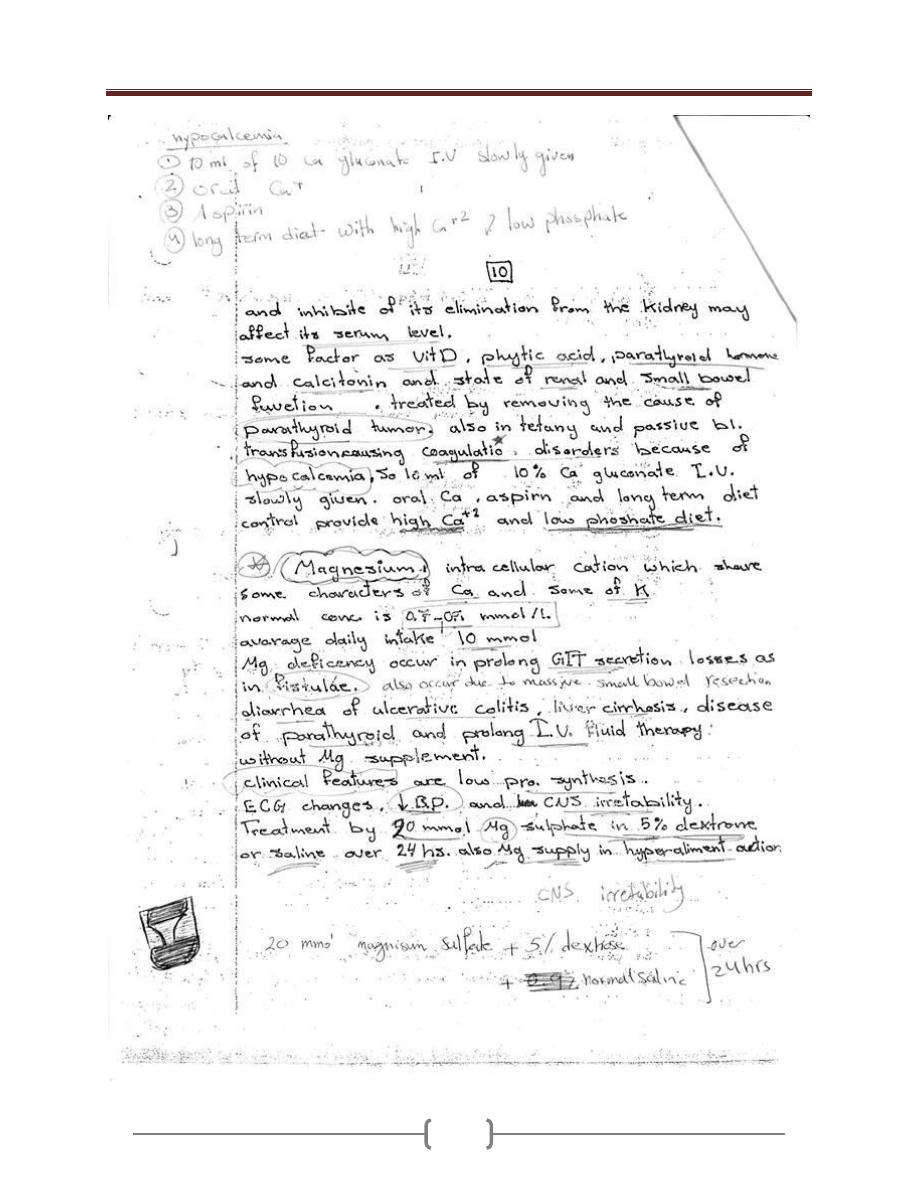
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
40
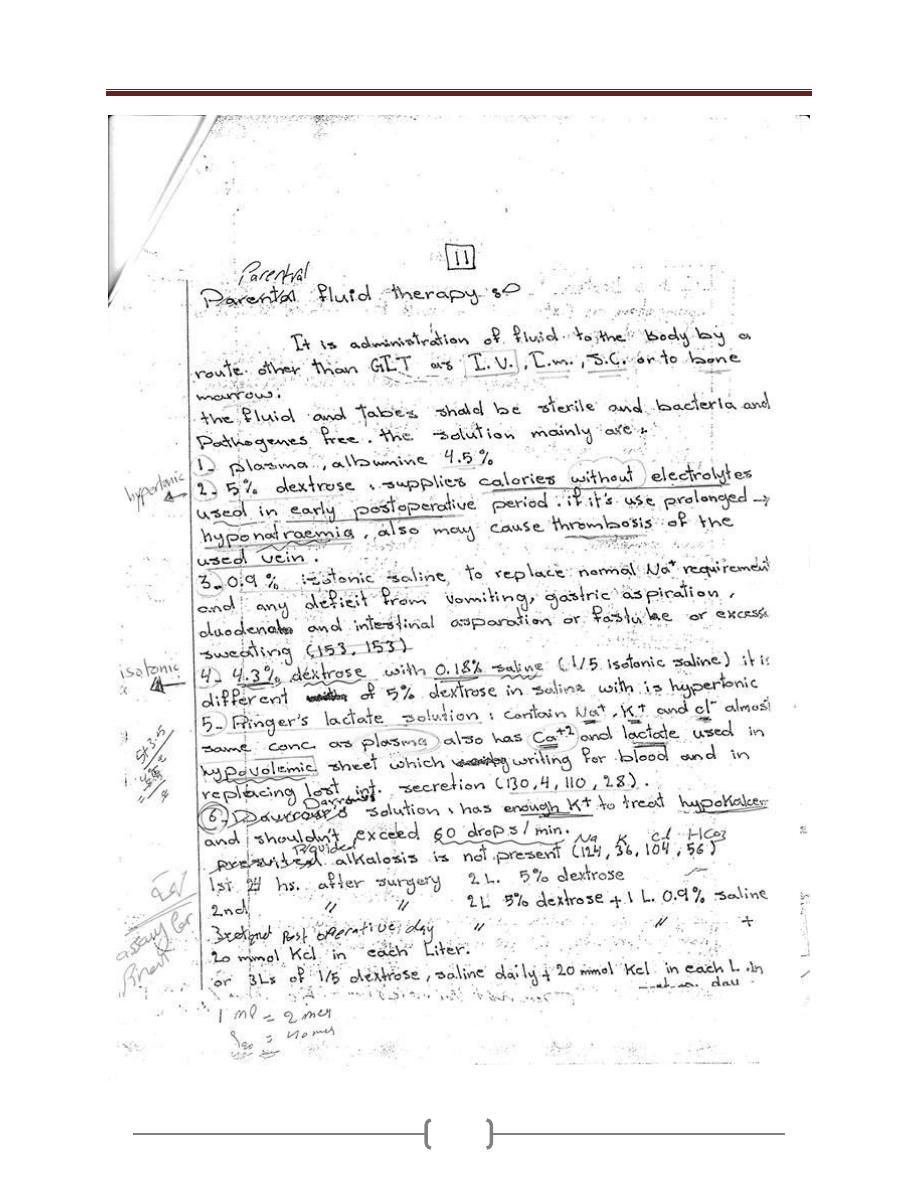
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
41
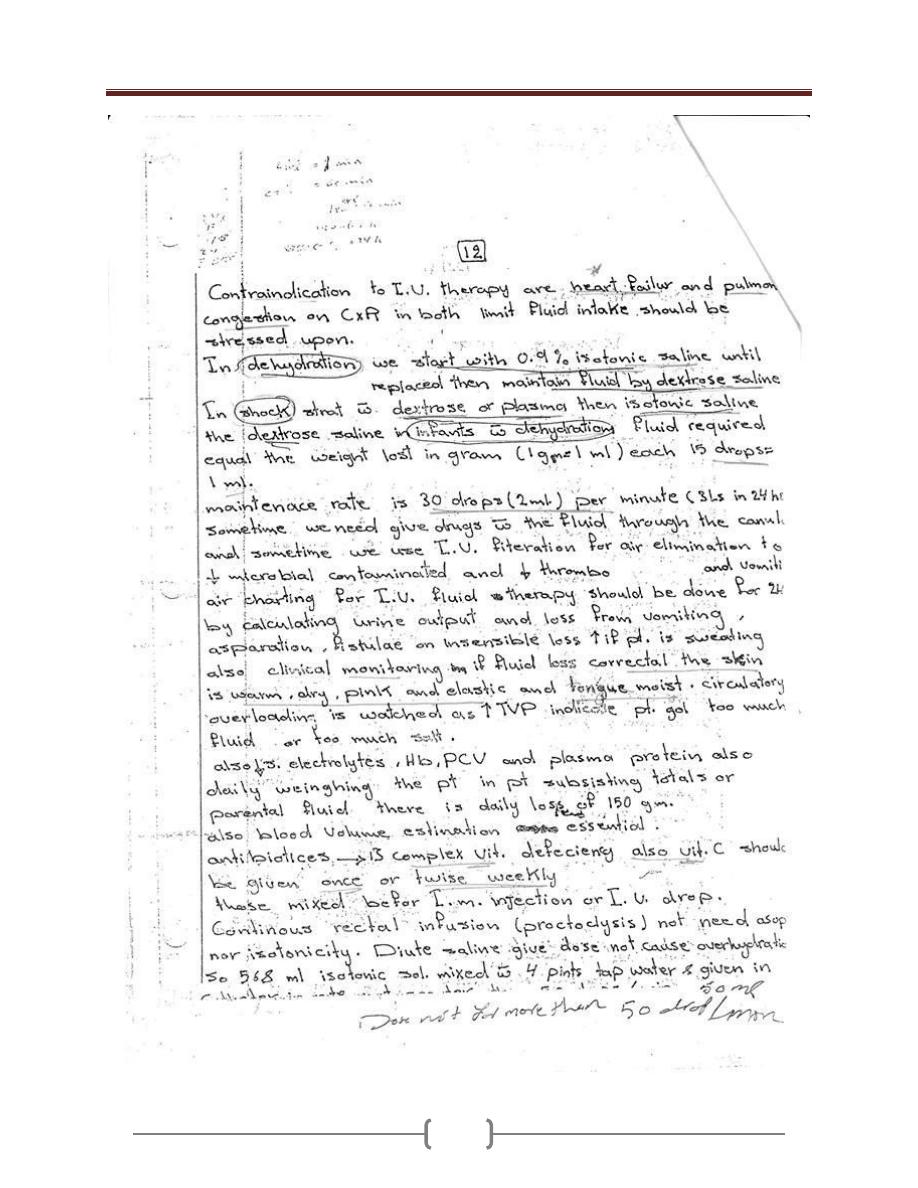
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
42
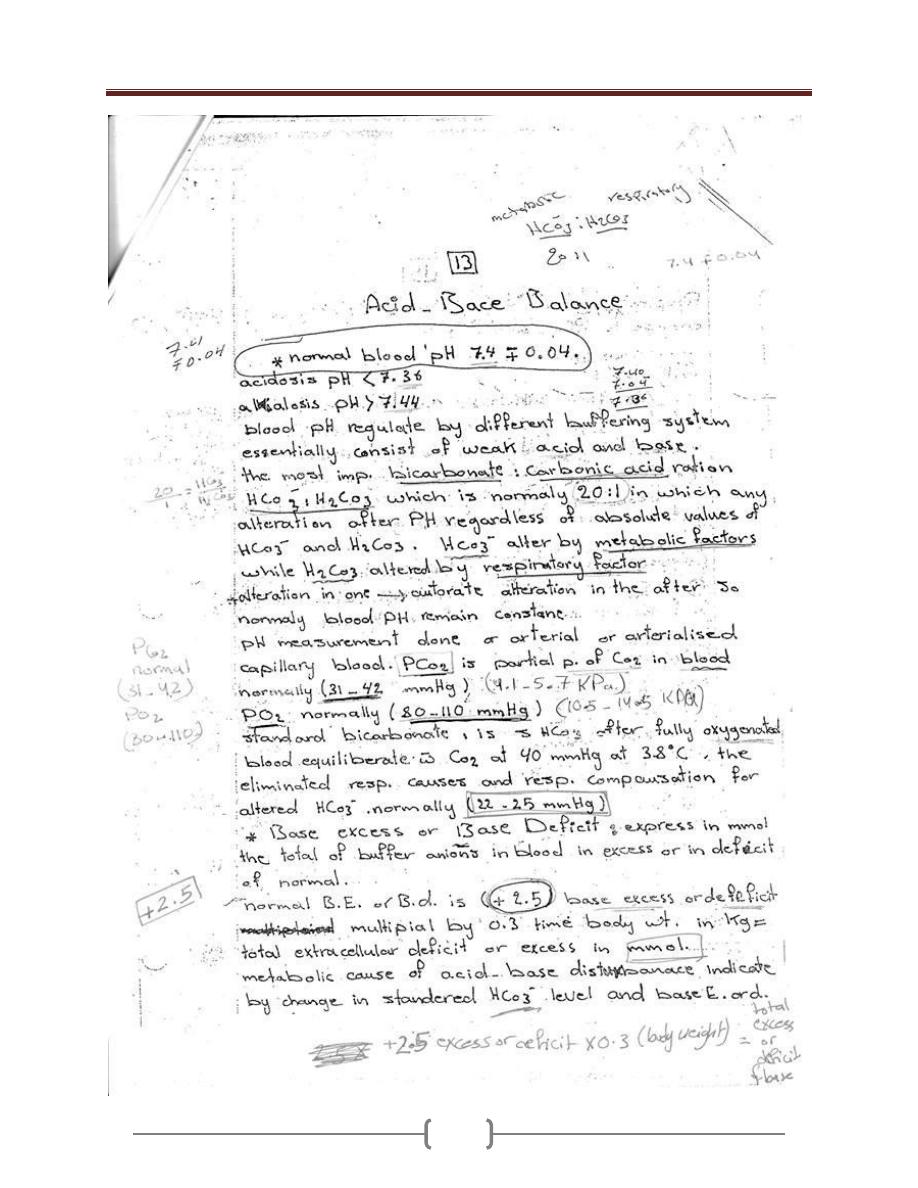
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
43
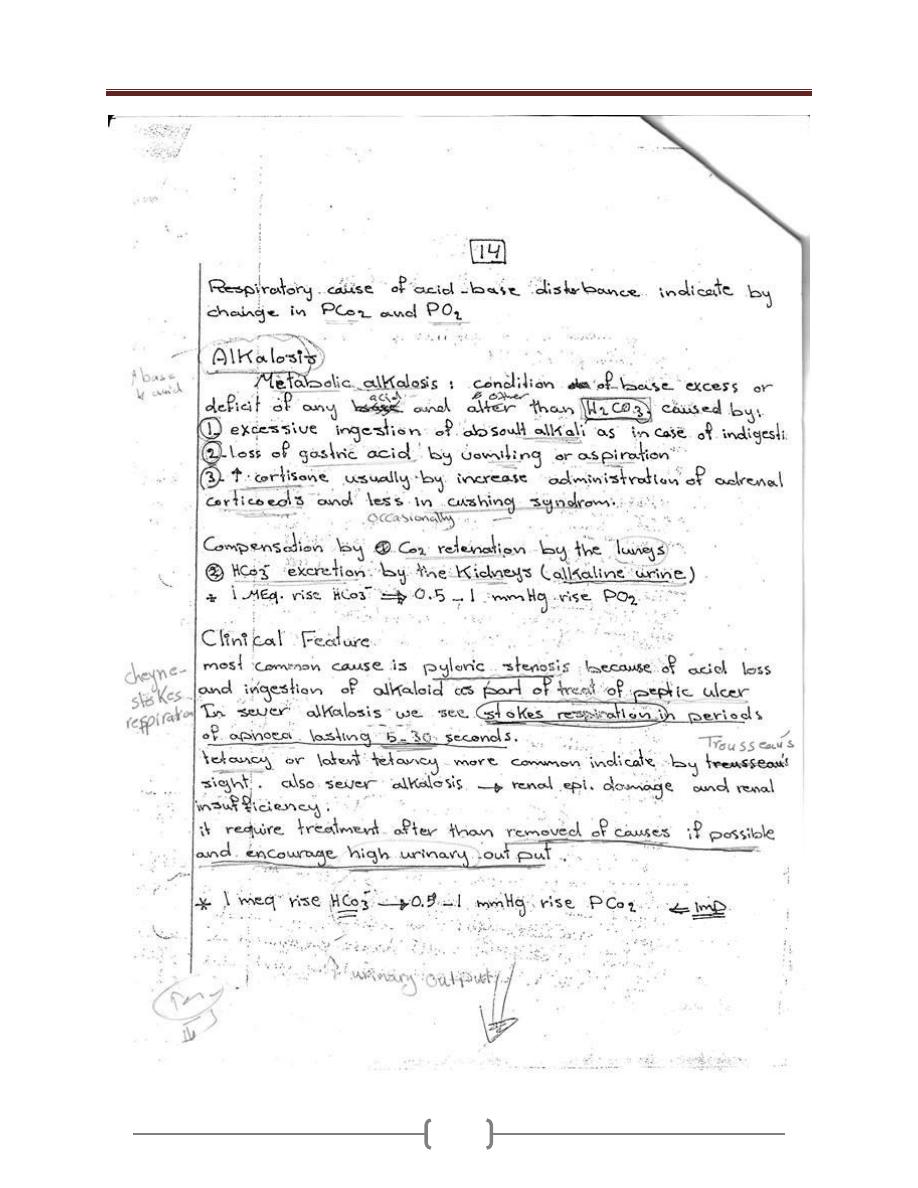
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
44
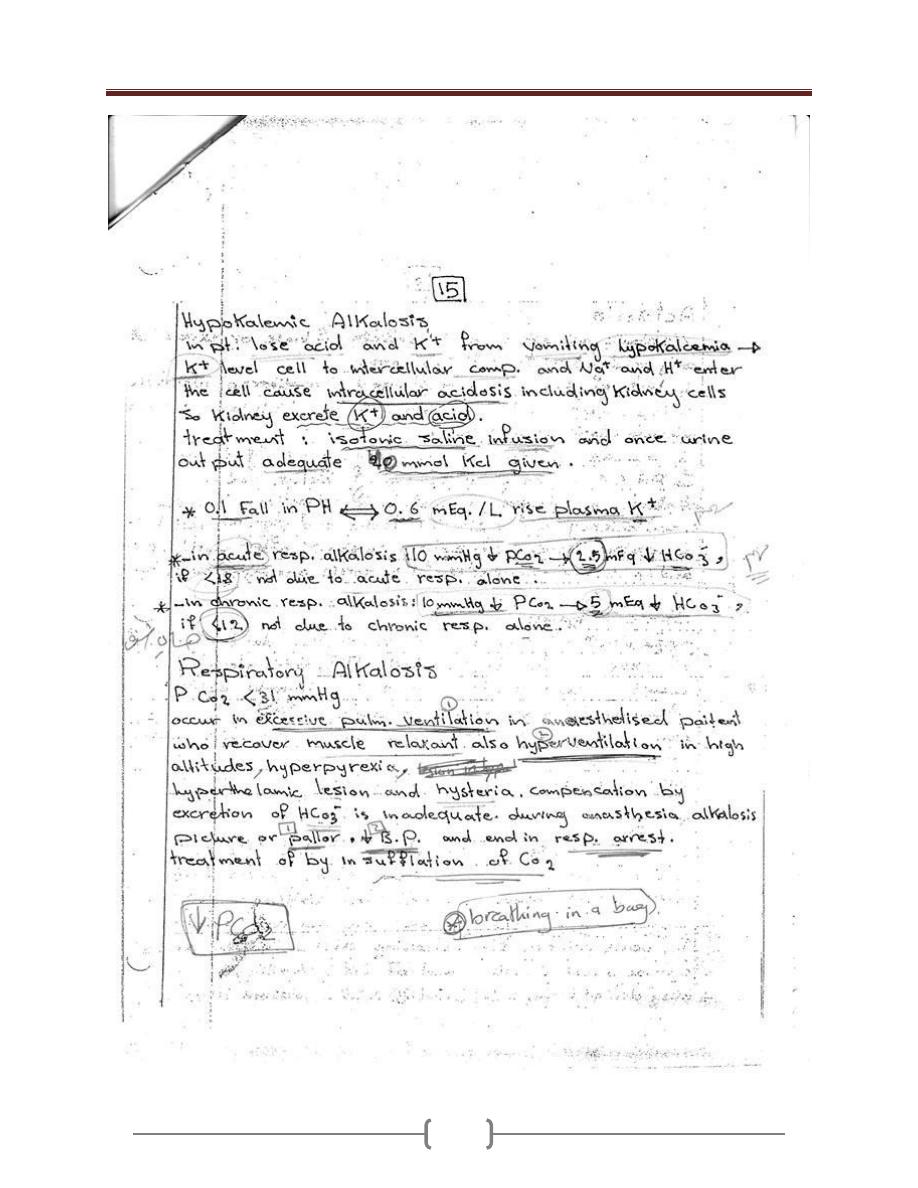
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
45
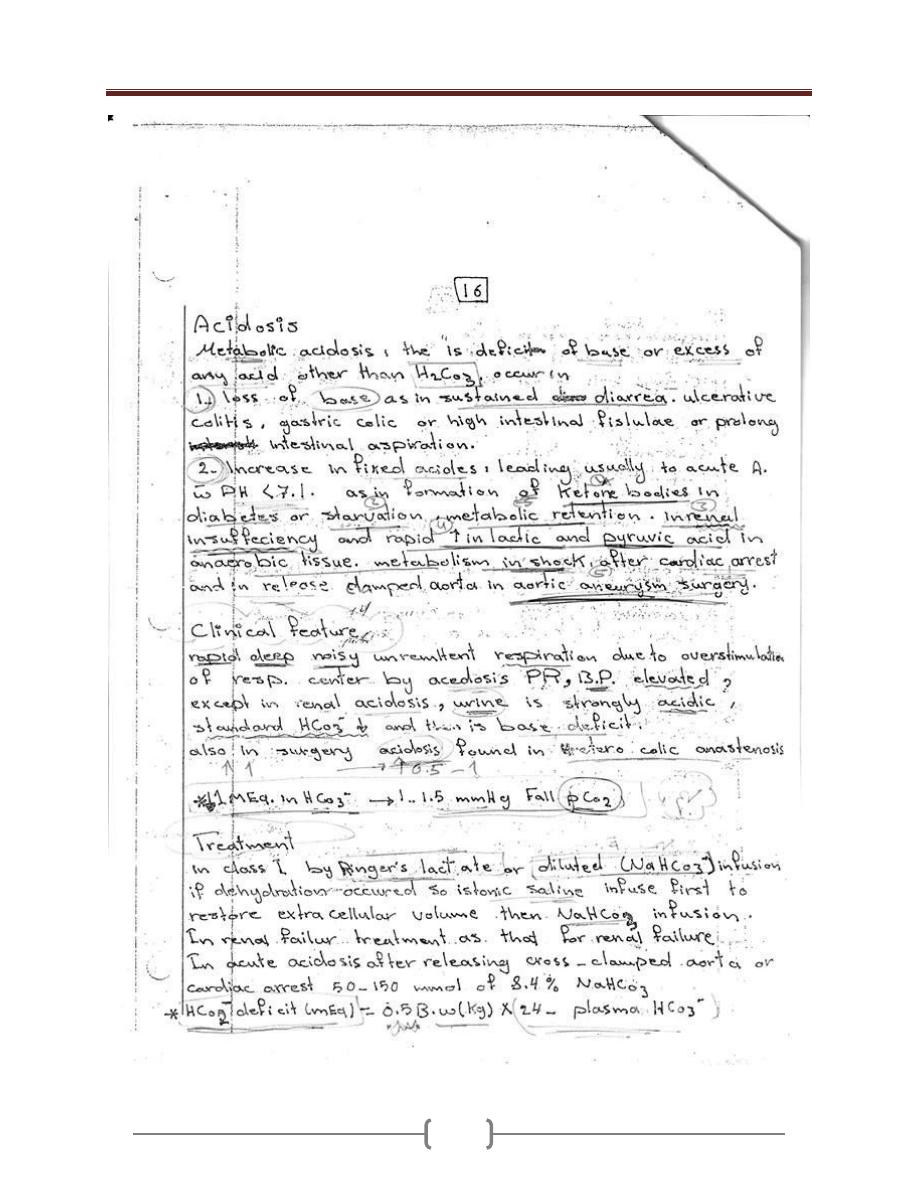
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
46
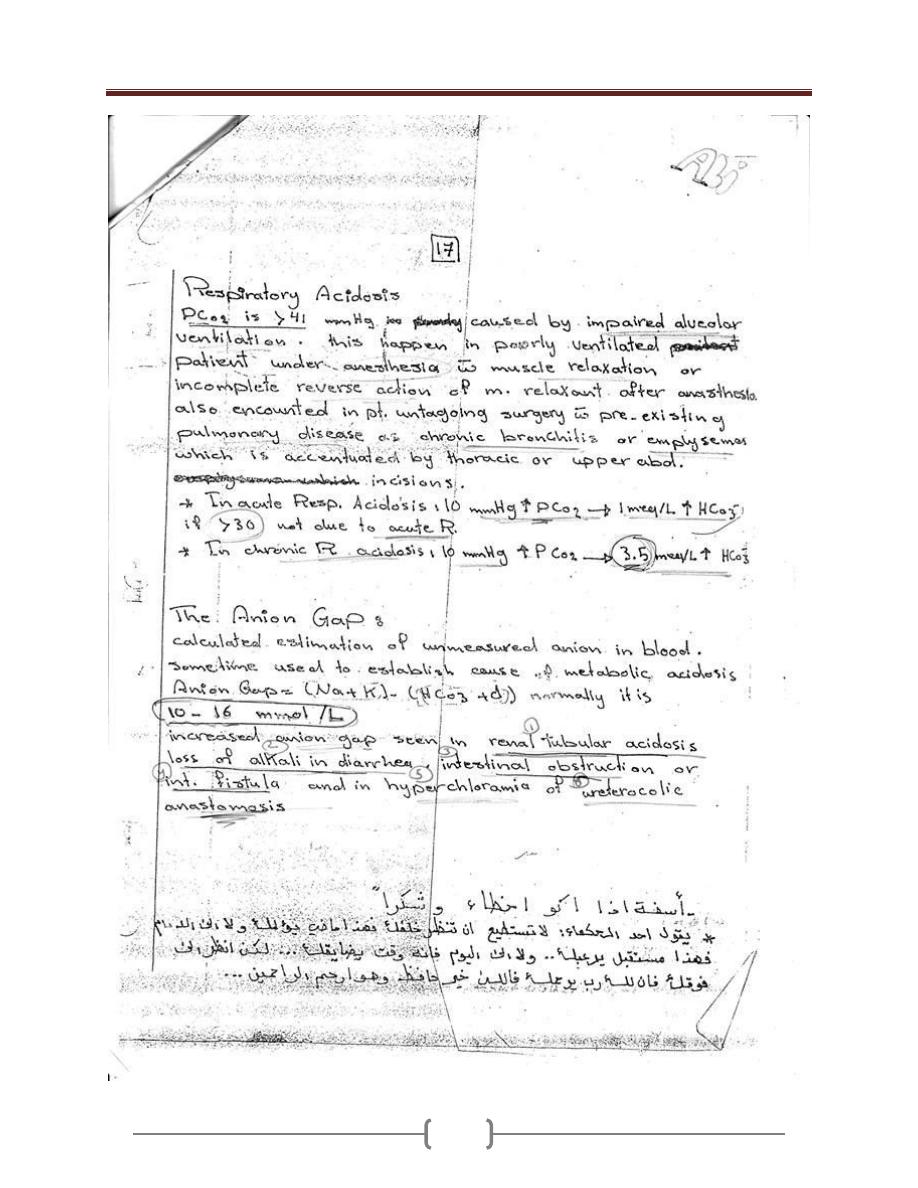
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
47
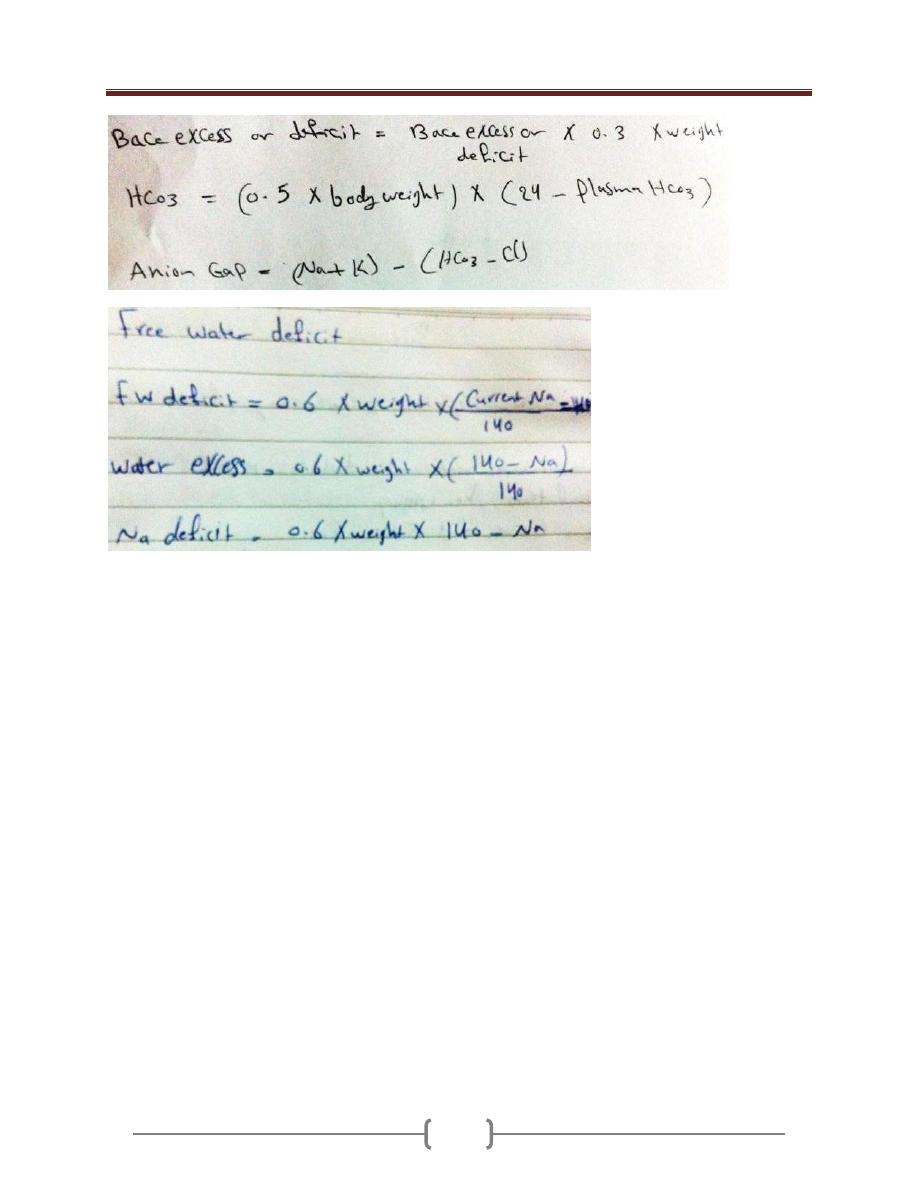
Lecture 8+9 – Fluid Electrolyte & Acid-Base balance
48
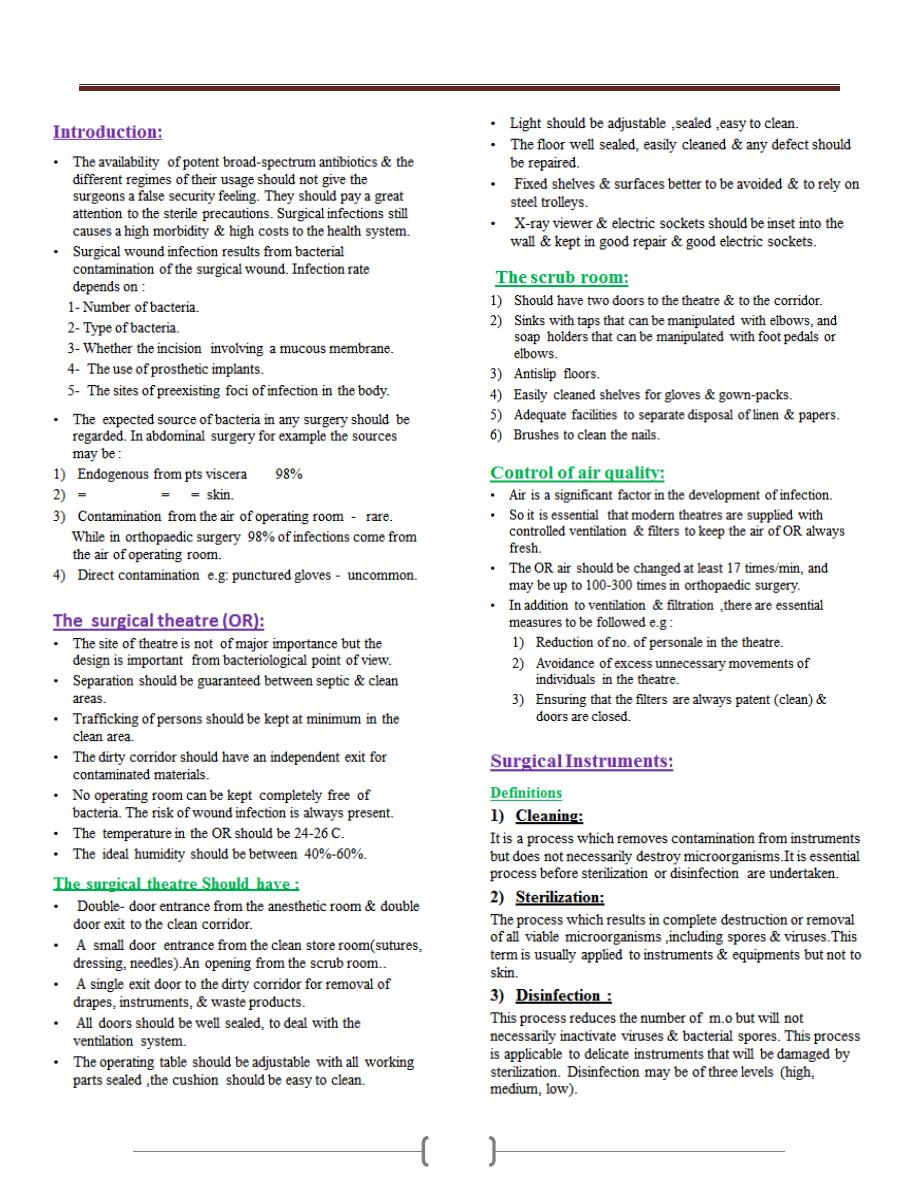
Lecture 10+11 - Operating Room Sterilization & Sterile precautions
49
Lecture 10+11 - Operating Room Sterilization & Sterile precautions
50
Lecture 10+11 - Operating Room Sterilization & Sterile precautions
51
Lecture 12+13 - Burn lecture
52
Lecture 12+13 - Burn lecture
53
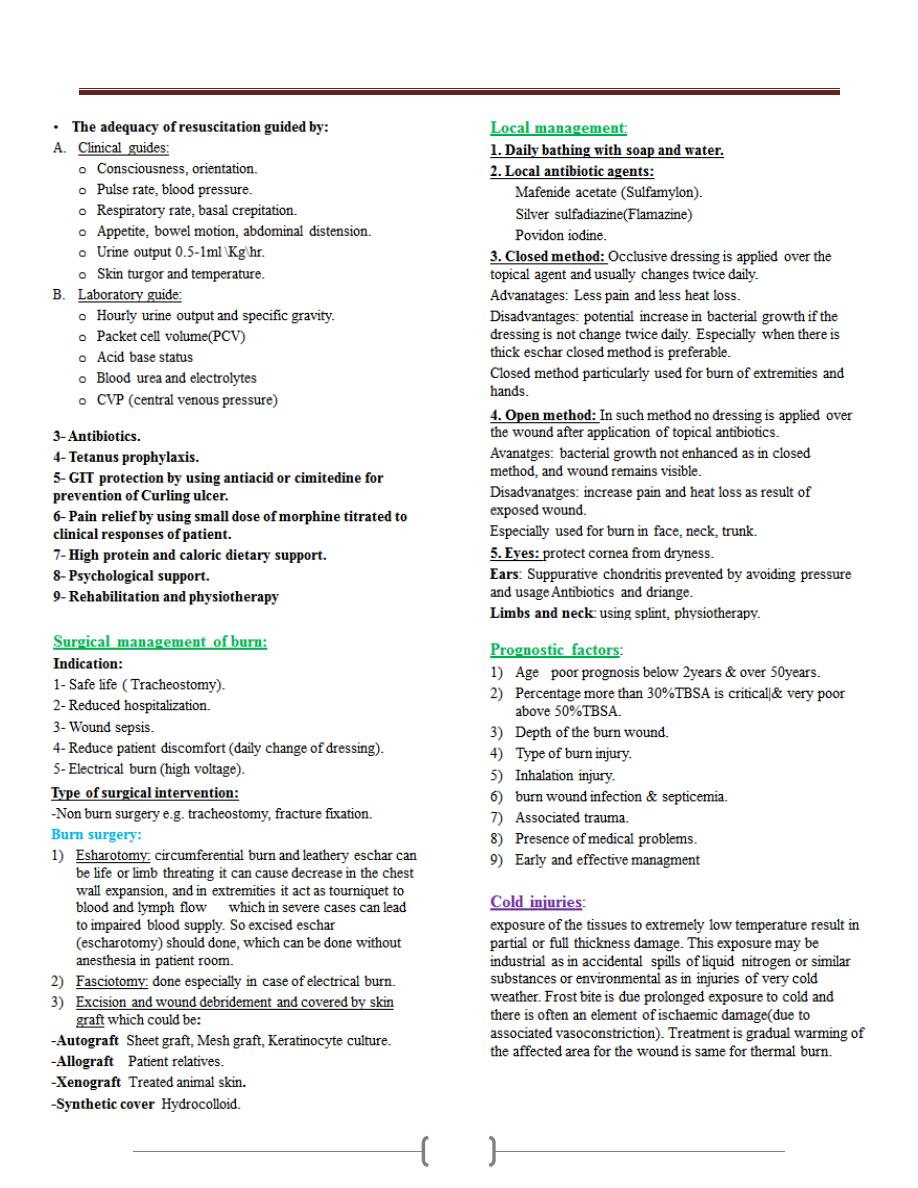
Lecture 12+13 - Burn lecture
54
Lecture 12+13 - Burn lecture
55

56
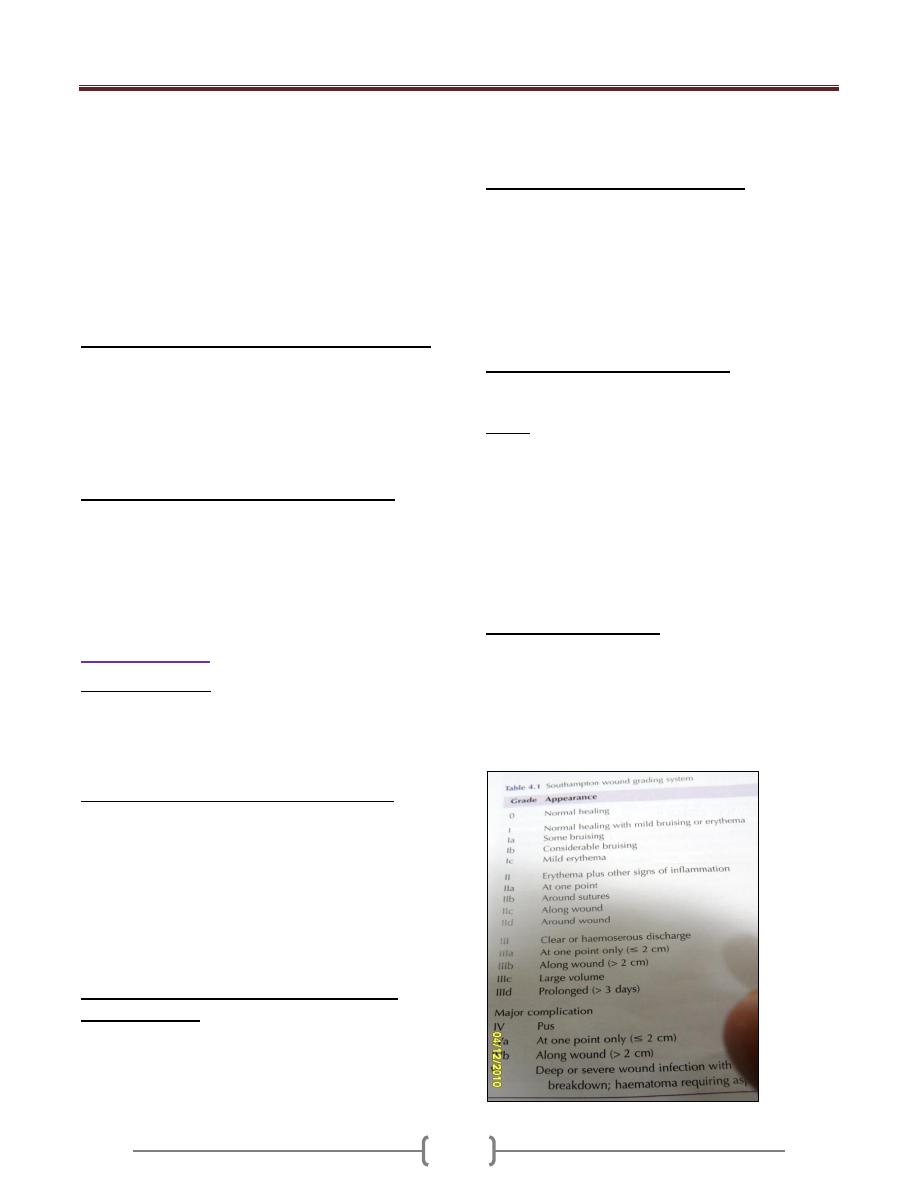
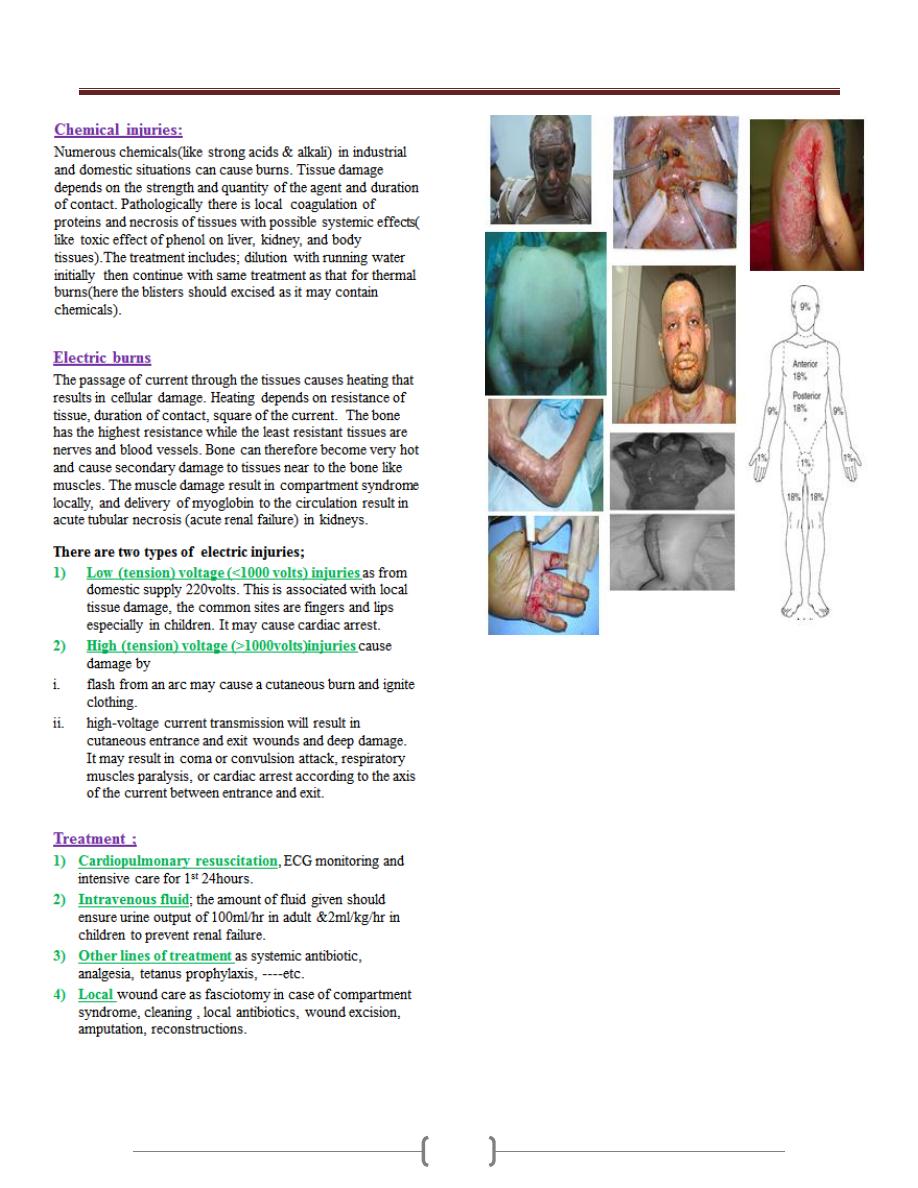
Lecture 1 - Surgical infection
57
Surgical infection has always been a major complication of
surgery& trauma & has been documented for 4000-5000 year
The Egyptians had some concepts about infection as they were
able to prevent putrefaction, testified by mummification skills.
The Hippocratic teaching described the use of anti-
microbials such as wine and vinegar.
Ignac puerperals sepsis could be reduced from over 10% to
under 2% by the simple act of hand-washing between cases
Koch laid down the first definition of infective disease by
microbes.
Koch postulates proving of an infective organism:
It must be found in considerable numbers is the septic
focus
It should be possible to culture it in a pure form from that
septic focus
It should be able to produce similar lesions when injected
into another host
Advances in the control infection in surgery:
1) Aseptic operating theatre techniques have replaced toxic
antiseptic techniques
2) Antibiotics have reduced postoperative infection rates
after elective and emergency surgery
3) Delayed primary, or secondary, closure remains useful in
contaminated.
Wound infection
Protective factors:
1) Intact epithelial surfaces.
2) Chemical.
3) Humeral.
4) Cellular phagocyte, macrophages, W.B.C.
Factors for increase risk of wound infection:
Malnutrition
Obesity
Weight loss (D.M. ,uremia, jundice)
Immunosuppression cancer, AIDS, steroid
Colonisation & translocation in the gastronintestinal tract
Poor perfusion.
F .b. material.
Poor surgical technique.
Factors that determine whether a wound will
become infected:
1) Host response
2) Virulence and inoculum of infected agent
3) Vascularity and health of tissue being invaded
including local ischaemia as well as systemic shock
4) Presence of dead or foreign tissue
5) Presence of antibiotics during the decisive period.
Classification of sources of infection:
Primary: acquired from a community or endogenous
source (such as that following a perforated peptic ulcer)
Secondary or exogenous (HAI): acquired from the
operating theatre (such as inadequate air filtration) or the
ward (e.g. poor hand –washing compliance) or from
contamination at or after surgery (such as an anastomotic
leak).
Local and systemic manifestation :
Infection is invasion of m.o. through tissues foloowing a
breakdown of local and systemic host defences.
Sepsis: is the systemic manifestation of a documented
infection include:
hyperthermia > 38c
Hypothermia <36c
Tachycardia or tachypnia
Increase WBC >12* 10^9/L
Sever sepsis or sepsis syndrom is sepsis with evidence
of one or more organ failure.
Infection may be 1-Endogenous. 2-Exogenous.
Major Wound Infection:
It discharge pus
Systemic manifestation of tachycardia, pyrexia and
increase WBC.
Minor Wound Infection
May discharge pus but should not be associated with
excessive discomfort,systemic signs or delay in return home.
Lecture 1 - Surgical infection
58
Types of infection
1) wound abscess:
It is characterized by heat, redness, pain, swelling, loss of
function.
M.o. is pyogenic staph. Aureus.
Consequence of abscess;
-May discharge spontaneously
1.May need debridment and curretage
2.Chronic abscess,fistula or sinus
3.Perianastomotic abscess.
4.Deep cavity abscess.
The role of antibiotic is controversial unless there is signs
of spreading infection (cellulitis or lymphangitis).
Surgical curretage and decompression must be adequate.
Delayed primary or secondery suture is safer than
primary.
2) Cellulitis and Lymphangitis:
It is non suppurative invasion infection of tissues.
There is sign of inflammation with poor localisation.
M.o. is B. haemolytic streptococcus , staph. Or
c.perfringene.
There is tissue destruction and ulceration.
Systemic signs of toxaemia are common.
Lymphangitis present as painful red streaks in affected
lymphatic and often accompanied by painful lymph node
in the related drainage area.
3) Gas Gangrene:
It is caused by C.perfringens
Usually found in nature ,soil and faeces
Military, traumatic, and colorectal operation.
Wound infection,sever local wound pain and crepitus with
gas in the tissue
Wound appear as thin brown sweet swelling exudate,
oedema, and spreading gangrene, systemic complication,
circulatory collapse and MSOF.
Prophylaxis is with large doses of I.V. penicillin and
debridement of affected tissue.
Treatment:
Suppurative wound infection take 7-10 days
Cellulitis appear in 3-4 days
Major wound infection or cellulitis need antibiotic either
impirical or based on culture and sensitivity
Change of antibiotic lead to resistance.
When wound is under tension and there suppuration so
removal of sutures and evacuation of pus.
In severely contaminated wound ,it is logic to leave the
skin layer open & delayed primary or secondary suture
Sample of pus is taken for culture and sensitivity.
Prophylaxis:
By I.V. antibiotic should be given at induction of
anasthesia when local wound defences are at their least
(decisive period) and before contamination occur.
Ex. Lower limb amputation, patient with known valvular
disease of the heart.
Amoxyl for dental surgery
Second generation cephalosporine for urology
In open viscus surgery metronidazol is added.
Preoperative preparation:
Short preoperative hospital stay
The value of personal hygiene
Shaving should be undertaken immediately before surgery
Scrubbing of operating hands
Skin preparation by hibiscrub ,betadine ,savlyon
Theatre technique
Operator skill in gentle manipulation and dissection with
avoidance of dead space and haematoma.
Similar wound surveillance is needed in postoperative
care.
Major wound infection:
significant quantity of pus
delayed return home
patient are systemically ill
Lecture 2+3 – Cyst, Ulcer, sinuses & Fistulas
59
Cysts (bladder)
Definition
Classification of cysts
Lecture 2+3 – Cyst, Ulcer, sinuses & Fistulas
60
Clinical features
Differential diagnosis
Diagnosis
Complication
Ulcers
Definition
Types
Trophic ulcer
Lecture 2+3 – Cyst, Ulcer, sinuses & Fistulas
61
Life history of an ulcer
Zones of healing
Clinical examination of an ulcer
Local treatment of nonspecific ulcer
The ideal dressing should have
Lecture 2+3 – Cyst, Ulcer, sinuses & Fistulas
62
Antiseptic and topical antibodies
Wound dressing
Sinuses & Fistulas
Sinuses
Fistula
Causes of persistence of Fistulas & Sinuses
Treatment
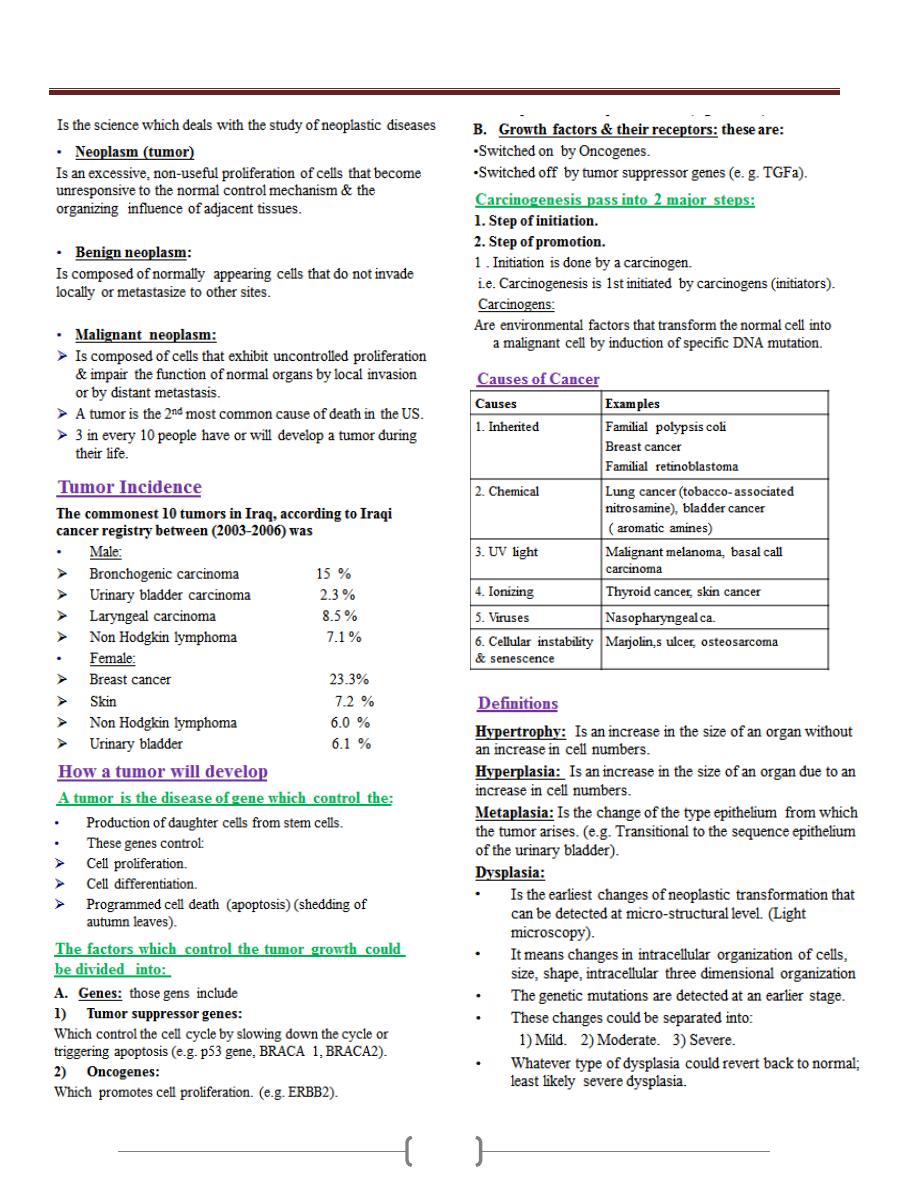
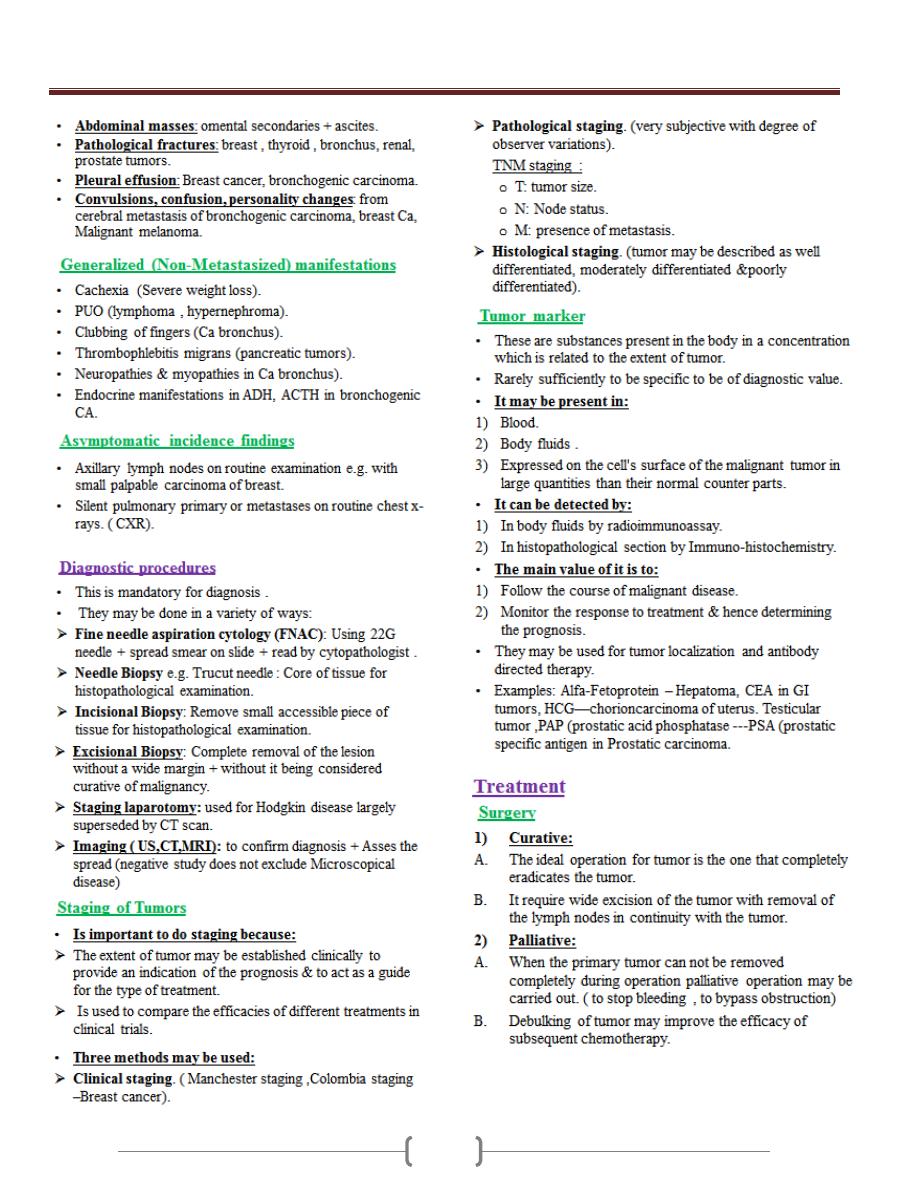
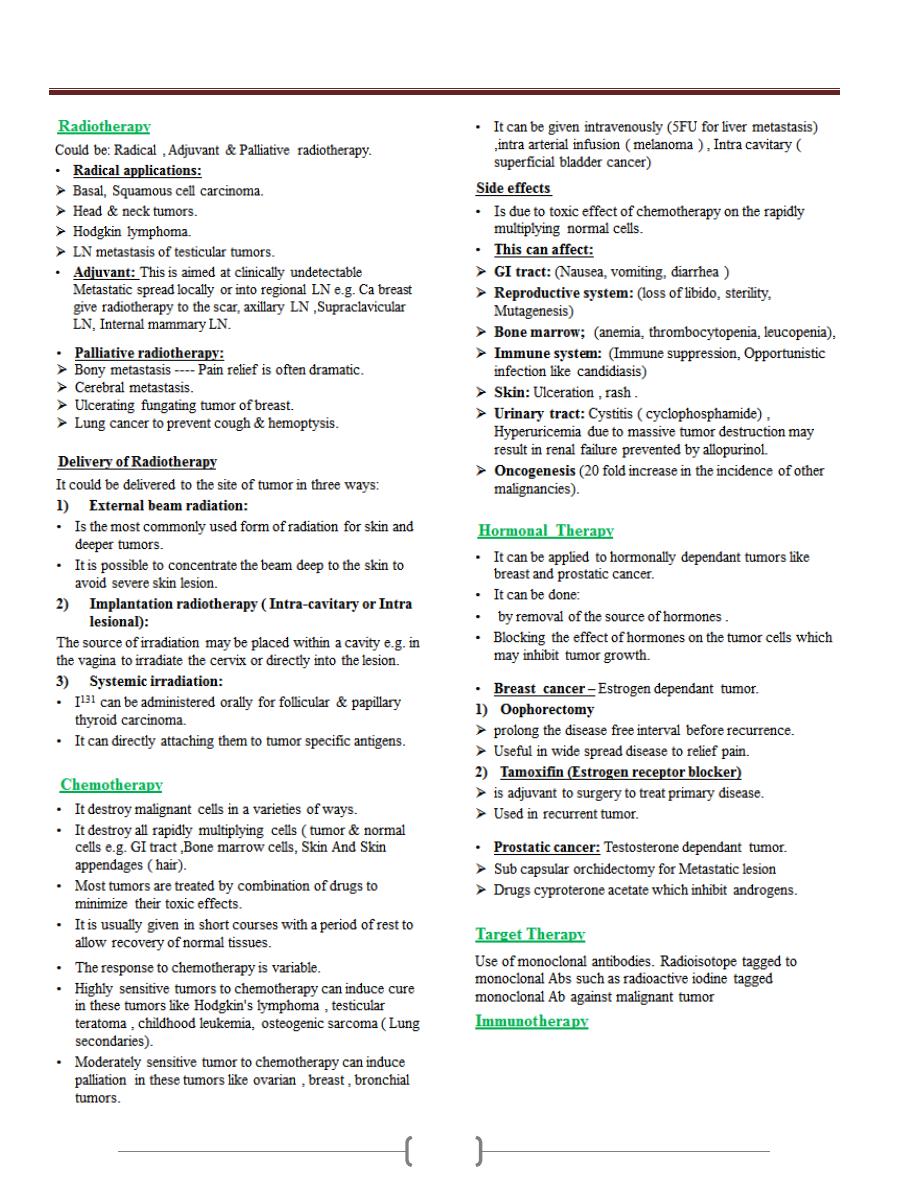
Lecture 4+5+6 - Oncology
63
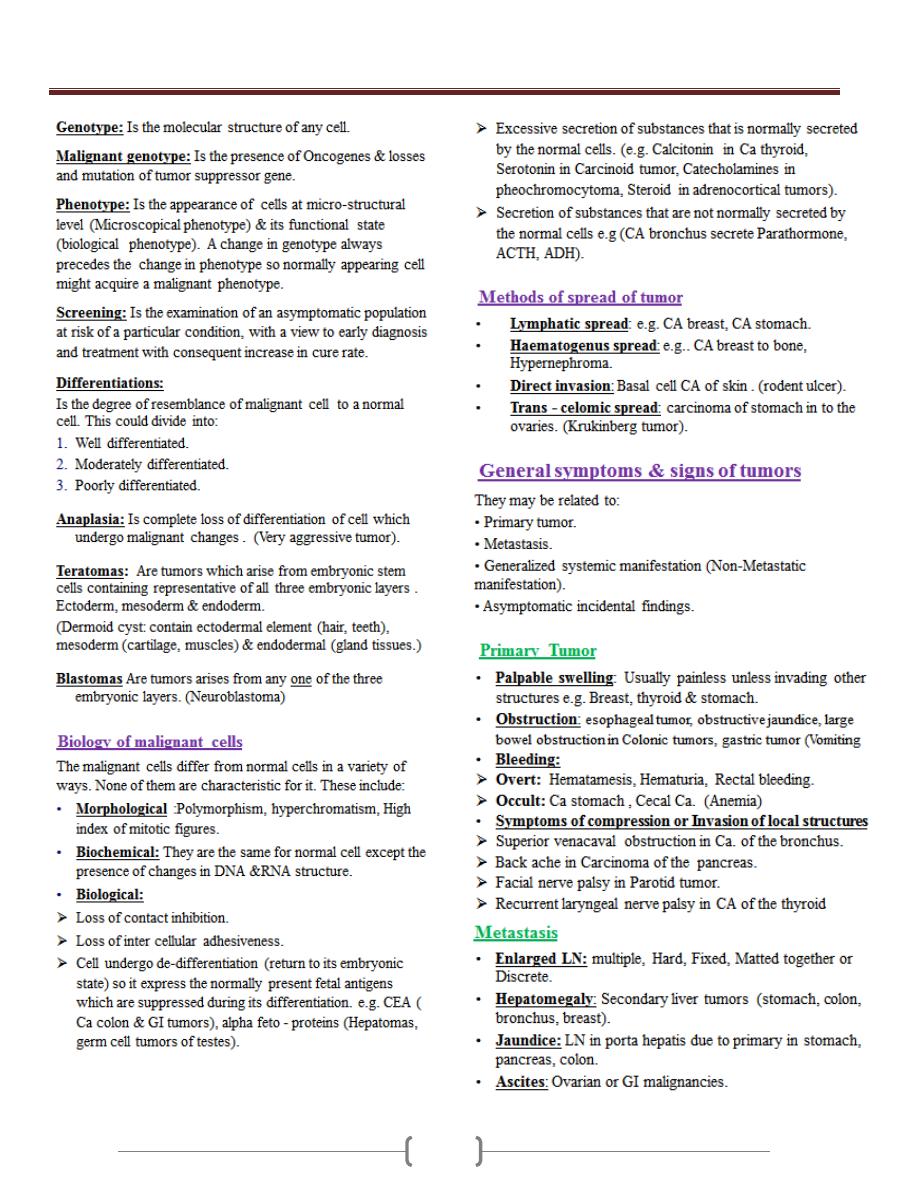
Lecture 4+5+6 - Oncology
64
Lecture 4+5+6 - Oncology
65
Lecture 4+5+6 - Oncology
66
Lecture 7+8 – Artificial nutritional support
67

Lecture 7+8 – Artificial nutritional support
68
Lecture 7+8 – Artificial nutritional support
69
Lecture 7+8 – Artificial nutritional support
70
Lecture 7+8 – Artificial nutritional support
71
Lecture 7+8 – Artificial nutritional support
72
Lecture 7+8 – Artificial nutritional support
73
Lecture 7+8 – Artificial nutritional support
74
Lecture 7+8 – Artificial nutritional support
75
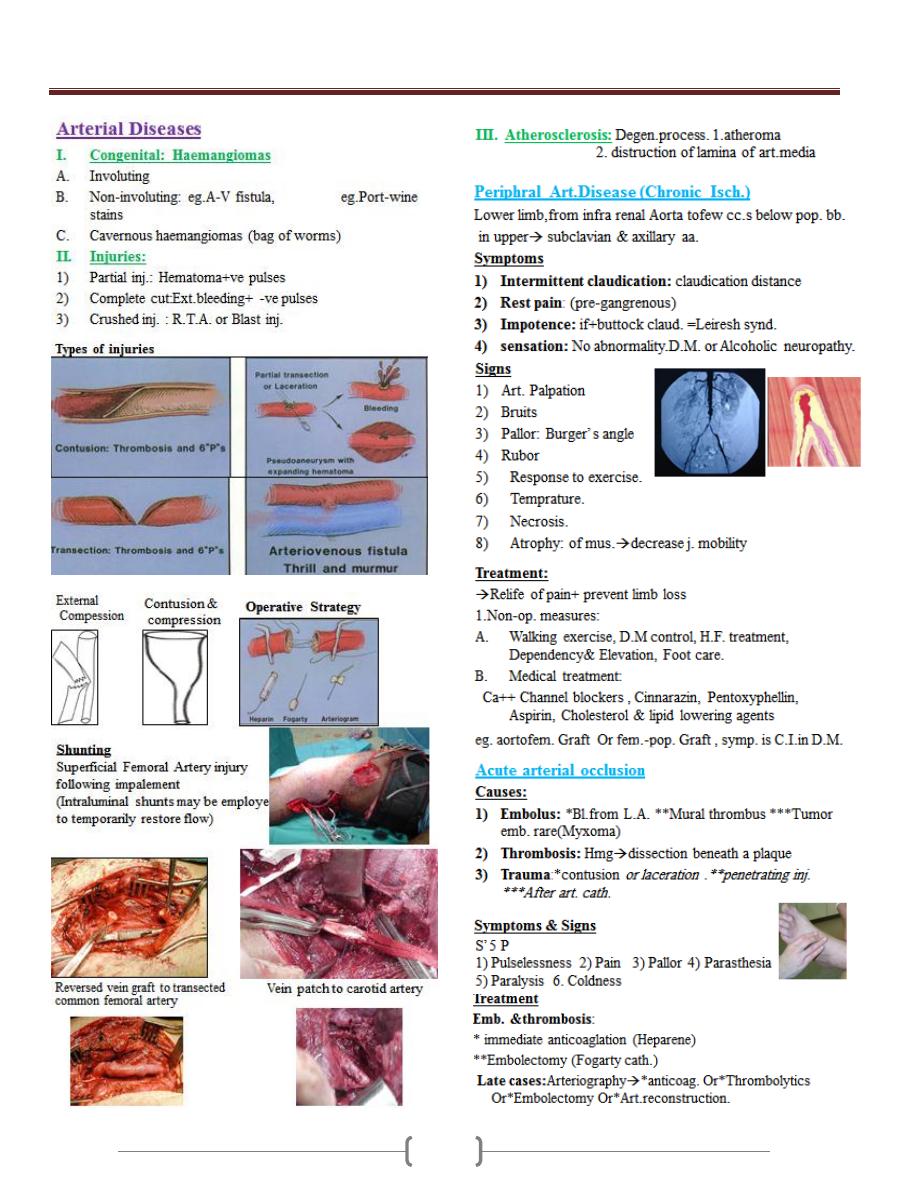
Lecture 9 - Vascular Surgery
76
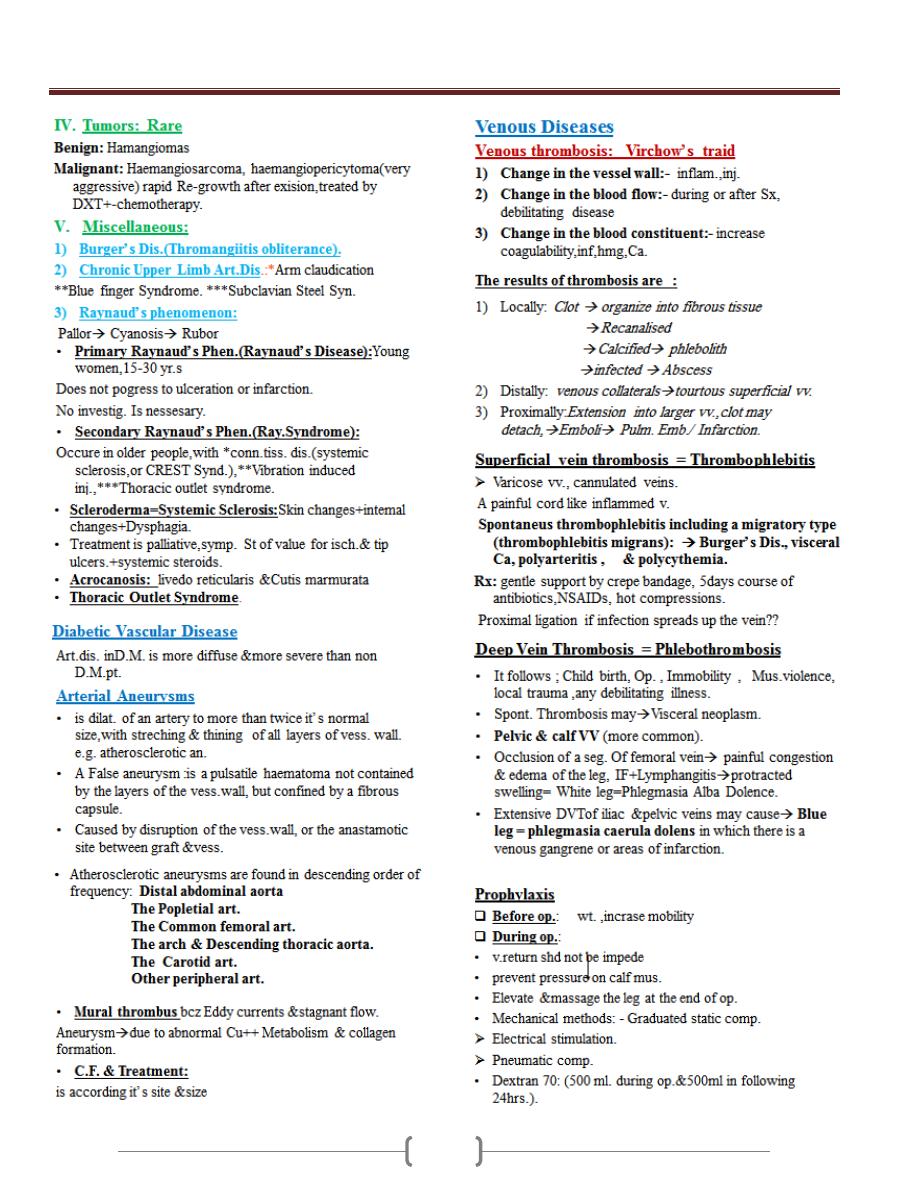
Lecture 9 - Vascular Surgery
77
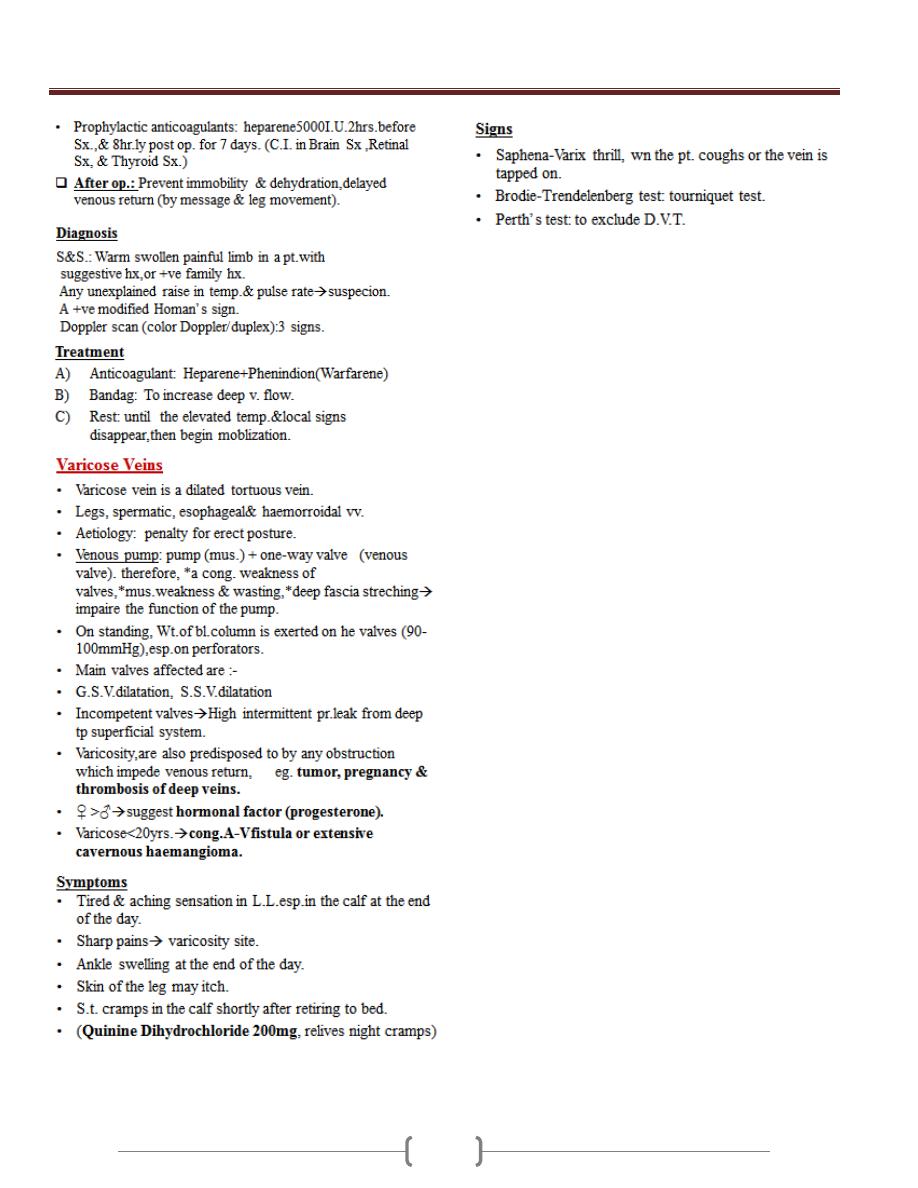
Lecture 9 - Vascular Surgery
78
