Gynaecology
Dr. Raghad
Lec 23 - Development of The Genital Tract
DR. RAGHAD - LEC 2

1
Normal and Abnormal Development of the
Genital Tract
Embryology
Sexual differentiation and its control are vital to the continuation of our
species. The basis of mammalian development is that a 46XY embryo will
develop as a male and a 46XX embryo will differentiate into a female. It is,
however, the presence or absence of the Y chromosome which determines
whether the undifferentiated gonad becomes a testis or an ovary.
There are several genes involved in the formation of the bipotential
gonad and later the testis and the ovary. It has been proven that the testis
determining factor is on chromosome Yp11.31 and this gene is termed the SRY
(sex-determining region of the Y chromosome). This gene triggers testis
formation from the indifferent gonad. Mutations of SRY cause pure gonadal
dysgenesis or hermaphroditism.
Ovarian differentiation seems to be determined by the presence of two
X chromosomes and the ovarian determinant is located on the short arm of
the X chromosome and this was discovered as a result of the absence of the
short arm results in an ovarian agenesis. It is believed at the present time that
DAX1 is the gene which determines the differentiation of the bipotential gonad
to an ovary.
Influence of the differentiated gonad on the development of other
genital organs is thus fundamental and the presence of a testis will lead to male
genital organ development, but if the testes do not form the individual will
develop female genital organs whether ovaries are present or not.
Development of the genital organs
The genital organs and those of the urinary tract arise in the
intermediate mesoderm on either side of the root of the mesentery beneath
the epithelium of the coelom. Mesonephric (Wolffian) duct gives rise to male
genital organs while the paramesonephric (Müllerian) duct gives rise to most
of female genital organs.

2
At the beginning of the third month, the Müllerian and Wolffian ducts
and mesonephric tubules are all present and capable of development. From
this point onwards in the female there is degeneration of the Wolffian system
and marked growth of the Müllerian system. In the male the opposite occurs as
the result of production of Müllerian-inhibitory substance (MIS) produced by
the fetal testis.
o The lower ends of the Müllerian ducts come together in the midline, fuse
and develop into the uterus and the cervix, while the cephalic ends of
the duct remain separate to form the fallopian tubes. The thick muscular
walls of the uterus and cervix develop from proliferation of mesenchyme
around the fused portion of the ducts.
Diagrammatic representation of genital tract development. (a) Indifferent stage; (b) female
development; (c) male development.
o Vagina developed from both paramesonephric duct and from the
urogenital sinus.
o The genital tubercle gives rise to clitoris in female and to penis in male.
o The genital folds become labia minora in female and penile urethra in
male.
o The genital swellings enlarge to become labia majora in female or
enlarge and fuse to form the scrotum in male.
3
Genital Tract Malformations
Uterine anomalies:
1) ABSENCE OF THE UTERUS: The uterus may be absent or of such
rudimentary development as to be incapable of function of any kind. This
condition is known as the Mayer-Rokitansky Kuster Hauser syndrome
(MRKH). This type of anomaly is usually found when the vagina is absent
also.
Presentation: primary amenorrhea. These patients have a 46XX
chromosome complement and normal ovarian function. However, cases of
absent uterus with the lower part of the vagina ending blindly, associated
with absence or scanty appearance of pubic hair must raise the suspicion of
androgen insensitivity.
Unfortunately, no treatment is currently possible for such uterine
abnormalities and in those cases where the diagnosis is androgen
insensitivity removal of any testicular tissue must be undertaken to avert
long-term risk of malignant change.
2) FUSION ANOMALIES: Fusion anomalies of various kinds are not uncommon
and may present clinically either in association with pregnancy or not.
v
The lesser degrees of fusion defects are quite common, the cornual
parts of the uterus remaining separate, giving the organ a heart-
shaped appearance known as the bicornuate uterus. Such minor
degrees of fusion defects DO NOT give rise to clinical signs or
symptoms.
v
The presence of a septum extending over some or the entire uterine
cavity, however, is likely to give rise to clinical features. Such a
septate or subseptate uterus may be of normal external appearance
or of bicornuate outline.
Presentation:
ü
it may present with recurrent spontaneous abortion or
malpresentation. A persistent transverse lie of the fetus in late
pregnancy may suggest a uterine anomaly since the fetus tends to lie
with its head in one cornu and the breech in the other.
(In more extreme forms of failure of fusion the clinical features may be less,
rather than more, marked).
4
ü
Two almost separate uterine cavities with one cervix are probably less
likely to be associated with abnormalities than are the lesser degrees of
fusion defect.
ü
Complete duplication of the uterus and cervix (uterus didelphys), if
associated with a clinical problem, may prevent descent of the head in
late pregnancy, or obstruct labour by the non-pregnant horn.
ü
Rudimentary development of one horn may give rise to a very serious
situation if a pregnancy is implanted there. Rupture of the horn with
profound bleeding may occur as the pregnancy increases in size. The
clinical picture will resemble that of a ruptured ectopic pregnancy with
the difference that the amenorrhea will probably be measured in months
rather than weeks, and shock may be profound. A poorly developed or
rudimentary horn may give rise to dysmenorrhea and pelvic pain if there
is any obstruction to communication between the horn and the main
uterine cavity or the vagina. Surgical removal of this rudimentary horn is
then indicated.
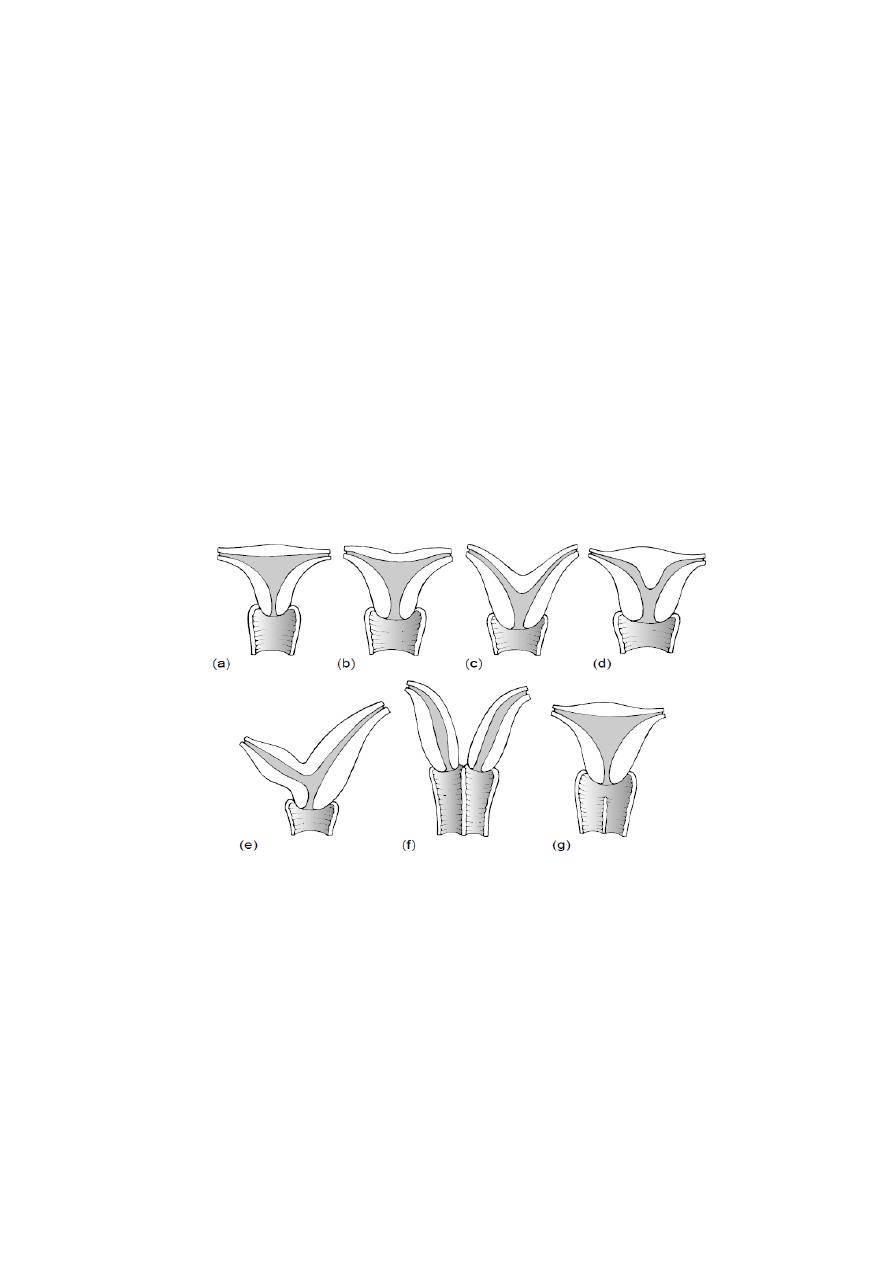
Various fusion abnormalities of the uterus and vagina. (a) Normal appearance; (b) arcuate
fundus with little effect on the shape of the cavity; (c) bicornuate uterus; (d) subseptate
uterus with normal outline; (e) rudimentary horn; (f) uterus didelphys; (g) normal uterus
with partial vaginal septum.
5
Vaginal anomalies
ABSENCE OF THE VAGINA
Absence of the vagina is generally associated with absence of the uterus
or a rudimentary uterus. This is known as MRKH syndrome. Rarely the uterus
may be present and the vagina, or a large part of it, is absent.
Presentation: the patient will probably present between age 12 and 16 years
with primary amenorrhea. Secondary sexual characteristics will be present as
the ovaries are normally developed and functional. This combination of normal
secondary sexual development and primary amenorrhea suggests an
anatomical cause, such as an imperfect or absent vagina, for the failure to
menstruate.
Examination: Inspection of the vulva and abdominal examination will be
required to exclude the presence of any retained blood in the upper part of the
genital tract and will delineate the abnormality. (Vulval development is normal)
Investigation: In every case of apparent vaginal absence a Karyotype should be
performed and if chromosome analysis confirms an XY sex chromosome
complement the case should be managed appropriately.
All patients with abnormalities of the lower genital tract should have the
renal tract investigated. Some 40% of patients with lower genital tract
abnormalities will be found to have renal abnormalities, 15% of whom have an
absent kidney. All patients should have a renal ultrasound performed to
determine whether there is absence of a kidney and if more detailed analysis of
the urinary tract is required this may be performed by intravenous urography.
Treatment: Once the diagnosis is certain, management may be divided into
two sections:
- the first devoted to psychological counseling
- the second aspect which involves the creation of a new vagina, and this is
either by non-surgical method using graduated glass dilator or surgically by
vaginoplasty.
6
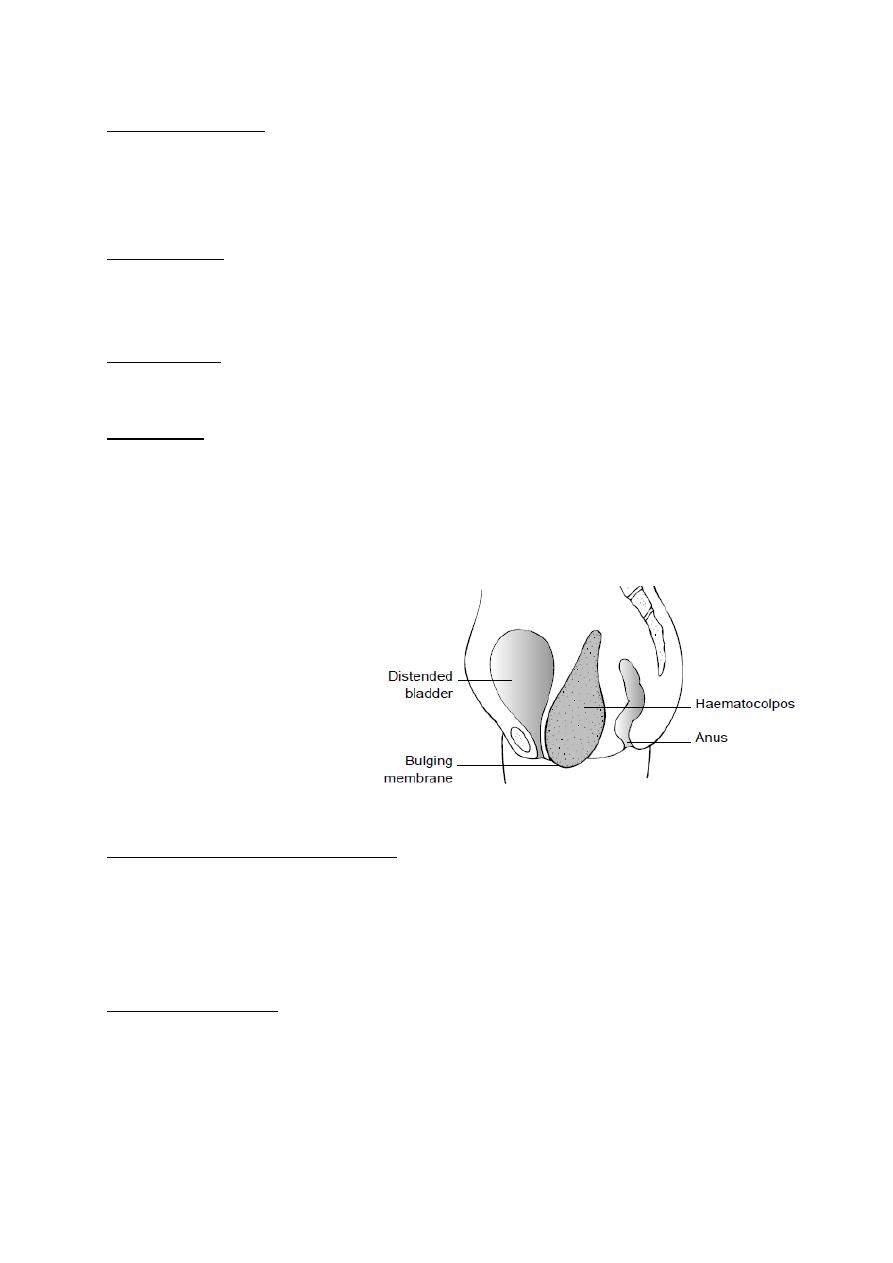
HAEMATOCOLPOS
An imperforate membrane may exist at the lower end of the vagina,
which is loosely referred to as the imperforate hymen, although the hymen can
usually be distinguished separately.
Presentation: At puberty (14-15 years old) the retention of menstrual flow
gives rise to the clinical features of haematocolpos. The features of
haematocolpos are predominantly cyclical lower abdominal pain, primary
amenorrhea and occasionally interference with micturition (retention of urine).
Examination: reveals a lower abdominal swelling, and per rectum a large
bulging mass in the vagina may be appreciated. Inspection of vulva may reveal
a bluish bulging membrane according to the thickness of the membrane.
Treatment: If the membrane is thin, then a simple excision of the membrane
and release of the retained blood resolve the problem.
In few cases the cause of haematocolpos is absence of some part of the
vagina. In such cases, the treatment is less straightforward. Resection of the
absent segment and reconstruction of the vagina may be done by either an
end-to-end anastomosis of the vagina or a partial vaginoplasty.
Diagrammatic view of
haematocolpos. Note how the
blood collecting in the vagina
presses against the urethra and
bladder base, ultimately causing
retention of urine
.
LONGITUDINAL VAGINAL SEPTUM
A vaginal septum extending throughout all or part of the vagina is not
uncommon; such a septum lies in the sagital plain, midline. The condition may
be found in association with a completely double uterus and cervix or with a
single uterus only.
Clinical significance: In obstetrics this septum may have some importance if
vaginal delivery is to be attempted. In these circumstances the narrow
hemivagina may be inadequate to allow passage of the fetus and serious tears
may occur if the septum is still intact at this time. It is therefore prudent to
arrange to remove the vaginal septum as a formal surgical procedure
whenever one is discovered, either before or during pregnancy.

7
Wolffian Duct Anomalies:
Remnants of the lower part of the Wolffian duct may be evident as
vaginal cysts, while remnants of the upper part may be seen as thin-walled
cysts lying within the layers of the broad ligament (paraovarian cysts). The
cysts may cause dyspareunia and this is the most likely reason for their
discovery and surgical removal.
A painful and probably paraovarian cyst will require surgical exploration
and its precise nature will be unknown until the abdomen is opened. Such cysts
normally come out easily from the broad ligament
.
Good Luck
