The wrist and hand
Dr. Ammar Talib Al- YassiriCollege of Medicine / Baghdad University
CONGENITAL ANOMALIES OF THE WRIST AND HAND
CLASSIFICATION:failure of formation of parts;
failure of differentiation of parts;
duplication;
overgrowth;
undergrowth;
constriction bands;
generalized skeletal abnormalities.
FAILURE OF FORMATION
Transverse arrest:The most common levels of absence are at the proximal forearm and midcarpus, then at the metacarpals and humerus.
Associated anomalies are unusual.
Treatment:
Proximal forearm:
Prosthetic fittings in young children
myoelectric prostheses in older children
and adolescents
Transverse arrest of fingers
microvascular transfer of a toe
non-vascularized transfer of a toe phalanx
Longitudinal arrest
radial (pre-axial),ulnar (post-axial),
central (cleft hand) or
intersegmental (intercalated) structures
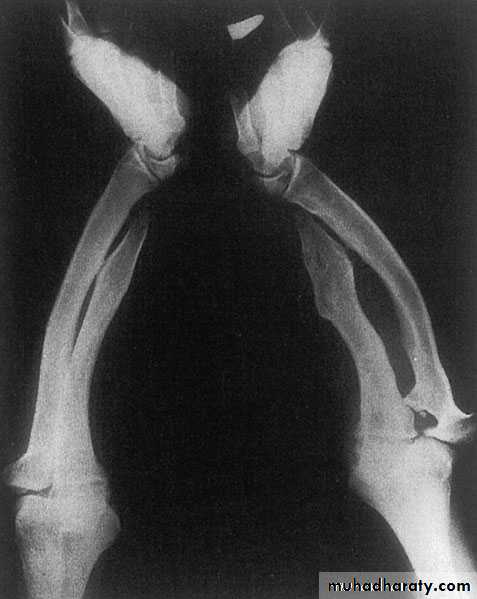
RADIAL DYSPLASIA
rare condition (incidence 1:50 000 to 1:100 000 live births)may involve any (or all) of the structures from the elbow to the thumb, it usually occurs as an isolated abnormality
occasionally associated with other skeletal, cardiac, haematological, renal or craniofacial anomalies
The infant is born with the wrist in marked radial deviation ‘radial club hand’
half the patients are affected bilaterally
There is absence of the whole or part of the radius; often the thumb, scaphoid and trapezium fail to develop normally.
Treatment:
mild→gentle stretching and splintage,
More serious cases →distraction prior to a tension-free soft-tissue correction
older technique of ‘centralizing’ the carpus over the remaining forearm structures.
ULNAR DYSPLASIA
less common than radial dysplasiaMost cases are sporadic, but the condition may be part of a larger syndrome,
The new-born infant presents with ulnar deviation of the wrist (or both wrists),
Due to partial or complete absence of the ulna;
some of the carpal bones may be absent
ulnar rays of the hand may be missing.
With growth the radius elongates and bowed;
ultimately the radial head may dislocate.
Treatment
stretching and splinting
excision of any tethering ulnar anlage and osteotomy of the radius
the radial head can be excised
(The Straub procedure).
CENTRAL DYSPLASIA (CLEFT HAND)
The true cleft hand presents with V-shaped cleft in the centre of the handmay be associated with the absence of one or more digits, transverse bones, syndactyly of digits bordering the cleft, and a tight first web space.
Surgery is complex, having to deal with closure of the cleft, reconstruction of the first web space
INTERCALARY SEGMENTAL DYSPLASIA
Very rarely an intercalary segment in the upper limb fails to developthe forearm or hand may be attached directly to the trunk,
or the hand is attached to the humerus.
also known as phocomelia
FAILURE OF DIFFERENTIATION
Syndactyly:Conjoined digits is the commonest congenital malformation
The anomaly may be
simple (soft tissue only) or complex (skin and bone),
complete (affecting the entire web) or incomplete (only part of the web).
Treatment:
Mild incomplete, of central digits need no treatment
complete syndactyly involves separation and skin grafting.
DUPLICATION
Polydactyly (‘extra digits’)
radial (pre-axial),
the ulnar (post-axial)
the central part of the hand.
Duplication of the little finger:
is one of the most common
often inherited
If a phalanx or entire digitis duplicated, removal and soft-tissue reconstruction
Duplications of the thumb or central digits:
extremely rare
require complex reconstructive surgery of the digit, its tendons and the overlying skin.
OVERGROWTH
DDX: other forms of enlarged digitsNeurofibromatosis
multiple enchondromatosis
vascular malformations
TREATMENT:
Surgical correction: extremely difficult and unrewarding.
Amputation may be the best option.
UNDERGROWTH
Undergrowth (brachydactyly) is common
May be part of a wider syndrome (e.g. Turner’s syndrome).
It can affect a single bone, a digit or an entire limb.
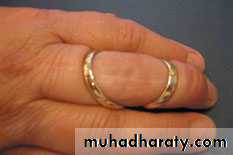
CONSTRICTION RING SYNDROME
The condition presents as localized ‘strangulation’, most commonly of the ring finger;
the distal part of the finger may be painful, swollen and cyanotic, or sometimes threatened with amputation
Treatment consists of excision of the constricting band and soft-tissue reconstruction using multiple Z-plasties
Madelung’s deformity
congenital or post-traumatic,the lower radius curves forwards (ventrally), carrying with it the carpus and hand but leaving the lower ulna sticking out as a lump on the back of the wrist.
The congenital
isolated entity
part of a generalized dysplasia;
although the abnormality is Present at birth but is rarely seen before the age of 10 years.
Function is usually excellent.
Treatment: If deformity is severe, the lower end of the ulna may be shortened; this is sometimes combined with osteotomy of the radius
KIENBOCK’S DISEASE
a form of ischaemic necrosis, probably due to chronic stress or injury
Pathology:the pathological changes proceed in four stages
Clinical features:
young adult,
Ache and stiffness.
Tenderness
grip strength is diminished.
movements are limited and painful
Imaging:
Radioscintigraphy may reveal
increased activity
X-rays
MRI
Treatment
NON-OPERATIVE TREATMENT
splintage of the wrist for 6–12 weeks
OPERATIVE TREATMENT
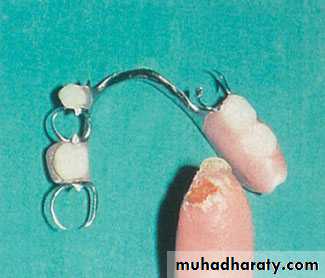
pedicled bone graft
shortening the radius
replacement by a silicone prosthesis
intercarpal fusion or excision of the proximal row of the carpus
radio-carpal arthrodesis
Wrist replacement
DE QUERVAIN’S DISEASE
Pathology: reactive thickening of the sheath around the extensor pollicis brevis and abductor pollicis longus tendonsClinical features
woman aged 40–50
Pain on the radial side of the wrist
history of unaccustomed activity
Swelling
Tenderness
Finkelstein’s test
(hitch-hiker’s sign)
The differential diagnosis:
arthritis at the base of the thumb
scaphoid non-union
intersection syndrome
Treatment
SWELLINGS AROUND THE WRIST
GANGLION CYSTSthe most common swelling in the wrist
Pathology
Clinical features
young adult,
painless lump
occasionally there is slight ache and weakness
Treatment
EXTENSOR TENOSYNOVITIS
Localized swelling of a tendon sheath on the dorsum of the wrist
CARPO-METACARPAL BOSS
firm round swelling over the back of the second and third carpo-metacarpal joint
may be caused by some instability at the joint.
COMPOUND PALMAR GANGLION’
Chronic inflammation distends the common sheath of the flexor tendons both above and below the flexor retinaculum.
CARPAL TUNNEL SYNDROME
Carpal tunnel is a fibro-osseous tunnelthere is barely room for all the tendons and the median nerve
compression and ischaemia of the nerve.
(1)the soft tissues increase in bulk (pregnancy,menopause, myxoedema ,rheumatoid arthritis,trauma or drugs) or
(2) there is a local obstruction (e.g. a ganglion or osteophytic spur).
Clinical features:
Pain and paraesthesia
Night after night the patient is woken with burning pain, tingling and numbness.
clumsiness and weakness
more common in women (40–50 y) ; in younger patients it is not uncommon to find related factors such as pregnancy, rheumatoid disease, chronic renal failure or gout.
Tinel’s sign
Phalen’s test.
In late cases there is wasting of the thenar muscles, weakness of thumb abduction and sensory dulling in the median nerve territory.
Electrodiagnostic tests are reserved for those with atypical symptoms
Differential diagnosis: Radicular symptoms of cervical spondylosis
TreatmentLight splints
Steroid injection into the carpal canal, provides temporary relief
Open surgical division of the transverse carpal ligament usually provides a quick and simple cure.
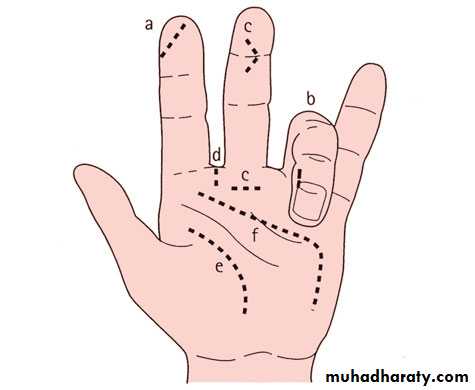
Cuts and burns of the palmar skin are liable to heal with contracture
Surgical incisions should never cross skin creases perpendicularly they should lie more or less parallel or oblique to them, or in the mid-axial line of the fingers
A useful alternative zig-zag incision
Treatment:
excision of the scar, Z-plasty of the remaining skin, skin grafts, a pedicled flap and occasionally a free flap.
SKIN CONTRACTURE
Nodular hypertrophy and contracture of the superficial palmar fascia (palmar aponeurosis).autosomal dominant trait
most common in people of European (especially Anglo-Saxon) descent
more common in males than females
prevalence increases with age
There is high incidence in epileptics receiving phenytoin therapy;
associations with diabetes, smoking, alcoholic cirrhosis, AIDS and pulmonary tuberculosis
DUPUYTREN’S CONTRACTURE
The essential problem in Dupuytren’s disease is proliferation of myofibroblasts
initial proliferative phasefibrous tissue within the palmar fascia and fascial bands within the fingers contracts
flexion deformities of the MCP and PIP joints
Fibrous attachments to the skin lead to puckering
digital nerve is displaced or enveloped, but not invaded, by fibrous tissue
Occasionally the plantar aponeurosis also is affected
:pathology
middle-aged man –
nodular thickening in the palm.
Gradually this extends distally to involve
the ring or little finger.
Pain
Often both hands are involved, one more than the other.
The palm is puckered, nodular and thick.
flexion deformities at the MCP and PIP joints.
(Garrod’s pads).
(Ledderhose’s disease).
(Peyronie’s disease).
Clinical features:
(1) skin contracture (where the previous laceration is usually obvious),
(2) tendon contracture (in which the finger deformity changes with wrist position) and(3) PIP joint contracture (in which there may
be a history of clinodactyly or joint injury).
Differential diagnosis:
Indication
nuisance or rapidly progressingPIP joint contractures can become irreversible
The aim is reasonable, not complete, correction
recurrence or extension is common
Only the thickened part of the fascia is excised (complete fasciectomy is usually unnecessary)
Skin closure may be facilitated by multiple Z-plasties
Treatment:
MALLET FINGER
injury to the extensor tendon of the terminal phalanxDue to direct trauma but more often when the finger tip is forcibly bent during active extension
terminal joint is held flexed and the patient cannot straighten it, but passive movement is normal.
X-rays show or exclude a fracture
Treatment:
TENDON LESIONS
BOUTONNIÈRE DEFORMITY
flexion deformity of the PIP joint and extension of the DIP jointinterruption or stretching of the central slip of the extensor tendon
The usual causes are direct trauma or rheumatoid disease.
treatment:
SWAN-NECK DEFORMITY
reverse of the boutonnière deformity; the PIP joint is hyperextended and the DIP joint flexed.imbalance of extensor versus flexor action at the PIP joint and laxity of the palmar plate.
Thus it may occur: (1) if the PIP extensors overact (e.g. due to intrinsic muscle spasm or contracture, after mallet finger, or following volar subluxation of the MCP joint); (2) if the PIP flexors are inadequate (inhibition or division of the flexor superficialis); or (3) if the palmar plate of the PIP joint fails (in rheumatoid arthritis, lax-jointed individuals or trauma).
Treatment depends on the cause and whether or not the deformity has become fixed.
TRIGGER FINGER (DIGITAL TENOVAGINOSIS)
A flexor tendon may become trapped by thickening at the entrance to its sheath; on forced extension it passes the constriction with a snap (‘triggering’).common in patients with diabetes.
rheumatoid disease may
Occupational factors are unlikely to be causative
Clinical features
Any digit may be affected, but the thumb, ring and middle fingers most commonly
click as the finger is flexed
tender nodule
Treatment:
injection of corticosteroid carefully placed at the mouth of the tendon sheath
Refractory cases need operation
most common sites:(MCP) joints, the wrists and
distal (RA) jointsPATHOLOGY:
Synovitis of the joints and tendon sheaths
the disease joints become eroded
attenuation of the ligaments and tendons
instability and progressive deformity
tendon rupture
Clinical features:
Stiffness and swelling of the fingers
carpal tunnel compression
swelling of the MCP and PIP joints, giving the fingers a spindle shape;
Bilateral symmetrically.
The joints are tender and crepitus may be felt on moving the tendons.
grip strength are diminished.
Early deformity : slight radial deviation of the wrist and ulnar deviation of the fingers, correctable swanneck deformities of some fingers, an isolated boutonnière or the sudden appearance of a drop-finger or mallet thumb (from extensor tendon rupture).
Late deformity: the carpus settles into radial tilt and volar subluxation; there is marked ulnar drift of the fingers and volar dislocation of the MCP joints, often associated with multiple swan-neck and boutonnière deformities.
RHEUMATOID ARTHRITIS
X-ray:
TREATMENT:EARLY STAGE DISEASE:
Established disease
Late disease
80% of people over the age of 65 have radiological signs of osteoarthritis in one or more joints of the hand; fortunately, most of them are asymptomatic.
DISTAL INTERPHALANGEAL JOINTS:
very common in postmenopausal women.
pain in one or two fingers;
swollen and tender,
On examination: bony thickening around the joints (Heberden’s nodes) and some restriction of movement.
Treatment: symptomatic, cortisone injection will give temporary relief. Joint fusion is a good solution.
OSTEOARTHRITIS
PROXIMAL INTERPHALANGEAL JOINTS:
(Bouchard’s nodes).Strongly associated with osteoarthritis elsewhere in the body (polyarticular OA).
The joints are swollen and tend to deviate ulnarwards due to mechanical pressure in daily activities.
Treatment : is usually non-operative. If the joint is very painful or unstable then surgery is considered. Fusion restores reliable, pain-free pinch in the index and middle finger PIP joints; fusion of the ring and little fingers compromises grip and so joint replacement is usually preferable.
Carpo-metacarpal joint of the thumb:
Osteoarthritis of the trapezio-metacarpal joint is common in postmenopausal women.Heberden’s nodes of the finger joints,
bilateral and part of a generalized osteoarthritis.
Infection of the hand is frequently limited to one of several well-defined compartments:
(1)under the nail-fold (paronychia);(2) the pulp space (felon)
(3) the deep fascial spaces;
(4) tendon sheaths; and joints.
Usually the cause is a staphylococcus which has been implanted during fairly trivial injury.
ACUTE INFECTIONS OF THE HAND
Pathology:
infection an acute inflammatory reaction (oedema, suppuration) increased tissue tension pressures may rise to levels where the local blood supply is threatened tissue necrosis.In neglected cases infection can spread from one compartment to another
lymphatic and haematogenous spread;
Clinical features:
history of trauma (a superficial abrasion, laceration or penetrating wound),painful and swollen.
throbbing
the patient feels ill and feverish.
finger or hand is red and swollen,
exquisitely tender over the site of tension.
With deep infections active flexion is not possible.
lymphangitis and swollen glands,
signs of septicaemia.
X-ray examination:
foreign body but isfeatures of osteomyelitis
septic arthritis,
bone necrosis
IX: If pus becomes available, this should be sent for bacteriological examination.
Differential diagnosis:
(1)an insect bite or sting (which can closely mimic a subcutaneous infection),
(2)a thorn prick (which, itself, can become secondarily infected),
(3) acute tendon rupture (which may resemble a septic tenosynovitis) and
(4)acute gout (which is easily mistaken for septic arthritis).
Principles of treatment:
AntibioticsRest, splintage and elevation
Drainage
Rehabilitation
Apley’s System of Orthopaedics and Fractures
Review of Orthopedics, MillerCampbell’s operative orthopaedics