د. زينة مكي عبد الكريمماجستير احياء مجهريةكلية طب الموصل
The Platyhelminthes (Flatworms)
1- Class trematoda – Flukes 2- Class cestoda - TapewormsIntroduction
Trematodesare parasites of vertebrates. They have complex life cycles requiring one or more intermediate hosts.
Most are hermaphroditic and capable of self-fertilization.
Eggs shed by the adult worm pass outside to the environment, and a larva (called a miracidium) .
Each species requires a certain species of mollusk (snail, clam, etc) as an intermediate host.
A series of generations occurs in the mollusk, resulting in the liberation of larvae known as cercariae.
Class Trematoda- the flukes:
1-BloodSchistosoma spp
2-Intestinal flukes:
Heterophyes heterophyes
3-Liver flukes :
Fasciola hepatica4 Lung- pulmonary flukes:
Paragonimus westermaniThe Platyhelminthes (Flatworms): Flukes
The Blood FlukesSchistosoma mansoni ___ intestinal veins
Schistosoma haematobium ____ vesical veins
Schistosoma japonicum ____ intestinal veins
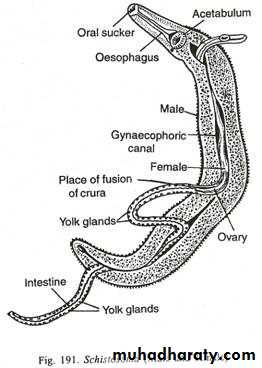
Adult morphology:
Separate male and female worms exist in this group of flukes.The female is long and narrower, the male is shorter, cylindrical and has characteristic ventral groove to form a gynecophoral canal in which the female embeded during copulation.
The intestine bifurcates into two ceca which unite in the posterior part of the body forming single blined stem.
Life Cycle
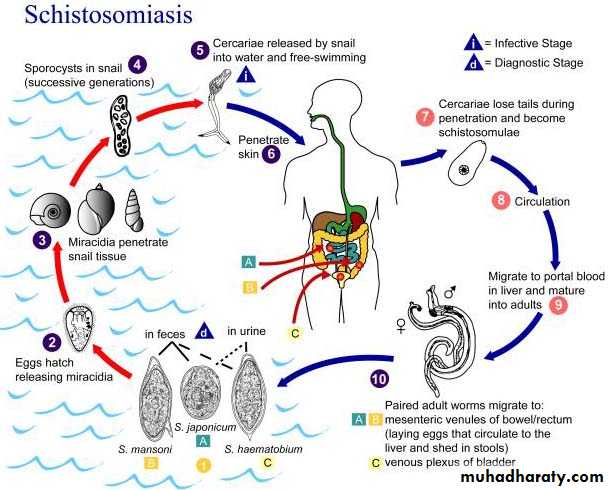
• Parasite eggs released into freshwater (from human urine, feces)• Eggs hatch ciliated miracidia, free swimming
• Miracidia find & infect snail host (different species prefer diff’t snail sp.)
• Each miracidia transforms into many fork-tailed, free swimming forms called cercariae within 4-6 weeks of entering snail.
• Cercariae leave snail and move into water at a rate of 1500/day for up to 18 days.
6. Cercariae find a human host,
penetrate skin, and differentiate intolarval forms called schistosomulae.
7. Migrate through the host’s skin,
gain access to the lymphatic system.
8. Travel to the lungs (stay 3-8 days and ~70% are eliminated)
9. Migrate to liver portal system, mature into male & female adults
Life Cycle
• 10. In liver, m & f pair up female inserts
• herself into the gynecophoral canal of male• they are now ‘paired’.
• 11. Migrate to favoured sites:
• S. mansoni – mesenteric venules of large bowel & rectum
• S. japonicum – mesenteric veins of the small intestine S. haematobium – perivesical venous plexus surrounding the bladder
Life Cycle
• 12. Females release eggs.
• 12. Eggs enter lumen of excretory organs 50% passed out of body 50% trapped in tissues, carried away by blood circulation, lymph.Life Cycle
Life Cycle
Schistosoma haematobium
Disease : Vesical schistosomiasis, urinary bilharziasisThe definitive host: man
The intermediate host: fresh water snails
Egg morphology
the eggs are large, oval , non operculated, having a terminal spine.
Cercaria
Epidemiology
Schistosomiasis is a rural disease , affects farmers mainly.Infection depends on:
1- contamination of water with human urine containing sch. Eggs.
2- presence of proper snails in the water capable of infection with meracedium and producing cercaria.
3- human contact with contaminated water.
It is highly endemic in Africa (Egypt) , and parts of Asia ( Jordan, Syria, Iraq, Iran, Yemen).
Pathology
1- Mild urticarial lesion: at the site of cercarial entry.2- Migration of immature worm to the lung produces toxic and allergic reaction that leads to peticheal hemorrhage, cough and haemoptysis.
3- Microscopical and macroscopical changes in the U. bladder takes place due to the deposition of eggs in the mucosa and submucosa:
Micro. changes include: granuloma, intense inflammatory reaction, ulceration, polyps , later fibrous tissue formation and calcification.
Macro. changes include : diffuse hyperemia, minute papular elevation of the mucosa & polypoid formation.
Later on : sloughing of the mucosa, ulceration , Ca deposits and eggs gives the mucosa a sandy or granular appearance.
With chronic condition the bladder become contracted and may predispose to malignancy (squamous cell carcinoma).
Oedema of the lower end of ureters may lead to hydronephrosis.
Symptoms
• The incubation period : 2 months to 2 years.• Irritative dermatitis at site of cercarial penetration.
• Cough & haemoptysis.
• Acute febrile illness at time of worm maturation .
• Haematuria in the terminal drops of urine.
• Painful micturition, frequency& sometimes mucus and pus are found in urine.
• Hepatomegaly & sometimes spleenomegaly.
Diagnosis
1- Urine examination: the last few drops of urine at noon-time or after exercise are either examined directly or after centrifugation & examine the sediment.2- Hatching test: add few drops of water to urine sediment and examine after few minutes to see meracidium which hatch from egg.
3- Cystoscopal examination.
4- X-ray to see calcification and U/S for hydroureter.
5- Blood test for eosinophilia.
6- Serological test for antibody detection.
7- Intradermal skin test.
Treatment
Correction of anemia.
Metrifonate 7.5 mg/kg orally every 2 weeks (3 doses).
Niridazole 25 mg/kg orally for 5 days.
Praziquantel 40 mg/kg orally single dose.
Schistosoma mansoni
Pathology and symptoms :Dermatitis at the site of cercarial penetration will develop cause pruritis and rash.
S.mansoni inhabit the mesenteric veins and their eggs invade intestinal wall to be released with stool. Some of them return back to blood stream to invade variable organs like intestine , liver and lungs.
In the intestine : congestion, cellular infiltration, polyps formation, ulcerations, fibrosis and stricture, secondary bacterial infection.
In the liver : fibrosis, cirrhosis, portal hypertension and ascitis.
In the lungs : cough and haemoptysis.
Other symptoms include: fever, weight loss, eosinophilia, abdominal pain, anemia, diarrhea, dysentery, enlarge liver and spleen.
Egg morphology
Large size, oval shape, embryonated, lateral spine.Diagnosis
1- Stool examination: direct, concentration or viability test.
2- Sigmoidoscopy and biopsy.
3- serological tests, skin test and liver Bx.
Treatment
Oxamniquine 15 mg/kg orally, 2-4 dosesNiridazole
Praziquantel
Prevention
• Diagnosis and treatment of cases.• Prevent water contamination with urine and stool.
• Snail control : remove vegetations from canals, use mulluscacides, introduction of fish or birds to remove snails.
• Avoid contact of human especially farmers with contaminated water by cercaria.
• Education of people.