1
LYMPHATIC DESEASE OF THE NECK
The body has approximately 600-800 lymph nodes.
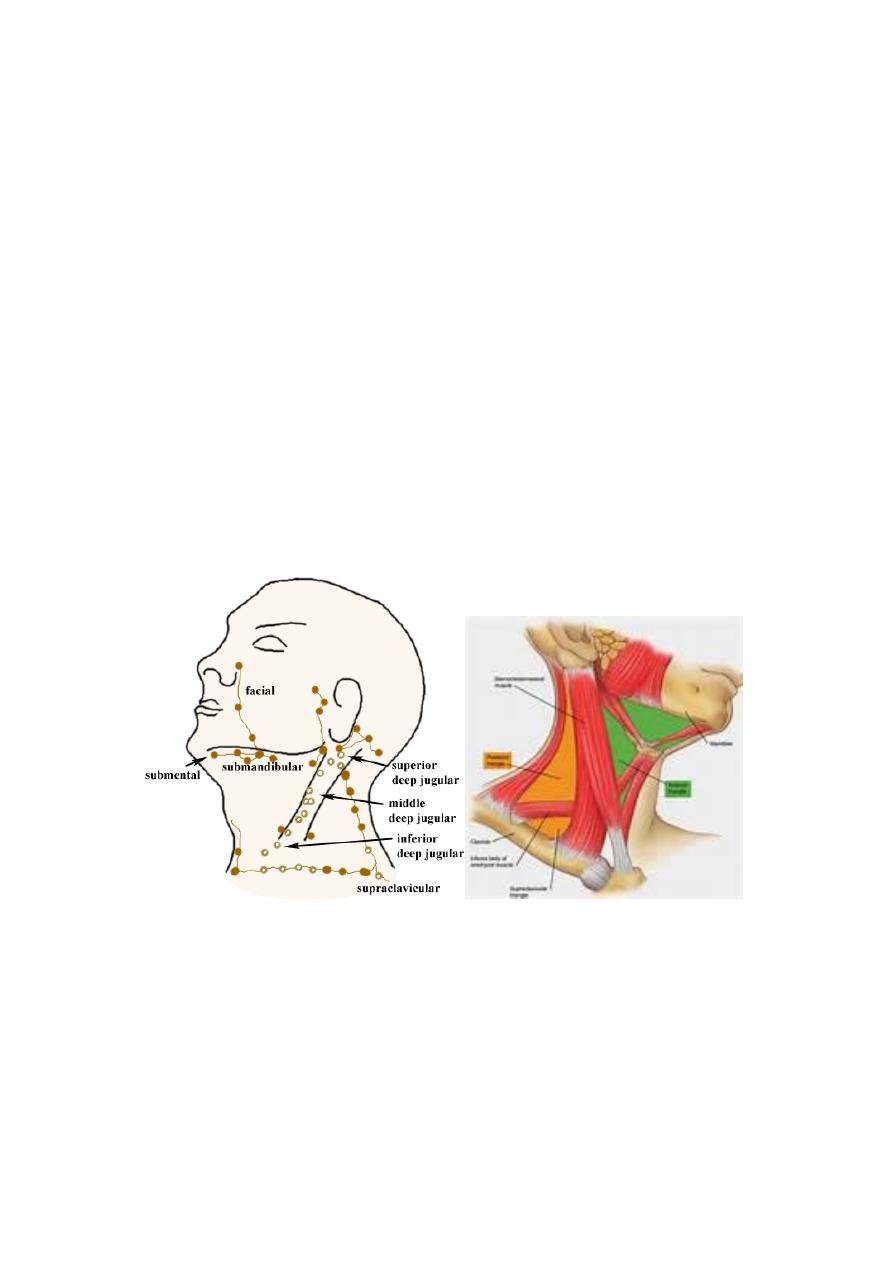
Half of the lymph nodes in the neck, they are divided into groups
according to anatomical position and to levels.
Anatomically the neck divided into 4 triangles by medline,
trapezeus, sternomastoid and digastric muscles
1- the submental
2- the submandibular
3- anterior triangle
4- posterior triangle
2
Level I— the submental and submandibular nodes
Level Ia—the submental nodes.
drain the skin of the chin, the mid-lower lip, the tip of the tongue,
and the anterior floor of the mouth.
Level Ib—the submandibular nodes. Drain the lower nasal cavity,
the hard and soft palate, the maxillary and mandibular alveolar
ridges, the cheek, the upper and lower lips, and most of the
anterior tongue.
Level II—upper jugular chain nodes drain the face, parotid gland,
and the submandibular, submental and retropharyngeal nodes,
nasal cavity, pharynx, larynx, external auditory ca-nal,
middle ear, and from sublingual and submandibular glands.
Level III—middle jugular chain nodes drain the base of the
tongue, tonsils, larynx, hypopharynx and thyroid gland.
Level IV—lower jugular chain nodes drain from the
hypopharynx, , esophagus, larynx, trachea and thyroid gland.
Level V-posterior triangle nodes drain the occipital and retro-
auricular node, parietal and occipital scalp, nasopharynx, the
oropharynx and the thyroid gland.
Level VI—anterior compartment nodes. composed of the pre-
laryngeal, pre-tracheal (delphen LN)and para-tracheal (recurrent
laryngeal nerve) nodes drain the anterior floor of mouth, the tip of
the tongue, the lower lip,, the glottic and subglottic larynx, the
hypopharynx, thyroid glandnd the cervical esophagus.
Level VII: contains the mediastinal lymph node drains esophagus
3
4
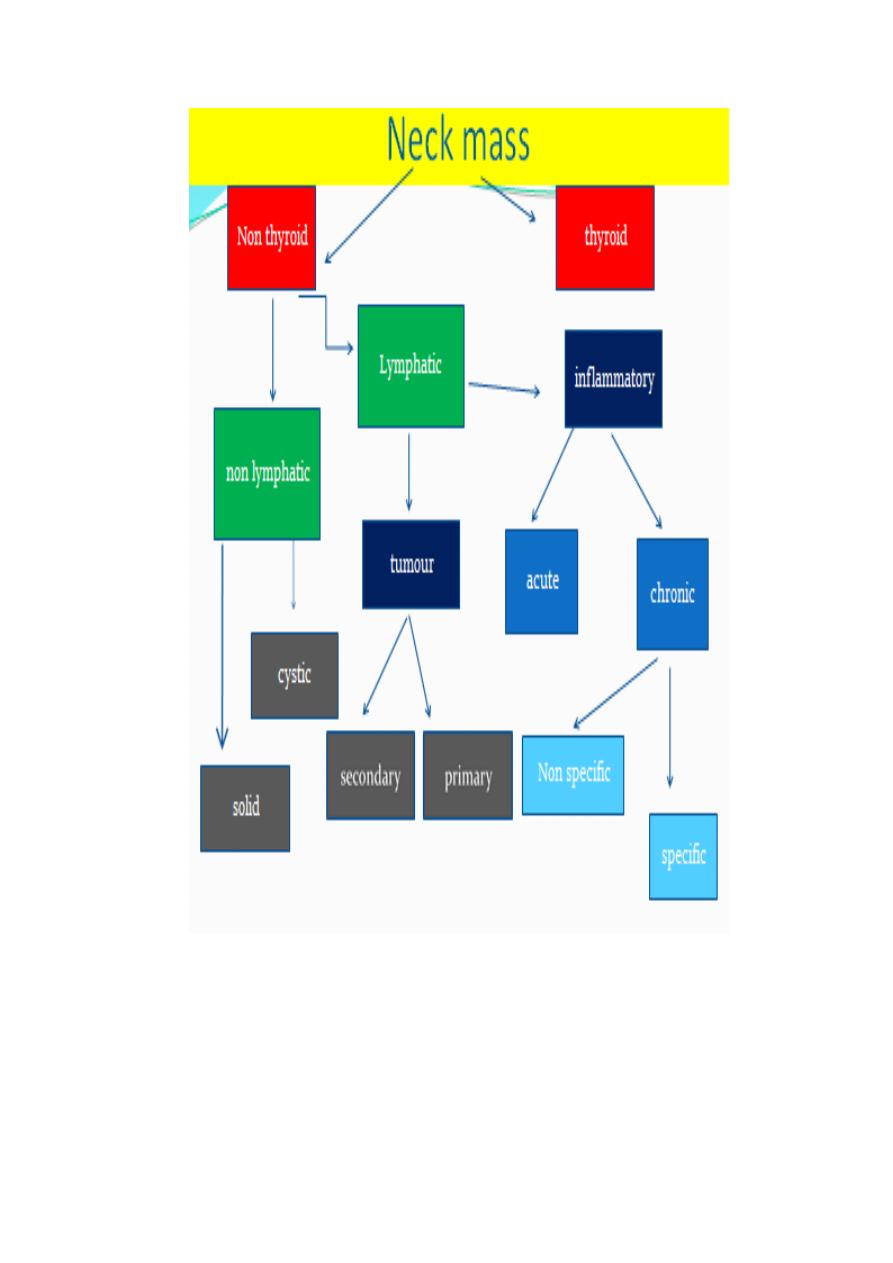
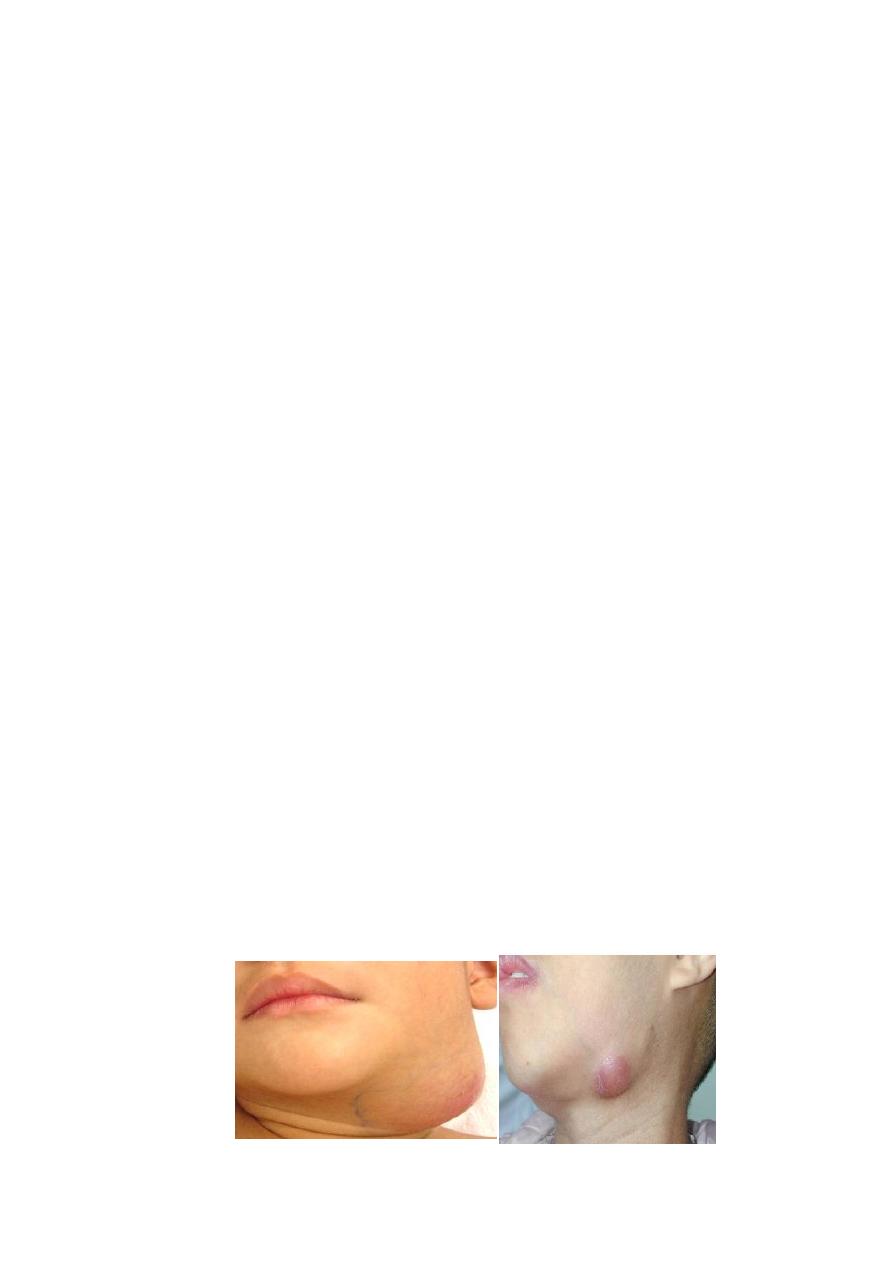
ACUTE CERVICAL LAYMPHADENITIS:
Infection is carried to LN from inflamed focus in head or neck,
face, pharynx. larynx, tonsil, ear , nose.
Mo=staph aureus, strept. Pyogens & anaerobe if dental cares.
Condition is more in children.
CLINICALLY :
Beside picture of the cause , there are LN are enlarged, unilateral, hot,
red ,tender, soft or firm& if pus formed, fluctuation +ve. There may be
tender red streaks between primary focus & affected LN (Lymphangitis).
COMPLICATIONS:
Spread to more proximal LN.
Spread to nearby tissue
Suppuration (Abscess)
MO remains dormant in LN & flare up later.
TRAETMENT:
Treat causative agent.
Rest & AB
local heat & review in 48 hours.
Incision & drainage if no response or fluctuation
formed.

5
CHRONIC NON SPECIFIC LYMPHADENITS
. ETIOLOGY
1. It is due to chronic infection of nearby focus like septic teeth,
sinusitis, tonsillitis or adenoiditis.
2. Chronic non specific lymphadenitis of post. triangle in children
may be due to head pediculosis or rubella.
3. Chronic non specific lymphadenitis following incomplete
resolution of acute lymphadenitis.
CLINICALLY
The LN are slightly enlarged, mobile, mildly tender & firm or elastic in
consistency.
TREATMENT:
Treatment of original focus
Nodes need no treatment.
Chronic non specific lymphadenitis that persists for more than
3-4 months ;TB or lymphomas must be excluded.
6
TUBERCULOUS LYMPHADENITIS (Scrofula or kings Evil)
It is common in children or young adults.
Commonest LN are JUGULODIGASTRIC. (level 2)
The MO reaches them from adenoids & tonsils from infected
milk.
Both human and bovine type of TB MO can be responsible..
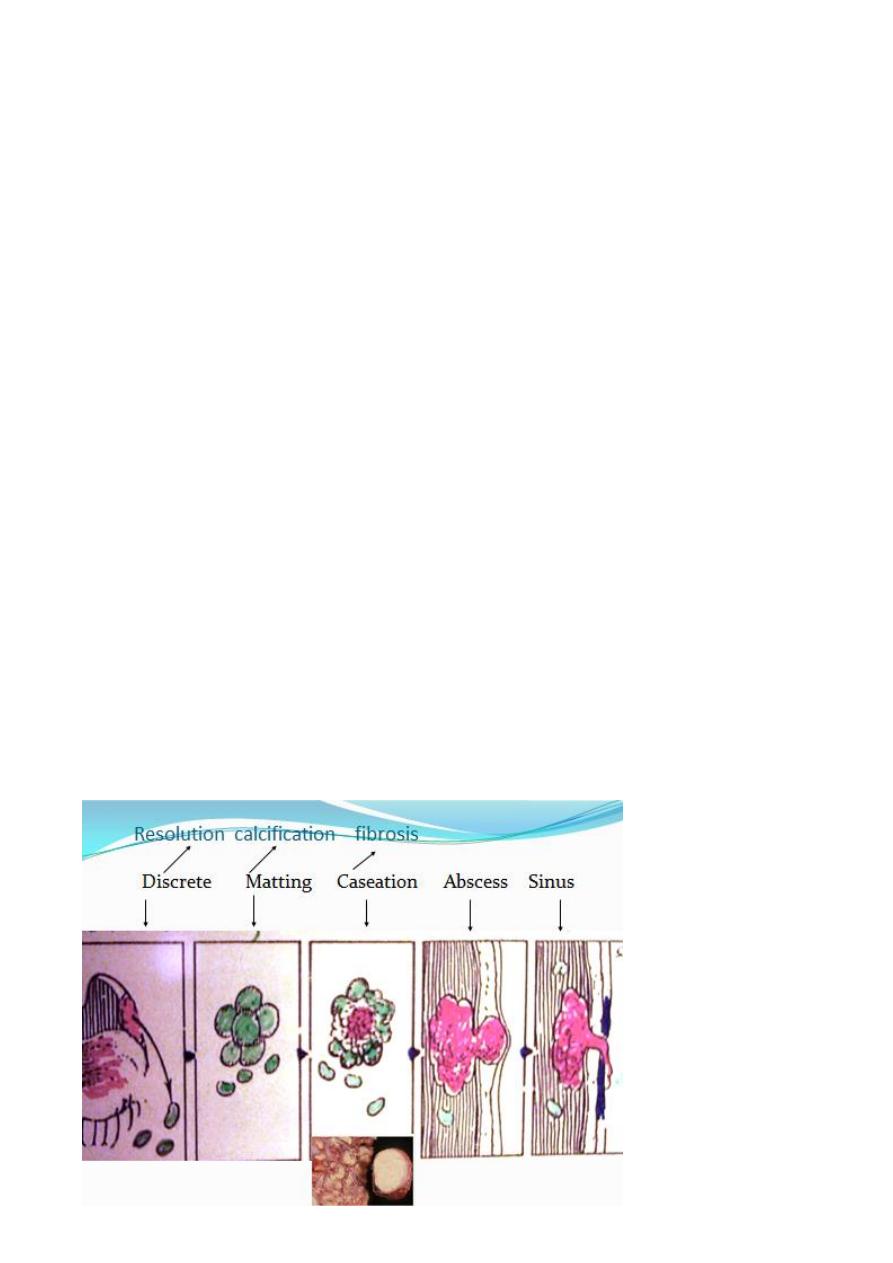
Pathology: The consequence of events are as follows:
1- TB lymphadenitis.
2-TB periadenitis involvement of the capsule presented as matted LN.
3-Multiple tubercles will form, coalesce, break down to form cold
abscess.
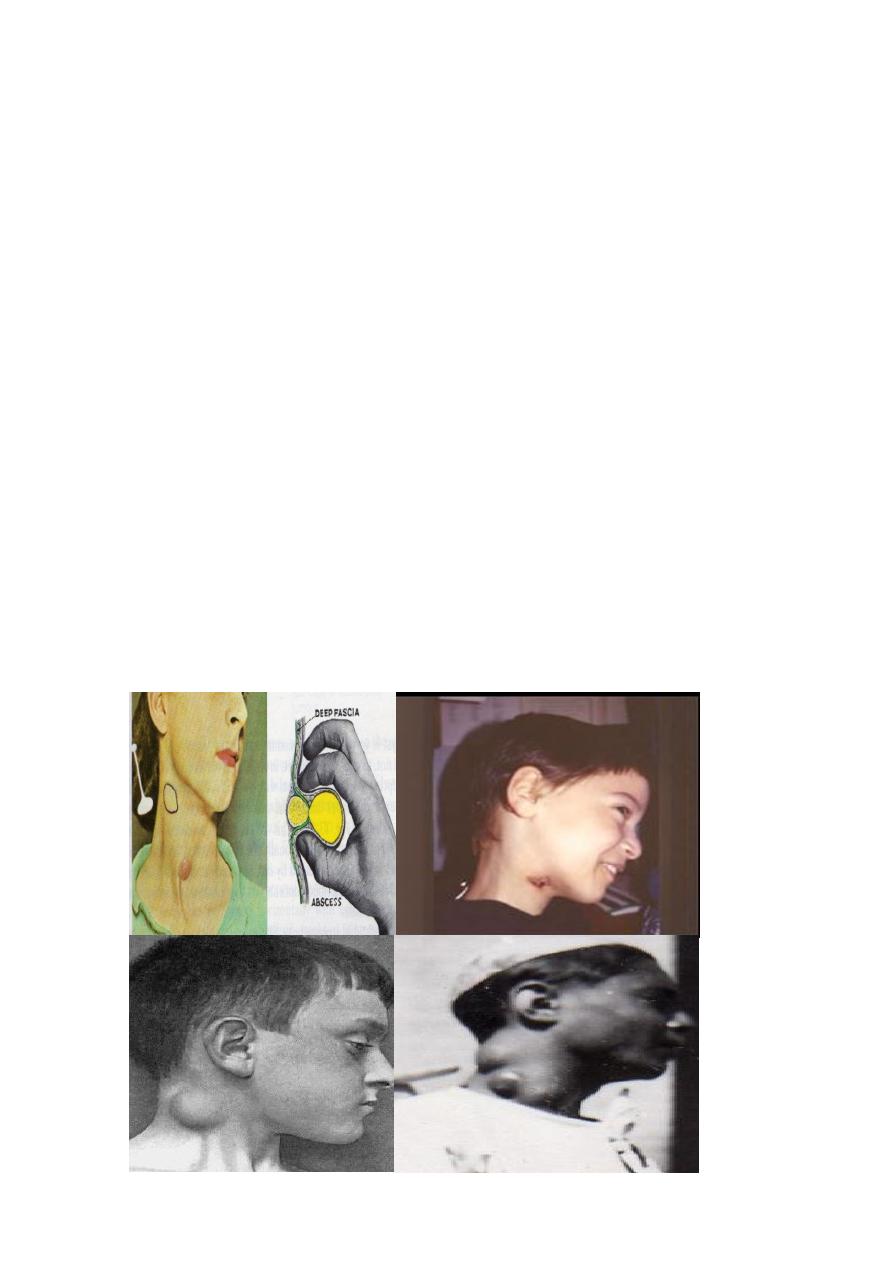
4-Burst through the deep fascia into subcutaneous space producing
collar stud abscess.
5- Rupture through skin producing TB sinus or ulcer.
6-At any stage ? resolution or calcification or fibrosis may happened.
7
CLINICALLY
:
General features : fever, night sweat, anorexia & weight loss
The disease is unilateral in 80% and limited to single group in
80%,
may associated with pulmonary or renal TB in 20%.
Stage of lymph adenitis:
LN enlarged non tender not warm ,firm or elastic & matted to
each other.
The cold abscess, it is slightly warm not tender, connected to
underlying caseating LN.
Fluctuation occur when the abscess burst to the superficial
fascia to form collar stud abscess.
Sinus formation with thin blue margin, undermined edges &
thin serous discharge. Healing of sinuses leaves scar.
8
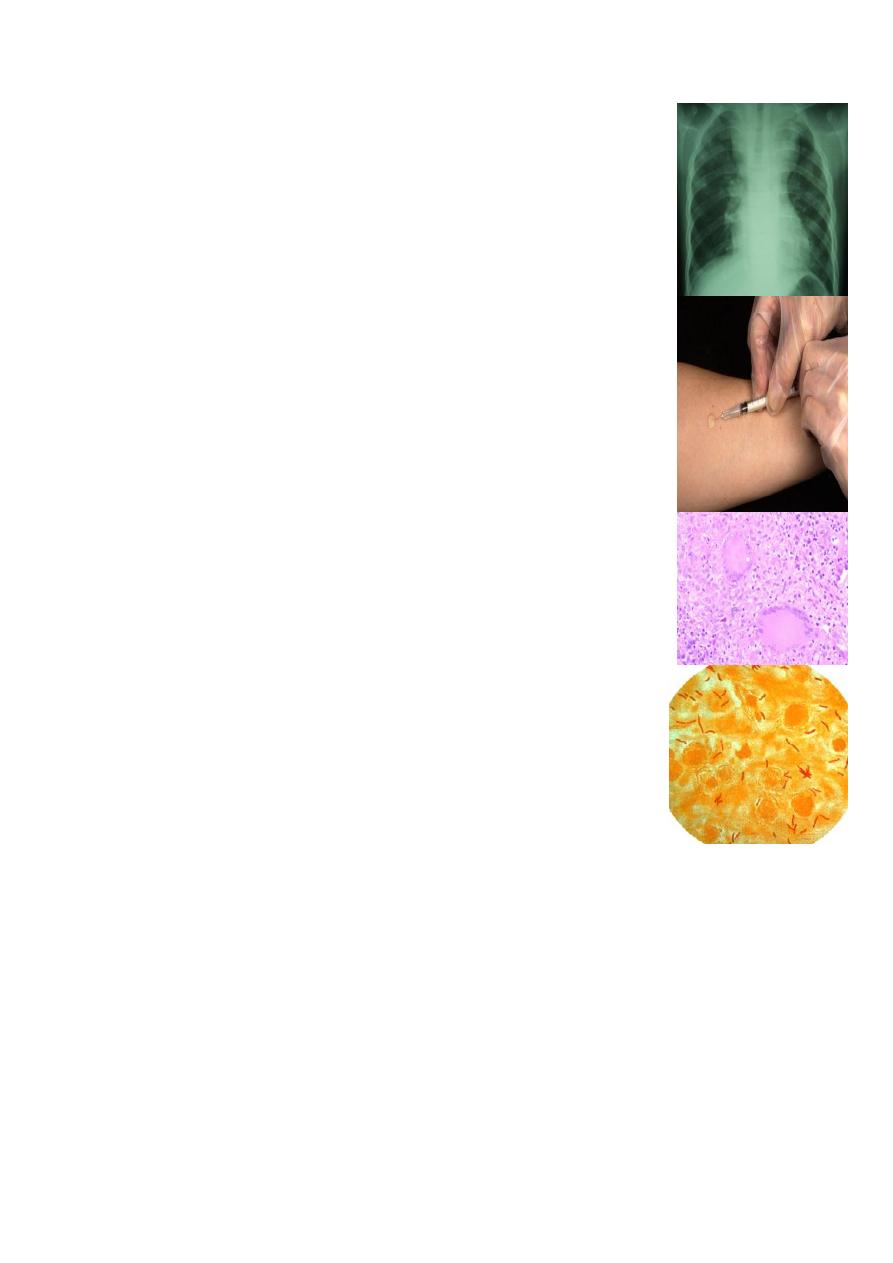
INVESTIGATIONS:
1.CXR, CBP & E.S.R, lymhocytosis
2.Tuberculine -ve.
3.LN biopsy ( T.B Granuloma).
4.Aspiration of cold abscess & guinea pig inoculation
5.Smears of sinus for AFB.
TREATMENT:
IN stage of lymphadenitis :
Improve general condition
Anti TB( 9 months)
Surgical excision of single or group of LN if no
response or complications.
IN cold abscess and sinus:
Anti TB
Drainage.
Excision of underlying LN

9
Tumour of lymphatic system in the neck
80% of tumour in the neck LN are secondary mostly from
A- primary in head and neck (85%)
1- oral cavity
2- nasopharynx
3- oropharynx
4-hypopharynx
5- thyroid
B- primary below the clavicle (15%)
1- bronchus
2- esophagus, stomach, colon, pancreas.
3- testes, prostate.
The presence of cervical metastasis decreases the 5-year survival rate in
patients by approximately 50%.
Primary neck LN malignancy represent 20% of malignant tumour mostly
in form of Lymphomas.
Usually involve children & young adults.& More common in male.

11
Clinically
:
Painless progressive enlargement of discrete rubbery LN, may
associated with hepato/Splenomegaly with or without constitutional
symptom.
Character of LN involved by secondary malignant deposit are
rapidly enlarged, hard, irregular shape, fixed, painless and
subsequent ulceration to skin.
The primary should always searched and managed accordingly.
Biopsy or fine needle aspiration are needed for confirmation of
diagnosis.
Image study needed for diagnosis of the primary
Treatment
The gold standard treatment for control of cervical metastasis is
radical neck dissection (RND) with en-block removal of the
primary tumour if feasible
The classic RND removes levels I to VI of the cervical lymphatics
in addition to the sternomastoid muscle, internal jugular vein,
the spinal accessory nerve (CN XI) and submandibular salivary
gland.
Many incisions has been used
11
The aim is to fulfill
1-Adequate exposure.
2-Capible for extension.
3- Cosmetically acceptable
4- Not damage vital structure under the skin
5- Avoid middle portion of the neck
Any modification of the RND that preserves nonlymphatic structures
(i.e., CN XI, SCM muscle, or internal jugular vein) is defined as a modified
radical neck dissection (MRND).
A neck dissection that preserves lymphatic compartments normally
removed as part of a classic RND is termed a selective neck dissection
lateral2/3/4 posterolateral 2/3/4/5 or supraomohyoid level1 (SND).
Radiotherapy
1-Can be used initially like in nasopharyngeal ca.
2- Recurrent nodal disease.
3- Residual tumour
Complication of RND
A- Early:
1- Bleeding
2-Pneumothorax
3- Increase intracranial pressure due to
ligation of IJV.
4-Chylus fistula due to injury to thoracic duct.
5- Carotid artery rapture.
B-Late:
1- Scarformation
and disfiguring
2-
Frozenshoulder
3- Recurrence of
tumour

12
