
Respiratory
Dr. Mohi
“ Wheezing in infants ”
Total Lec: 33

1
Wheezing in infants
• A wheeze is a musical and continuous sound that originates from
oscillations in narrowed airways.
• Wheezing is heard mostly on expiration as a result of critical
airway obstruction.
Acute bronchiolitis
•
Predominantly a viral disease. Respiratory syncytial virus (RSV) is
responsible for >50% of cases .Other agents include
parainfluenza, adenovirus,
Mycoplasma,
and, occasionally, other
viruses.
•
Acute bronchiolitis is characterized by bronchiolar obstruction
with edema, mucus, and cellular debris.
CLINICAL MANIFESTATIONS
•
The infant 1st develops a mild upper respiratory tract infection
with sneezing and clear rhinorrhea.
•
fever of 38.5–39°C
•
Gradually, respiratory distress ensues, with paroxysmal wheezy
cough, dyspnea, and irritability.
PHYSICAL EXAMINATION
•
Wheezing.
•
The degree of tachypnea does not always correlate with the
degree of hypoxemia or hypercarbia
•
Nasal flaring and retractions.
•
Fine crackles or overt wheezes, with prolongation of the
expiratory phase.
•
Hyperinflation of the lungs may permit palpation of the liver and
spleen.
2
DIAGNOSIS
•
The diagnosis is clinical, particularly in a previously healthy
infant presenting with a first-time wheezing episode during a
community outbreak.
•
Chest radiography reveals hyperinflated lungs with patchy
atelectasis.
•
The white blood cell and differential counts are usually normal.
•
Viral testing
TREATMENT
•
Infants with acute bronchiolitis who are experiencing respiratory
distress should be hospitalized.
•
Mainstay of treatment is supportive.
•
If hypoxemic, the child should receive cool humidified oxygen.
•
The infant may be fed through a nasogastric tube.
•
Frequent suctioning of nasal and oral secretions often provides
relief of distress or cyanosis.
•
A trial dose of inhaled bronchodilator may be reasonable, with
further therapy predicated on response in the individual patient.
•
Corticosteroids are not recommended in previously healthy
infants with RSV
•
Ribavirin, an antiviral agent administered by aerosol, has been
used for infants with congenital heart disease or chronic lung
disease.
•
Antibiotics have no value unless there is secondary bacterial
pneumonia.
•
No support for RSV immunoglobulin administration during acute
episodes of RSV bronchiolitis.
3
PROGNOSIS
•
The case fatality rate is <1%, with death attributable to apnea,
uncompensated respiratory acidosis, or severe dehydration.
•
Infants with conditions such as congenital heart disease,
bronchopulmonary dysplasia, and immunodeficiency often have
more severe disease, with higher morbidity and mortality.
•
There is a higher incidence of wheezing and asthma in children
with a history of bronchiolitis unexplained by family history or
other atopic syndromes.
PREVENTION
•
Pooled hyper immune RSV intravenous immunoglobulin (RSV-
IVIG) and palivizumab, an intramuscular monoclonal antibody to
the RSV F protein, before and during RSV season.
•
Palivizumab is recommended for infants <2 yr of age with chronic
lung disease (bronchopulmonary dysplasia) or prematurity.
•
Meticulous handwashing is the best measure to prevent
nosocomial transmission.
Wheezing associated conditions
•
Bronchial asthma
•
Cystic fibrosis
•
Congenital malformations
(Rings and slings )
•
Foreign body aspiration
•
Gastro esophageal reflux
•
Trauma and tumors
Bronchial asthma
•
Asthma is characterized by airway inflammation, bronchial
hyperreactivity, and reversibility of obstruction.
•
Of all the infants who wheezed before 3 yr old, almost 60%
stopped wheezing by 6 yr.
4
•
Risk factors for persistent wheezing included maternal asthma,
maternal smoking, allergic rhinitis, and eczema at <1 yr of age.
Cystic fibrosis
•
Persistent respiratory symptoms, digital clubbing, malabsorption,
failure to thrive, electrolyte abnormalities, or a resistance to
bronchodilator treatment.
Congenital malformations
•
External vascular compression
includes a vascular ring, or a
vascular sling
•
Cardiovascular causes
of wheezing include dilated chambers of
the heart, and pulmonary edema.
Foreign body aspiration
•
78% of those who die from foreign body aspiration are between 2
mo and 4 yr old.
•
Atypical histories or misleading clinical and radiologic findings
may be misdiagnosed with asthma or another obstructive
disorder as inflammation and granulation develop around the
foreign body.
Gastroesophageal reflux
•
Can cause wheezing with or without direct aspiration into the
tracheobronchial tree.
•
Without aspiration, the reflux is thought to trigger a vagal or
neural reflex, causing increased airway resistance and airway
reactivity
5
Trauma and tumors
•
Accidental or nonaccidental aspirations, burns, or scalds of the
tracheobronchial tree can cause inflammation of the airways and
subsequent wheezing.
•
Any space-occupying lesion either in the lung itself or extrinsic to
the lung can cause tracheobronchial compression and
obstruction.
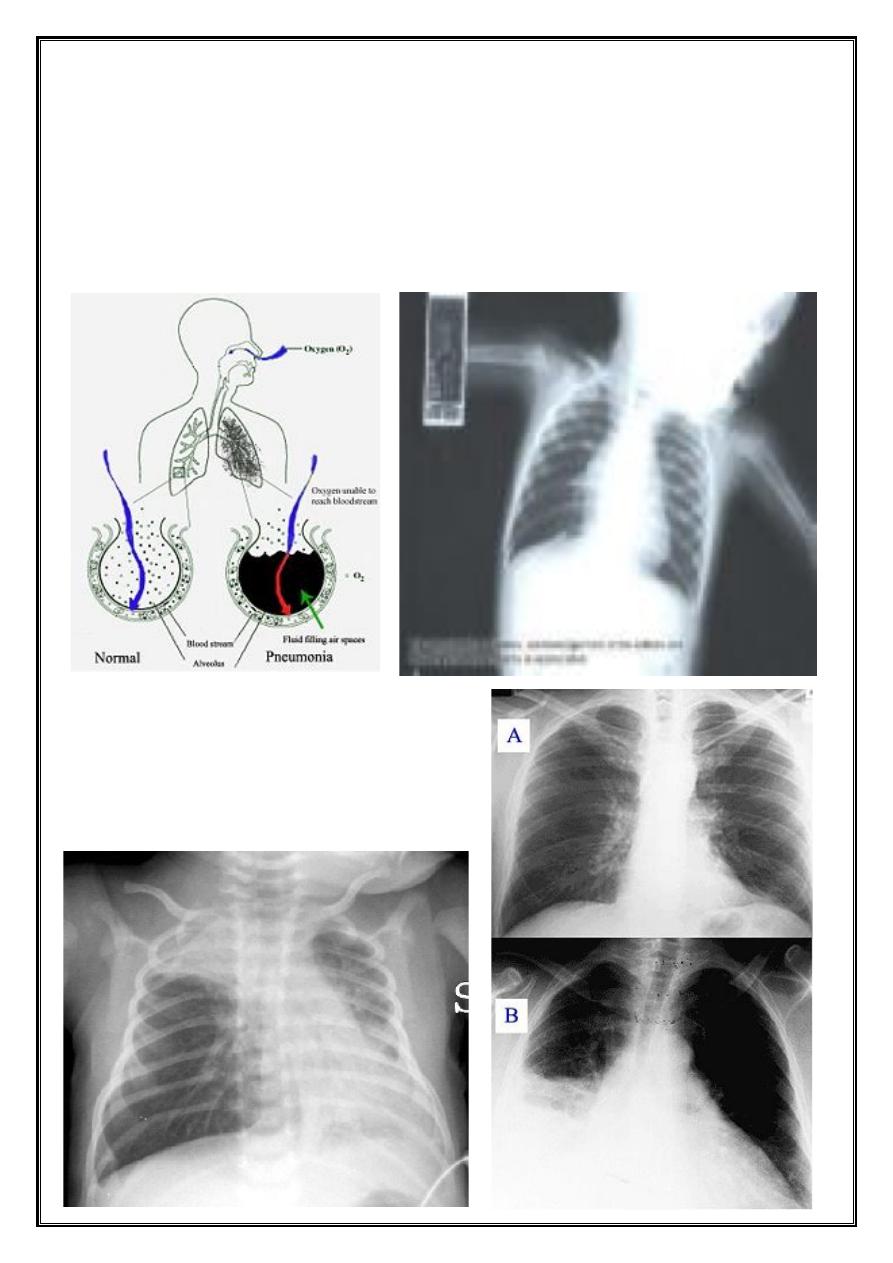
PNEUMONIA
•
Community-acquired pneumonia
(CAP): acute infection of the
pulmonary parenchyma in a patient who has acquired the
infection in the community, as distinguished from….
•
Hospital-acquired pneumonia (
nosocomial
).
Viral pneumonia
•
Most children younger than 5 years of age who are admitted to
the hospital with pneumonia have viral pneumonia.
•
Viral pneumonia does not require antibiotic therapy, unless a
mixed infection or secondary bacterial infection is suspected.
Typical bacterial pneumonia
• Typical bacterial pneumonia may occur in children in all ages.
• Streptococcus pneumonia is the most common type of bacterial
cause of pneumonia in children of all ages.
• S. aureus.
• Strept. Pyogenes.
• H. influenza type b, nontypeable H. influenzae, and M catarralis.
• Antibiotic regimens include:
o Amoxicillin, ceftriaxone and cefotaxime.
Atypical bacterial pneumonia
•
(M. pneumoniae and Chlamydia pneumoniae) is most common in
children older than 5 years.
6
•
Antibiotic include:
•
Erythromycin or Azithromycin
•
For children older than 8 years: Doxycycline
Nosocomial pneumonia
•
S. aureus, Enterobacteriaceae, Pseudomonas aeruginosa, and
anaerobes.
•
Acceptable broad-spectrum empiric regimens include an
aminoglycoside plus:
•
Piperacillin-tazobactam or Meropenem.
•
clindamycin plus an aminoglycosides
Aspiration pneumonia
•
Appropriate antibiotics regimens for hospitalized children
include:
•
Clindamycin or Meropenem
•
Immunocompromised host: vancomycin if methicillin-resistant
staphylococcus is considered.
•
And possibly trimethoprim-sulfamethoxazole for Pneumocystis
jirovecii.
DURATION OF TREATMENT
•
Uncomplicated cases :
•
7-10 days or at least one week beyond resolution of fever.
•
Complicated cases (necrotizing pneumonia and lung abscess) :
•
Four weeks or two weeks after the patient is afebrile and has
improved clinically.
7
PROGNOSIS
•
Most otherwise healthy children with pneumonia recover
without sequelae, even if the pneumonia is complicated.
v
All that wheeze is not asthma, but when recurs …
it is!
Acute Bronchiolitis
Pneumonia




