Dr. Athal Humo pediatricDIABETIC KETO ACIDOSIS
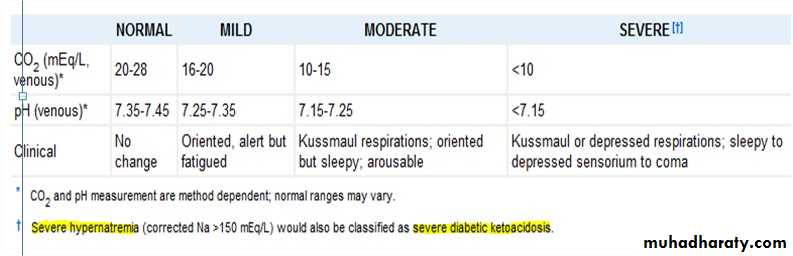
DKA occur in the following conditions:1. 20-40% of children with new onset diabetes.2. Omitted insulin doses.3. Unsuccessful management of an intercurrent illness.CLASSIFICATIONAccording to the severity, DKA can be classified into mild, moderate & severe DKA.
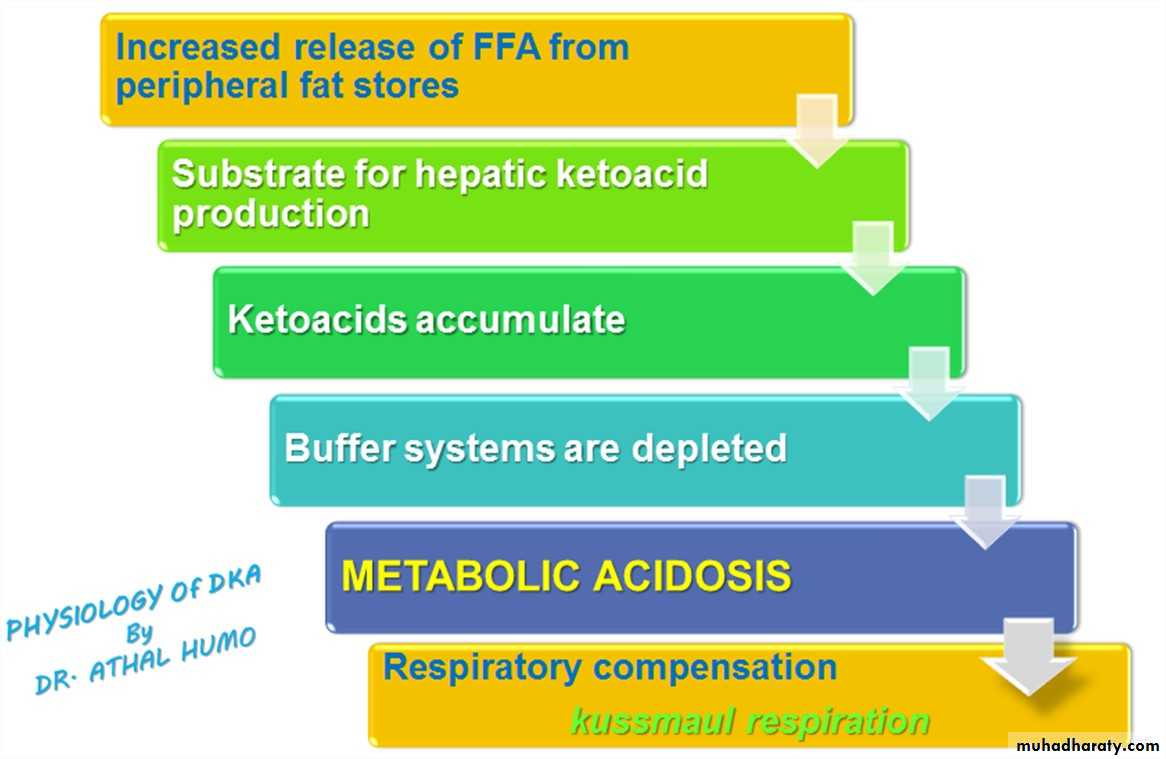
PHYSIOLOGY OF DKA
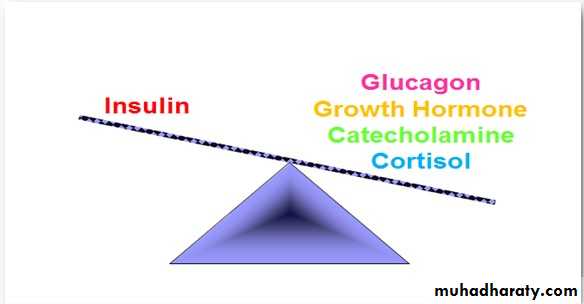
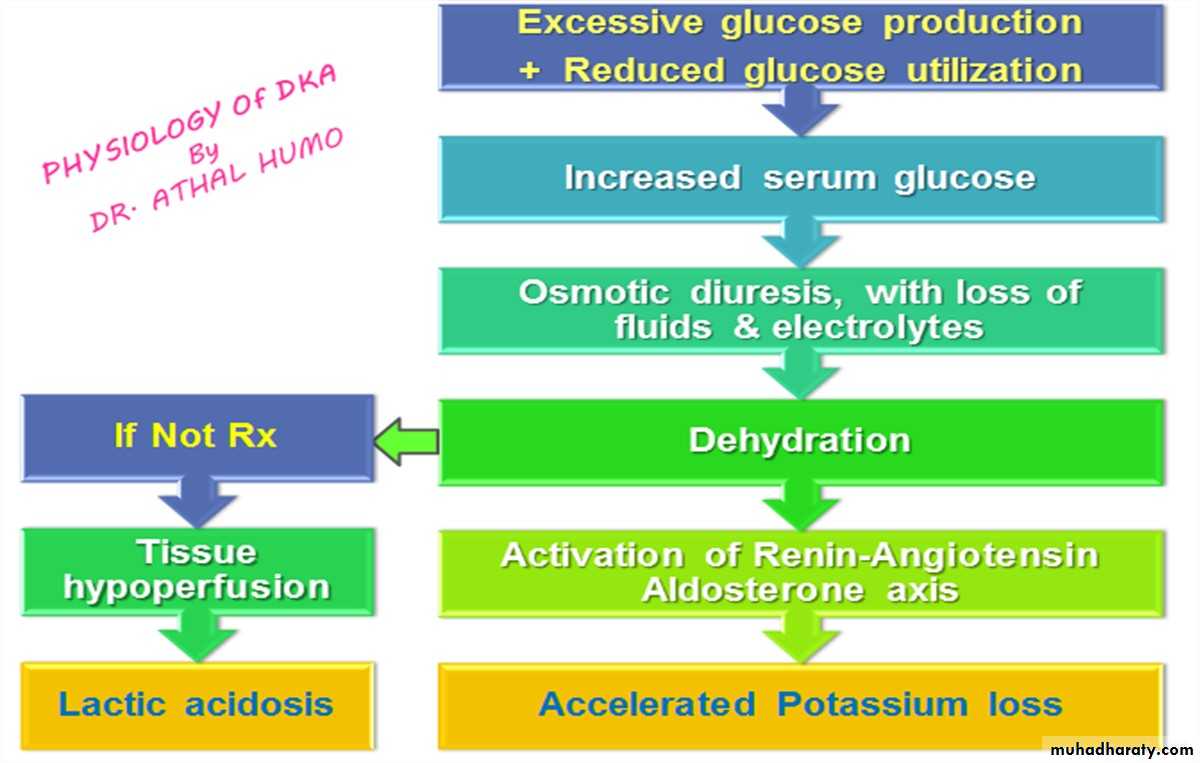
PHYSIOLOGY OF DKA Diabetic ketoacidosis is a superfasted state in which the body’stissues are robbed of their normal energy substrate Glucose. And the body resorts to catabolism of glycogen, protein and fat forenergy.• Glycogen is broken down to form glucose (glycogenolysis)• Protein is catabolized to amino acids which are converted to glucose(gluconeogenesis)• Fats are broken down to free fatty acids, which are converted in theliver to glucose or ketoacids (ketogenesis)
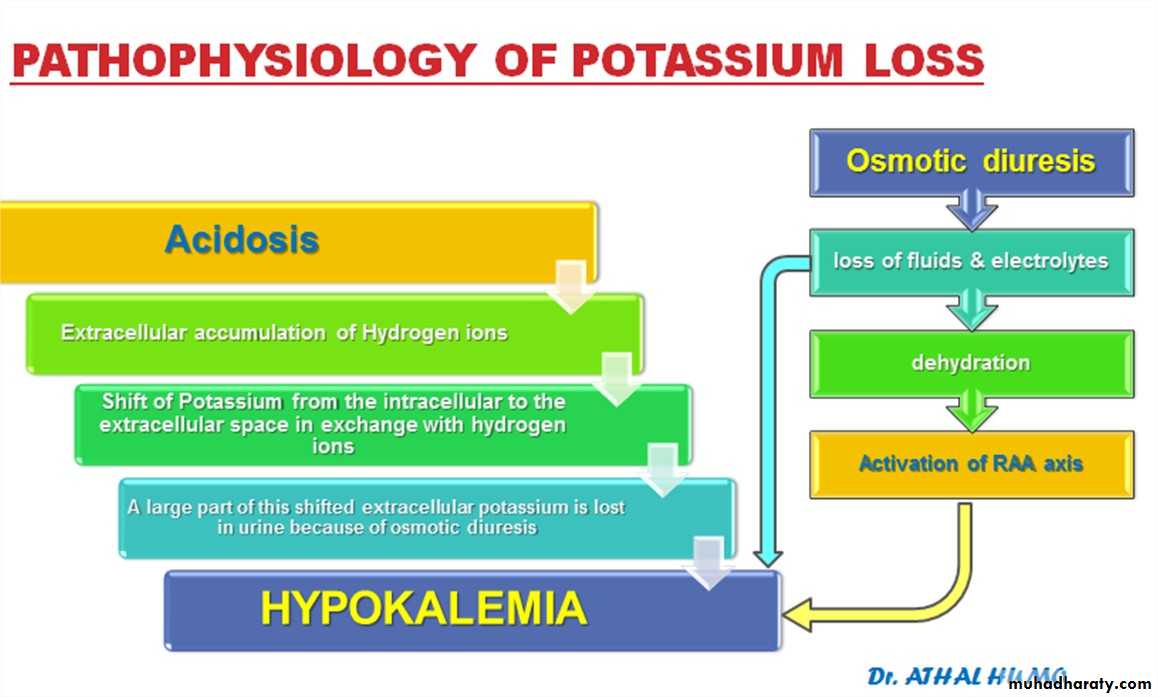
POTASSIUM The most characteristic disturbance in electrolytes is total body potassium loss. K+ is largely an intracellular ion. Both lack of insulin (catabolic predominance) and acidosis cause a shift of K+extracellularly. High urinary losses of K+ occur due to: compartmental shift. osmotic diuresis. kaliuretic effect of hyperaldosteronism. This loss is not mirrored in serum potassium levels, which may be low, withinthe normal range, or even high. Serum K+ levels are usually normal, even when total body K+ is depleted,because: The compartmental shift of K+ from inside to outside the cell Only extracellular K+ is measured
SODIUM Initial serum sodium may be ‘low’ for several reasons:Depletion secondary to urinary losses / vomitingHyperlipidemia displaces sodium in the most frequentlyused laboratory assay, factitiously lowering sodium values.Hyperglycemia High serum osmolarilty Water drivenfrom Intra to Extracellular space Dilutional hyponatremia↑Glucose ↓Sodium For each 100mg% increase of serum glucose above 100mg%, thereis an expected decrease of about 1.6mEq/L in measured sodium. The ‘true’ serum sodium level can be calculated as:
[Na] + Glucose-100 x 1.6
100
[Na] + Glucose-100 x 1.6
100
The sodium should increase by about 1.6 mmol/L for each 100mg/dLdecline in glucose. If the corrected value is >150 mmol/L, severe hypernatremicdehydration may be present and may require slower fluid replacement. Declining sodium may indicate excessive water accumulation & risk ofcerebral edema. Electrolytes losses continue for several hours during therapyuntil catabolic state is reversed & diuresis is controlled. Even though Sodium deficit may be repaired within 24 hours,intracellular Potassium & Phosphate may not be completelyrestored for several days. The combined effects of serum hyperosmolarity, dehydration,and acidosis; result in increased osmolarity in brain cellsclinically manifests as an altered consciousness.PRESENTATION The acidosis and ketosis of DKA creates an ileus (in particular betahydroxybutyrate), causing patients to develop nausea and vomiting, thatconsequently aggravate fluid and electrolyte loss already existing inDKA. Occasionally the ileus will produce pain severe enough to raiseconcern for an acute abdomen. The ketosis (Acetone ) can give patients a fruity breath. As the DKA becomes more severe, the patients will develope lethargythat can progress to coma.
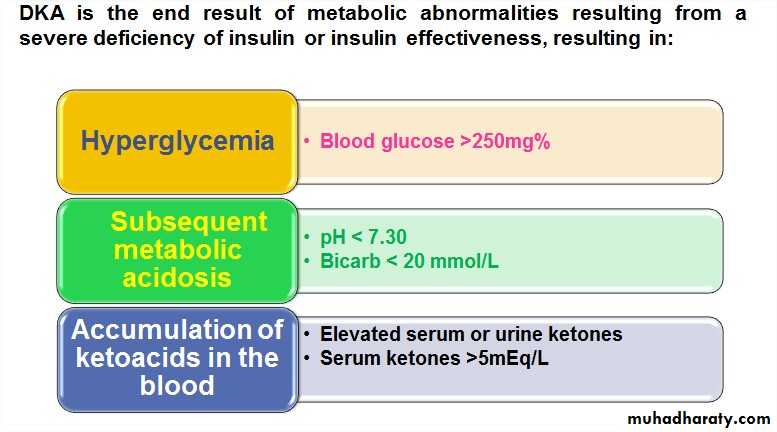
LAB ABNORMALITIES AND DIAGNOSIS Serum glucose is elevated >250mg/dL Serum bicarbonate <20 mmol/L Arterial pH <7.3, depending on the severity of the acidosis. Elevated serum osmolarity Urine analysis: Glucosuria + Ketones Blood Urea Nitrogen (BUN) may be elevated due to dehydration. Complete Blood Counts: may reveal possible infectious etiology.
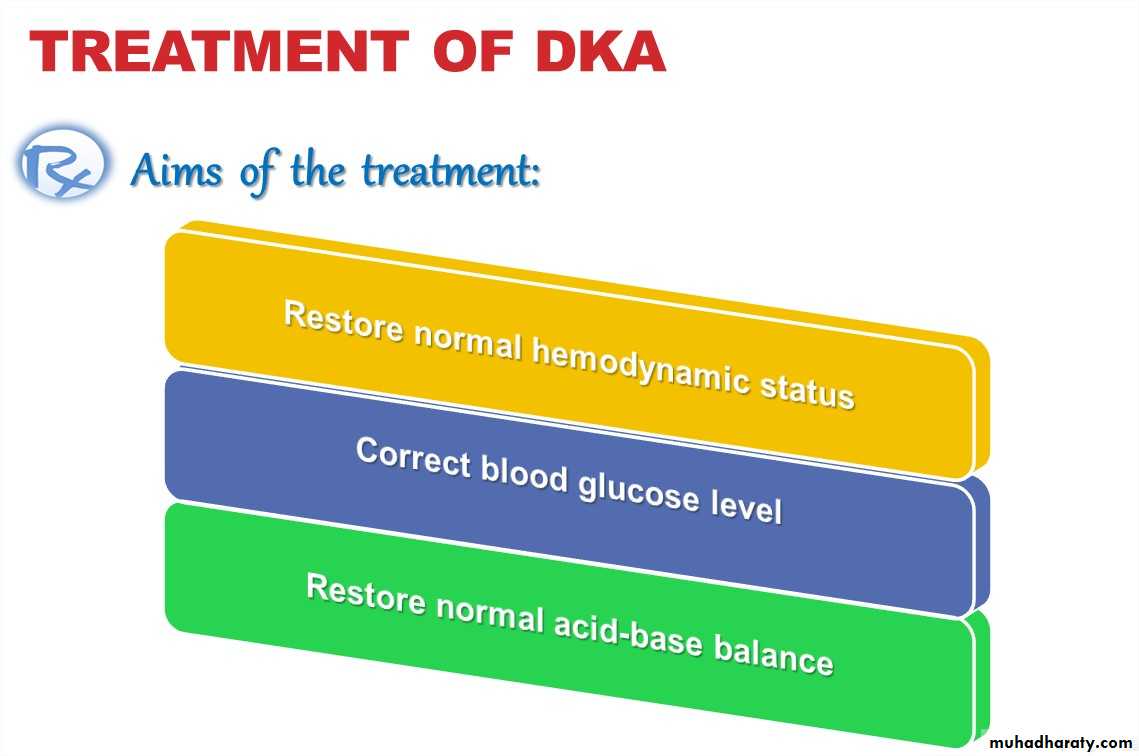
Restore perfusion by giving fluids, which will increase glucose usein the periphery, restore GFR, and reverse the progressive acidosis. Stop ketogenesis by giving insulin, which will reverse proteolysisand lipolysis, and stimulate glucose uptake and processing,normalize blood glucose, and reverse acidosis. Correct electrolyte losses by electrolyte supplementation. Avoid the complications of treatment, including intracerebralcomplications, hypoglycemia, and hypokalemia.
IV rate = 85ml/kg + maintenance – bolus
23 hr
IV rate = 85ml/kg + maintenance – bolus
23 hr
I. CORRECTION OF DEHYDRATION: It is prudent to approach any child in any hyperosmotic state withcautious rehydration due to the risk of cerebral edema. Therefore, patients should not be allowed oral fluids untilrehydration is well progressed and significant electrolyte shifts areno longer likely. All fluid intake and output should beclosely monitored. Calculation of fluid deficits using clinical signs isdifficult in children with DKA because intravascular volume isbetter maintained in the hypertonic state. The fluid deficit considered to be 8.5% of body weight.Deficit= (8.5/100)x Body weight x 1000= 85ml/kg Maintenance (24 hr) = 100 mL/kg (for the 1st 10 kg) + 50 mL/kg (for the 2nd10 kg) + 25 mL/kg (for all remaining kg) This protocol corrects a deficit of 85ml/kg (8.5% dehydration) for allpatients in the first 24 hours. Children with mild DKA rehydrate earlier & can be switched to oral intake,whereas those with severe DKA and a greater volume deficit require 30-36hours with this protocol. The rehydration start by giving a bolus of 20ml/kg of normal saline or ringerlactate over a short time (20min-1hr) & can be repeated . This ensures quickvolume expansion. Subsequent fluid is hypotonic (like glucose saline ) to repair the free waterdeficit, to allow intracellular rehydration. Usually to start with it when bloodglucose reaches 250mg/dl or less.
SODIUM The corrected sodium is usually normal or slightly elevated andindicates moderate hypernatremic dehydration. If the corrected value is > 150 mmol/L, severe hypernatremicdehydration may be present and may require slower fluidreplacement. The sodium should steadily increase with therapy. Decliningsodium may indicate excessive free water accumulation andthe risk of cerebral edemaPOTASSIUM Therefore, unless the patient is hyperkalemic or anuric, potassium isadded to the intravenous fluids at the beginning of the second hour oftherapy; otherwise it is added as soon as urine output is established orthe hyperkalemia abates. If the patient presents with hypokalemia, potassium replacement shouldbe initiated immediately. During treatment of DKA, the insulin that isgiven, as well as correction of the acidosis thatoccurs, both cause potassium to moveintracellularly. Because of this hypokalemia is apotentially fatal complication duringtreatment of DKA. Most patients will require 40 mEq/L of potassium in thereplacement fluids (given as 20 mEq/L Kphos & 20 mEq/L Kac) If K <3 mEq/L, give: 0.5 to 1.0 mEq/kg as oral K solution OR increase IV K to 80 mEq/L, adjusted based on serumpotassium levels measured every 1 to 2 hours. If patient tolerate oral feeding potassium can given orally.PHOSPHATE Clinical studies have not shown benefit from phosphatereplacement during the treatment of DKA. Although phosphate replacement should be given if thelevel drops less than 1 mg/dL. In the absence of severe hypophosphatemia,phosphate may be provided by giving half of thepotassium replacement as potassium phosphate.II. CORRECTION OF HYPERGLYCEMIA: Insulin treatment is begun at the beginning of the secondhour of therapy, with regular monitoring of blood glucoselevel. It is given as a continuous intravenous infusion of regularinsulin at a rate of 0.1 U/kg/h. Short or rapid acting insulin injected intramuscularlyevery 2 hours can be used. Once insulin is infused at appropriate rates, ketoacid production stops,the bicarbonate buffers are regenerated leading to correction of acidosiswithout the need for sodium bicarbonate adminstration. Urine testing for ketone bodies is not reliable because correction ofacidosis leads to conversion of betahydroxybutyric acid to acetoaceticacid which gives a positive result on such test. Hyperglycemia is corrected well before the correction of acidosis.Therefore, even after normal glucose levels are reached, insulin is stillrequired to control fatty acid release. The dose of insulin should remain at 0.1U/kg/h until the acidosis resolves(pH >7.3, bicarbonate > 18).III. CORRECTION OF ACIDOSIS: Clinical trials have failed to show any benefit of bicarbonate useduring the treatment of DKA. Potential risks of bicarbonate therapyinclude paradoxical CNS acidosis and exacerbation of hypokalemia.Bicarbonate treatment has also been associated with cerebral edema,the most common cause of mortality for children with DKA. Therefore, bicarbonate treatment should only be considered in casesof extreme acidosis, such as: Those with pH less than 6.9 When the acidosis may impair cardiovascular stability. As treatment of life-threatening hyperkalemia. If bicarbonate is felt to be necessary, 1 to 2 mmol/kg (added to 0.45%saline) should be given over 1 to 2 hours.MONITORING Vital signs and mental status are monitored frequently, at least every hour.If the patient is markedly obtunded, NGT should be placed to decrease therisk of aspiration. The balance of total fluid intake and fluid output should also be calculatedeach hour. Serum glucose and pH should be measured hourly. Serum electrolytes and urine ketones measured every 2 to 3 hours. The goal for correction of hyperglycemia is a fall of 100 mg/dLper hour. The persistence of severe hyperglycemia suggests inadequaterehydration (or incorrectly mixed insulin), while too rapid a fall may be an indicatorof too rapid a rate of rehydration.TRANSITION TO ORAL INTAKE & SC INSULIN: Criteria for this transition include: normal sensorium. normal vital signs. an ability to tolerate oral intake, with no emesis. serum sodium 135-145mEq/L resolution of the acidosis reflected by:• serum PH > 7.3.• serum bicarbonate >15mEq/L.• normal anion gap. The IV insulin infusion is stopped & the 1st dose of insulin 0.2-0.4unit/kg is given s.c & repeated every 6 hrs for the next 24-48hrs.
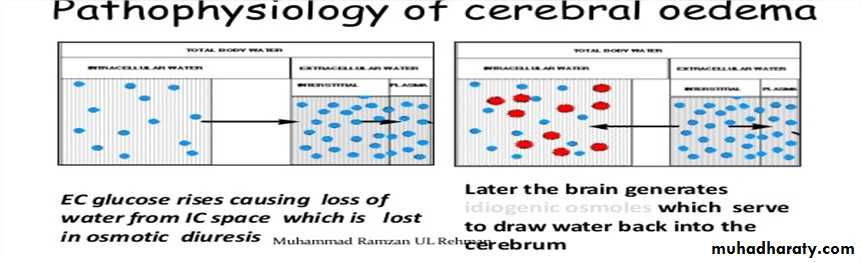
CEREBRAL EDEMA Cerebral edema is responsible for the majority of deaths relatedto DKA in children, and significant neurologic morbidity persistsin many of the survivors. While it typically presents 4 to 12 hours after treatment is begun,it can present later, or earlier, including before treatment isinitiated.
RISK FACTORS FOR CEREBRAL EDEMA
The cause of cerebral edema in DKA is not known, but there are somerisk factors attributed to cerebral edema. These include: young age. Rapid fluid replacement & insulin infusion. Injudicious use of bicarbonate therapy. Severe presentation: pH < 7.2 lower serum bicarbonate concentration higher serum glucose concentration higher blood urea nitrogen concentration hypernatremiaCLINICAL FEATURES severe headache. sudden deterioration in mental status. bradycardia (or a sudden, persistent drop in heart rate notattributable to improved hydration). Hypertension. depressed respiration cranial nerve dysfunction. posturing, and seizures incontinence. Papilledema is a late sign.TREATMENT The 1st thing to be excluded is hypoglycemia. Mannitol 0.5g/kg is infused over 30-60 min & can repeated if necessary. Fluid restricted to 2/3 maintenance & the total correction should madeover 48-72hrs. If the patient requires intubation, hyperventilation should be avoided, asit has been shown to be associated with worse outcomes