Congenital Hypothyroidism
Dr .athal - prdiatric - 5th stageEpidemiology:
The worldwide prevalence is 1/ 3000 to 1/4000.
The condition is sporadic or familial.
Females are affected twice as commonly as males
It is one of the few preventable causes of severe learning difficulties.
Etiology
It can be either primary or secondary1ry hypothyroidism: it is the most common category of congenital hypothyroidism. E.g.:
Defect of fetal thyroid development (dysgenesis). Account for 85% of the cases. It include:
Aplasia: total absence of thyroid tissue.
Hypoplasia: atrophic malfunctioning.
Ectopic: remnant of thyroid tissue are found at any place from the tongue base to neck.
Defect in thyroid hormone synthesis (dyshormonogenesis). Account for 10% of the cases, a goiter is almost always present.
Iodine deficiency: this responsible for the endemic goiter.
Maternal antibodies: TSH receptor blocking antibodies in the mother can cross the placenta & cause hypothyroidism.
Maternal medication: e.g. iodides, radioiodine, propylthiouracil & methimazole.
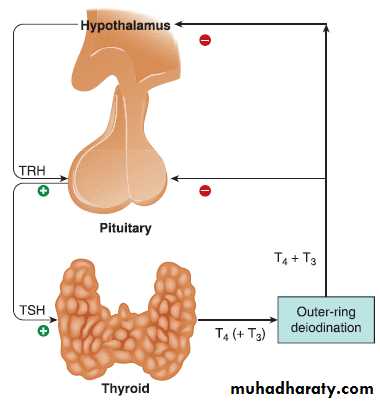
Central Hypothyroidism:
this can be due to:
TSH deficiency, isolated or multiple pituitary hormone def.
TSH unresponsiveness.
TRH deficiency, isolated or multiple hypothalamic hor def. e.g. craniopharyngioma.
TRH unresponsiveness.
Clinical Manifestation
Most infants with congenital hypothyroidism are asymptomatic at birth, even if there is complete agenesis of the thyroid gland. This situation is attributed to the transplacental passage of moderate amounts of maternal T4, which provides fetal levels that are approximately 33% of normal at birth.Birth weight and length are normal, but head size may be slightly increased because of myxedema of the brain.
the baby is sluggishness, lack of interest & somnolence.
Affected infants cry little, sleep much& have poor appetites.
Feeding difficulties and choking spells during nursing.
Respiratory difficulties, due in part to the large tongue, include apneic episodes, noisy respirations, and nasal obstruction.
The abdomen is large, and an umbilical hernia is usually present.
Edema of the genitals and extremities may be present.
Constipation.
Prolongation of physiologic jaundice, caused by delayed maturation of glucuronide conjugation.
Macrocytic anemia is often present and is refractory to treatment with hematinics.
The temperature is subnormal, often <35?C, and the skin, particularly that of the extremities, may be cold and mottled.
The pulse is slow, and heart murmurs, cardiomegaly, and asymptomatic pericardial effusion are common.
If congenital hypothyroidism goes undetected and untreated, these manifestations progress.
Retardation of physical and mental development becomes greater during the following months, and by 3-6 mo of age the clinical picture is fully developed.
The child's growth will be stunted, the extremities are short, and the head size is normal or even increased.
The anterior and posterior fontanels are open widely.
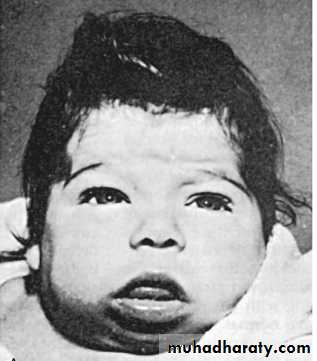
The scalp is thickened, and the hair is coarse, brittle, and scanty. The hairline reaches far down on the forehead, which usually appears wrinkled, especially when the infant cries.
The eyes appear far apart, and the bridge of the broad nose is depressed. The palpebral fissures are narrow and the eyelids are swollen.
The mouth is kept open, and the thick, broad tongue protrudes. Dentition will be delayed.
The neck is short and thick, and there may be deposits of fat above the clavicles and between the neck and shoulders
The voice is hoarse, and they do not learn to talk..
The hands are broad and the fingers are short.
The skin is dry and scaly, and there is little perspiration. Carotenemia can cause a yellow discoloration of the skin, but the sclerae remain white.
Sexual maturation may be delayed or might not take place at all.
Pseudohypertrophy of muscle especially of calf may be present.
Approximately 10% of infants with congenital hypothyroidism have associated congenital anomalies. Cardiac anomalies are most common, but anomalies of the nervous system and eye have also been reported. Infants with congenital hypothyroidism may have associated hearing loss.
Diagnosis:
Serum T4 is low & TSH is increase to >100 mU/L in 1ry hypothyroidism.the serum cholesterol level is usually elevated.
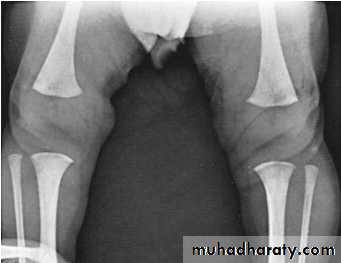
Radiological finding:
The distal femoral epiphysis is absent.
epiphyseal dysgenesis
deformity (“beaking”) of the 12th thoracic or 1st or 2nd lumbar vertebra.
skull X- ray: show large fontanels and wide sutures; intersutural (wormian) bones are common. The sella turcica is often enlarged and round; there may be erosion and thinning. Formation and eruption of teeth can be delayed.
Cardiac enlargement or pericardial effusion may be present.
Scintigraphy can help to detect the cause of congenital hypothyroidism.
Ultrasonographic examination of the thyroid is helpful.
The electrocardiogram may show low-voltage P and T waves with diminished amplitude of QRS complexes and suggest poor left ventricular function and pericardial effusion. Echocardiography can confirm a pericardial effusion.
Since most cases of congenital hypothyroidism are asymptomatic at birth, clinical diagnosis is not easily made so there is a need for screening lab. test to make such a diagnosis.
Measurement of T4 is reliable , followed by measurement of TSH when T4 is low.
Measurement of TSH at 1st can miss cases of central hypothyroidism.
Treatment
Levothyroxine given orally is the treatment of choice.In neonates, the recommended initial starting dose is 10-15 microgram/kg/day.
In older children, 4 microgram/kg/day.
Thyroxine tablets should not be mixed with soy protein formulas, concentrated iron, or calcium, because these can bind T4 and inhibit its absorption.
thyroid tests should be measured:
2 to 4 weeks after treatment is begun
every 1 to 2 months in the first 6 months of life
every 3 to 4 months between 6 months and 3 years of age
and regularly thereafter.
Prognosis
Early diagnosis and adequate treatment from the first weeks of life result in normal linear growth and intelligence comparable with that of unaffected siblings.
Delay in diagnosis, inadequate treatment, and poor compliance in the first 2-3 yr of life result in variable degrees of brain damage. Without treatment, affected infants are profoundly mentally deficient and growth retarded.