Testosterone and Other Male Sex Hormones
Lecture 223-2-2016
SECRETION, METABOLISM, AND CHEMISTRY OF THE MALE SEX HORMONE
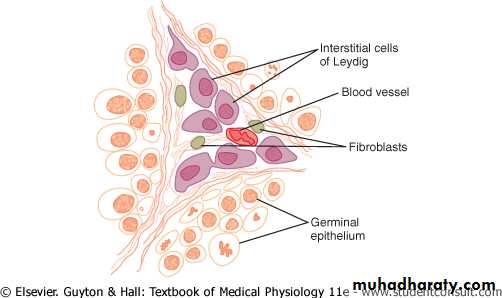
Secretion of Testosterone by the Interstitial Cells of Leydig in the Testes. The testes secrete several male sex hormones, which are collectively called androgens, including testosterone, dihydrotestosterone, and androstenedione. Testosterone is so much more abundant than the others that one can consider it to be the significant testicular hormone, although as we shall see, much, if not most, of the testosterone is eventually converted into the more active hormone dihydrotestosterone in the target tissues.Testosterone is formed by the interstitial cells of Leydig, which lie in the interstices between the seminiferous tubules and constitute about 20 per cent of the mass of the adult testes, as shown in Figure 80-7. Leydig cells are almost nonexistent in the testes during childhood when the testes secrete almost no testosterone, but they are numerous in the newborn male infant for the first few months of life and in the adult male any time after puberty; at both these times the testes secrete large quantities of testosterone. Furthermore, when tumors develop from the interstitial cells of Leydig, great quantities of testosterone are secreted. Finally, when the germinal epithelium of the testes is destroyed by x-ray treatment or excessive heat, the Leydig cells, which are less easily destroyed, often continue to produce testosterone.
Figure 80-7 Interstitial cells of Leydig, the cells that secrete testosterone, located in the interstices between the seminiferous tubules.
Secretion of Androgens Elsewhere in the Body. The term "androgen" means any steroid hormone that has masculinizing effects, including testosterone itself; it also includes male sex hormones produced elsewhere in the body besides the testes. For instance, the adrenal glands secrete at least five androgens, although the total masculinizing activity of all these is normally so slight (less than 5 per cent of the total in the adult male) that even in women they do not cause significant masculine characteristics, except for causing growth of pubic and axillary hair. But when an adrenal tumor of the adrenal androgen-producing cells occurs, the quantity of androgenic hormones may then become great enough to cause all the usual male secondary sexual characteristics to occur even in the female.
Rarely, embryonic rest cells in the ovary can develop into a tumor that produces excessive quantities of androgens in women; one such tumor is the arrhenoblastoma. The normal ovary also produces minute quantities of androgens, but they are not significant.
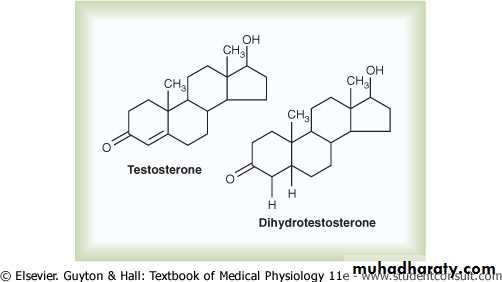
Chemistry of the Androgens. All androgens are steroid compounds, as shown by the formulas in Figure 80-8 for testosterone and dihydrotestosterone. Both in the testes and in the adrenals, the androgens can be synthesized either from cholesterol or directly from acetyl coenzyme A.
Figure 80-8 Testosterone and dihydrotestosterone.
Metabolism of Testosterone. After secretion by the testes, about 97 per cent of the testosterone becomes either loosely bound with plasma albumin or more tightly bound with a beta globulin called sex hormone-binding globulin and circulates in the blood in these states for 30 minutes to several hours. By that time, the testosterone either is transferred to the tissues or is degraded into inactive products that are subsequently excreted.Much of the testosterone that becomes fixed to the tissues is converted within the tissue cells to dihydrotestosterone, especially in certain target organs such as the prostate gland in the adult and the external genitalia of the male fetus. Some actions of testosterone are dependent on this conversion, whereas other actions are not. The intracellular functions are discussed later in the chapter.
Degradation and Excretion of Testosterone. The testosterone that does not become fixed to the tissues is rapidly converted, mainly by the liver, into androsterone and dehydroepiandrosterone and simultaneously conjugated as either glucuronides or sulfates (glucuronides, particularly). These are excreted either into the gut by way of the liver bile or into the urine through the kidneys.
Production of Estrogen in the Male. In addition to testosterone, small amounts of estrogens are formed in the male (about one fifth the amount in the nonpregnant female), and a reasonable quantity of estrogens can be recovered from a man's urine. The exact source of estrogens in the male is unclear, but the following are known: (1) the concentration of estrogens in the fluid of the seminiferous tubules is quite high and probably plays an important role in spermiogenesis. This estrogen is believed to be formed by the Sertoli cells by converting testosterone to estradiol. (2) Much larger amounts of estrogens are formed from testosterone and androstanediol in other tissues of the body, especially the liver, probably accounting for as much as 80 per cent of the total male estrogen production.
FUNCTIONS OF TESTOSTERONE
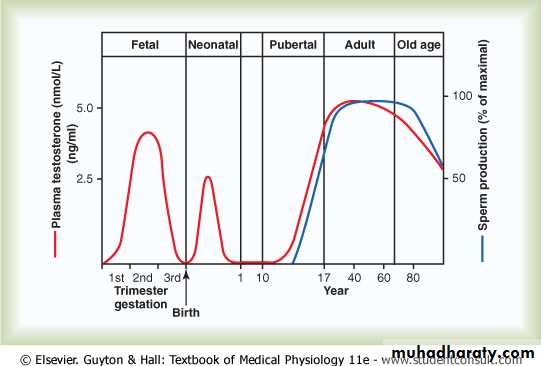
In general, testosterone is responsible for the distinguishing characteristics of the masculine body. Even during fetal life, the testes are stimulated by chorionic gonadotropin from the placenta to produce moderate quantities of testosterone throughout the entire period of fetal development and for 10 or more weeks after birth; thereafter, essentially no testosterone is produced during childhood until about the ages of 10 to 13 years. Then testosterone production increases rapidly under the stimulus of anterior pituitary gonadotropic hormones at the onset of puberty and lasts throughout most of the remainder of life, as shown in Figure 80-9, dwindling rapidly beyond age 50 to become 20 to 50 per cent of the peak value by age 80.Figure 80-9 The different stages of male sexual function as reflected by average plasma testosterone concentrations (red line) and sperm production (blue line) at different ages.
Functions of Testosterone During Fetal Development
Testosterone begins to be elaborated by the male fetal testes at about the seventh week of embryonic life. Indeed, one of the major functional differences between the
female and the male sex chromosome is that the male chromosome has the sex-determining region Y (SRY) gene that encodes a protein called the testis determining factor (also called the SRY protein). The SRY protein initiates a cascade of gene activations that cause the genital ridge cells to differentiate into cells that secrete testosterone and eventually become the testes, whereas the female chromosome causes this ridge to differentiate into cells that secrete estrogens.
Injection of large quantities of male sex hormone into pregnant animals causes development of male sexual organs even though the fetus is female. Also, removal of the testes in the early male fetus causes development of female sexual organs.
Thus, testosterone secreted first by the genital ridges and later by the fetal testes is responsible for the development of the male body characteristics, including the formation of a penis and a scrotum rather than formation of a clitoris and a vagina. Also, it causes formation of the prostate gland, seminal vesicles, and male genital ducts, while at the same time suppressing the formation of female genital organs.
Effect of Testosterone to Cause Descent of the Testes. The testes usually descend into the scrotum during the last 2 to 3 months of gestation when the testes begin secreting reasonable quantities of testosterone. If a male child is born with undescended but otherwise normal testes, the administration of testosterone usually causes the testes to descend in the usual manner if the inguinal canals are large enough to allow the testes to pass.
Administration of gonadotropic hormones, which stimulate the Leydig cells of the newborn child's testes to produce testosterone, can also cause the testes to descend. Thus, the stimulus for descent of the testes is testosterone, indicating again that testosterone is an important hormone for male sexual development during fetal life.
Effect of Testosterone on Development of Adult Primary and Secondary Sexual Characteristics
After puberty, the increasing amounts of testosterone secretion cause the penis, scrotum, and testes to enlarge about eightfold before the age of 20 years. In addition, testosterone causes the secondary sexual characteristics of the male to develop, beginning at puberty and ending at maturity. These secondary sexual characteristics, in addition to the sexual organs themselves, distinguish the male from the female as follows:
1-Effect on the Distribution of Body Hair. Testosterone causes growth of hair (1) over the pubis, (2) upward along the linea alba of the abdomen sometimes to the umbilicus and above, (3) on the face, (4) usually on the chest, and (5) less often on other regions of the body, such as the back. It also causes the hair on most other portions of the body to become more prolific.
2-Baldness. Testosterone decreases the growth of hair on the top of the head; a man who does not have functional testes does not become bald. However, many virile men never become bald because baldness is a result of two factors: first, a genetic background for the development of baldness and, second, superimposed on this genetic background, large quantities of androgenic hormones. A woman who has the appropriate genetic background and who develops a long-sustained androgenic tumor becomes bald in the same manner as does a man.
3-Effect on the Voice. Testosterone secreted by the testes or injected into the body causes hypertrophy of the laryngeal mucosa and enlargement of the larynx. The effects cause at first a relatively discordant, "cracking" voice, but this gradually changes into the typical adult masculine voice.
4-Testosterone Increases Thickness of the Skin and Can Contribute to Development of Acne. Testosterone increases the thickness of the skin over the entire body and increases the ruggedness of the subcutaneous tissues. Testosterone also increases the rate of secretion by some or perhaps all the body's sebaceous glands. Especially important is excessive secretion by the sebaceous glands of the face, because this can result in acne. Therefore, acne is one of the most common features of male adolescence when the body is first becoming introduced to increased testosterone. After several years of testosterone secretion, the skin normally adapts to the testosterone in a way that allows it to overcome the acne.
5-Testosterone Increases Protein Formation and Muscle Development. One of the most important male characteristics is development of increasing musculature after puberty, averaging about a 50 per cent increase in muscle mass over that in the female. This is associated with increased protein in the nonmuscle parts of the body as well. Many of the changes in the skin are due to deposition of proteins in the skin, and the changes in the voice also result partly from this protein anabolic function of testosterone.
Because of the great effect that testosterone and other androgens have on the body musculature, synthetic androgens are widely used by athletes to improve their muscular performance. This practice is to be severely deprecated because of prolonged harmful effects of excess androgens. Testosterone or synthetic androgens are also occasionally used in old age as a "youth hormone" to improve muscle strength and vigor, but with questionable results.
6-Testosterone Increases Bone Matrix and Causes Calcium Retention. After the great increase in circulating testosterone that occurs at puberty (or after prolonged injection of testosterone), the bones grow considerably thicker and deposit considerable additional calcium salts. Thus, testosterone increases the total quantity of bone matrix and causes calcium retention. The increase in bone matrix is believed to result from the general protein anabolic function of testosterone plus deposition of calcium salts in response to the increased protein.
Testosterone has a specific effect on the pelvis to (1) narrow the pelvic outlet, (2) lengthen it, (3) cause a funnel-like shape instead of the broad ovoid shape of the female pelvis, and (4) greatly increase the strength of the entire pelvis for load-bearing. In the absence of testosterone, the male pelvis develops into a pelvis that is similar to that of the female.
Because of the ability of testosterone to increase the size and strength of bones, it is often used in older men to treat osteoporosis.
When great quantities of testosterone (or any other androgen) are secreted abnormally in the still-growing child, the rate of bone growth increases markedly, causing a spurt in total body height. However, the testosterone also causes the epiphyses of the long bones to unite with the shafts of the bones at an early age. Therefore, despite the rapidity of growth, this early uniting of the epiphyses prevents the person from growing as tall as he would have grown had testosterone not been secreted at all. Even in normal men, the final adult height is slightly less than that which occurs in males castrated before puberty.
7-Testosterone Increases Basal Metabolism. Injection of large quantities of testosterone can increase the basal metabolic rate by as much as 15 per cent. Also, even the usual quantity of testosterone secreted by the testes during adolescence and early adult life increases the rate of metabolism some 5 to 10 per cent above the value that it would be were the testes not active. This increased rate of metabolism is possibly an indirect result of the effect of testosterone on protein anabolism, the increased quantity of proteins-the enzymes especially-increasing the activities of all cells.
8-Effect on Red Blood Cells. When normal quantities of testosterone are injected into a castrated adult, the number of red blood cells per cubic millimeter of blood increases 15 to 20 per cent. Also, the average man has about 700,000 more red blood cells per cubic millimeter than the average woman. This difference may be due partly to the increased metabolic rate that occurs after testosterone administration rather than to a direct effect of testosterone on red blood cell production.
9-Effect on Electrolyte and Water Balance. Many steroid hormones can increase the reabsorption of sodium in the distal tubules of the kidneys. Testosterone also has such an effect, but only to a minor degree in comparison with the adrenal mineralocorticoids. Nevertheless, after puberty, the blood and extracellular fluid volumes of the male in relation to body weight increase as much as 5 to 10%.
CONTROL OF MALE SEXUAL FUNCTIONS BY HORMONES FROM THE HYPOTHALAMUS AND ANTERIOR PITUITARY GLAND
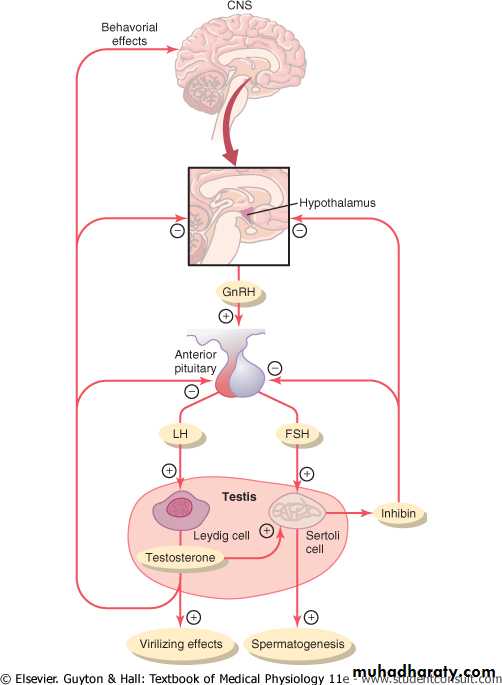
A major share of the control of sexual functions in both the male and the female begins with secretion of gonadotropin-releasing hormone (GnRH) by the hypothalamus. This hormone in turn stimulates the anterior pituitary gland to secrete two other hormones called gonadotropic hormones: (1) luteinizing hormone (LH) and (2) follicle-stimulating hormone (FSH). In turn, LH is the primary stimulus for the secretion of testosterone by the testes, and FSH mainly stimulates spermatogenesis.
GnRH and Its Effect in Increasing the Secretion of LH and FSH
GnRH is a 10-amino acid peptide secreted by neurons whose cell bodies are located in the arcuate nuclei of the hypothalamus. The endings of these neurons terminate mainly in the median eminence of the hypothalamus, where they release GnRH into the hypothalamic-hypophysial portal vascular system. Then the GnRH is transported to the anterior pituitary gland in the hypophysial portal blood and stimulates the release of the two gonadotropins, LH and FSH.GnRH is secreted intermittently a few minutes at a time once every 1 to 3 hours. The intensity of this hormone's stimulus is determined in two ways: (1) by the frequency of these cycles of secretion and (2) by the quantity of GnRH released with each cycle.
The secretion of LH by the anterior pituitary gland is also cyclical, with LH following fairly faithfully the pulsatile release of GnRH. Conversely, FSH secretion increases and decreases only slightly with each fluctuation of GnRH secretion; instead, it changes more slowly over a period of many hours in response to longer-term changes in GnRH. Because of the much closer relation between GnRH secretion and LH secretion, GnRH is also widely known as LH-releasing hormone.
Gonadotropic Hormones: LH and FSH
Both of the gonadotropic hormones, LH and FSH, are secreted by the same cells, called gonadotropes, in the anterior pituitary gland. In the absence of GnRH secretion from the hypothalamus, the gonadotropes in the pituitary gland secrete almost no LH or FSH.LH and FSH are glycoproteins. They exert their effects on their target tissues in the testes mainly by activating the cyclic adenosine monophosphate second messenger system, which in turn activates specific enzyme systems in the respective target cells.
Testosterone-Regulation of Its Production by LH. Testosterone is secreted by the interstitial cells of Leydig in the testes, but only when they are stimulated by LH from the anterior pituitary gland. Furthermore, the quantity of testosterone secreted increases approximately in direct proportion to the amount of LH available.
Mature Leydig cells are normally found in a child's testes for a few weeks after birth but then disappear until after the age of about 10 years. However, either injection of purified LH into a child at any age or secretion of LH at puberty causes testicular interstitial cells that look like fibroblasts to evolve into functioning Leydig cells.
Inhibition of Anterior Pituitary Secretion of LH and FSH by Testosterone-Negative Feedback Control of Testosterone Secretion. The testosterone secreted by the testes in response to LH has the reciprocal effect of inhibiting anterior pituitary secretion of LH (see Figure 80-10). Most of this inhibition probably results from a direct effect of testosterone on the hypothalamus to decrease the secretion of GnRH. This in turn causes a corresponding decrease in secretion of both LH and FSH by the anterior pituitary, and the decrease in LH reduces the secretion of testosterone by the testes. Thus, whenever secretion of testosterone becomes too great, this automatic negative feedback effect, operating through the hypothalamus and anterior pituitary gland, reduces the testosterone secretion back toward the desired operating level. Conversely, too little testosterone allows the hypothalamus to secrete large amounts of GnRH, with a corresponding increase in anterior pituitary LH and FSH secretion and consequent increase in testicular testosterone secretion.
Figure 80-10 Feedback regulation of the hypothalamic-pituitary-testicular axis in males.
Regulation of Spermatogenesis by FSH and TestosteroneFSH binds with specific FSH receptors attached to the Sertoli cells in the seminiferous tubules. This causes these cells to grow and secrete various spermatogenic substances. Simultaneously, testosterone (and dihydrotestosterone) diffusing into the seminiferous tubules from the Leydig cells in the interstitial spaces also has a strong tropic effect on spermatogenesis. Thus, to initiate spermatogenesis, both FSH and testosterone are necessary.
Negative Feedback Control of Seminiferous Tubule Activity-Role of the Hormone Inhibin.
When the seminiferous tubules fail to produce sperm, secretion of FSH by the anterior pituitary gland increases markedly. Conversely, when spermatogenesis proceeds too rapidly, pituitary secretion of FSH diminishes. The cause of this negative feedback effect on the anterior pituitary is believed to be secretion by the Sertoli cells of still another hormone called inhibin (see Figure 80-10). This hormone has a strong direct effect on the anterior pituitary gland to inhibit the secretion of FSH and possibly a slight effect on the hypothalamus to inhibit secretion of GnRH.Inhibin is a glycoprotein, like both LH and FSH, having a molecular weight between 10,000 and 30,000. It has been isolated from cultured Sertoli cells. Its potent inhibitory feedback effect on the anterior pituitary gland provides an important negative feedback mechanism for control of spermatogenesis, operating simultaneously with and in parallel to the negative feedback mechanism for control of testosterone secretion.
Human Chorionic Gonadotropin Secreted by the Placenta During Pregnancy Stimulates Testosterone Secretion by the Fetal Testes
During pregnancy, the hormone human chorionic gonadotropin (hCG) is secreted by the placenta, and it circulates both in the mother and in the fetus. This hormone has almost the same effects on the sexual organs as LH.
During pregnancy, if the fetus is a male, hCG from the placenta causes the testes of the fetus to secrete testosterone. This testosterone is critical for promoting formation of the male sexual organs, as pointed out earlier.
Puberty and Regulation of Its Onset
Initiation of the onset of puberty has long been a mystery. But it has now been determined that during childhood the hypothalamus simply does not secrete significant amounts of GnRH. One of the reasons for this is that, during childhood, the slightest secretion of any sex steroid hormones exerts a strong inhibitory effect on hypothalamic secretion of GnRH. Yet, for reasons still not understood, at the time of puberty, the secretion of hypothalamic GnRH breaks through the childhood inhibition, and adult sexual life begins.