AFTER MID
TOTAL LEC: 26
Gynaecology
Dr. Haydar Al-Shama’a
Lec 22 - Ovarian Tumours
DR. HAYDAR - LEC 3+4
مكتب املدينة

Benign and Malignant cysts and tumors of the
ovary
INTRODUCTION
•
The ovaries give rise to a wide varieties of tumors and cysts more
than any organ in the body. This gives number of problems
regarding classification, diagnosis and treatment.
•
The picture is more confused by the occurrence of functional and
physiological cysts (which are difficult to differentiate from
neoplastic cysts).
•
Ovarian cysts and tumors can affect all age groups. They are often
asymptomatic even the malignant ones (so there is a risk of
delayed diagnosis).
CLASSIFICATION OF OVARIAN TUMORS
There are many types of classification (according to histopathology),
which we depend on in determining:
o the prognosis
o Type of chemotherapy
o Method of treatment
WHO Classification:
1) Epithelial tumors 75%
• serous (benign , borderline , malignant)
• mucinous
• endometrioid
• clear cell
• Brenner
• mixed
• unclassified
2) Sex cord tumors 5-10%
• granulosa stromal cell tumor:
1- granulosa
2- thecoma
3- fibroma
• androblastoma (Sertoli – Leydig )
• gynandroblastoma (Sertoli – granulosa)
3)
Germ cell tumors 15-20%
• teratoma
• dysgerminoma
• choriocarcinoma
• endodermal sinus tumor
• embryonal carcinoma
• polyembryoma
•
mixed
4)
metastatic tumors 5%
• Krukenberg tumor
• lymphoma
5)
Others
Serov classification
1)
Epithelial
2)
Sex cord
3)
Lipid cell
4)
Germ cell
5)
Gonadoblastoma
6)
Soft tissue tumors non specific to ovaries
7)
Unclassified
8)
Secondary ovarian tumors
Tumor like conditions
1.
Follicular cyst
2.
Corpus luteum cyst
3.
Theca-lutein cyst
4.
Polycystic disease
5.
Endometriomatous cyst
6.
Inflamatory
7.
others
EPITHELIAL TUMORS
Serous tumor
: (comprises 40% of all tumors
)
•
Benign (serous cystadenoma): Presented as a single Loculus of
moderate size and smooth outline containing clear serous fluid,
lining may have papilliferous processes. could be bilateral in 50% of
cases.
Histopathology: single columnar or cuboidal epithelium with cilia (
like the Fallopian tube).
•
Malignant (serous cystadenocarcinoma)
It is the most common type
of ovarian cancer. May be cystic or solid or a combination of both. it
is usually lined by fine papilliferous processes which may perforate
the cyst wall causing spread to peritoneal cavity, tubes, uterus.
Calcium deposition may occur (psammoma bodies). It could be
bilateral in 50% cases.
Mucinous tumor:
•
Benign (mucinous cystadenoma):
It is a unilateral, multilocular cyst
with smooth outlines that may reach an enormous size. Its lining is
tall columnar cells with dark nuclei similar to cervical glands and is
filled with jelly like mucin.
Spontaneous perforation may cause seedling of benign or low
malignant cells in the peritoneal cavity. Ascitis containing gelatinous
fluid may develop (pseudomyxoma peritonei) which can lead to
cachexia then death, usually after several laparotomies. (there is 5-
10% tendency for malignant transformation)
•
Malignant (mucinous cystadenocarcinoma) are relatively chemo
and radio resistant.
Endometrioid tumor:
Solid cystic tumor often contains hemorrhagic
area. its lining is similar to that of proliferative endometrium with
glands. It is usually malignant (benign are rare) and sometime is found in
association with endometrial cancer.
Brunner tumor: I
t is a borderline malignant unilateral, solid tumor
measuring 5 to 15 cm.
Histopathology: transitional epithelial cells embedded in a fibrous tissue
stroma.
SEX CORD TUMORS
Granulosa cell tumor:
It is unilateral yellow lobulated solid or partly
cystic tumor which can occur at any age group. it is considered a Low
grade malignancy (borderline malignant) that mostly secret estrogen
and rarely testosterone.
Histopathology: composed of granulosa cells which sometimes form
micro follicles called Call – Exner bodies.
Theca cell tumor:
Firm yellow tumor that is mostly benign
,
usually
secret estrogen rarely androgens.
Fibroma:
These are solid white lobulated VERY HARD masses that and
highly mobile. They are mostly benign tumor associated with ascitis and
pleural effusion , this triad is named Meig’s syndrome.
Androblastoma:
Composed of Sertoli and Leydig cells and form
seminiferous tubules like those found in testis but without spermatozoa,
they mainly Secret testosterone.
GERM CELL TUMORS
These are tumors derived from totipotent stem cells (has the
potential to differentiate to all types of tissues) i.e., can differentiates to
embryonic cell line or extra-embryonic cell line (chorionic cells).
Teratoma
•
Mature teratoma (benign dermoid cyst): considered the commonest
ovarian cyst seen in young women. It affects women in 2
nd
and 3
rd
decade of life and is 20% bilateral.
It is seen as smooth unilocular cyst (filled with sebum) that lies in the
vesico-uerine pouch, there is a hump of tissue at one side called
mammillary process. The hump consists of endoderm, mesoderm and
ectoderm types of tissue (bone, teeth, cartilage, skin, sebaceous
glands, hair) that project inside the cavity. It may be also composed of
thyroid tissue causing thyrotoxicosis called stroma ovarii.
•
Immature teratoma: It is usually solid and unilateral affecting women
in 2
nd
decade of life. They are mostly malignant ( benign solid
teratomas are rare).
Dysgerminoma:
Presented as yellow creamy lobulated solid tumor
that is soft in consistency, it is 10 – 20 % bilateral. Being highly radio and
chemo sensitive is a very important feature of this tumor.
Histopathology: large polyhedral cells with glycogen.
Choriocarcinoma (non gestational):
These are tumors that consist
of trophoblastic tissue and secret hCG.
SECONDARY OVARIAN TUMORS
Could be metastasis from other organs (uterus, stomach, colon, breast)
Krukenberg tumor:
Bilateral solid masses of adenocarcinoma,
composed of signet ring cells with mucin which push the nucleus to the
periphery of the cell. The tumor may become larger than the primary
site.

ETIOLOGY OF OVARIAN TUMORS
o Unknown
o Environmental
- High fat diet - Low fiber diet
- Vitamin A - Talcum powder
- Caffeine - Asbestos
- Viral infection (mumps, rubella, influenza) - Radiation
o Hormonal effect
Protective factors: pregnancy, breast feeding, OCCP
Risk factors: Nulliparity, drugs for ovulation induction, early
menarche and late menopause
o Tubal ligation and hysterectomy are considered protective
against ovarian cancer.
o Endometriosis increase the risk of ovarian cancer
o Genetic factors
1. Site specific ovarian cancer (autosomal dominant)
2. Hereditary breast-ovarian cancer syndrome
Lynch syndrome II hereditary non polyposis colonic cancer (HNPCC)
EPIDEMIOLOGY
•
Constitutes 35% of genital tract malignancy
•
The risk increases in industrialized countries
•
More than 50% mortality
•
Most epithelial cancers occur in post menopausal women
•
The disease is usually asymptomatic and at the time of
presentation, it has usually extended beyond the ovaries and
involved adjacent organs.
SPREAD OF OVARIAN TUMORS
1. Local infiltration to near organs (by perforating the capsule)
reaching the omentum, broad ligament, bowel, uterus...etc.
2. Transperitoneal spread through seedling of peritoneal cavity.

3. Lymphatic spread through para-aortic lymph nodes to thoracic
duct then to left supraclavicular L.N
4. Hematological spread (uncommon)
STAGING
Is the determination of the extent of the disease by
preoperative clinical
exam and investigations, but the final staging is surgical.
•
FIGO staging
1. Stage I ( limited to the ovaries )
2. Stage II ( pelvic extension )
3. Stage III (intraperitoneal metastasis )
4. Stage IV ( distant metastasis )
CLINICAL FEATURES OF OVARIAN TUMORS
•
Age incidence: with the exception of germ cell and sex cord
tumors , most ovarian tumor occur at the age of 40 to 60 years.
•
Asymptomatic: many ovarian masses are discovered accidentally
during routine antenatal care or during routine exam at medical or
surgical clinics
•
Pain: pain is an unusual symptom but it could occur in the
following situation:
o Metastasis to sacral plexus causes sacral root pain and dull
aching back pain.
o Complicated cysts (rupture, hemorrhage, twist, impaction
and
infection)
cause
acute
abdominal
pain
(acute abdomen)
•
Abdominal enlargement
•
Pressure symptoms
1) bowel : indigestion, loss of appetite, vomiting ,constipation
2) bladder: frequency, retention of urine
3) venous plexus: varicose veins of the vulva or lower limbs,
hemorrhoids
•
Menstrual cycle neither benign nor malignant tumors affect the
menstrual cycle (the cycle usually remains regular) except when
the tumor is hormonally active (rare)
•
Tumors that secret estrogen
child → precocious puberty
adult → menstrual irregularity
old → post menopausal bleeding
• Tumors that secret androgens
child → heterosexual precocious puberty
adult → defeminization (breast atrophy, amenorrhea) followed
by masculinization (deep voice, hirsutism, enlarged clitoris,
muscular built)
PHYSICAL SIGNS OF OVARIAN TUMORS
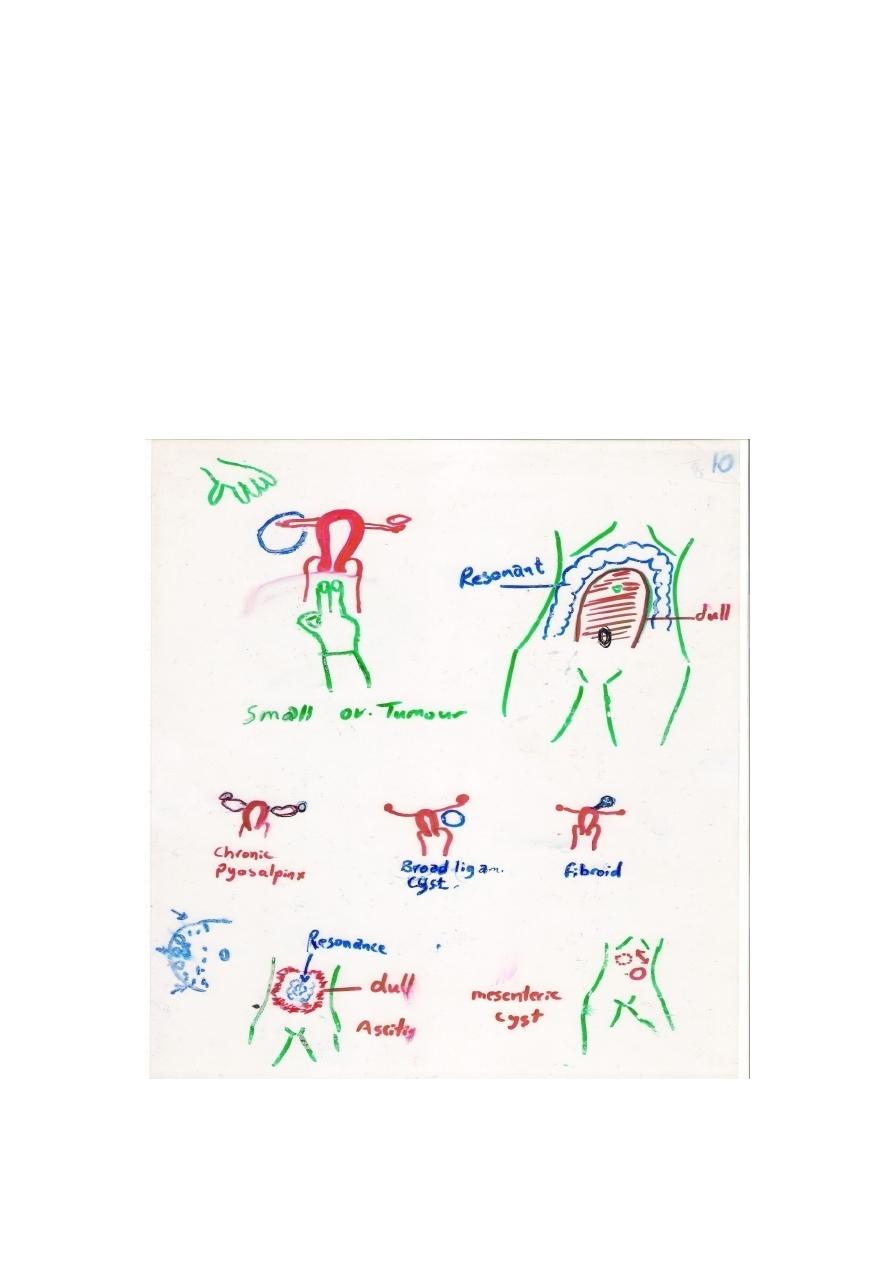
•
Small pelvic ovarian tumor: since they lie in the pelvis they are not
palpable abdominally and are only palpable by vaginal
examination
.
ovarian tumor feels as a smooth mobile mass behind and to
the side of the uterus (the uterus can be separated from the
mass). Sometimes the mass may be felt anterior to the uterus
suggesting dermoid cyst or torsion.
• Big ovarian tumor: extends from the pelvis to the abdomen. It has
a tendency to lie in the midline just under the abdominal wall
pushing the bowl up and to the side.
DIFFERENTIAL DIAGNOSIS of SMALL pelvic ovarian tumor
1. tubo-ovarian abscess (bilateral and fixed, painful associated with
pyrexia).
2. Broad ligament cyst (unilateral and fixed pushing the uterus to the
other side, painless)
3. Pedunculated fibroid (difficult to differentiate)
4. Chronic ectopic pregnancy
5. Pelvic kidney (posterior fixed mass, IVP is diagnostic)
DIFFERENTIAL DIAGNOSIS of LARGE pelvic ovarian tumor
1. Full bladder (voiding or catheterization → mass disappears)
2. Fecal mass (elongated liable for indentation, defecation changes
the shape and site of the mass)
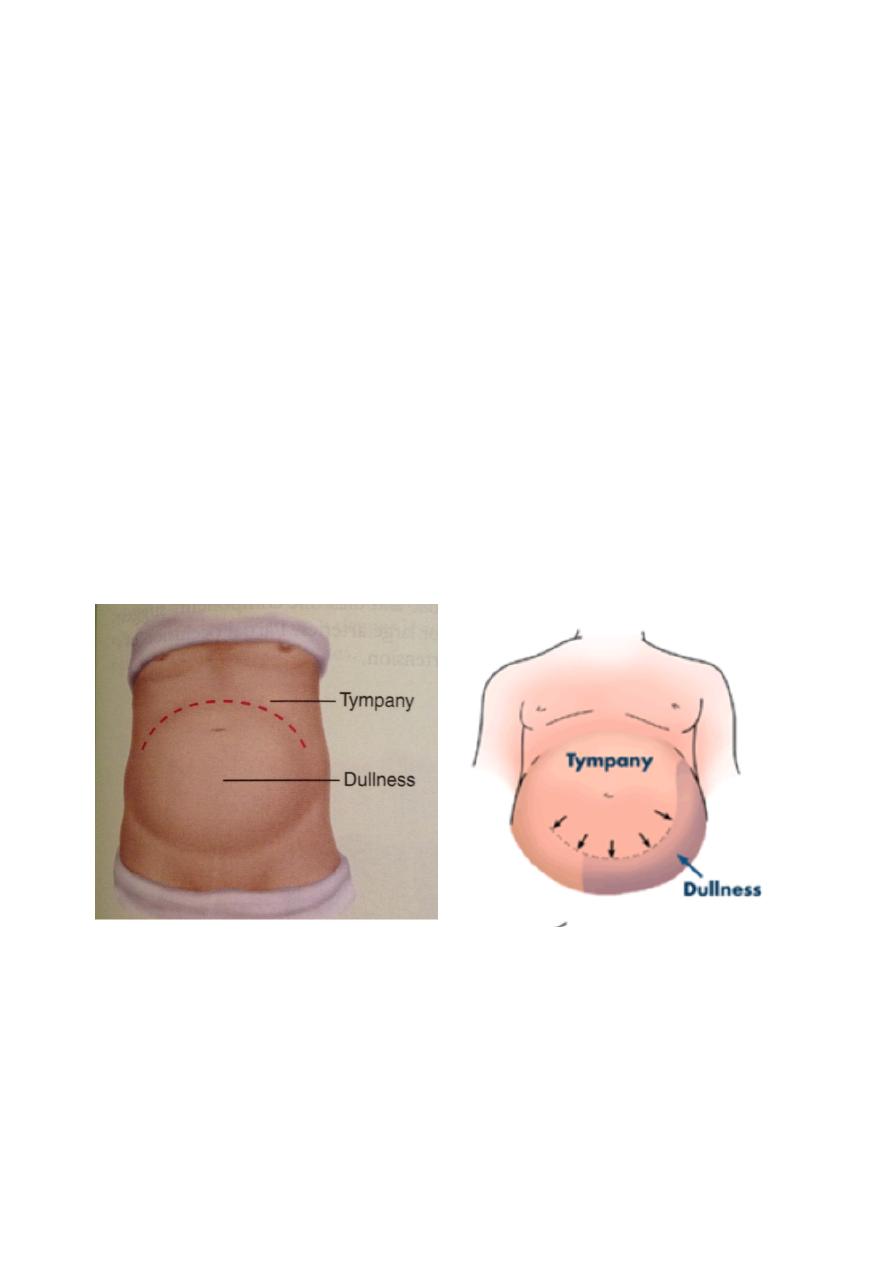
3. Ascitis (resonant at the center, dull at the periphery)
4. Fibroid (firm mass that moves with the uterus, if pedunculated it
is hard to differentiate it from ovarian tumor)
5. Pregnancy (central mass, characteristic consistency, fetal parts
can be felt and fetal heart sound can be measured)
6. Gross obesity (distended abdomen, no mass can be felt)
7. Large hydrosalpinx
8. Enlarged spleen
9. Flatulence
10. Mesenteric cyst (you can feel a whole cyst, moving only in one
plane perpendicular to the root of mesentery)
Dullness of Ovarian tumor Dullness of Ascitis
COMPLICATIONS OF OVARIAN TUMOR/CYST
1)
Torsion:
twisting of the cyst along with the ovary on its pedicle,
leading to venous blood flow obstruction, congestion, hemorrhage
inside the cyst and pain, followed by obstruction of arterial blood
flow resulting in necrosis.
Large cysts are unlikely to twist due to the presence of adhesions, so
torsions usually occur in moderate size cysts.
Presentation: colicky abdominal pain (intermittent then continuous)
associated with vomiting. On PV exam there is tender adnexial mass.
Treatment: emergency laparotomy/laparoscopy.
2) Rupture: it is either Spontaneous (occurring in large rapidly growing
tumor with necrosis of the wall) or Traumatic (during PV exam or
after blow to the abdomen)
The symptoms and signs depend on the content of the cyst:
• If clear non irritant material → no symptoms (only diagnosed
when the cyst suddenly disappears on u/s follow up)
• If irritant as blood or sebum → acute abdomen
Treatment: laparotomy/laparoscopy.
3) Hemorrhage: may occur inside a cyst causing rapid enlargement and
acute abdominal pain
Treatment: laparotomy/laparoscopy.
4) Impaction: the cyst grows but remains in the pelvis, pressing on the
bladder neck and rectum causing abdominal pain, retention of urine
and constipation.
Treatment: laparotomy/laparoscopy
5) Infection: from nearby structure like appendix, diverticulum, cause
pelvic abscess
Treatment:- laparotomy/laparoscopy

INVESTIGATIONS OF OVARIAN TUMOR/CYST
1. Ultrasound + Doppler ( Is the main investigation )
2. radiology:
a) may show calcifications, teeth.
b) CXR preoperative investigation
c) IVP
d) CT scan MRI
3. Paracentesis: cytology of ascitis (avoid puncturing the cyst)
4. OGD , colonoscopy
5. Tumor markers ( CA125 for epithelial Cancer and hCG, CEA , AFP,
for germ cell tumors)
CLINICAL FEATURES SUGGESTING MALIGNANCY
1. Age: childhood tumors are usually malignant. while in adults,
chances of malignancy increase with increasing age.
2. Pain: dull aching pain and sacral root pain suggest malignancy
3. Rapid growth
4. Solid or solid/cystic
5. Bilateral
6. Ascitis
7. Leg edema
8. Fixation
9. Vulvar varices
10. Metastasis *** indicates malignancy
TREATMENT OF OVARIAN TUMORS / CYST
•
First step to do is to determine whether the mass is functional or
neoplastic. If proven to be neoplastic, determine whether it is
benign or malignant.
•
Calculate the Risk of Malignancy Index ( RMI ) = CA 125 u/ml x US
score x menopausal score
•
US score = is calculated by giving 1 point for each of the following
feature : multilocular, bilateral, solid area, metastasis, ascitis.
(0 = for no feature on US, 1 = for one US finding , 3 = for two or
more features found on US )
•
Menopausal Score = (1 = if the patient is Premenopausal, 3 = if
the patient is postmenopausal)
EXAMPLE 1: 25 year old patient presented with a simple bilateral
ovarian cyst. CA 125 = 20 u/ml
RMI = CA 125 u/ml x US score x menopausal score
RMI = 20 x 1 x 1
RMI = 20 → low risk of malignancy ( cutoff value = 200 )
EXAMPLE 2: 55 year old patient presented with a solid bilateral tumor.
CA125 = 90 u/ml
•
RMI = CA 125 u/ml x US score x menopausal score
•
RMI = 90 x 3 x 3
•
RMI = 810 high risk of malignancy
TREATMENT:
v
FUNCTIONAL CYST: (unilateral, simple cyst, thin walled, no ascitis,
less than 7 cm) and the patient is asymptomatic → only follow up
for 6 weeks (Functional cyst will disappear).
v
OVARIAN NEOPLASM: Mainly surgical
•
Laparoscopy for benign ( low risk )
•
Laparotomy for malignant (high risk)
v
BENIGN OVARIAN CYST:
•
Below age of 45 years → cystectomy for small cyst
→ oopherectomy for large cysts
•
Above age 45 years → TAH + BSO
v
MALIGNANT OVARIAN TUMOR
•
Stage I and II → TAH + BSO + omentectomy + para aortic
lymphadenectomy + biopsy from diaphragm.
•
Stage III and IV → surgical staging + cytoreduction +
chemo/radio therapy
TERMINAL CARE
o Ascitis: repeated aspiration, sometimes local chemotherapy.
o Intestinal obstruction: subacute obstruction is treated
conservatively, Surgical treatment is indicated if the disease is
limited to a small segment of the bowel.
o Pain: pain relief is an essential part of terminal care and it is the
least thing to do to the patient.
TUMOR LIKE CONDITIONS
Follicular cyst:
presents as thin walled cyst lined by granulosa cells
containing clear fluid. They are very common and rarely exceed 5 cm
(When it is small, follicular cyst is not regarded abnormal).
•
occurs when the Graffian follicle does not rupture during
ovulation.
•
Mainly asymptomatic but they secret estrogen, so may cause
endometrial hyperplasia.
Corpus luteum cyst:
Bleeding inside the corpus luteum results in cyst
formation that secrets progesterone.
Corpus luteum will persist
(Increase its life span) → Delayed menstruation and since sometimes it is
painful, it could be misdiagnosed as ectopic.
Theca lutein – graulosa lutein cyst
: usually Bilateral, occuring when
there is an excessive ovarian stimulation by gonadotrophins.
•
From H- mole secreting hCG
•
From Clomiphene treatment or FSH
Cyst disappears when gonadotrophin stimulation is withheld.
OVARIAN TUMORS IN PREGNANCY
•
Occur in 1/1000 pregnancy
•
5% malignant
•
10% functional
•
85% benign, dermoid and cystadenoma
Treatment:
•
Malignant → treat irrespective to pregnancy
•
Benign → treat in 2nd trimester
