BRONCHIAL ASTHMA IN CHILDREN
Prof.Dr. Muhi K. AljanabiMRCPCH; DCH; FICMS
Consultant Pediatric Pulmonologist
ASTHMA---OBJECTIVES
• Understand the natural history of asthma during childhood.• Be familiar with the key features of history and examination that support a diagnosis of asthma.
• Be familiar with the other common clinical conditions that can mimic asthma (gastroesophageal reflux, cystic fibrosis, viral induced wheezing, bronchiolitis, croup).
ASTHMA---OBJECTIVES
• 4-Be able to manage an acute exacerbation of asthma.• 5-Know the details of the drugs used to treat acute and chronic asthma and understand their mechanism of action.
• 6-Know the guidelines for the management of asthma.
• 7-Be able to advise parents about how to care for a child with asthma.
Childhood Asthma..Definition
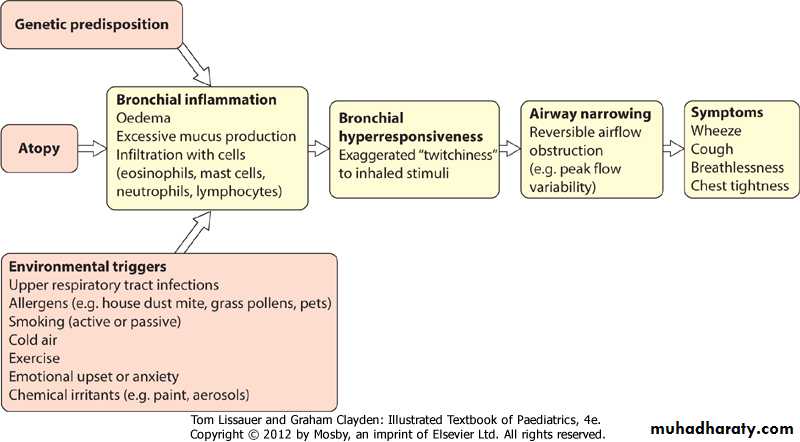
• Asthma is a chronic inflammatory condition of the lung airways resulting in episodic airflow obstruction.• This chronic inflammation heightens the “twitchiness” of the airways—airways hyperresponsiveness (AHR)—to provocative exposures.
ETIOLOGY
• Genetics:
• More than 22 loci on 15 autosomal chromosomes have been linked to asthma.
ETIOLOGY
• Environment :• common respiratory viruses .
• Indoor and home allergen exposures in sensitized individuals
• Environmental tobacco smoke and air pollutants (ozone, sulfur dioxide)
• Cold dry air and strong odors
EPIDEMIOLOGY
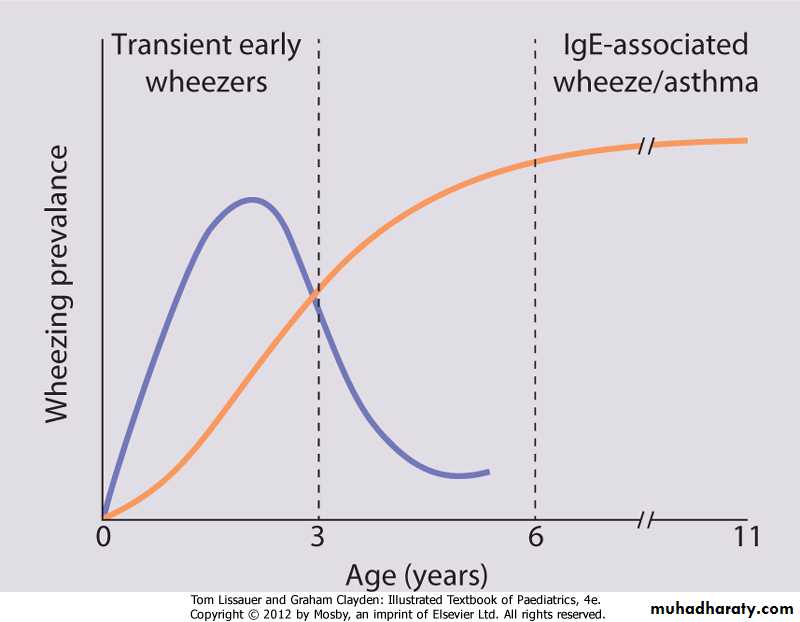
• Worldwide, childhood asthma appears to be increasing in prevalence, despite considerable improvements in management.• in 56 countries found a wide range in asthma prevalence, from 1.6 to 36.8%.
• Approximately 80% of all asthmatics report disease onset prior to 6 yr of age.
• only a minority will go on to have persistent asthma in later childhood.
•
•
CLINICAL MANIFESTATIONS
• Intermittent dry coughing and/or expiratory wheezing are the most common chronic symptoms of asthma.• shortness of breath
• worse at night
• Daytime symptoms, often linked with physical activities
Risk factor
• history of other allergic conditions (allergic rhinitis, allergic conjunctivitis, atopic dermatitis, food allergies)• parental asthma, and/or symptoms apart from colds, supports the diagnosis of asthma.
LABORATORY FINDINGS
• Lung function tests can help to confirm the diagnosis of asthma and determine disease severity.• Chest radiographs in children with asthma often appear to be normal, hyperinflation (flattening of the diaphragms) and peribronchial thickening.
LABORATORY FINDINGS
• asthma masqueraders (aspiration pneumonitis, bronchiolitis obliterans)• asthma exacerbations (atelectasis, pneumomediastinum, pneumothorax). CT scans may be needed .
• Other tests, such as allergy testing to assess sensitization to inhalant allergens, help with the management and prognosis of asthma.
• 88% of asthmatic children had inhalant allergen sensitization by allergy prick skin testing.
TREATMENT
• Principles of Asthma Pharmacotherapy:• treat all “persistent” asthma with anti-inflammatory controller medication
• Daily controller therapy is not recommended for mild intermittent asthma.
The “three strikes” rule
• Day time asthma symptoms at least 3 times per wk,• awakens at night at least 3 times per mo,
• experiences asthma exacerbations that requires short courses of systemic corticosteroids at least 3 times a yr.
• then that patient should receive daily controller therapy
TREATMENT
• (ICS) therapy is recommended as preferred therapy for all levels of asthma severity except for the mild intermittent category.• Leukotriene pathway modifiers or sustained-release theophylline (only for patients >5 yr of age) are alternatives for mild persistent asthmatics.
TREATMENT
• Combination of a low-to-medium dose ICS with a long-acting β-agonist or a leukotriene modifier or theophylline is a mainstay therapy for moderate persistent asthma in older children.• For infants and young children, medium-dose ICS alone it is considered a preferred treatment for moderate persistent asthma.
TREATMENT
• Severe persistent asthmatics should receive high-dose ICS, a long-acting bronchodilator, and routine oral corticosteroids if needed.
• SABAs are the recommended quick-reliever medications for symptoms and exercise pretreatment for all asthma severity levels
INHALED CORTICOSTEROIDS
• Daily ICS therapy as the treatment of choice for all patients with persistent asthma.• ICS reduce asthma symptoms, improve lung function, reduce “rescue” medication use and, most important, reduce urgent care visits, hospitalizations, and prednisone use for asthma exacerbations by about 50%
LONG-ACTING INHALED β-AGONIST
• Although LABAs (salmeterol, formoterol) are considered to be daily controller medications, not intended for use as “rescue” medication for acute asthma symptoms or exacerbations,• nor as monotherapy for persistent asthma.
LEUKOTRIENE-MODIFYING AGENTS
• leukotriene receptor antagonists (LTRA)• Montelukast > 1 yr.
• Zafirlukast > 5 yr
• Decrease need for rescue β-agonist use
NONSTEROIDAL ANTI-INFLAMMATORY AGENTS
• Cromolyn and nedocromil are non-corticosteroid anti-inflammatory agents that can inhibit allergen-induced asthmatic responses and reduce exercise-induced bronchospasm.THEOPHYLLINE
• Although it is considered an alternative monotherapy controller agent for older children and adults with mild persistent asthma,
• it is no longer considered a first-line agent for small children in whom there is significant variability in the absorption and metabolism of different theophylline preparations, necessitating frequent dose monitoring (blood levels) and adjustments.
SHORT-ACTING INHALED β-AGONISTS
• SABAs (albuterol, levalbuterol, terbutaline, pirbuterol) are the first drugs of choice for acute asthma symptoms (“rescue” medication) and for preventing exercise-induced bronchospasm.ANTICHOLINERGIC AGENTS
• ipratropium bromide are much less potent than the β-agonists.• Inhaled ipratropium is primarily used in the treatment of acute severe asthma.
• When used in combination with albuterol, ipratropium can improve lung function and reduce the rate of hospitalization in children who present to the emergency department with acute asthma.
Home Management of Asthma Exacerbations
• Immediate treatment with “rescue” SABA• Short course of oral corticosteroid therapy
• Injectable forms of epinephrine
• Portable oxygen at home.
• Call for emergency support services.
ED Management of Asthma
• Oxygen• Inhaled β-agonist
• Systemic corticosteroids
• Inhaled ipratropium
• Intramuscular injection of epinephrine or other β-agonist
• Close monitoring of clinical status, hydration, and oxygenation
• Intubation and mechanical ventilation
PROGNOSIS
• Recurrent coughing and wheezing occurs in 35% of pre–school-age children.
• ⅓ continue to have persistent asthma into later childhood.
• ⅔ improve on their own through the preteen years.
• That entire wheeze is not asthma
• &• asthma does not always wheeze
Mark yes or no
Wheeze after 3 yearWheeze before 3 years
Atopy
Mostly persistSmoking mother during pregnancy
Mark yes or no
controllerpreventer
drug