Medicine
Dr. Zuhair
Neurology
“
Coma
”
Dr. Zuhair
LECTURE 13
Coma Dr. Zuhair
2
Coma
Objectives
To roughly understand the anatomical basis of Consciousness
To know the common causes of coma
To know the basic management of patients with coma.
Definition
Consciousness is a state of awareness of self and environment, responsiveness
(by thought and physical action) to external stimulation and inner need and
wakefulness (eyes are open.)
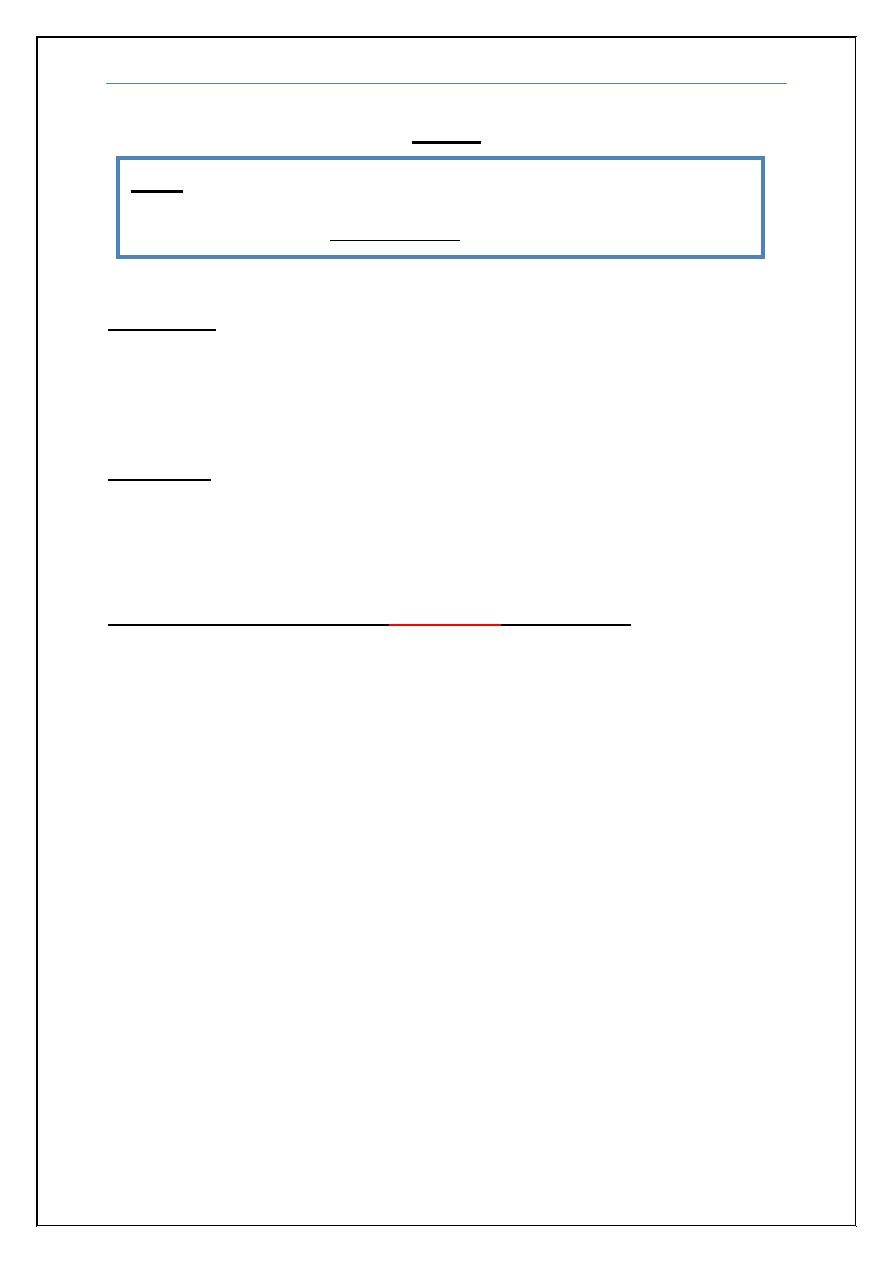
Anatomy of consciousness (
Important
for the exam
!)
Almost all instances of diminished alertness can be traced to widespread
(bilateral) abnormalities of the cerebral hemispheres or unilateral (small) lesion
of a special system termed the reticular activating system (RAS) which
originates from rostral brain stem and projects after synaptic relays in the
thalamic nuclei to the cerebral cortex; it controls the overall degree of central
nervous system activity, including wakefulness, attentiveness and sleep.
It follows that the principal causes of coma are (1) lesions that damage
the RAS or its projections (even small lesion that are unilateral); (2)
destruction of large portions of both cerebral hemispheres; and (3)
suppression of reticulo-cerebral function by drugs, toxins, or metabolic
derangements such as hypoglycemia, anoxia, uremia, and hepatic failure.
The proximity of the RAS to structures that control pupillary function
and eye movements (in the brainstem) permits clinical localization of the
cause of coma in many cases. Abnormalities in pupillary reactivity to light and
eye movements suggest brain stem lesion while preservation of these functions
indicates lesions or metabolic suppression of the cerebral hemispheres.
Note
: This lecture has been extensively edited by the students and contains much
more information than the one presented by the doctor, if you want you can find the
original unedited lecture in muhadharaty.com as a pdf or a slideshow.
Coma Dr. Zuhair
3
Aetiology
1) Metabolic: Many systemic metabolic abnormalities cause coma by
interrupting the delivery of energy substrates hypoxia, ischemia, and
hypoglycemia (single most important metabolic cause) or by altering neuronal
excitability (drug and alcohol intoxication, anesthesia, and epilepsy).
Extrinsic:
Alcohol
Substance abuse
Drugs
Heavy metals and
poisons
Intrinsic:
Fluid (Shock) and
electrolytes
Nutritional (e.g.
Thiamine deficiency)
Endocrine
Organ failure
Note mentioned by Dr. Zuhair:
Most important metabolic
causes
of coma are
hypoglycemia, Thiamine
deficiency (Wernicke's
encephalopathy) and morphine
or benzodiazepine intoxication.
Rx
: Glucose water for
hypoglycemia, Thiamine
(VitB1) for thiamine deficiency,
Naloxone for morphine
intoxication and Flumazenil for
benzodiazepine intoxication.
Coma Dr. Zuhair
4
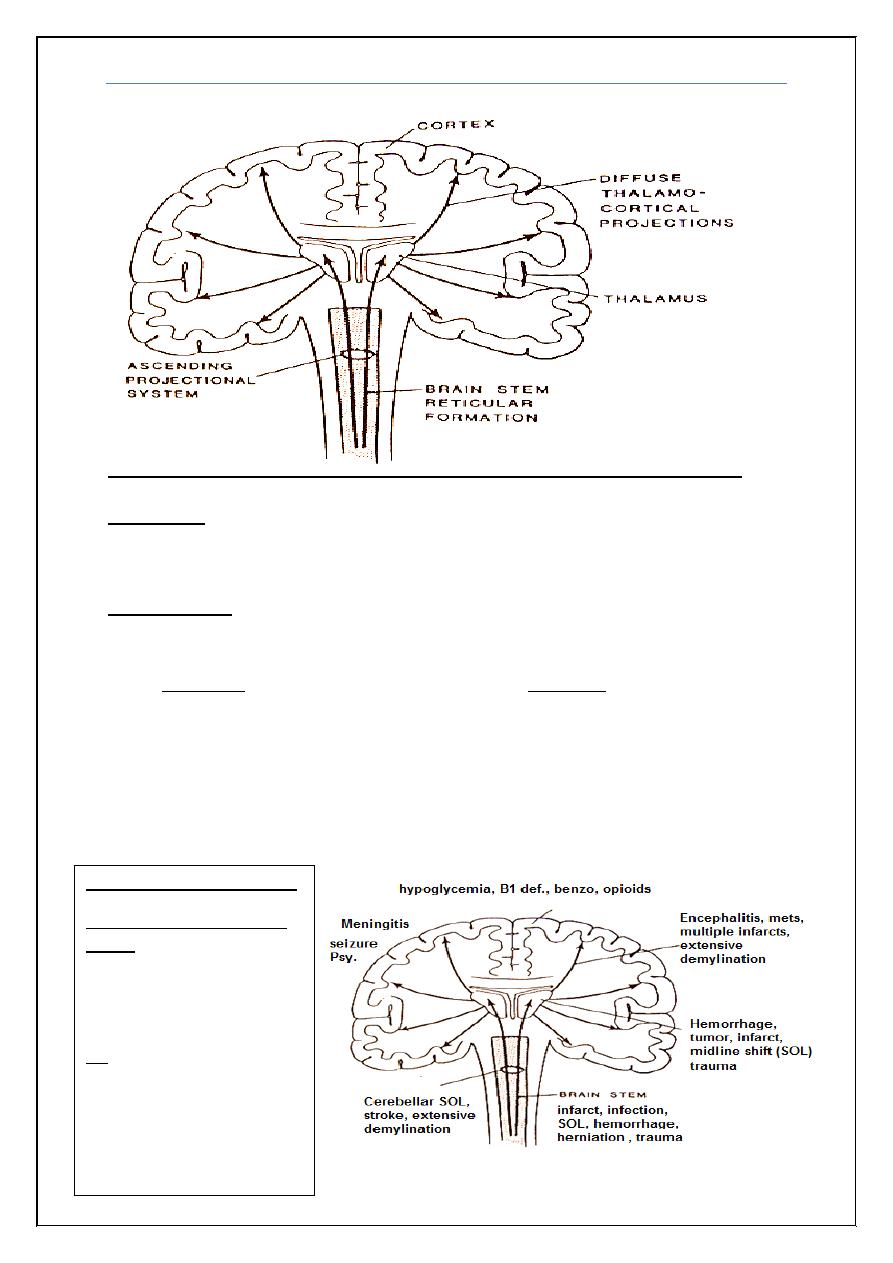
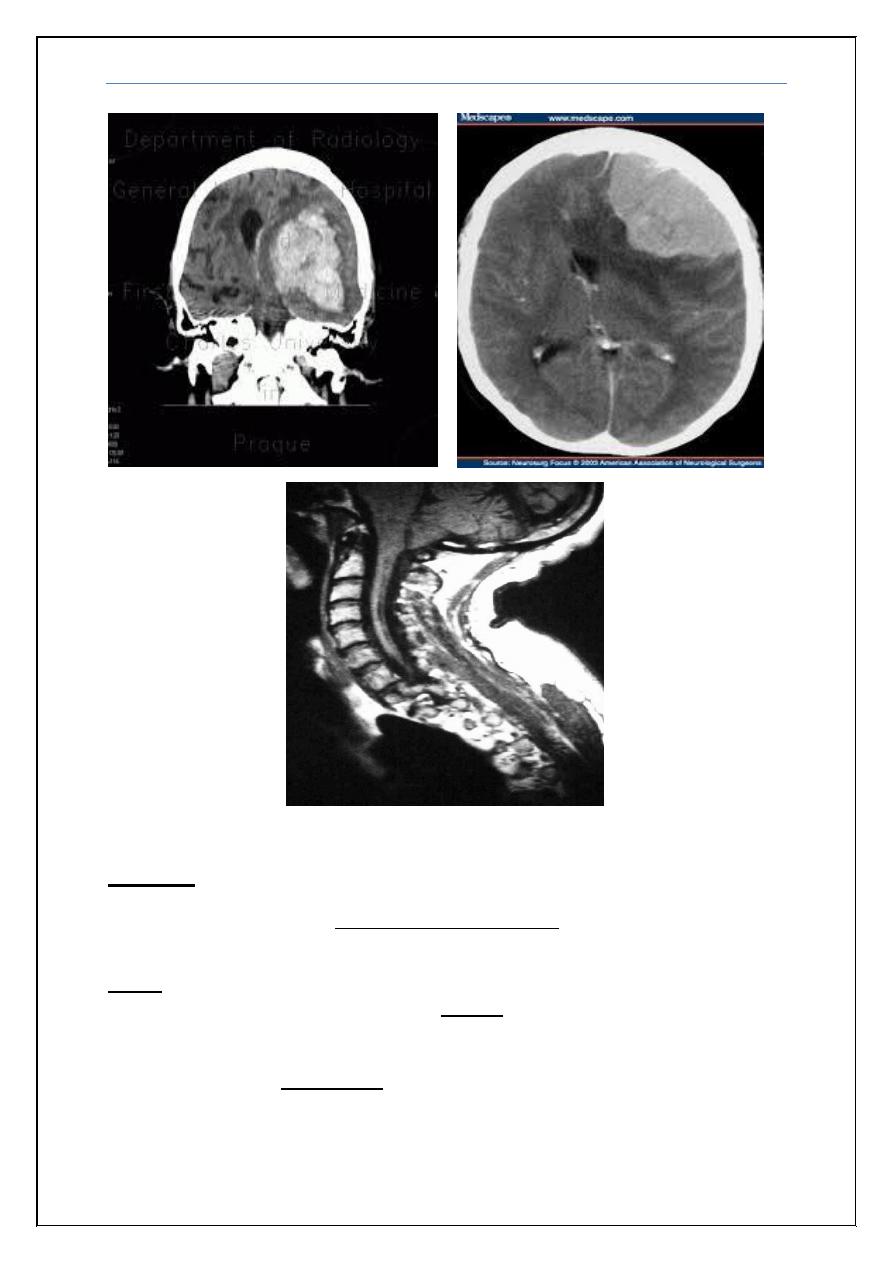
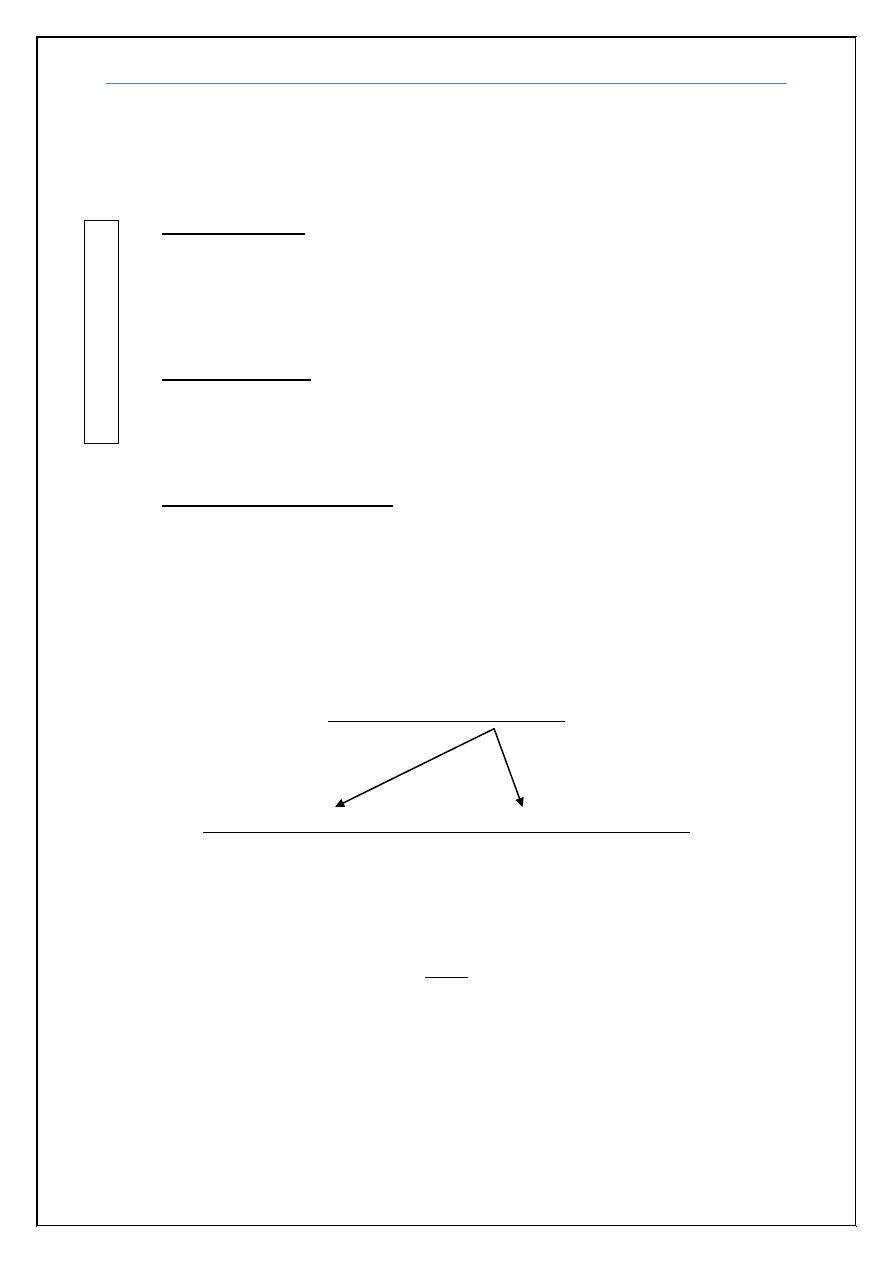
2) Structural (Cerebral Mass Lesions and Herniations)
The cranial cavity is separated into compartments by infoldings of the dura. The
two cerebral hemispheres are separated by the falx and the anterior and
posterior fossae by the tentorium.
Herniation refers to displacement of brain tissue into a compartment that it
normally does not occupy. The most common herniations are from the
supratentorial to the infratentorial compartments through the tentorial opening,
hence transtentorial. The causes of structural coma is usually (Traumatic,
Vascular, Inflammatory, Neoplastic or Degenerative)
Supratentorial herniation (should be extensive)
1) Uncal transtentorial herniation refers to impaction of the anterior
medial temporal gyrus (the uncus) into the tentorial opening just anterior
to and adjacent to the midbrain. The displaced brain tissue compresses the
third nerve as it traverses the subarachnoid space, and results in
enlargement of the ipsilateral pupil.
2) Central transtentorial herniation denotes a symmetric downward
movement of the thalamic medial structures through the tentorial opening
with compression of the upper midbrain.
3) Cingulate (subfalcine) is the displacement of the cingulate gyrus under
the falx and across the midline.
4) Transcalvarial
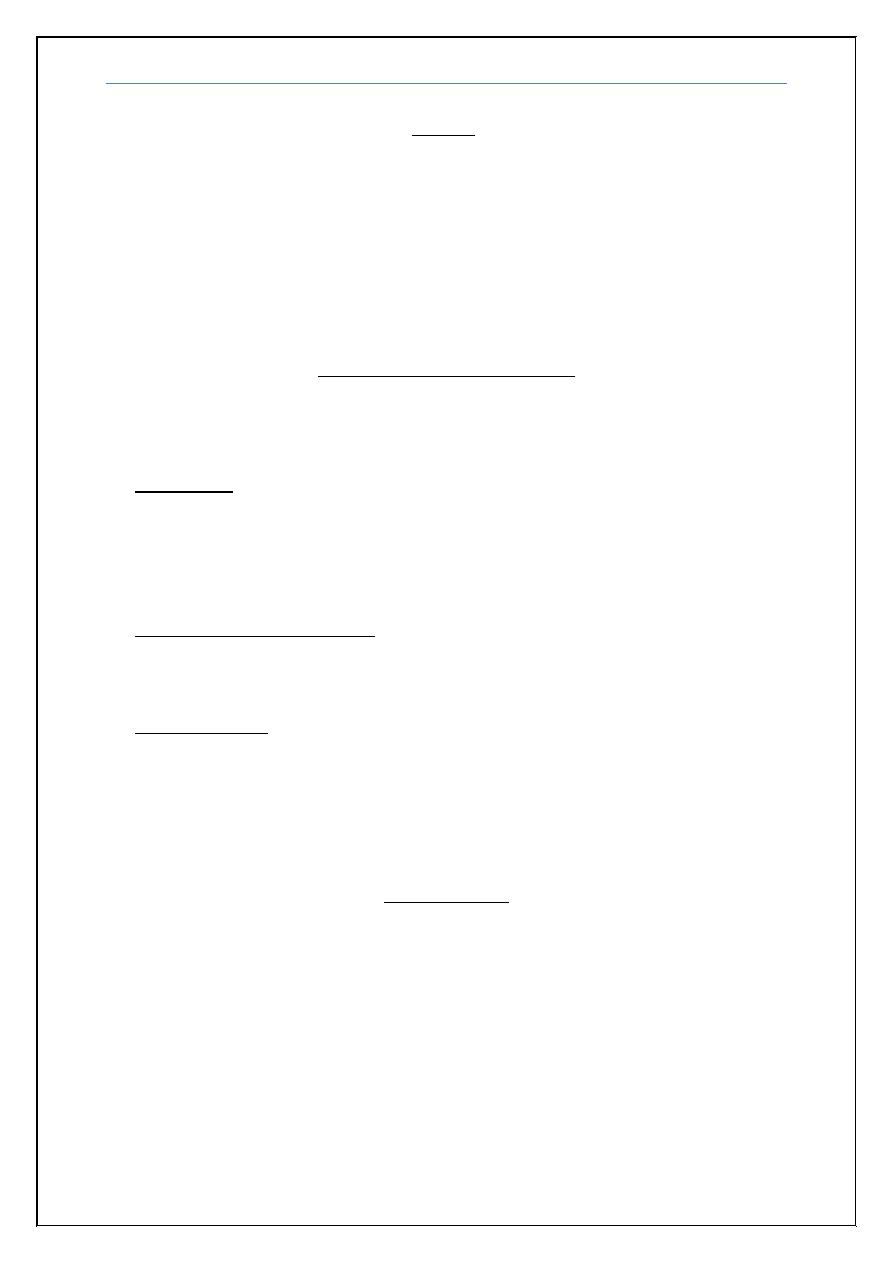
Infratentorial herniation (even small
lesion can cause coma)
5) Upward cerebellar or
upward transtentorial
6) Tonsillar (downward cerebellar or
foraminal) forcing of the cerebellar
tonsils into the foramen magnum
which causes compression of the
medulla and respiratory arrest.
Coma Dr. Zuhair
5
Workup
Is it Coma? How bad it is?
There is a continuum of states of reduced alertness, the severest form being
Coma, which is a state of unconsciousness from which the patient cannot be
aroused, even by powerful stimulation. Stupor refers to a higher degree of
arousability in which the patient can be awakened only by vigorous stimuli,
accompanied by motor behavior that leads to avoidance of uncomfortable or
aggravating stimuli. Drowsiness, which is familiar to all persons, simulates
light sleep and is characterized by easy arousal and the persistence of alertness
for brief periods.
Coma Dr. Zuhair
6
Several other neurologic conditions render patients apparently
unresponsive and thereby simulate coma, and certain subsyndromes of coma
must be considered separately because of their special significance:
Locked in state: a condition in which a patient is aware-cortex is intact-
but cannot move or communicate verbally due to complete paralysis of
nearly all voluntary muscles in the body except for the eyes, usually
caused by caudal brain stem lesion and since the patient cortex is intact
he/she is cognitively intact.
Vegetative state: signifies a state of apparent awakefulness (eyes are
open) but nonresponsive, usually due to widespread lesions of the
cerebral cortex and thalamus. The patient cognitively and emotionally is
impaired.
Minimally conscious state: closely related but less severe then
vegetative state the patient with this state may make intermittent
rudimentary vocal or motor responses.
The severity of the coma can be assessed by glasgow coma scale which will be
disscussed later in the appendix.
Is it metabolic or structural?
Disscussed above.
Is it Supratentorial (Cortex) or Infratentorial (Brainstem)?
This may be assessed on axial images of CT and MRI scans
ABC
Acute respiratory and cardiovascular problems should be attended prior to any
physical or neurological assessment.
I
M
P
O
R
T
A
N
T
Coma Dr. Zuhair
7
History:
In many cases, the cause of coma is immediately evident (e.g., trauma, cardiac
arrest, or known drug ingestion). In the remainder, certain points are especially
useful for identifying the cause:
1) the circumstances and rapidity with which neurologic symptoms developed.
2) the antecedent symptoms (confusion, weakness, headache, fever, seizures,
dizziness, double vision, or vomiting).
3) the use of medications, illicit drugs, or alcohol.
4) chronic liver, kidney, lung, heart, or other medical disease.
General physical examination:
The temperature, pulse, respiratory rate and pattern, and blood pressure
should be measured quickly.
Temprature: Fever suggests a systemic infection, bacterial meningitis, or
encephalitis. While Hypothermia is observed with alcoholic, barbiturate,
sedative, or phenothiazine intoxication; hypoglycemia; peripheral
circulatory failure; or hypothyroidism. Hypothermia itself causes coma only
when the temperature is <31°C.
Respiratory rate and pattern: Tachypnea may indicate systemic acidosis or
pneumonia. Aberrant respiratory patterns that reflect brainstem disorders
are discussed later.
Blood pressure: Marked hypertension either indicates hypertensive
encephalopathy or is the result of a rapid rise in intracranial pressure most
often after cerebral hemorrhage or head injury. Hypotension is characteristic
of coma from alcohol or barbiturate intoxication, internal hemorrhage,
myocardial infarction, sepsis, profound hypothyroidism, or addisonian crisis
Medical exam.
For example funduscopic examination can detect subarachnoid hemorrhage
(subhyaloid hemorrhages), hypertensive encephalopathy (exudates,
hemorrhages, vessel-crossing changes, papilledema), and increased ICP
(papilledema).
Coma Dr. Zuhair
8
Neurological exam.
The goals of neurological exam is:
Functional assessment
Is there structural brain damage?
Supra x Infra tentorial?
Differential diagnosis of Coma?
First by inspection,
Tossing about in the bed, reaching up toward the face, crossing legs, yawning,
swallowing, coughing, or moaning denotes a state close to normal awakeness.
Lack of restless movements on one side or an outturned leg suggests a
hemiplegia. Intermittent twitching movements of a foot, finger, or facial muscle
may be the only sign of seizures.
The terms decorticate rigidity and decerebrate rigidity, describe
stereotyped arm and leg movements occurring spontaneously or elicited by
sensory stimulation. Flexion of the elbows and wrists and supination of the arm
(decortication) suggests bilateral damage rostral to the midbrain, whereas
extension of the elbows and wrists with pronation (decerebration) indicates
damage to motor tracts in the midbrain or caudal diencephalon.
Level of arousal,
Sequence of increasingly intense stimuli is used to determine the threshold for
arousal and the optimal motor response of each side of the body. Tickling the
nostrils with a cotton wisp is a moderate stimulus to arousal, while pressure on
the knuckles or bony prominences and pinprick stimulation are humane forms
of noxious stimuli.
Brain stem reflexes,
Assessment of brainstem function is
essential to localization of the lesion in
coma. The brainstem reflexes that are
conveniently examined are pupillary
responses to light (midbrain function),
spontaneous and elicited eye
movements, corneal responses (pontine
function), and the respiratory pattern
(medullary function) as demonstrated in
the figure.
Coma Dr. Zuhair
9
As a rule, when these brainstem activities are preserved, particularly the
pupil reactions and eye movements, coma must be ascribed to bilateral
hemispheral disease. The converse, however, is not always true, as a mass in the
hemispheres may be the underlying cause of coma but nonetheless produce
brainstem signs by inducing transtentorial herniation.
1) Pupillary Signs (Midbrain function)
Pupillary reactions are examined with a bright, diffuse light:
• Normally reactive and round pupils of midsize (2.5–5 mm) essentially
exclude midbrain damage, either primary or secondary to compression.
•
The most extreme pupillary sign, bilaterally dilated and unreactive
pupils, indicates severe midbrain damage, usually from compression
by a supratentorial mass. (Mydriatic pupil= Midbrain damage)
• Very small but reactive pupils (<1 mm) characterize narcotic or
barbiturate overdoses but also occur with extensive pontine hemorrhage.
(Pinpoint pupil = Pontine Hemorrhage or Morphine)
•
Hutchinson's pupil is a clinical sign in which the pupil on the side of an
intracranial mass lesion (example uncal herniation) is dilated and
unreactive to light, due to compression of the oculomotor nerve on that
side. It has 3 stages:
Stage 1, the parasympathetic fibers on the side of injury are irritated,
leading to constriction of pupil on that side. In stage 2, the parasympathetic fibers on the side of injury
are paralysed, leading to dilatation of pupil. The fibers on the opposite oculomotor nerve are irritated,
leading to constriction on opposite side. In stage 3, the parasympathetic fibers on both sides are
paralysed - leading to bilateral pupillary dilatation.
2) Ocular Movements (Pontine function)
The eyes are first observed by elevating the lids and noting the resting position
and spontaneous movements of the globes. Lid tone, tested by lifting the eyelids
and noting their resistance to opening and the speed of closure, is reduced
progressively as coma deepens.
• Horizontal divergence of the eyes at rest is normal in drowsiness.
As
coma deepens, the ocular axes may become parallel again.
• Conjugate horizontal ocular deviation to one side indicates damage to the
pons on the opposite side or alternatively, to the frontal lobe on the same
side. This phenomenon is summarized by the following maxim: The eyes
look toward a hemispheral lesion and away from a brainstem lesion.
I
M
P
O
R
T
A
N
T

Coma Dr. Zuhair
10
The oculocephalic reflexes depend on the integrity of the ocular motor
nuclei and their interconnecting tracts that extend from the midbrain to the pons
and medulla. These reflexes are elicited by moving the head from side to side or
vertically and observing evoked eye movements in the direction opposite to the
head movement also called doll’s eyes maneuver.
Preservation of evoked reflex eye movements signifies the integrity of the
brainstem and implies that the origin of unconsciousness lies in the cerebral
hemispheres. The opposite, an absence of reflex eye movements, usually
signifies damage within the brainstem but can be produced infrequently by
profound overdoses of certain drugs.
Thermal, or “caloric,” stimulation of the vestibular apparatus
oculovestibular response) provides a more intense stimulus for the
oculocephalic reflex but gives fundamentally the same information. The test is
performed by irrigating the external auditory canal with cool water in order to
induce convection currents in the labyrinths. After a brief latency, the result is
tonic deviation of both eyes to the side of cool-water irrigation and nystagmus
in the opposite direction. (The acronym “COWS” has been used to remind
generations of medical students of the direction of nystagmus— “cold water
opposite, warm water same.”)
The loss of conjugate ocular movements indicates
brainstem damage. The absence of nystagmus despite conjugate deviation of
the globes indicates that the cerebral hemispheres are damaged or
metabolically suppressed.
I
M
P
O
R
T
A
N
T
I
M
P
O
R
T
A
N
T
Coma Dr. Zuhair
11
Corneal reflex, by touching the cornea with a wisp of cotton, a response
consisting of brief bilateral lid closure is normally observed. The corneal
reflexes depend on the integrity of pontine pathways between the fifth (afferent)
and both seventh (efferent) cranial nerves.
Eyelid release test, to test facial nerve, gently pull eyelids up with your
both thumbs and release them simultaneously. The eyelid on hemiplegic side
glide down slowly.
3) Respiratory patterns (medullary function):
(not important
for the exam
)
These are of less localizing value in comparison to other brainstem signs.
Many respiratory patterns have been identified:
Shallow, slow, but regular breathing: metabolic or drug depression.
Cheyne-Stokes (in its classic cyclic form, ending with a brief apneic
period): Supra-tentorial /metabolic
Central neurogenic hyperventilation: Midbrain/pons
Apneustic (short-cycle Cheyne-Stokes): pons/medulla
Ataxic (Biot): medulla
Intermittent: medulla
Motor system exam,
Signs of hemiplegia/ asymmetry
Wrist-dropping test
Arm-dropping test faster drop on site of hemiplegia
Legs-dropping test
Driven postures: Decorticate or Decerebrate (discussed previously.)
Meningeal Irritation Signs.
Neck stiffness: this sign is postive only if there is limitation of forward
flexion which indicates meningism. Stiffness and limitation in more than
one direction usually exclude meningitis as the cause as it may be due to
cervical spondylitis. So examining the head for all types of movments is a
must to differntiate between different causes.
Coma Dr. Zuhair
12
Kernig's sign: positive when the thigh is flexed at the hip and knee at 90
degree angles, and subsequent extension in the knee is painful (leading to
resistance).
Brudzinski's signs: Is the appearance of involuntary lifting of the legs
when lifting a patient's head off the examining couch, with the patient
lying supine
Investigations
The studies that are most useful in the diagnosis of coma are: chemical-
toxicologic analysis of blood and urine, cranial CT or MRI, EEG, and CSF
examination
Management
The immediate goal in a comatose patient is prevention of further nervous
system damage.
Specific: Hypotension, hypoglycemia, hypercalcemia, hypoxia, hypercapnia,
and hyperthermia should be corrected rapidly.
IV access is established, and naloxone and dextrose are administered if
narcotic overdose or hypoglycemia are even remote possibilities.
Thiamine is given along with glucose to avoid provoking Wernicke
disease in malnourished patients.
In cases of suspected basilar thrombosis with brainstem ischemia, IV
heparin or a thrombolytic agent is often utilized, after cerebral
hemorrhage has been excluded by a neuroimaging study.
Physostigmine may awaken patients with anticholinergic-type drug
overdose but should be used only by experienced physicians.
Antibiotics for suspected meningitis
Non specific: Feeding, Positioning, physiotherapy, monitoring, nursing care,
etc…
End
Coma Dr. Zuhair
13
Appendix
:
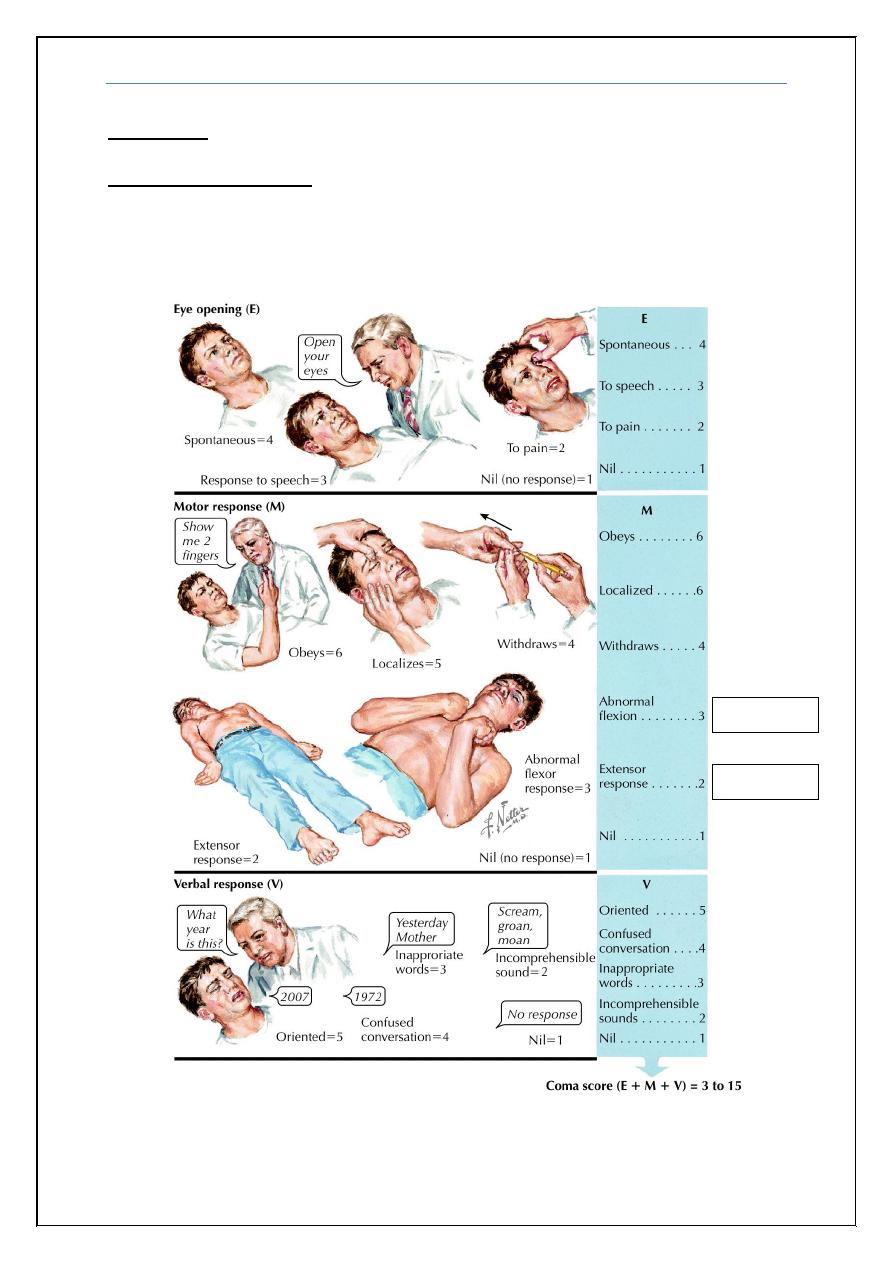
Glasgow coma scale
: is a neurological scale which aims to give a reliable
and objective way of recording the conscious state of a person for initial as well
as subsequent assessment. It consists of 3 elements (Eye opening (E), Verbal
response (V) and Motor response (M)).
Decortication
Decerebration
Coma Dr. Zuhair
14
Case example mentioned by Dr. Zuhair:
1) Female with coma, on exam eye lid release test was positive on the right,
wrist and arm drop test were positive also on the right, brain stem reflexes were
intact.
What do you think the site of the lesion? It is supratentorial (cortical)
Is it unilateral or bilateral? Since it is only to the right this means that it is
unilateral but as we mentioned previously that the cortical causes of coma
should be bilateral and extensive! So we have to think about a unilateral lesion
that is complicated by herniation as an example.
After 6 hours during your re-examination you found pupillary signs, what do
you expect? This proves that the cause was herniation and now it is
compressing the brain stem structures giving pupillary signs.
If the eyelid release positive on one side and leg release test was on the opposite
side, what are the possible sites of the lesion? It is either bilateral supratentorial
or brain stem lesion.
Note:
Lesion in the rostral (upper) brain stem causes coma. (Even a small lesion)
Lesion in the caudal (lower) brain stem causes locked in state.
