DISEASES OF THE SMALL INTESTINE Lec2
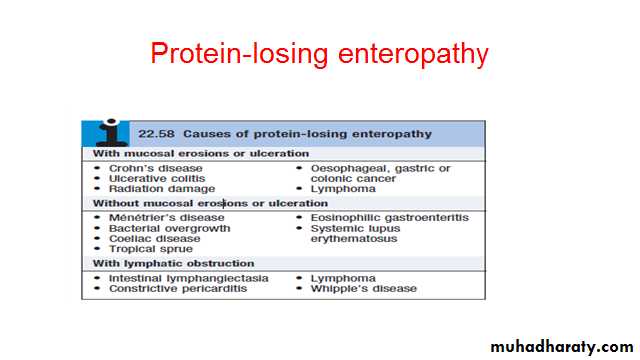
Abdullah AlyouzbakiThe diagnosis can be confirmed by measurement of faecal clearance of α1-antitrypsin or 51Cr-labelled albumin after intravenous injection. Other investigations should be performed to determine the underlying cause.
Treatment is that of the underlying disorder, with nutritional support and measures to control peripheral oedema.
Adverse food reactions
Adverse food reactions are common and are subdivided into food intolerance and food allergy, the former being much more common.In food intolerance, there is an adverse reaction to food which is not immune-mediated and results from pharmacological (histamine, tyramine or monosodium glutamate), metabolic (lactase deficiency)or other mechanisms (toxins or chemical contaminants in food).
Lactose intolerance
In most populations, enterocyte lactase activity declines throughout childhood.In cases of genetically determined (primary) lactase deficiency, jejunal morphology is normal. ‘Secondary’ lactase deficiency occurs as a consequence of disorders which damage the jejunal mucosa, such as coeliac disease and viral gastroenteritis.
Unhydrolysed lactose enters the colon, where bacterial fermentation produces volatile short-chain fatty acids, hydrogen and carbon dioxide.
Clinical features
In most people, lactase deficiency is completely asymptomatic.
However, some complain of colicky pain , abdominal distension, increased flatus, borborygmi and diarrhoea after ingesting milk or milk products.
The lactose hydrogen breath test is a useful non-invasive confirmatory investigation.
Dietary exclusion of lactose is recommended, although most sufferers are able to tolerate small amounts of milk without symptoms.
Addition of commercial lactase preparations to milk has been effective
Food allergy
Food allergies are immune-mediated disorders, most commonly due to type I hypersensitivity reactions with production of IgE antibodies, although type IV delayed hypersensitivity reactions are also seen.The most common culprits are peanuts, milk, eggs, soya and shellfish.
Clinical manifestations occur immediately on exposure and range from trivial to life-threatening or even fatal anaphylaxis
‘gastrointestinal anaphylaxis’ consists of nausea, vomiting, diarrhoea and sometimes cardiovascular and respiratory collapse. Fatal reactions to trace amounts of peanuts are well documented.
The diagnosis of food allergy is difficult .
Skin prick tests.Double-blind placebo-controlled food challenges are the gold standard, but are laborious and are not readily available. In many cases, clinical suspicion and trials of elimination diets are used.
Treatment of proven food allergy consists of detailed patient education and awareness, strict elimination of the offending antigen.
Anaphylaxis should be treated as a medical emergency with resuscitation, airway support and intravenous adrenaline (epinephrine).
INFLAMMATORY BOWEL DISEASE IBD
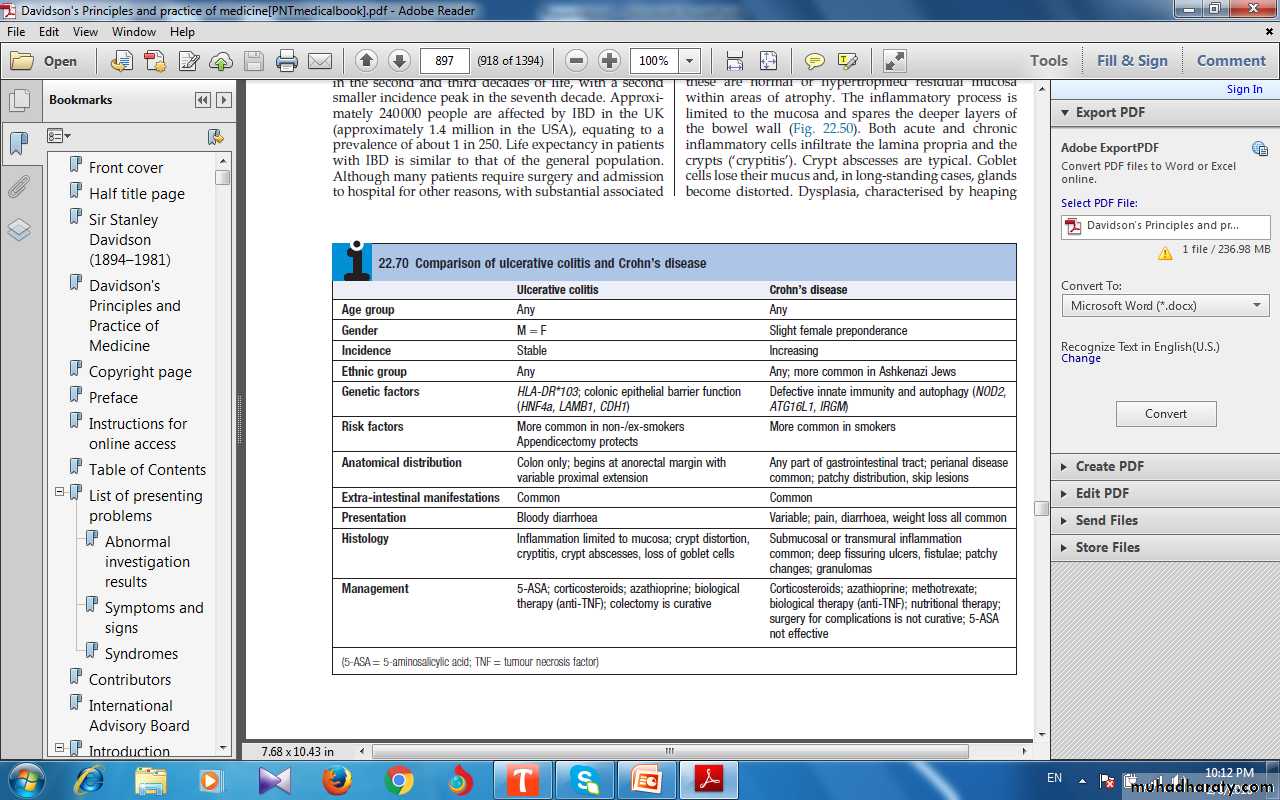
Ulcerative colitis and Crohn’s disease are chronic inflammatory bowel diseases which have a protracted relapsing and remitting course, usually extending over years.
The diseases have many similarities and it is sometimes impossible to differentiate between them.
INFLAMMATORY BOWEL DISEASE
Both diseases most commonly start in the second and third decades of life, with a second smaller incidence peak in the seventh decade.Life expectancy in patients with IBD is similar to that of the general population.
Pathophysiology of IBD
Genetic• Both CD and UC common in Ashkenazi Jews
• 10% have first-degree relative/≥1 close relative with IBD
• High concordance in identical twins (40–50% CD; 20–25% UC)
IBD associated with other inflammatory conditions (esp. ankylosing spondylosis and psoriasis)
Environmental
• UC more common in non-smokers and ex-smokers• CD more common in smokers (relative risk = 3)
• CD associated with low-residue, high-refined-sugar diet
• Commensal gut microbiota altered (dysbiosis) in CD and UC
• Appendicectomy protects against UC
Ulcerative colitis
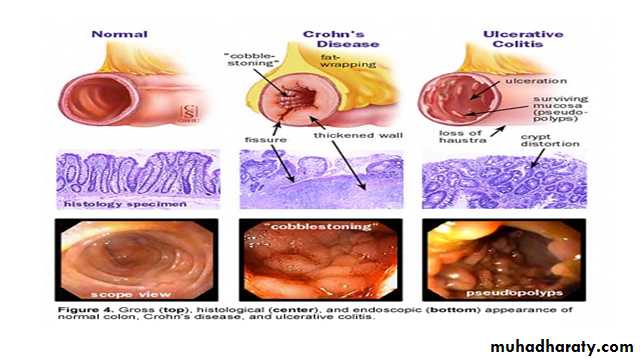
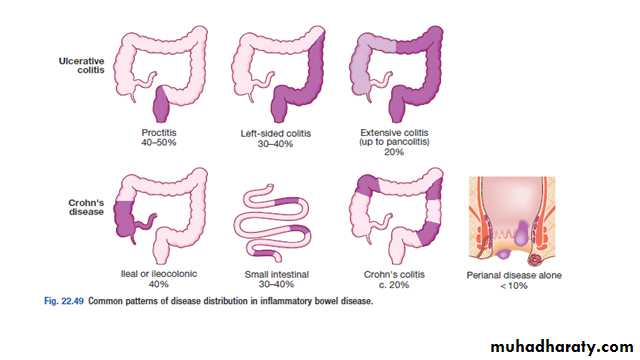
Inflammation invariably involves the rectum (proctitis) and spreads proximally in a continuous manner to involve the entire colon in some cases (pancolitis).
In long-standing pancolitis, the bowel can become shortened and post-inflammatory ‘pseudopolyps’ develop; these are normal or hypertrophied residual mucosa within areas of atrophy.
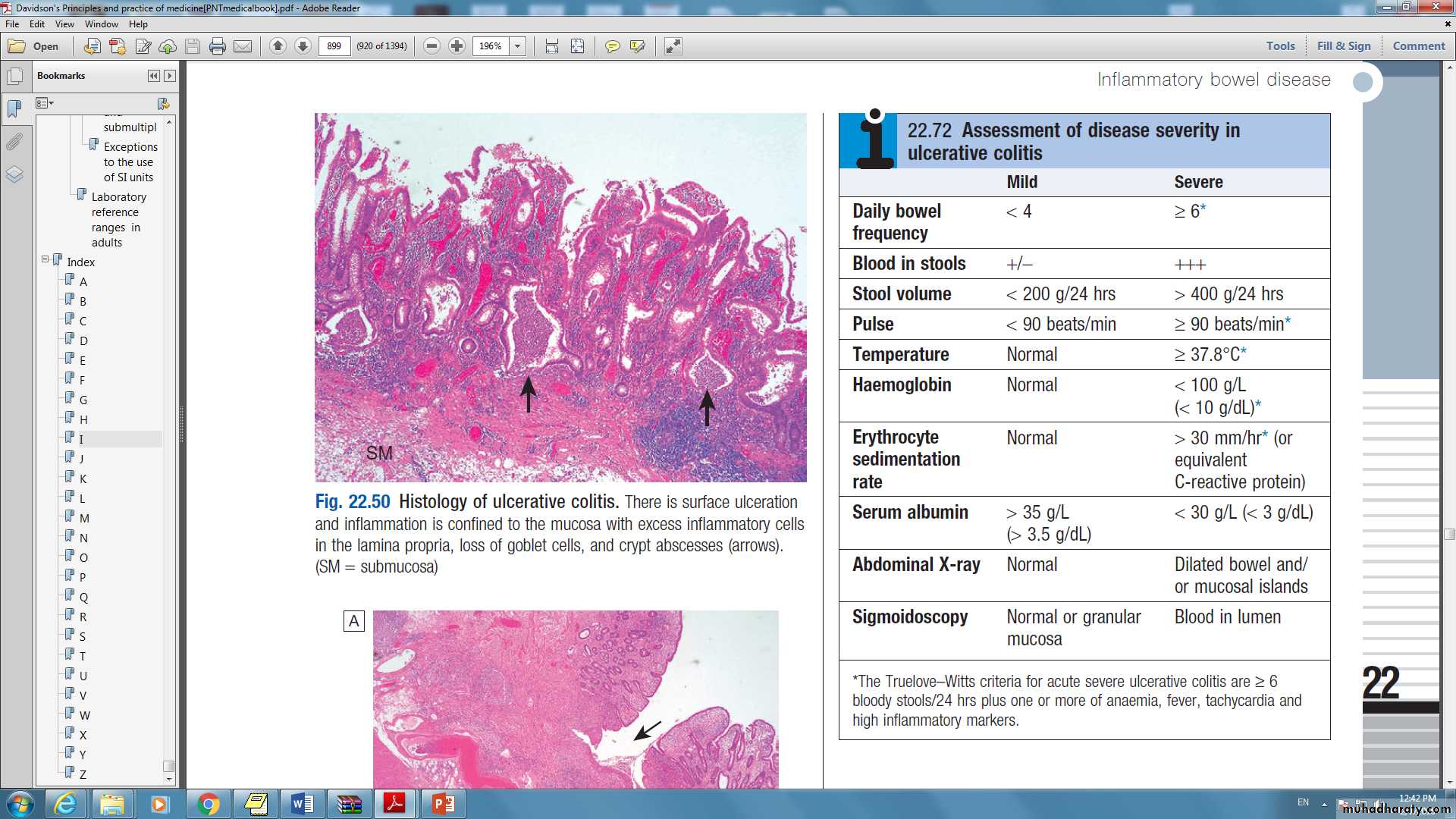
The inflammatory process is limited to the mucosa and spares the deeper layers of the bowel wall (Fig. 22.50).
Both acute and chronic inflammatory cells infiltrate the lamina propria and the crypts (‘cryptitis’). Crypt abscesses are typical.
Crohn’s disease
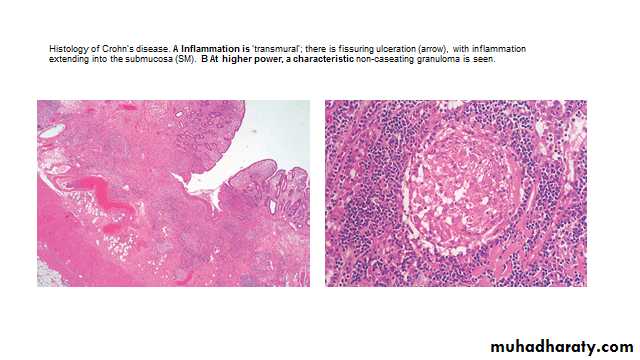
The sites most commonly involved are, in order of frequency, the terminal ileum and right side of colon, colon alone, terminal ileum alone, ileum and jejunum.The entire wall of the bowel is edematous and thickened, and there are deep ulcers which often appear as linear fissures; thus the mucosa between them is described as ‘cobblestone’.
These may penetrate through the bowel wall to initiate abscesses or fistulae involving the bowel, bladder, uterus, vagina and skin of the perineum.
mesenteric lymph nodes are enlarged and the mesentery is thickened.
Crohn’s disease has a patchy distribution and the inflammatory process is interrupted by islands of normal mucosa.
On histological examination, the bowel wall is thickened with a chronic inflammatory infiltrate throughout all layers.
Clinical features of IBD:Ulcerative colitis
The cardinal symptoms are rectal bleeding with passage of mucus and bloody diarrhoea. The presentation varies, depending on the site and severity of the disease , as well as the presence of extra-intestinal manifestations.The first attack is usually the most severe and is followed by relapses and remissions.
Emotional stress, intercurrent infection, gastroenteritis, antibiotics or NSAID therapy may all provoke a relapse.
Proctitis causes rectal bleeding and mucus discharge, accompanied by tenesmus. Some patients pass frequent, small volume fluid stools, while others pass pellety stools. Constitutional symptoms do not occur.
Left-sided and extensive colitis causes bloody diarrhoea with mucus, often with abdominal cramps. In severe cases, anorexia,malaise, weight loss and abdominal pain occur, and the patient is toxic, with fever, tachycardia and signs of peritoneal inflammation.
Clinical features of IBD:Crohn’s disease
The major symptoms are abdominal pain, diarrhoea and weight loss. Ileal Crohn’s disease may cause sub acute or even acute intestinal obstruction.
The pain is often associated with diarrhoea, which is usually watery and does not contain blood or mucus.
Almost all patients lose weight because they avoid food, since eating provokes pain. Weight loss may also be due to malabsorption, and some patients present with features of fat, protein or vitamin deficiencies.
Crohn’s colitis presents in an identical manner to ulcerative colitis, but rectal sparing and the presence of perianal disease are features which favour a diagnosis of Crohn’s disease.
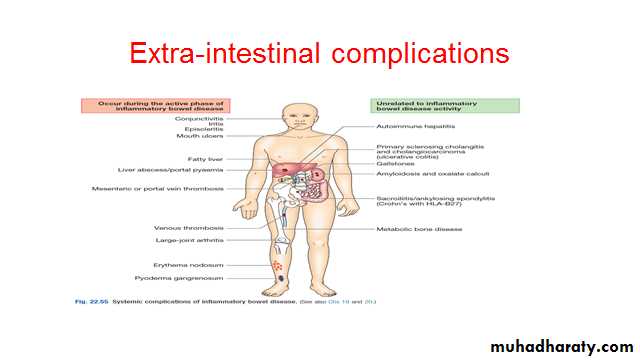
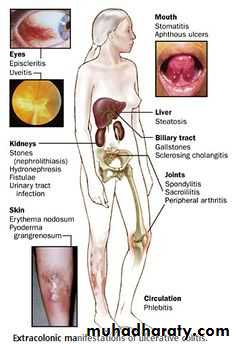
Complications of IBD
Life-threatening colonic inflammation:This can occur in both ulcerative colitis and Crohn’s colitis. In the most extreme cases, the colon dilates (toxic megacolon) and bacterial toxins pass freely across the diseased mucosa into the portal and then systemic circulation.
An abdominal X-ray should be taken daily because, when the transverse colon is dilated to more than 6 cm, there is a high risk of colonic perforation.
Haemorrhage:
Haemorrhage due to erosion of a major artery is rare but can occur in both conditions.Fistulae:
These are specific to Crohn’s disease. Enteroenteric fistulae can cause diarrhoea and malabsorption due to blind loop syndrome. Enterovesical fistulation causes recurrent urinary infections and pneumaturia. An enterovaginal fistula causes a faeculent vaginal discharge. Fistulation from the bowel may also cause perianal or ischiorectal abscesses, fissures and fistulae.
Cancer
The risk of dysplasia and cancer increases with the duration and extent of uncontrolled colonic inflammation.
The risk is particularly high inpatients who have concomitant primary sclerosing cholangitis for unknown reasons. Tumors develop in areas of dysplasia and may be multiple. Patients with long-standing colitis are therefore entered into surveillance programs beginning 10 years after diagnosis.
If high-grade dysplasia is found, panproctocolectomy is usually recommended because of the high risk of colon cancer.
Investigations
Investigations are necessary to confirm the diagnosis, define disease distribution and activity, and identify complications.Full blood count may show anaemia resulting from bleeding or malabsorption of iron, folic acid or vitamin B12.
Serum albumin concentration falls as a consequence of protein-losing enteropathy, inflammatory disease or poor nutrition.
The ESR and CRP are elevated in exacerbations and in response to abscess formation.
Faecal calproctectin has a high sensitivity for detecting gastrointestinal inflammation and may be elevated, even when the CRP is normal. It is particularly useful in distinguishing inflammatory bowel disease from irritable bowel syndrome at diagnosis, and for subsequent monitoring of disease activity.
Bacteriology: stool microscopy, culture and examination for Clostridium difficile toxin or for ova and cysts, blood cultures and serological tests should be performed.
Investigations: Endoscopy
Patients who present with diarrhoea plus raised inflammatory markers or alarm features, such as weight loss, rectal bleeding and anaemia, should undergo ileocolonoscopy.
Flexible sigmoidoscopy is occasionally performed to make a diagnosis, especially during acute severe presentations when ileocolonoscopy may confer an unacceptable risk.
In ulcerative colitis, there is loss of vascular pattern, granularity, friability and contact bleeding, with or without ulceration.
In Crohn’s disease, patchy inflammation, with discrete, deep ulcers, strictures and perianal disease (fissures, fistulae and skin tags), is typically observed, often with rectal sparing.
In Crohn’s disease, wireless capsule endoscopy ,enteroscopy may be required.
All children and most adults with Crohn’s disease should have upper gastrointestinal endoscopyInvestigations: Radiology
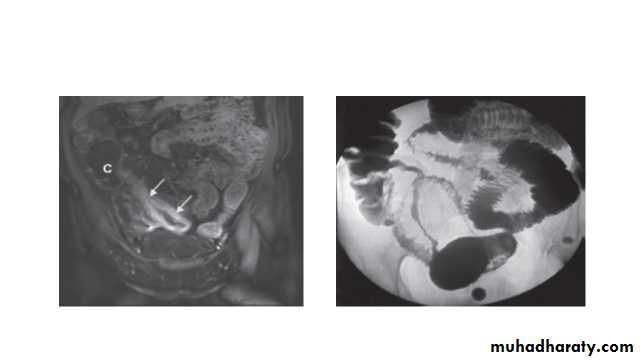
Barium enema is a less sensitive investigation than colonoscopy in patients with colitis and, where colonoscopy is incomplete, a CT colonogram is preferred.Small bowel imaging is essential to complete staging of Crohn’s disease. Traditional contrast imaging by barium follow-through demonstrates affected areas of the bowel as narrowed and ulcerated, often with multiple strictures. This has now largely been replaced by MRI enterography, which is a sensitive way of detecting extra intestinal manifestations and of assessing pelvic and perineal involvement.
A plain abdominal X-ray is essential in the management of patients who present with severe active disease. Dilatation of the colon , mucosal edema (thumb-printing) or evidence of perforation may be found.
Management of IBD
Although medical therapy plays an important role, optimal management depends on establishing a multidisciplinary team-based approach involving physicians, surgeons, radiologists, nurse specialists and dietitians.The key aims of medical therapy are to:
• treat acute attacks (induce remission)
• prevent relapses (maintain remission)
•prevent bowel damage
• detect dysplasia and prevent carcinoma
• select appropriate patients for surgery.