SURGERY
Anaesthesia
DR. SABAH
AFTER MID
TOTAL LEC: 2 LEC:1
Dr. Sabah
Pre-Operative
preparation

Page
3
of 10
Anaesthesia
P
REOPERATIVE PREPARATION
Introduction:
A
IMS OF THE PREOPERATIVE VISIT
1. To ensure that the patient is presented for theatre in an optimum state.
2. It offers an opportunity to discuss the anaesthetic technique with the
patient.
3. To minimize the patient anxieties.
4. To prescribe premedication
P
ATIENT
A
SSESSMENT
:
I.
Cardiovascular System:
1. Coronary Artery Disease:
The role of exercise tolerance
The role of Cardio-Pulmonary Exercise Test (CPET)
Stable Angina
Unstable Angina
Previous Myocardial Infarction
د
.
صباح نوري السعد
M.B.Ch.B, D.A,
F.I.M.S, C.A.B.A & I.C
Lecture: 1

Page
4
of 10
2. Cardiac Failure:
Careful assessment especially if the patient has basal crepitations or
Gallop rhythm.
3. Arrhythmias:
History of palpitation or stokes-Adams attacks
Infrequent ectopics are rarely significant unless associated with
electrolytes imbalance, or thyroid disease.
Usually diagnosed accurately by ECG.
Certain arrhythmia requires control or correction before operation, e.g.
rapid atrial fibrillation (AF), or 2
nd
and 3
rd
degree heart block.
4. Hypertension: Hypertension should be treated before operation:
Patients who have their diastolic blood pressure persistently exceeds
110 mmHg require control before operation.
Mild-moderate hypertension require control if hypertension is
associated with end-organ damage.
Hypertensive patient on treatment but still their hypertension not
adequately controlled.
All antihypertensive medications should be continued up to including
the day of surgery.
II. Respiratory System:
1.
Upper Airway: Lips – Trachea
Mouth Opening
Presence of diseased teeth or dentures
Cervical spine mobility
Thyro-mental distance
2. Chronic Obstructive Airway Disease (including Asthma)

Page
5
of 10
Severity of the disease can be assessed by: exercise tolerance, current
medication, frequency of hospital admission.
Physical signs such as cyanosis and wheezes are important in more
severe disease
Chest X-Ray although routinely taken but rarely helps.
Pulmonary Function Test (PFT) is usually performed, Peak Expiratory
Flow Rate (PEFR).
Patient with severe disease requires early admission.
Local and Regional Anaesthesia is preferred.
3. Upper and lower respiratory tract infections
Elective surgery should be delayed; otherwise life-threatening respiratory
tract infection may develop post-operatively.
III. Endocrine Diseases:
1. Diabetes Mellitus:
Usually they have cardiovascular and renal diseases.
The most common practical problem is the management of diabetes
mellitus during inevitable period of starvation
Random Blood Sugar (RBS) below 15 mmol/L is acceptable
General principles of management under General Anaesthesia:
1. Hypoglycaemia must be avoided
2. Regular measurements of random blood sugar is important
3. Insulin-Dependent diabetics require insulin even during starvation
and they require more insulin than usual.
4. Non-Insulin-Dependent diabetics may require insulin for a brief
period.
Page
6
of 10
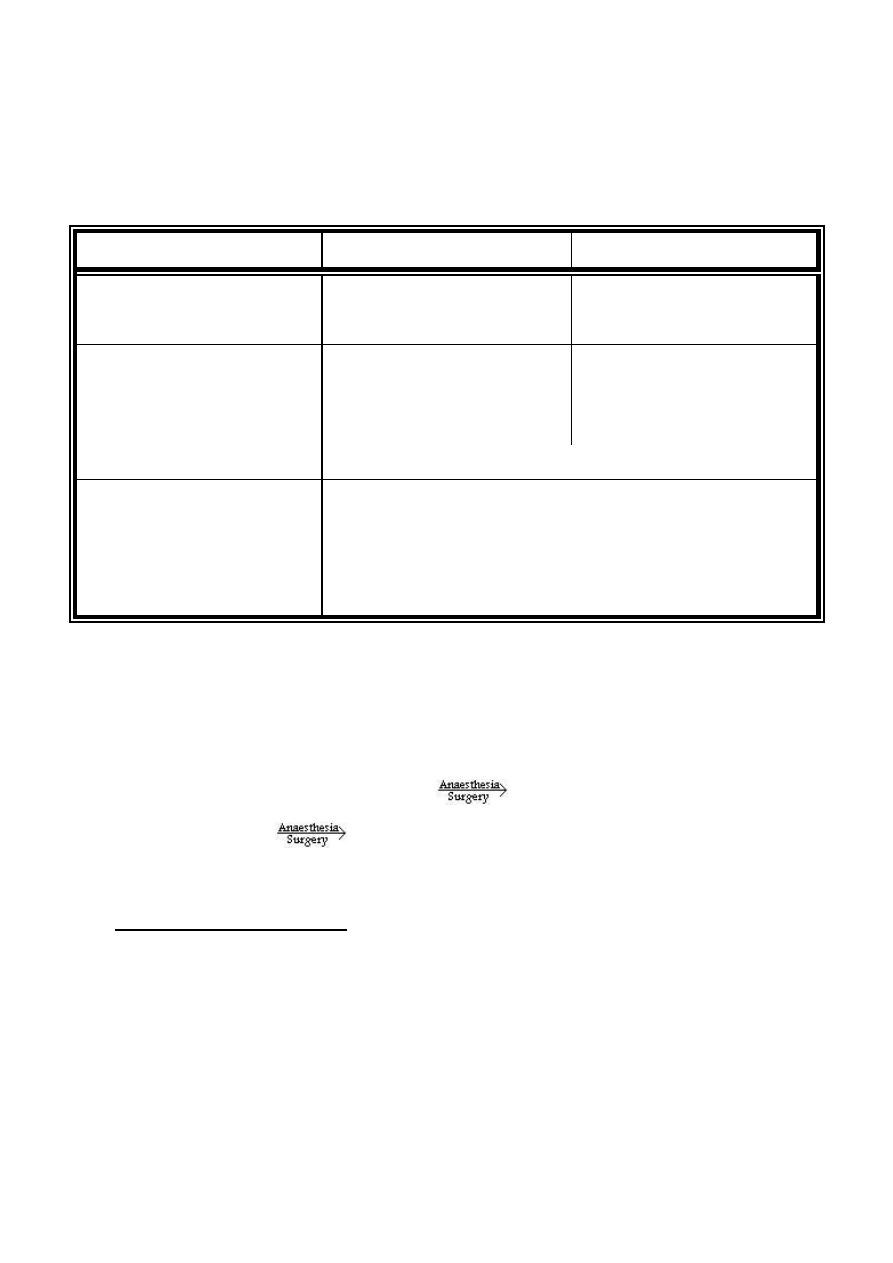
A suggested scheme for management of diabetic patient undergoing elective
surgery:
Type of Diabetes
Minor Surgery
Major Surgery
1. Diet controlled
Measure blood sugar
Rarely require treatment
Measure blood sugar
Rarely require insulin
2. Oral treatment
Measure blood sugar
Omit treatment 12-24 hours
before operation
Measure blood sugar
Omit treatment 12-24 hours
before operation
Both groups may require insulin after operation
3. Insulin-dependent
For both operation:
measure blood sugar
insulin (injection or infusion) + 5% dextrose infusion
(together or separately)
2. Thyroid Disease:
Patient with thyroid disease should have Thyroid Function Test before
elective surgery.
Uncontrolled hyperthyroidism
Thyroid Crises
Myxoedema
Delayed Recovery and Heart Failure
Clinical judgement and high index of suspicion is important.
IV. Neuromuscular System:
1. Epilepsy:
Avoid anaesthetic drugs which are suspected of being epileptogenic
(Ketamine)
Continue anticonvulsant medications including the day of surgery, and
as soon as possible post-operatively.
Page
7
of 10
راجعو شوية شكلكم ممضبطيها المحاظرة:D
2. Lower Motor Neuron disease:
Altered response to suxamethonium → hyperkalemia
3. Myasthenia Gravis:
assessment of severity
Highly sensitive to non-depolarizing muscle relaxants
Planning for post-operative intensive care unit (ICU) admission and
possibly mechanical ventilation.
4. Malignant Hyperthermia:
Runs in families
Hypermetabolic stat of skeletal muscles is triggered
hyperthermia and electrolyte imbalance.
5. Stroke:
There is no post-stroke “Risk Period”
It makes sense not to undertake elective surgery during recovery from
stroke
Good control of hypertension
V. Genito-urinary System:
1. Renal Failure:
The pathophysiology of Renal Failure whether acute or chronic is
complex
Chronic renal failure:
o Hypertension, cardiomyopathy, pericardial effusion
o Anaemia and platelet dysfunction
Page
8
of 10
o Impaired Blood-Brain barrier (highly sensitive to opioid analgesics
especially Morphine).
o Fluid and Electrolyte imbalance
o Dialysis may be required before operation.
2. Pregnancy
Elective surgery is contraindicated
Early pregnancy → Teratogencity of anaesthetics
Late pregnancy → Premature labour
VI. Haematological System:
1. Anaemia: Lowest Hemoglobin for elective surgery is 10 mg/dL except
chronic renal failure patients.
2. Clotting Disorders: chronic liver disease, primary haematological
disease, or drug (warfarin)
VII. Concurrent drug treatment: these might interact with anaesthetic drugs;
D
RUG
E
FFECT
A. Cardiovascular system:
1. Potent
antihyperensives,
e.g. β-
Blockers, ACE Inhibitors
→ Enhance hypotensive effect of general
anaesthesia or spinal anaesthesia
2. Antiarrhythmics,
e.g.
Digoxin,
amiodarone
→ Increased risk of bradycardia ± significant
myocardial depression, digoxin may cause
significant arrhythmia
3. Diuretics, e.g. thiazide, spironolactone → Dehydration ± electrolyte imbalance
4. Anticoagulant, e.g. warfarin
→ Major regional block contraindicated
B. Respiratory system:
Bronchodilators, e.g. Aminophylline
→ Increased likelihood of arrhythmia
C. Central Nervous System:
1. Sedative and hypnotics
→Chronic use induce tolerance to general
anaesthesia
Page
9
of 10
2. Monoamine Oxidase
→ Interact with sympathomimetic
(ephedrine), and pethidine to cause
hypertension and tachycardia → Fatal
3. Antiparkinson drugs
→ Levodopa increase risk of arrhythmia
4. Antiepileptics
→ Increase tolerance to general anaesthesia
D. Drug of abuse
1. Tobacco
→ Reduce O
2
carriage capacity by
formation
of
Carboxyhemoglobin
(COHb)
Major Factor in chronic obstructive
airway disease
May induce tolerance to general
anaesthetics
2. Alcohol
→ Tolerance to anaesthetics
Chronic use may cause cirrhosis and
cardiomyopathy
3. Intravenous drug abuse
→ Tolerance to effects of opioids
Risk of hepatitis and AIDS
May have difficult veins
E. Steroids: glucocorticoids
→ currently or in the previous 6 months
cause adrenocortical suppression
F. Oral Contraceptive Pills (OCP)
1. Oestrogen-containing OCP
→ Deep venous Thrombosis and pulmonary
embolism
N.B: Should be stopped 1 month before
elective operation
2. Progesterone-only OCP
→ No effect
G. Aspirin and Clopidogrel (Plavix)
→ Platelet dysfunction, better to be stopped
at least 1 week before elective operation.
In coronary stenting better not to stop
clopidogrel

Page
10
of 10
Thank you
Done by: Hussein Sadun Al-Nuaimy
