د
.
محمد حنون
y
Nephrolog
lec 2
1
Nephrology
Imaging techniques
Total : 2
Lec : 2
د
.
محمد حنون
y
Nephrolog
lec 2
2
د
.
محمد حنون
y
Nephrolog
lec 2
3
Imaging Techniques
Plain X-rays
:-
- renal outlines
opaque calculi
calcification within the renal tract.
Ultrasound
:-
This quick, non-invasive is the first and often the only.
renal size and position,
detect dilatation of the collecting system ( obstruction)
distinguish tumours and cysts.
the prostate and bladder, and estimate completeness of emptying
other abdominal, pelvic and retroperitoneal pathology.
In CKD ,U/S density (echogenicity) of the renal cortex is increased and
cortico-medullary differentiation is lost.
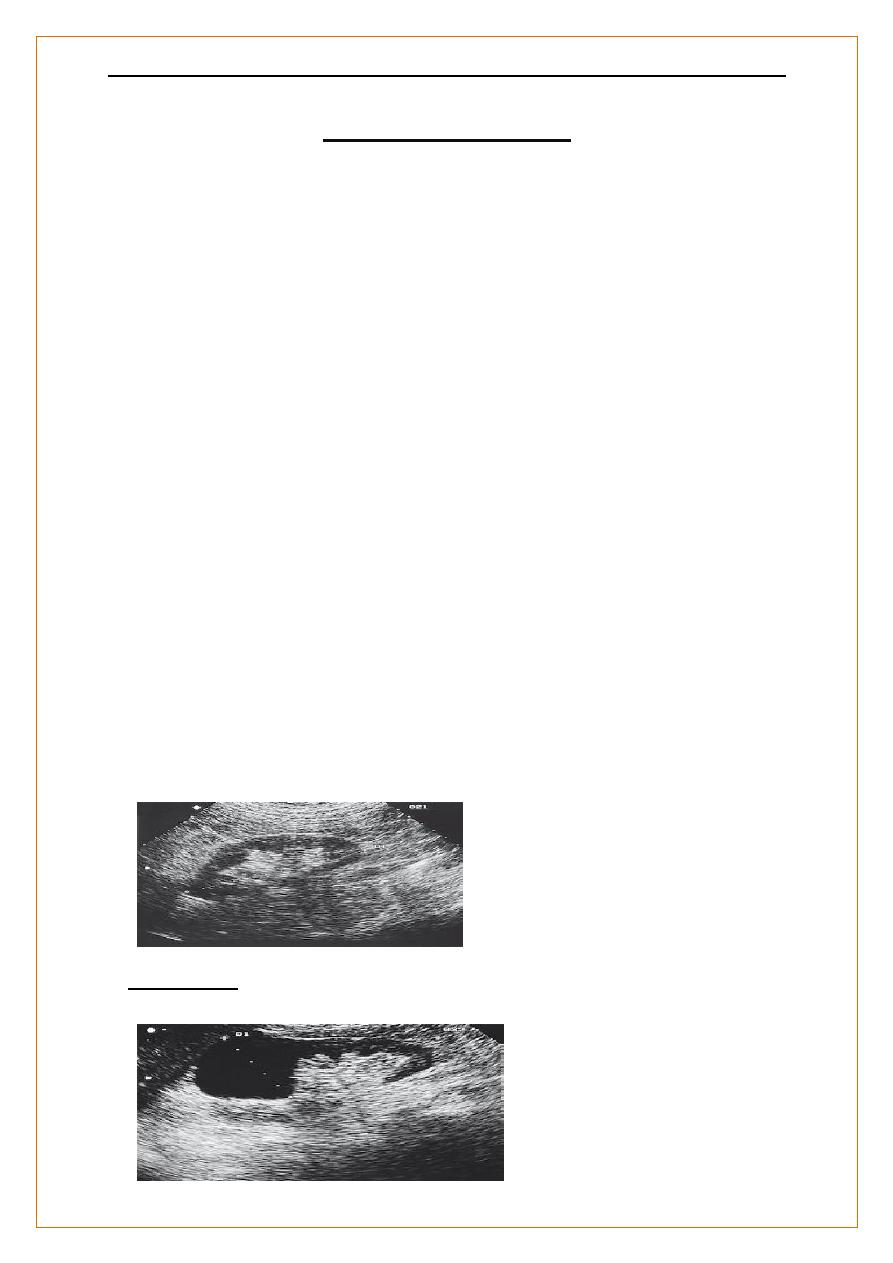
Normal kidney. The normal cortex is less echo-dense (blacker) than the
adjacent liver.
A simple cyst occupies the
upper pole of an otherwise normal kidney.
د
.
محمد حنون
y
Nephrolog
lec 2
4
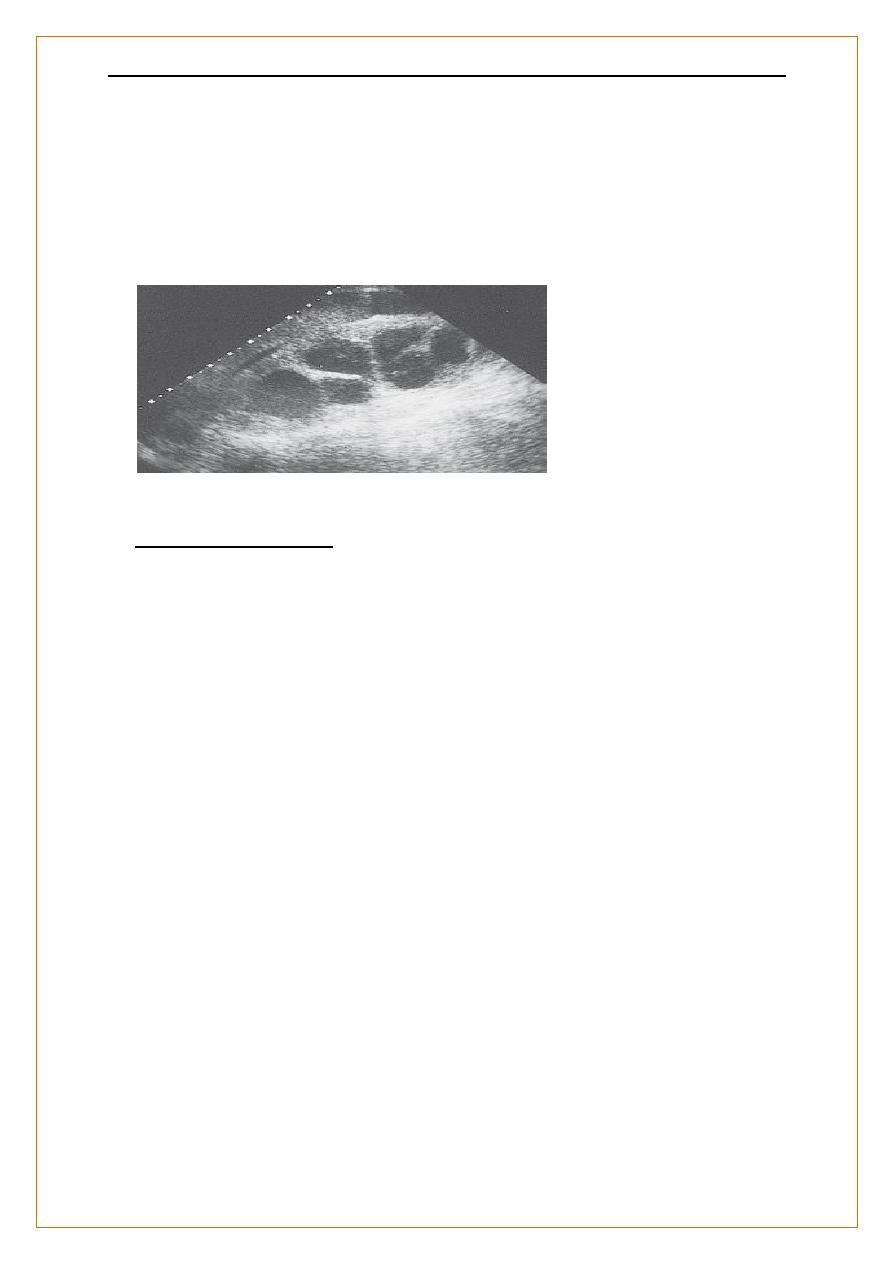
The renal pelvis and calyces are dilated by a chronic obstructionto urinary
outflow.
The thinness and increased density of the remaining renal cortex indicate
chronic changes
Imaging Techniques
Doppler techniques
show blood flow in extrarenal & larger intrarenal vessels.
-The resistivity index
is the ratio of peak systolic and diastolic velocities, and is influenced by the
resistance to flow through small intrarenal arteries. may be elevated in
various diseases,
acute glomerulonephritis
rejection of a renal transplant. High peak velocities
severe renal artery stenosis.
However, renal ultrasound is;-
operator-dependent,
stored images convey only a fraction of the information
it is often less clearin obese patients
د
.
محمد حنون
y
Nephrolog
lec 2
5
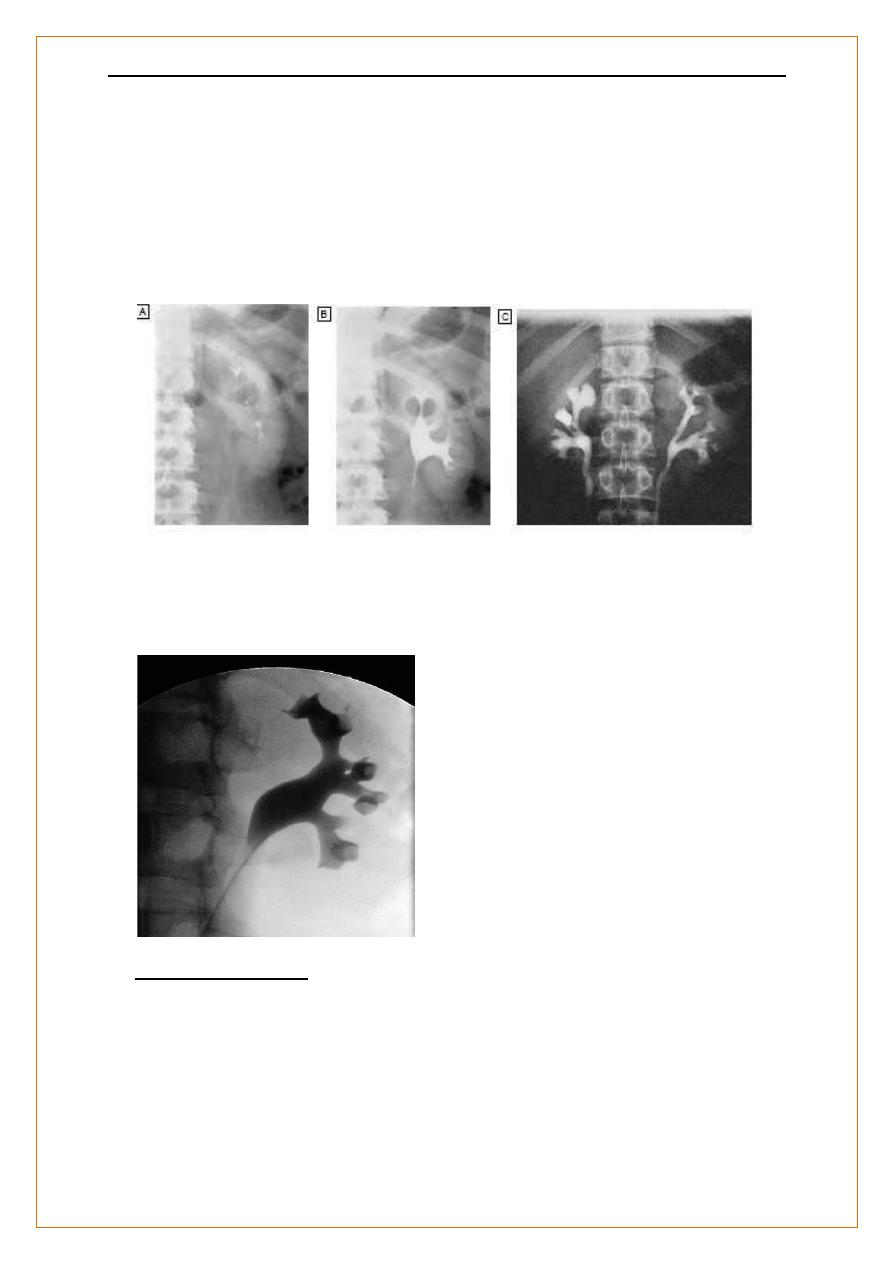
Intravenous urography (IVU)
:-
X-rays taken at intervals following administration of an IV bolus of an
iodine-containing compound that is excreted by the kidney.
An early image (1 minute after injection) demonstrates the nephrogram
phase of renal perfusion
followed by contrast filling the collecting system, ureters& bladder. An
excellent definition of the collecting system and ureters,
Superior to U/S for examining renal papillae, stones & urothelial malignancy
The disadvantages of this technique are the injection of a contrast medium,
exposure to irradiation , time requirement, dependence on adequate renal
function,
Pyelography
direct injection of contrast medium into the collecting system from above
or below.
best views of the collecting system and upper tract,
used to identify the cause of urinary tract obstruction).
Antegrade pyelography
requires the insertion of a fine needle into the pelvicalyceal system under
ultrasound or radiographic control.
difficult and hazardous in a non-obstructed kidney. In the presence of
obstruction, percutaneous nephrostomy drainage can be established, and
often stents can be passed through any obstruction.
Retrograde pyelography
can be performed by inserting catheters into the ureteric orifices at
cystoscopy.
د
.
محمد حنون
y
Nephrolog
lec 2
6
Intravenous urography (IVU).
A Normal nephrogram phase at 1 minute.
B Normal collecting system at 5 minutes.
C Bilateral reflux
Retrograde pyelography.. A catheter has been passed into the left renal
pelvis at cystoscopy.
The anemone-like calyces are sharp-edged and normal
Imaging Techniques
Renal arteriography and venography
to investigate suspected renal artery stenosis or haemorrhage.
Therapeutic balloon dilatation and stenting of the renal artery bleeding
vessels or arteriovenous fistulae occluded.
د
.
محمد حنون
y
Nephrolog
lec 2
7
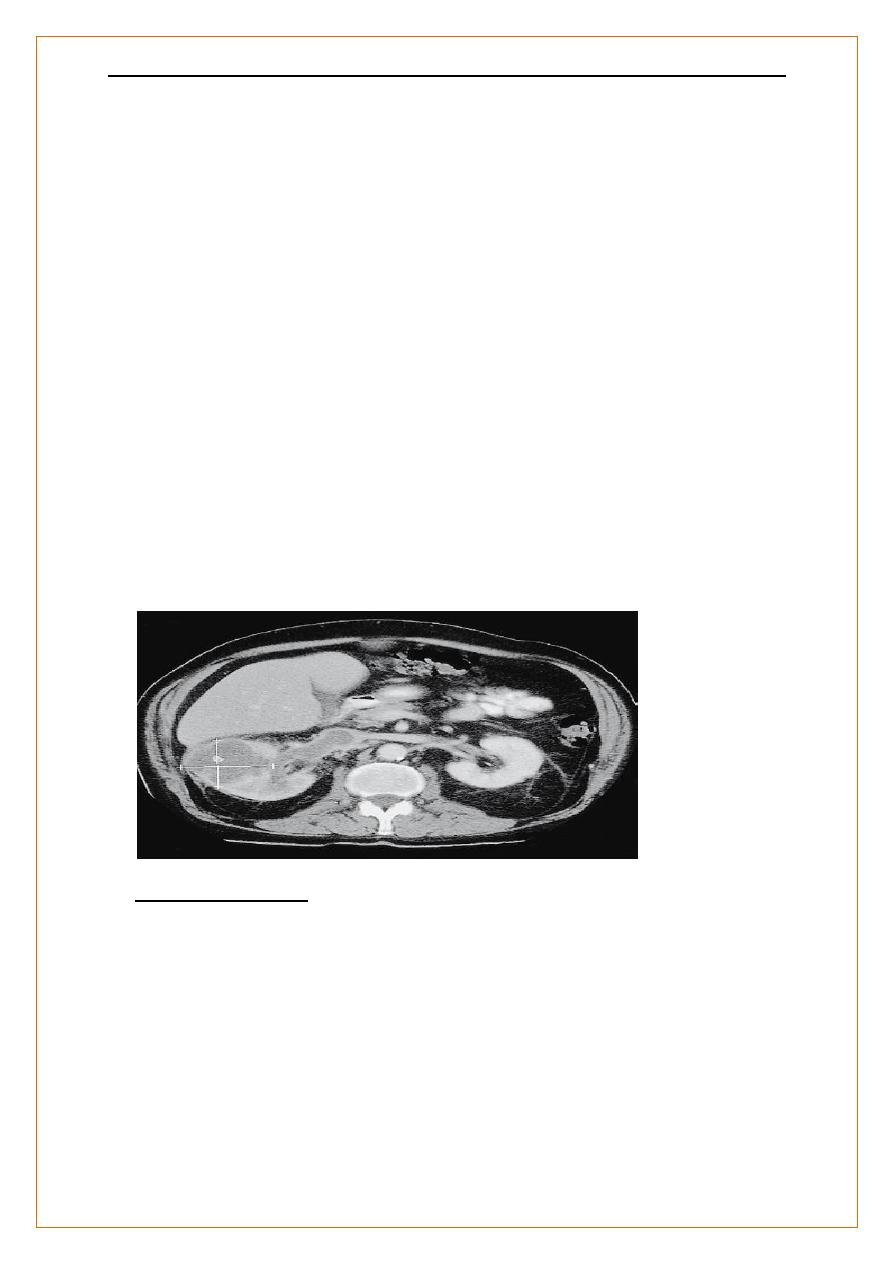
Computed tomography (CT)
characterizing masses & cystic lesions within the kidney
clear definition of retroperitoneal anatomy regardless of obesity.
Even without contrast medium it is better than IVU for demonstrating renal
stones.
In CT urography, after a first scan without contrast, scans are repeated
during nephrogram and excretory phases. This gives more information but
entails a substantially larger radiation
dose than IVU
CT, the Rt kidney is expanded by a low-density tumour which fails to take
up contrast material. Tumour is shown extending into the renal vein and
inferior vena cava .
Imaging Techniques
CT arteriograms
are reconstructed using a rapid sequence technique in which images are
obtained immediately following a large bolus injection of
intravenouscontrast medium.
This produces high-quality images of the main renal vessels and is of value
in trauma, renal haemorrhage and the investigation of possible renal artery
stenosis.
د
.
محمد حنون
y
Nephrolog
lec 2
8
enables functional assessment of vascular structures, e.g.
angiomyolipomas.
However, relatively large doses of contrast are required
Imaging Techniques
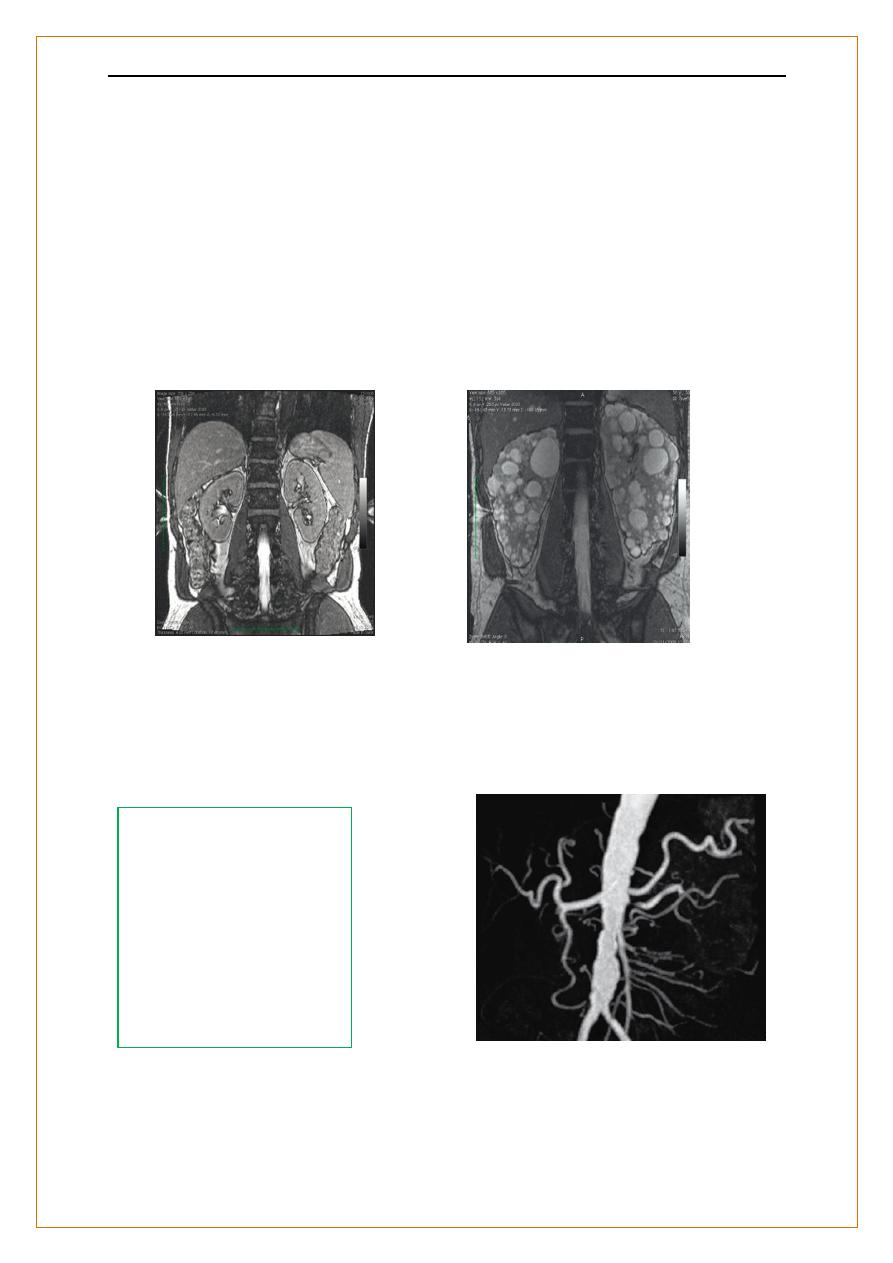
Magnetic resonance imaging (MRI)
excellent resolution and distinction between different tissues
.
B Polycystic kidney
Magnetic resonanceangiography (MRA)
uses gadolinium-based contrast media, which may carry risks for patients
with very low GFR . good images of main renal vessels but may miss branch
artery stenosis
Renal artery stenosis. MRA
following injection of
contrast.
The abdominal aorta is
severely irregular and
atheromatous
.
The left renal artery is
stenosed
Normal kidney
د
.
محمد حنون
y
Nephrolog
lec 2
9
Radionuclide studie:-
-
A functional studies requiring the injection of gamma ray-emitting
radiopharmaceuticals which are taken up and excreted by the kidney,
monitored by an external gamma camera.
(99mTc-DTPA) Diethylenetriamine-pentaacetic acid labelled with
technetium is excreted by glomerular filtration.
provides information regarding the arterial perfusion of each kidne
Delayed peak activity and reduced excretion is seen in RAS.
In patients with significant obstruction of the outflow tract, DTPA persists in
the renal pelvis, and a loop diuretic fails to accelerate its disappearance.
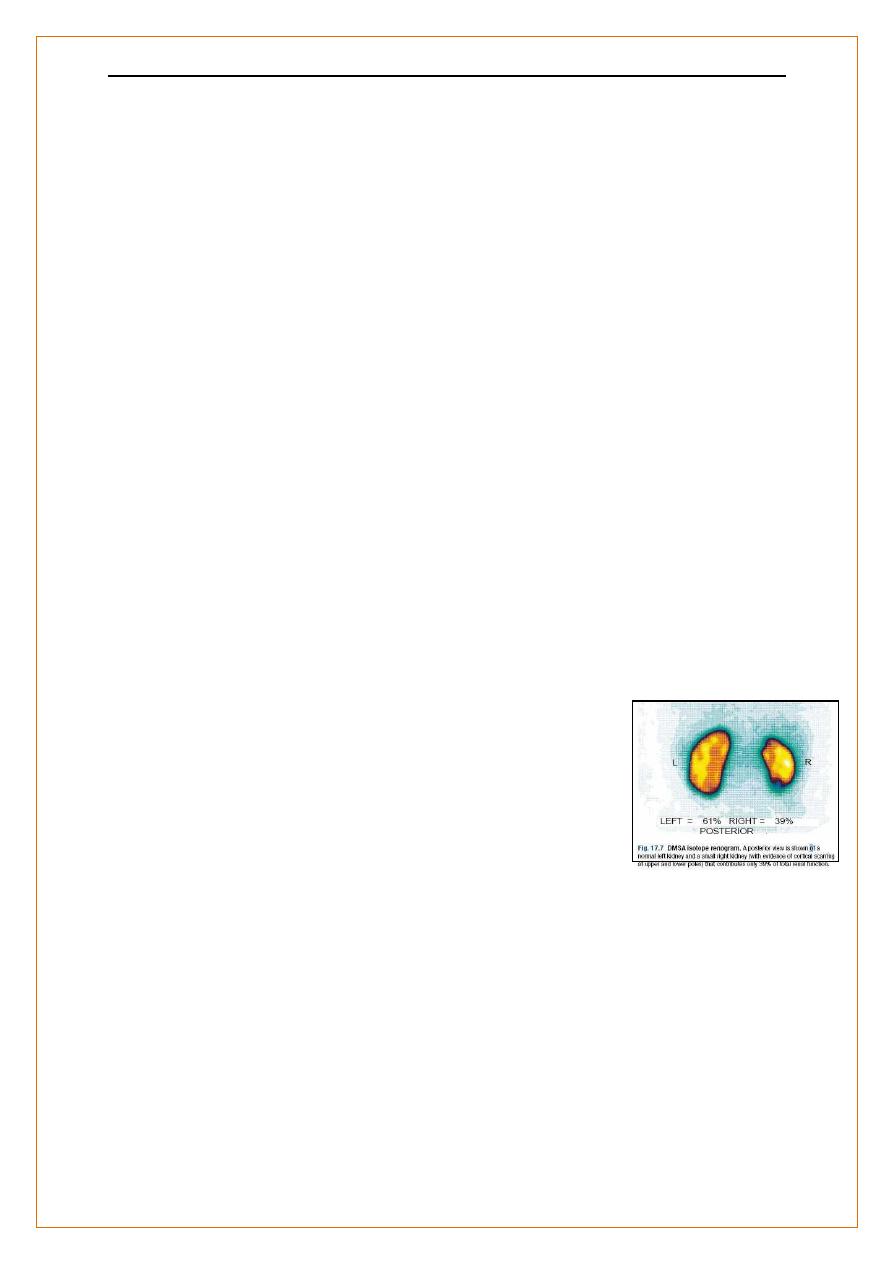
Radionuclide studies;-
(99mTc-DMSA) technetium labelled Dimercaptosuccinic acid
is filtered by glomeruli and partially bound to proximal tubular cells.
Following intravenous injection, images of the renal cortex show the shape,
size and relative function of each kidney.
sensitive method for showing cortical scarring that is of
particular value in children with vesico-ureteric reflux
and pyelonephritis.
Renal complications of radiological investigations
Contrast nephrotoxicity
:-
An acute deterioration in renal function,
commencing < 48 hrs after of i.v. radiographic contrast media
د
.
محمد حنون
y
Nephrolog
lec 2
11
Risk factors
1. Pre-existing renal impairment
2. Use of high-osmolality, ionic contrast media and repetitive
3. dosing in short time periods
4. Diabetes mellitus
5. Myeloma
6. Dehydartion
7. Drugs ACEI ARBs NSAIDs
Contrast nephrotoxicity
:-
Prevention
•• If the risks are high, consider alternative methods of imaging
Hydration, e.g. free oral fluids plus i.v. isotonic saline 500 mLthen 250 mL/hr
during procedure
Avoid nephrotoxic drugs; withhold (NSAIDs). Omit metformin for 48 hrs
after procedure in case renal impairment occurs
N-acetyl cysteine may provide weak additional protection
Cholesterol atheroembolism
Days to weeks after intra-arterial investigations or interventions.
caused by showers of cholesterol-containing microemboli, arising in
atheromatous plaques in major arteries.
in patients with widespread atheromatous disease, usually after
interventions such as surgery or arteriography but sometimes after
anticoagulation.
loss of renal function, haematuria ,proteinuria, eosinophilia and
inflammatory features ( mimic a small-vessel vasculitis.)
د
.
محمد حنون
y
Nephrolog
lec 2
11
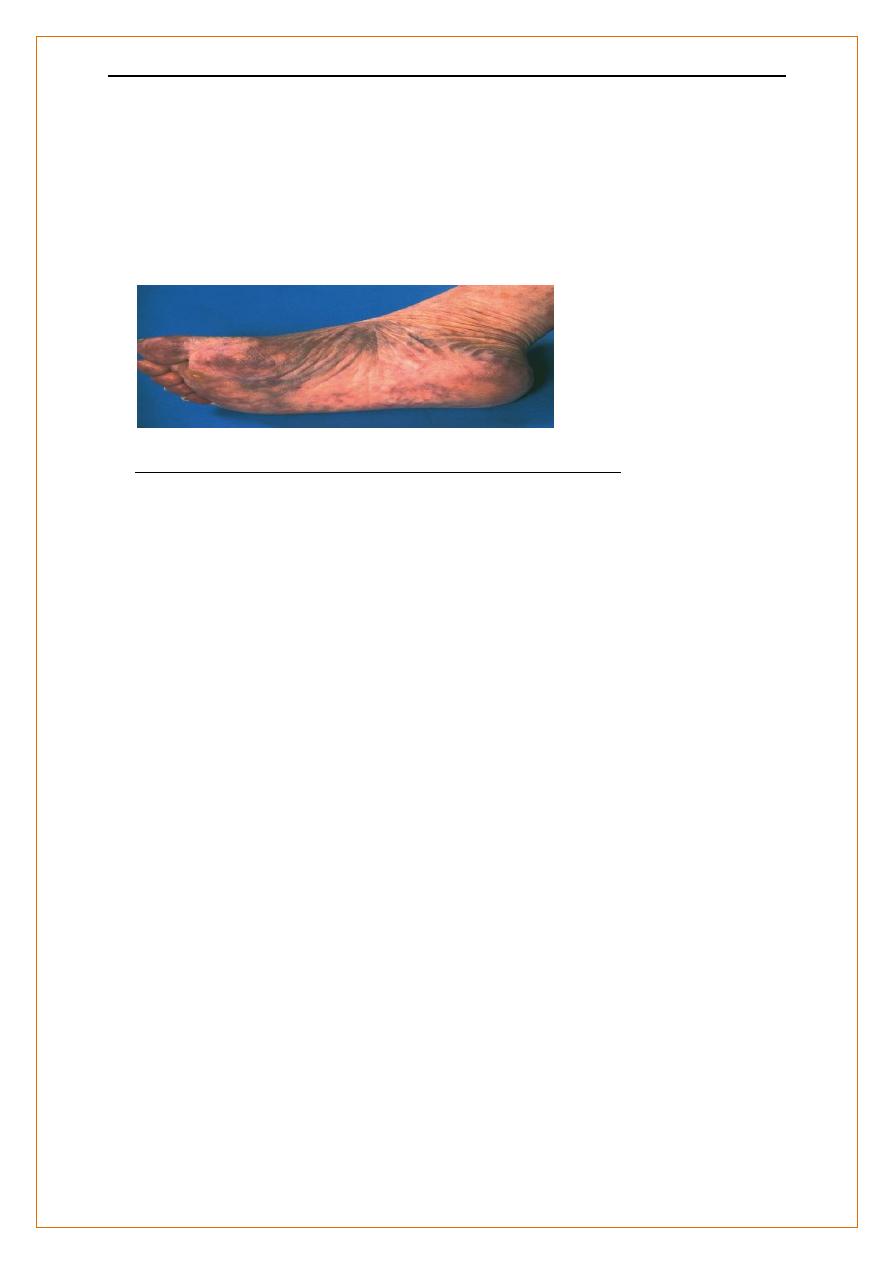
Accompanying signs of microvascular occlusion in the lower limbs (e.g.
ischaemic toes, livedo reticularis) are common There is no specific
treatment but anticoagulation may be detrimental.
The foot of a patient who suffered extensive
atheroembolism following coronary artery stenting.
Renal complications of radiologicalinvestigations
Nephrogenic sclerosing fibrosis after MRI contrast agents
Chronic progressive sclerosis of skin, deeper tissues and other organs,
associated with gadolinium-based contrast agents
Only reported in patients with renal impairment, typically on dialysis or
with GFR < 1mL/min/1.73m2.
caution is advised in patients with GFR < 30 mL/min/1.73m2
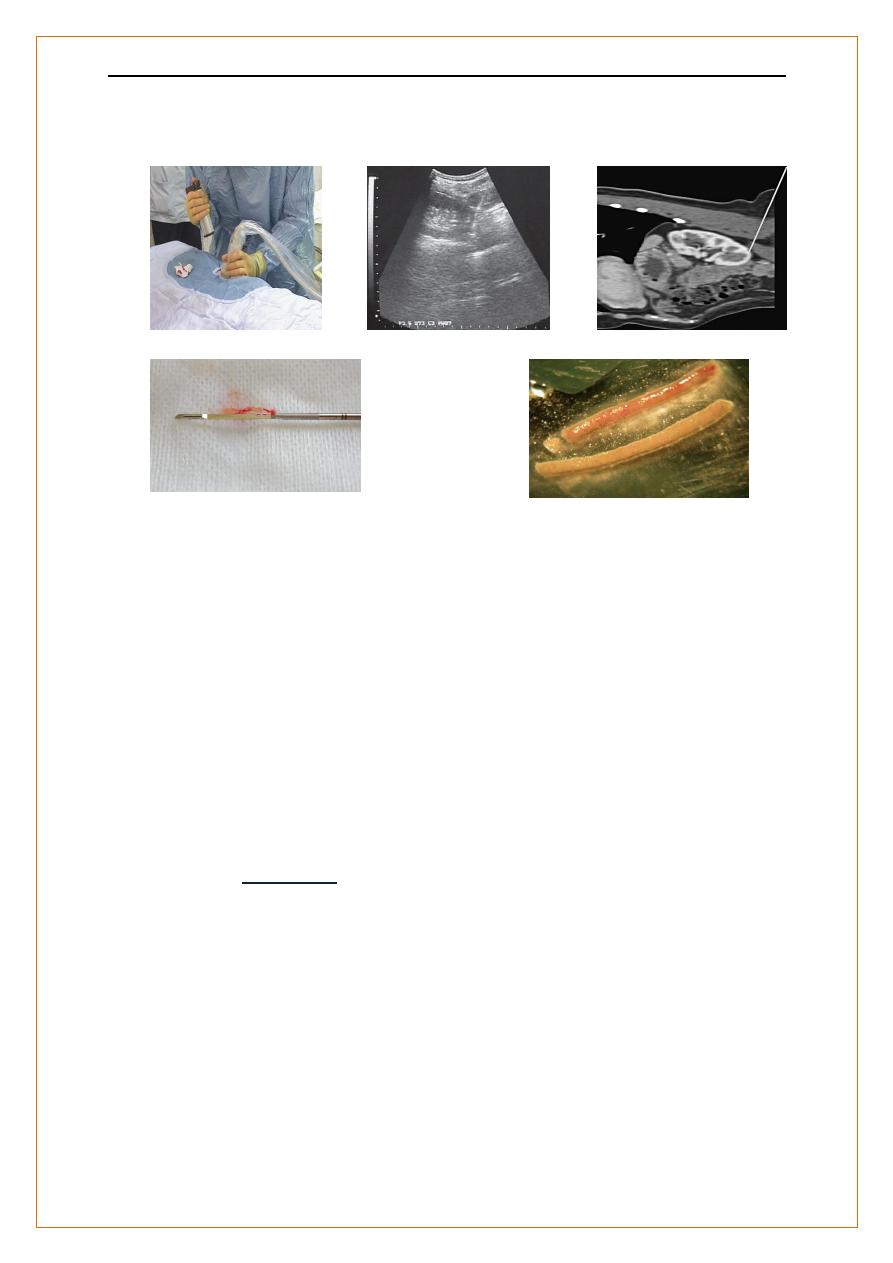
Renal biopsy
:-
Renal biopsy is used to establish the nature and extent of renal disease in
order to judge need for treatment & the prognosis.
Transcutaneous, with U/S or contrast radiography guidance to ensure
accurate needle placement into a renal pole.
-Specimens are divided into 3 samples and placed in
formalin for light microscopy,
normal saline for subsequent snap-freezing in liquid
nitrogen for immunofluorescence,
د
.
محمد حنون
y
Nephrolog
lec 2
12
glutaraldehyde for electron microscopy
Renal Biopsy :-
Indications
1-ARF , not adequately explained (after exclusion of obstruction,
reduced renal perfusion and ATN .
2-CKD with normal-sized kidneys or unexplained ,may be diagnostic, (e.g.,
identify IgA nephropathy )
3-Nephrotic syndrome or glomerular proteinuria in adults
4-Nephrotic syndrome in children with atypical features or is not
د
.
محمد حنون
y
Nephrolog
lec 2
13
responding to treatment
5-Isolated haematuria
6-Non Nephrotic range proteinuria >1g/24hr with renal characteristics
or associated abnormalities
7-Familial Renal Disease Biopsy of one affected member
8-Renal Transplant Dysfunction .
Renal biopsy:-
Contraindications
Pateint related
:-
1-Disordered coagulation or thrombocytopenia. Aspirin and other
antiplatelet agents increase bleeding risk
2-Uncontrolled hypertension
3- Uremia 4 - Obesity 5- Uncooperative patient
Kidney related
1. Kidneys < 60% predicted size
2. Solitary kidney (except transplants) (relative contraindication)
3. -Acute pyelonephritis/ perinephric abscess
4. -Renal neoplasm
Most contraindications are relative rather than absolute; when clinical
circumstances necessitate urgent biopsy, they may be overridden, apart
from uncontrolled bleeding diathesis.
Renal Biopsy:-
Complications
1. Pain, usually mild
د
.
محمد حنون
y
Nephrolog
lec 2
14
2. Bleeding into urine hematurea , usually minor / clot colic and
obstruction
3. Bleeding around the kidney hematoma, occasionally massive and
requiring angiography with intervention, or surgery
4. Arteriovenous fistula, rarely significant clinically
Hematurea
Haematuria :- indicates bleeding from anywhere in the renal tract.
Macroscopic:- - visible and reported by the patient
tumors (most)
severe infections or
renal infarction usually accompanied by pain.
microscopic ;- invisible and detected on dipstick testing of urine
Microscopy shows that normal individuals have occasional red blood cells
(RBC) in the urine (up to 12 500 RBC/mL).
The detection limit for dipstick testing is 15–20 000 RBC/mL,.
However, dipstick tests are also positive in the presence of free
haemoglobin or myoglobin.
Interpretation of dipstick-positive haematuria
د
.
محمد حنون
y
Nephrolog
lec 2
15
Urine microscopy
Suggested cause
---------------------------------------------------------------------------------------------------
Menstruation, strenuous exercise,
Haematuria
White blood cells Infection
Abnormal epithelial cells Tumour
Red cell casts with
Dysmorphic RBC Glomerular bleeding
------------------------------------------------------------------------------------------------
Haemoglobinuria
No red cells Intravascular haemolysis
-----------------------------------------------------------------------------------------------
Myoglobinuria
(brown urine) No red cells Rhabdomyolysis
Dipstick test negative Urine
Cause
Urine colour
Food dyes Acanthocyanins (beetroot)
Red
Drugs
Phenolphthalein
Pink
when alkaline
Senna/other anthaquinones
Orange
د
.
محمد حنون
y
Nephrolog
lec 2
16
Rifampicin
Orange
Levodopa
Darkens
on standing
Bilirubinuria
e.g. Obstructive jaundice
Dark
Dipstick +ve bilirubin,
- ve haemoglobin
Porphyria Darkens on standing
Alkaptonuria
Glomerular bleeding
Glomerular bleeding is characteristic of :-
1. inflammation
2. destruction
3. degeneration
these processes disrupt the glomerular basement membrane (GBM) to
cause microscopic or macroscopic haematuria
Approach to haematuria
Haematuria( repeated ) exclude menstruation infection, trauma
If RBC confirmed on urine microscopy, infection absent on culture
Renal imaging ? anatomical lesion: renal U/S, IVU & cystoscopy
+ ve Full assessment & Mx (Urology/Oncology)
If - ve :-
Are there features of significant renal disease?
e.g. Proteinuria HrT, Abnormal RFT Family Hx ?? Systemic dis.
د
.
محمد حنون
y
Nephrolog
lec 2
17
Yes Consider renal biopsy
No Observation (Urine test, BP, creatinine ) 6 – 24 months
Re-refer if anything changes
