Dr:Nibal Lec: 2
Neurology
Cerebral palsy
Total :39
Lec : 2
Dr:Nibal Lec: 2
Dr:Nibal Lec: 2
Cerebral palsy
Dr.Nebal waill
Definition (historical)
Non progressive disorder of motion and /or posture
secondary to an insult in the developing brain.
CP is a static encephalopathy.
Despite the static nature, its peripheral manifestations can seem to progress
and mimic progressive CNS pathology.
Delay in clinical expression in static brain lesion reflects changes in
maturation function & distribution of various neurotransmitters
Etiology
1. Prenatal
2. Perinatal
3. postnatal
Dr:Nibal Lec: 2
Most children with CP had been born at term with uncomplicated labors and deliveries.
For many decades the belief that birth complications caused most cases of cerebral palsy was widespread
among physicians , families and even medical researchers
less than 10% of children with CP had evidence of intrapartam asphyxia
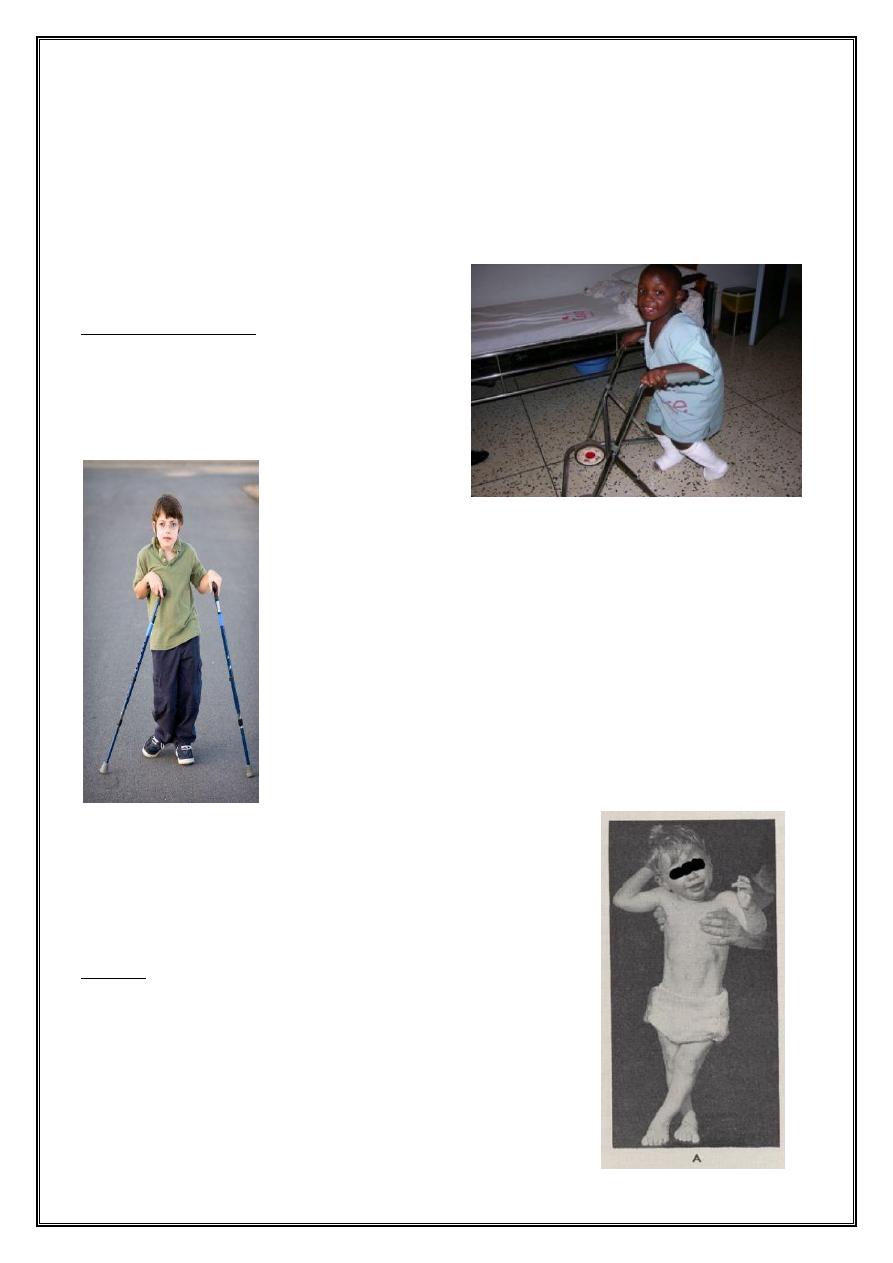
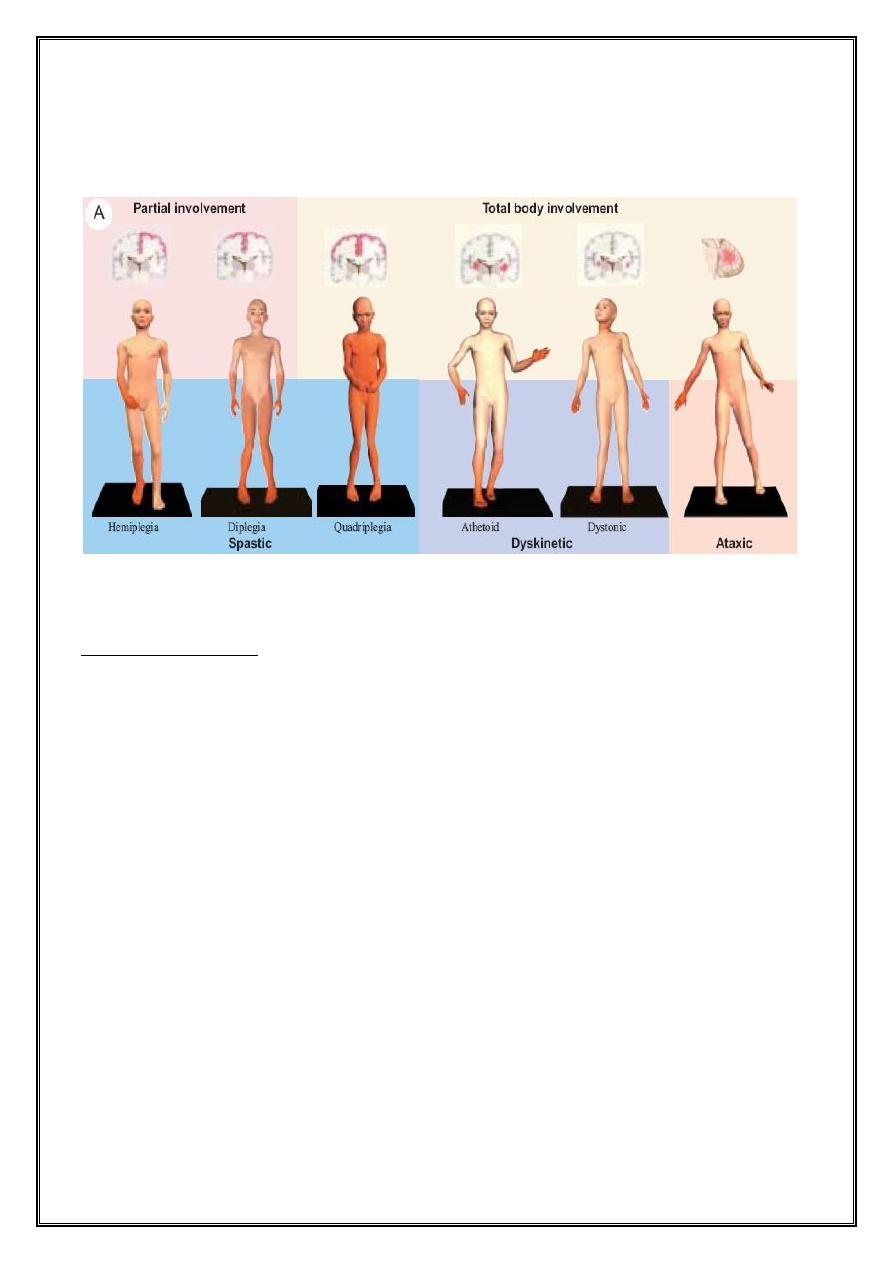
Physiologic classification
1. Spastic 70%-80%
2. Dyskinetic 10%-15% or dystonic ( extrapyramidal CP)
3. Ataxic < 5% ( cerebellar )
4. Hypotonic or atonic
5. mixed
Dr:Nibal Lec: 2
Topographic classification
Spastic cases further classified according to the involvement of extremities
1. Quadriplegic 10-15%
2. Diaplegic 30-40%
3. Hemiplegic 20-30%
4. Monoplegic
5. Double hemipleic
6. Triplegic
Functional classification
1. Mild
2. Moderate
3. Severe
Etiologic classification
1. Congenital
2. Acquired
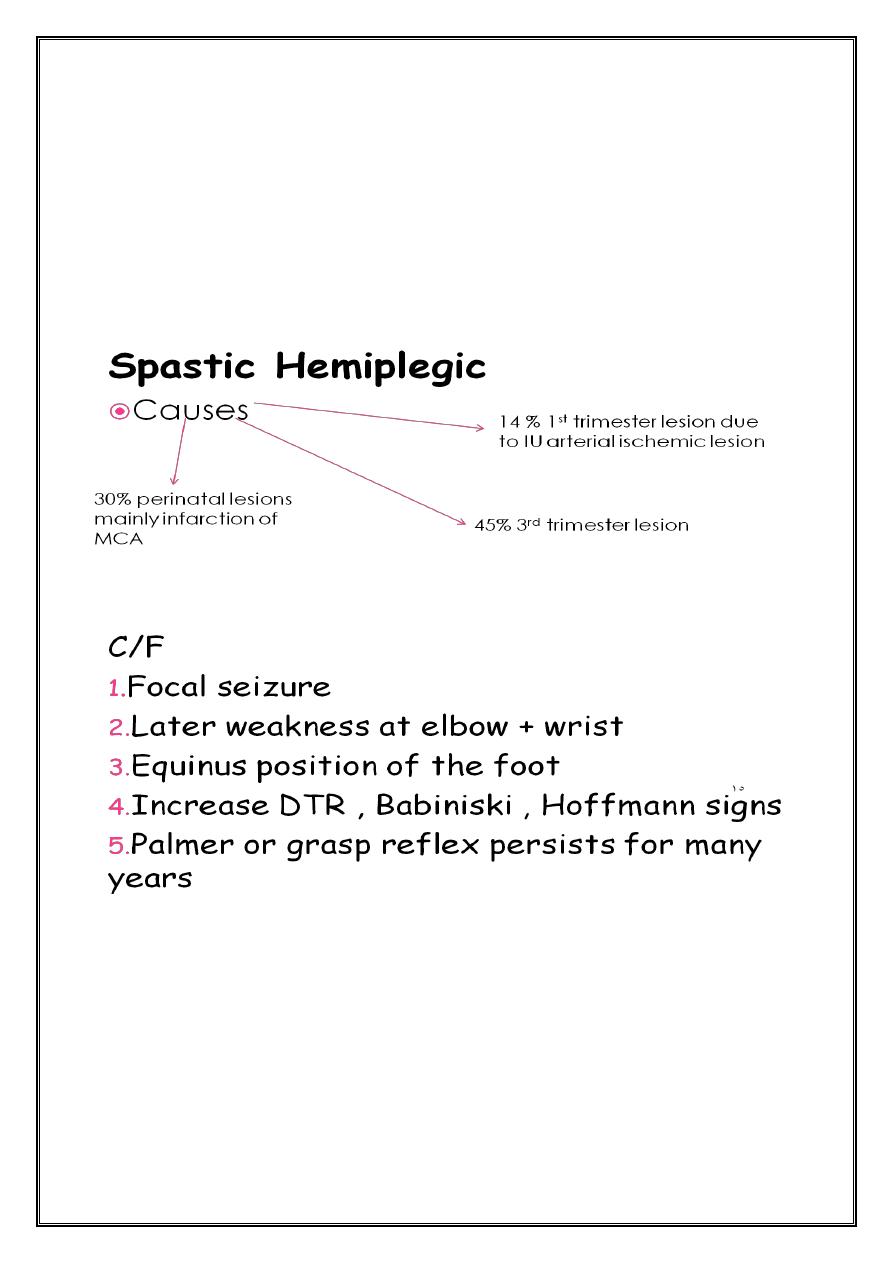
Spastic Diplegic
Bilateral spasticity of the legs more than the arms.
1st indication (commando crawl).
Difficult in application of a diaper.
Unable to sit.
Dr:Nibal Lec: 2
increase reflexes , ankle clonus and bilateral babiniski sign
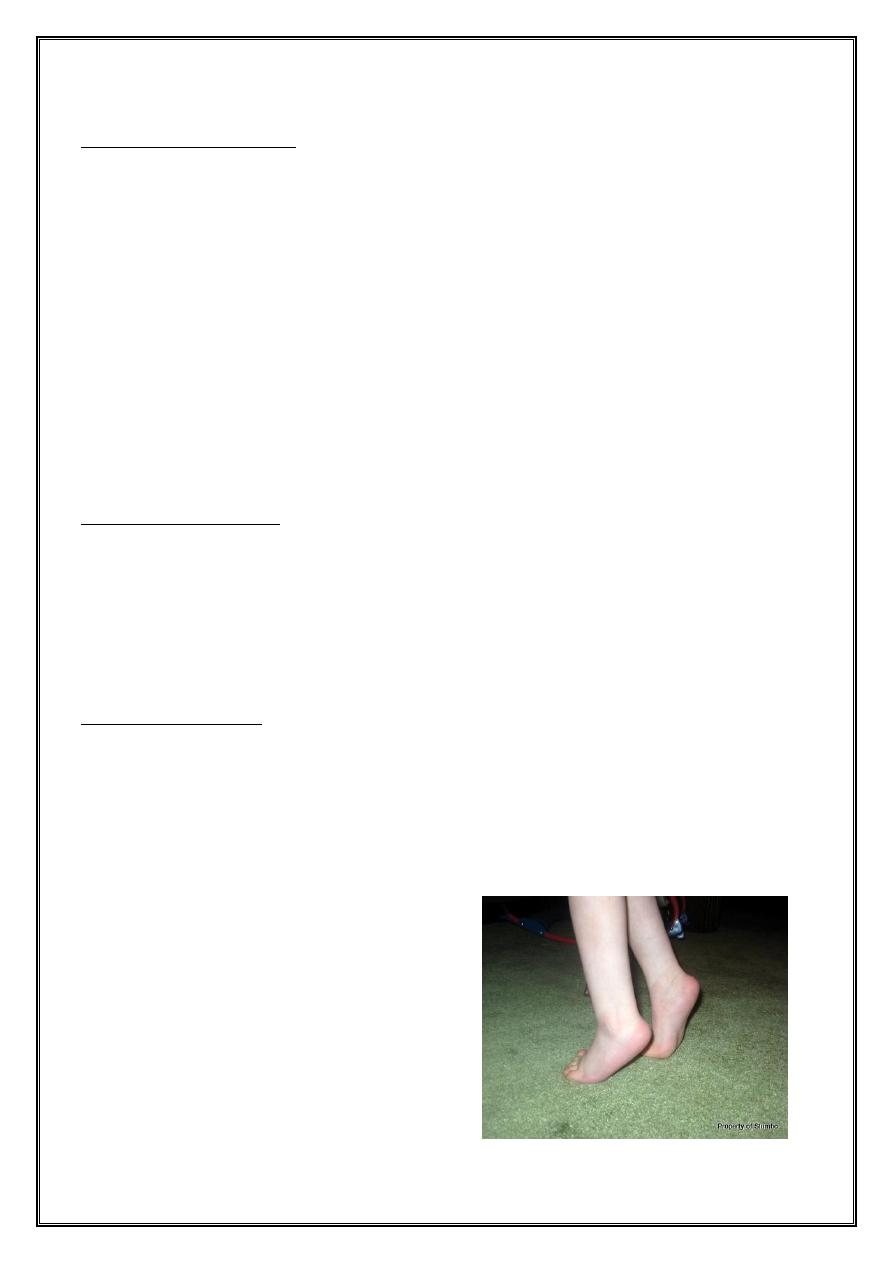
Feet in equinocanus , tiptoe (some time the only manifestation in mild type )
Normal intellectual development, minimal seizure.
causes : prematurity mainly
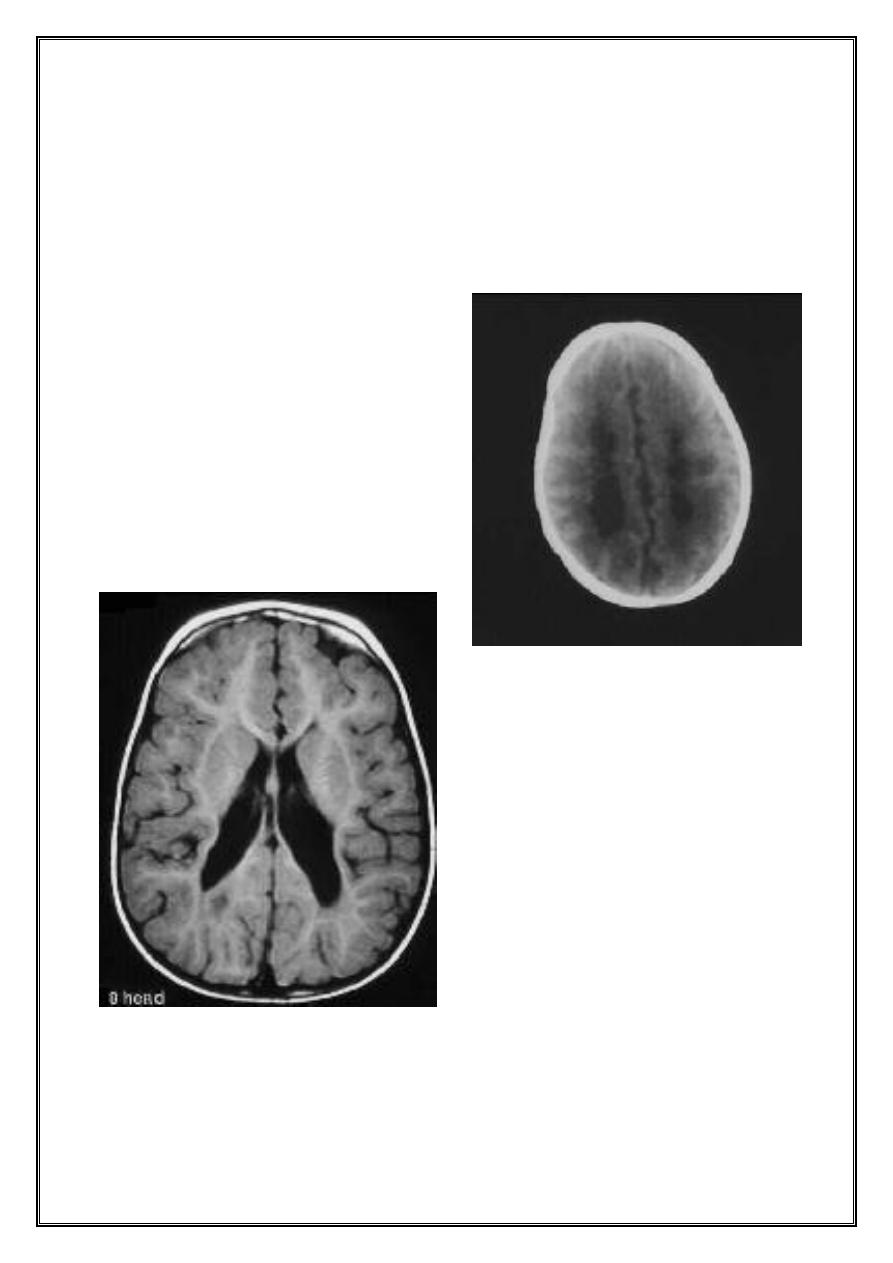
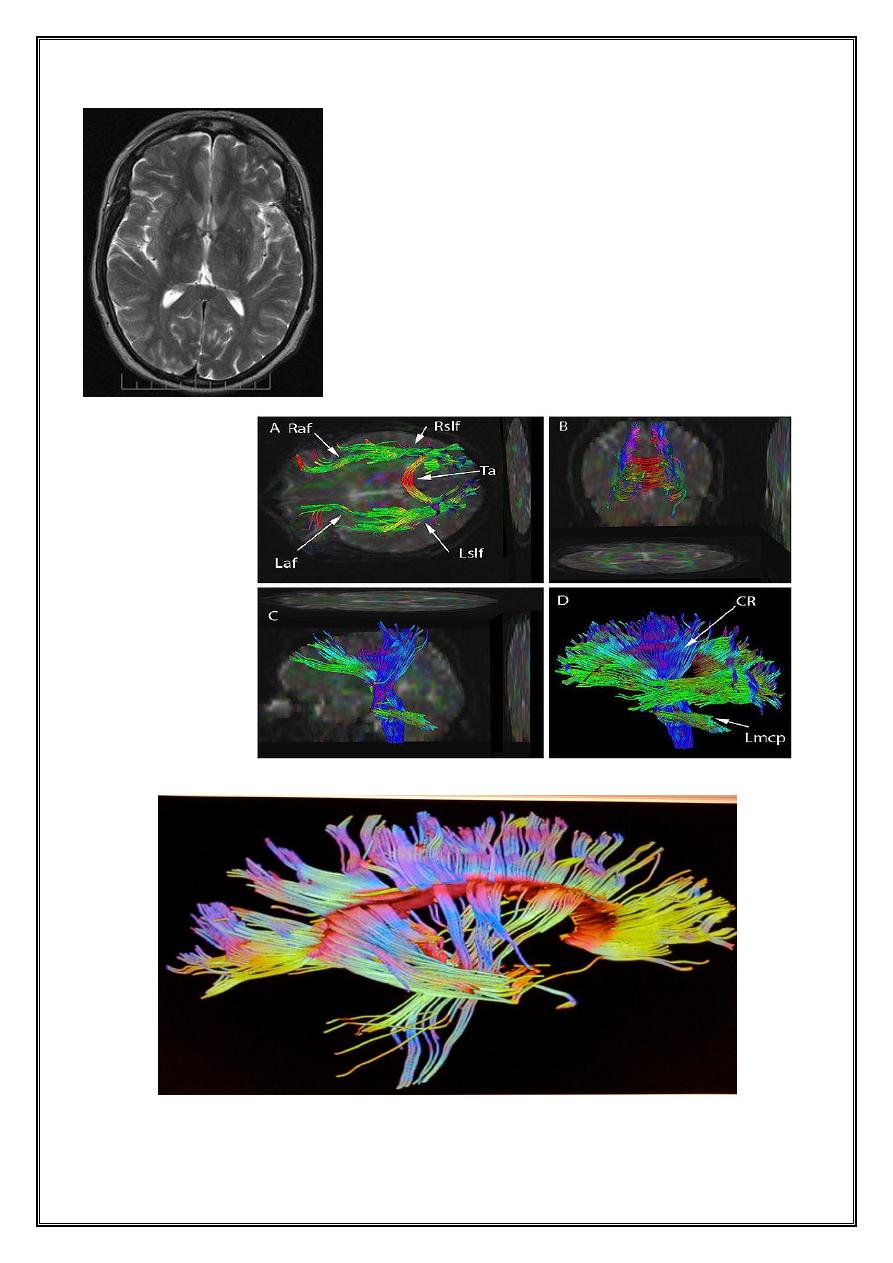
The ventricular margins are irregular, which is consistent
with incorporation of the periventricular cysts of PVL. Mild
ventriculomegaly
The lateral ventricles are enlarged without hydrocephalus.
The periventricular white matter is diminished
ž
ž
Dr:Nibal Lec: 2
if suspended by the axillae = scissoring posture
After 2 years contractures appeared
DTR may difficult to be elicited because of muscle rigidity
Vasomotor changes common
More than 50% develop seizure
50% have average IQ
Dr:Nibal Lec: 2
Spastic quadriplegic
1. Etiology : in the majority abnormalities in delivery particularly prolonged 2nd stage of labour
2. Pathology : extensive cystic degeneration of brain
3. MRI as above
4. C/F :
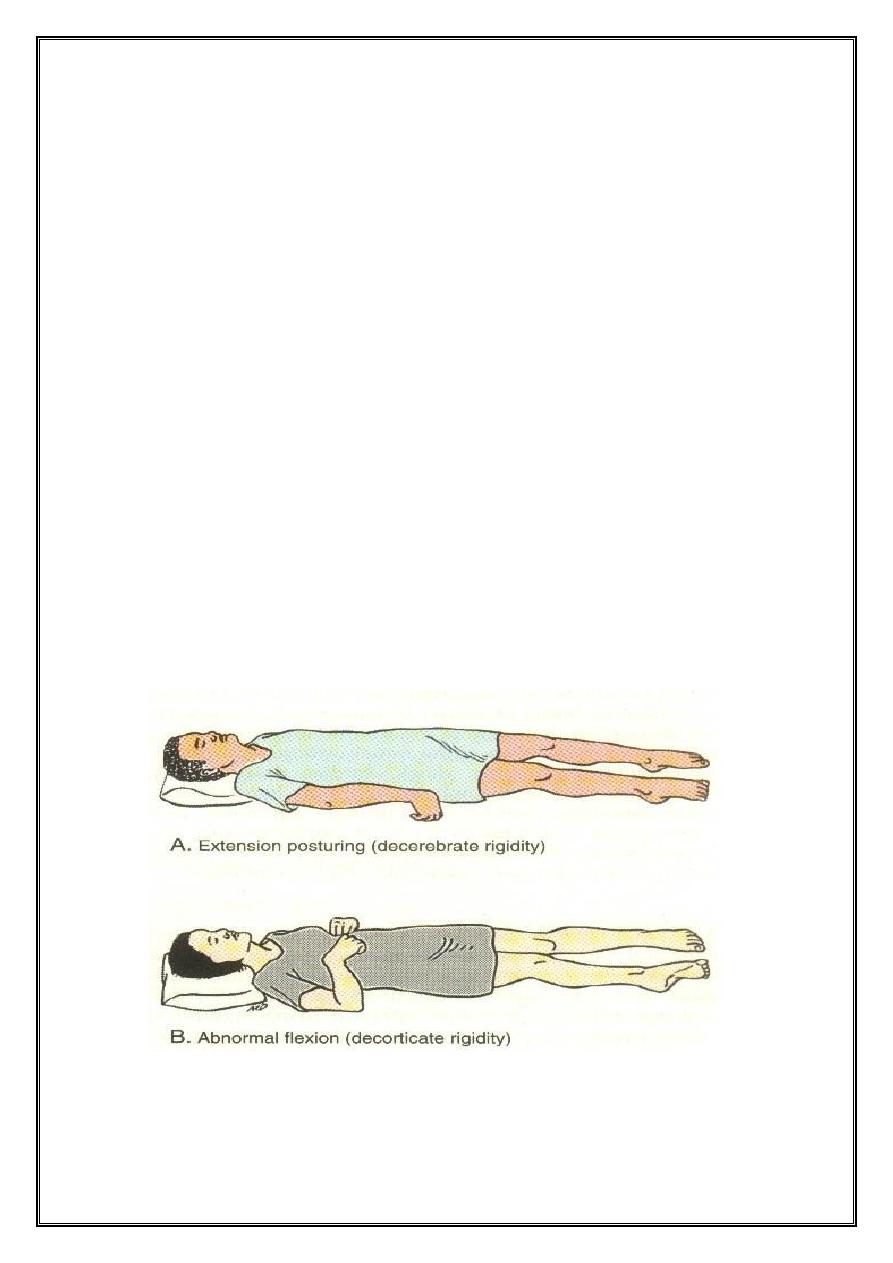
tone + rigidity of all limbs ( both flexion and extension )
Assume decerebrate posture
Vasomotor changes are common in extremities
Psedobulbar signs ---------- difficulty swallowing and recurrent aspiration
Optic atrophy
Grandmal seizure ---------- 50% of patients
Intellectual impairment --------- all
Dr:Nibal Lec: 2
58% experienced perinatal asphyxia
34% LBW + SGA
Evolves from hypotonia then choreoathetosis appear at the 2
nd
-3
rd
year of age
Some continue manifesting hypotonia
Dystonia may appear later ( 3
rd
decade of life )
Various involuntry movements with spasticity
Delayed development of motor functions
Skilled hand movement impaired
Speech impaired
Impaired swallowing and saliva control
Cranial nerves involvement less common
Seizure 25%-40%
Strabismus 1/3
Dr:Nibal Lec: 2
Optic atrophy rare
IQ underestimated ( delayed language and gross motor handicap )
MRI brain = high signal intensity at ant. Thalamus, post. Thalamus , posterior Potamen
Also changes in basal ganglia
Ataxic
Some have signs of cerebellar disorder.
Mainly due to developmental anomaly of cerebellum.
some due to perinatal trauma or perinatal asphyxia
Hypotonic CP
Ccc by generalize muscular hypotonia that persists beyond 2-3 yr of age & not result from 1 disorder of
muscle or nerve.
DTR = normal or hyperactive
50% develop frank cerebellar signs
My be a forruner to ECP although the majority of the latter develop involuntry movement before 3 yr
Cause unknown
MRI no significant anatomical changes
Mixed form
minor amounts of athetotic posturing in hight % of children with spastic hemiparesis
Extensor planter in patient with predominantly extrapyramidal disease
Dr:Nibal Lec: 2
Hyperreflexia , spasticity and contractures in child with frank dystonia or othere extrapyramidal movements
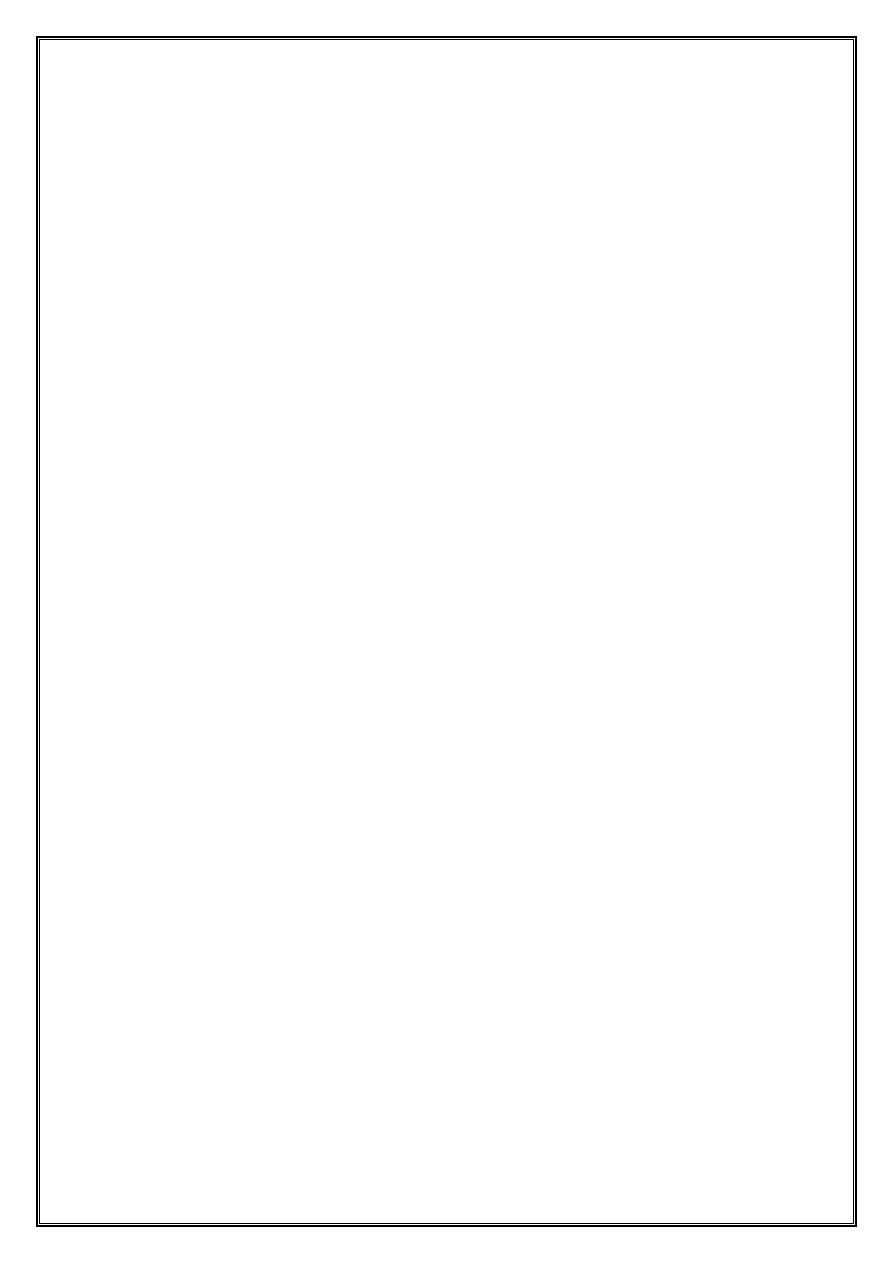
Clinical presentation
Ataxia
Spasticity, stiff muscles and exaggerated reflexes.
plegia – Hemiplegia • Impaired walk caused by asymmetrical walking gait
Irritability.
Variations in muscle tone, from too stiff to too floppy.
Excessive drooling or difficulties swallowing, sucking or speaking.
Tremors.
Abnormal sensation and perception.
Impairment of sight, hearing or speech.
Seizures.
Dr:Nibal Lec: 2
Difficulty with precise motions.
Mental retardation
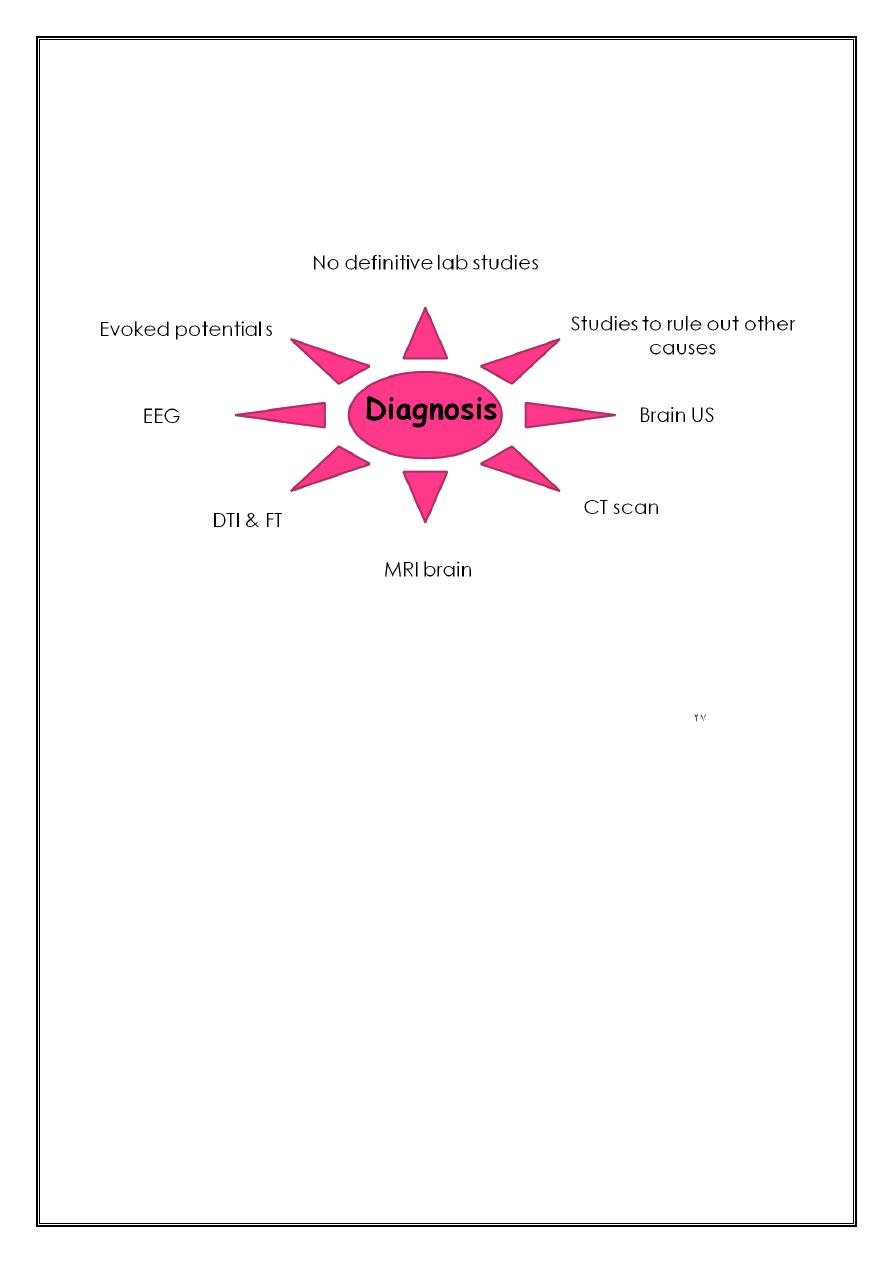
Diagnosis
1. Other studies to rule out other causes like TFT , lactate & pyruvate level , organic and amino acid ,
chromosomes & CSF protein
2. US predictive for very preterm newborn at risk of cerebral palsy
3. CT brain : cong. Malformation , IVH , PVL
4. MRI : location & extent of malformations
5. DTI & FT : orientation and integrity of white matter fibers
6. EEG: diagnosis of seizure
7. Evoked potentials : detect abnormalities of hearing and vision
Dr:Nibal Lec: 2
T2- MRI: no neural tract seen
DTI tractographic
assessment at different
views
Dr:Nibal Lec: 2
Dr:Nibal Lec: 2
Associated problems
The likelihood and severity of associated impairments increases with the severity of motor impairment.
1. Musculoskeletal deformities
2. Intellectual impairment
3. Speech impairments
4. Visual impairment
5. Hearing impairments
6. Feeding and nutrition
7. Urogenital impairment
8. Epilepsy
9. Spinal deformities
Dr:Nibal Lec: 2
10. Teeth problems
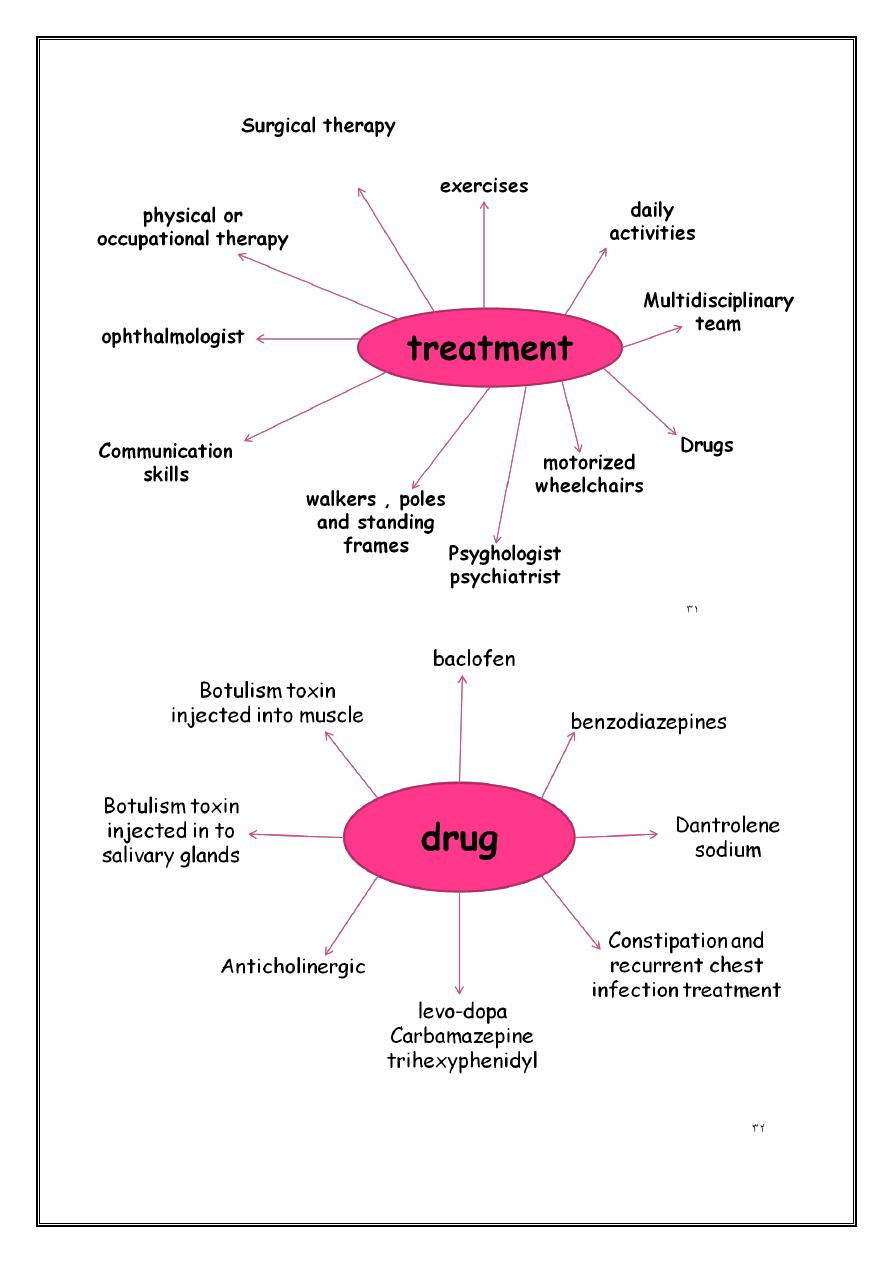
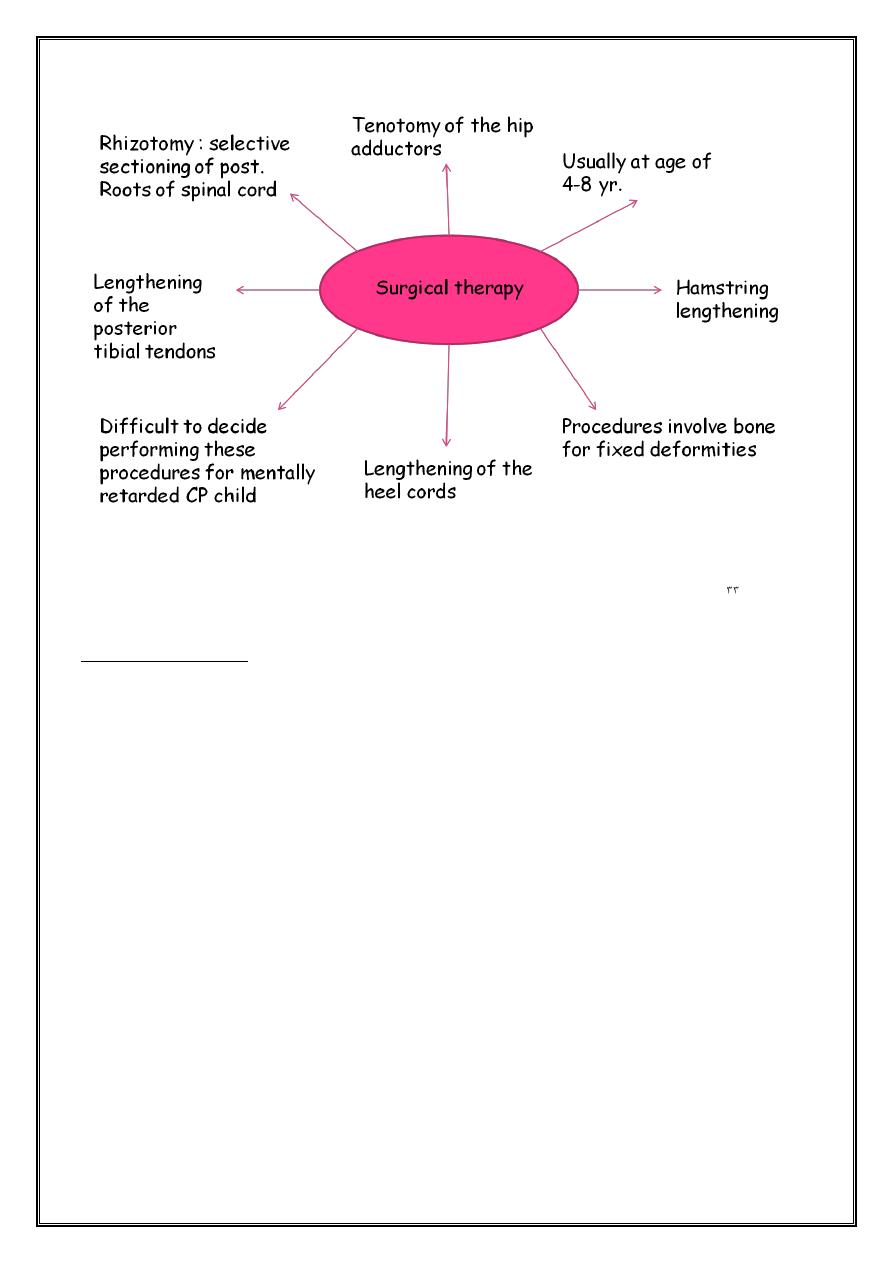
Special aids
Glasses
Hearing aids
Splints
Special shoes
Wheelchairs
Communication aid
Causes & risk factors
Maternal and prenatal 70-80%
1. Long menstrual cycle
2. Previous pregnancy loss
3. Previous loss of newborn
4. Maternal mental retardation
5. Maternal thyroid disorder ( iodine deficiency )
6. Maternal seizure disorder
7. Delivering child with weight less than 2000 gram
8. Delivering child with motor deficit , MR or sensory deficit
Dr:Nibal Lec: 2
9. IU infection
10. Abdominal trauma
11. Blood type incomaptibility
12. Teen ager mother
13. Incompetent cervix
14. Polyhydraminos
15. Treatment of the mother with estrogen or progesterone
16. Multiple gestation ( due to prematurity or LBW )
17. Exposure to high level of lead during pregnancy
18. Maternal antibiotics
Perinatal factors (10%)
1. Prematurity
2. Chorioamnionitis
3. BW less than 2500 gram
4. Growth retardation
5. Nonvertex and face presentation of the fetus
6. Birth asphyxia (≤10%)
7. Low apgar score alone can’t be used as an indicator of birth asphyxia
8. ICH
Postnatal factors
1. Infection ( e.g. meningitis , encephalitis )
2. ICH ( prematurity , trauma , vascular malformation )
Dr:Nibal Lec: 2
3. PVL
4. HI lesion
5. Seizure
6. Kernicterus
7. Neonatal pneumothorax , sepsis
8. Brain injuries as in drowning , car accidents
9. Coagulopathy
10. Persistent fetal circulation or persistent pulmonary HPT of the newborn
Prevention
Proven
1. MMR vaccination
2. Idodine supplement
3. Anti D for Rh –ve mother
4. Transfer of a very preterm infant in utero to tertiary centre
Probable
1. Early routine US
2. Ovoid excessive alcohol intake in pregnancy
3. Phototherapy for NNJ
4. Vitamin K at birth to prevent brain hemorrhage
5. Child abuse preventive strategy
6. SIDS preventive strategy
7. EPO has protective effect against HI injury
Dr:Nibal Lec: 2
8. Fetal exposure to magnesium sulfate in women at risk of preterm delivery significantly reduces the risk of
CP without increasing the rate of death
Possible
1. Zinc , folate , fish oil to prevent IUGR
2. Operative delivery of fetal distress
3. Rescue therapy for birth asphyxia
Doubtful
1. Electronic fetal monitoring for distress
2. Addition of fetal scalp sample or ECG
3. Bed rest for history of growth restriction
4. Hospitalization for multiple pregnancy
5. Antenatal endomethacin or thryotorpin releasing hormone
Prognosis
Ultimate social adjustment depends primarily on
1. Severity of physical and mental handicap
2. Presence or absence of associated disabilities including seizures and visual or hearing impairment
Predictors to inability to work:
1. IQ < 50
2. Non-ambulatory and without communication skills
3. Need assistance to use their hands
Dr:Nibal Lec: 2
1. All children with spastic hemiparesis became ambulatory
2. Children with spastic diaplegia ambulatory in 86-91%
3. ¼ of those with extrapyramidal CP are ultimately able to work competitively
4. None of those with spastic quadriparesis was gainfully employed
Adult with CP
1. New functional disabilities
2. Extremities contracture
3. Scoliosis
4. Cervical pain
5. Back pain
6. Reduced mobility at adulthood for mobile patients
7. Speech and self-feeding well preserved
8. Survival rates in ambulatory adults only moderately worser than general population
Hansen got his driver's license on the third try when he was in his
mid-20s. He has spastic diplegic cerebral palsy. It mostly affects his
legs. He drives with his hands. He and his dad installed a $450 hand
control system in his Ford Contour in just a couple of hours. Wil took
David Sommerstein for a demo to the gas station and the bank.
Dr:Nibal Lec: 2
Life expectancy in CP child
Mild – moderate disability 98% of them live to age of 35 years.
Profound handicapped & immobile child >1/3 of them die before age of 30 years.
