AFTER MID
LEC: 3
DR. KHUDAIR
Oncology
Chemotherapy
TOTAL LEC: 3
Dr. Khudair


Cancer Chemotherapy
Dr. Khdair Al-Rawaq
Cancer
•
It is basically a disease of cells characterized by the shi: in the
control mechanism that govern cell prolifera@on and
differen@a@on.
Special Characteris@cs of Cancer Cells
•
Uncontrolled Prolifera@on
•
Dedifferen@a@on and loss of func@on
•
Invasiveness (Spreading)
•
Metastasis (spread of cancer from its primary site to other places
in the body )
Management of Cancer
•
Surgical
•
Radia@on
•
Chemotherapy
•
The neoplas@c cell burden is ini@ally reduced either by surgery and
/or radia@on followed by chemotherapy or combina@on therapy.

Chemotherapy
Types of Therapis:
•
Adjuvant: Addi@onal treatment a:er the primary treatment to
lower the risk that the cancer will come back.
•
Neo-Adjuvant therapy :Treatment as a first step to shrink a tumor
before the main treatment.
•
Concurrent therapy: When two or more therapies are given
together, such as chemotherapy and radia@on.
CANCERS WITH ESTABLISHED OR PROBABLE BENEFIT FROM
ADJUVANT CHEMOTHERAPY
•
Breast cancer
•
Colorectal cancer
•
Osteosarcoma
•
Wilms' tumor
•
Stage II-III gastric cancer
•
Stage II-III non-small cell lung cancer
•
Stage III melanoma

The raLonale of neoadjuvant therapy is
•
The immediate exposure of local and possible distant disease to
effec@ve chemotherapy, avoiding the delay introduced by surgery
and recovery;
•
Immediate in vivo assessment of chemotherapy responsiveness of
the primary tumor, and therefore, of possible nodal or distant
micrometasta@c disease;
•
Bulk reduc@on of local disease to allow for a subsequent less
anatomically destruc@ve surgical procedure. In responding
pa@ents, chemotherapy is carried out in a flexible number of
cycles to the best or complete response, followed by defini@ve
surgery.
CANCERS WITH ESTABLISHED BENEFIT FROM NEOADJUVANT
CHEMOTHERAPY
•
Locally advanced breast cancer
•
Larynx cancer
•
Esophageal cancer
•
Bladder cancer
•
Anal cancer
•
Osteosarcoma
•
So: @ssue sarcoma
CANCERS WITH ESTABLISHED BENEFIT FROM Concurrent
ChemoradiaLon
•
Larynx cancer
•
Esophageal cancer
•
Cervical carcinoma
•
PNS Carcinoma
•
Rectal Carcinoma
Chemotherapy
•
It is the treatment of disease by chemicals especially by killing
micro-organisms or cancerous cells.
•
In popular usage, it refers to an@neoplas@c drugs used to treat
cancer or the combina@on of these drugs into a regimen.
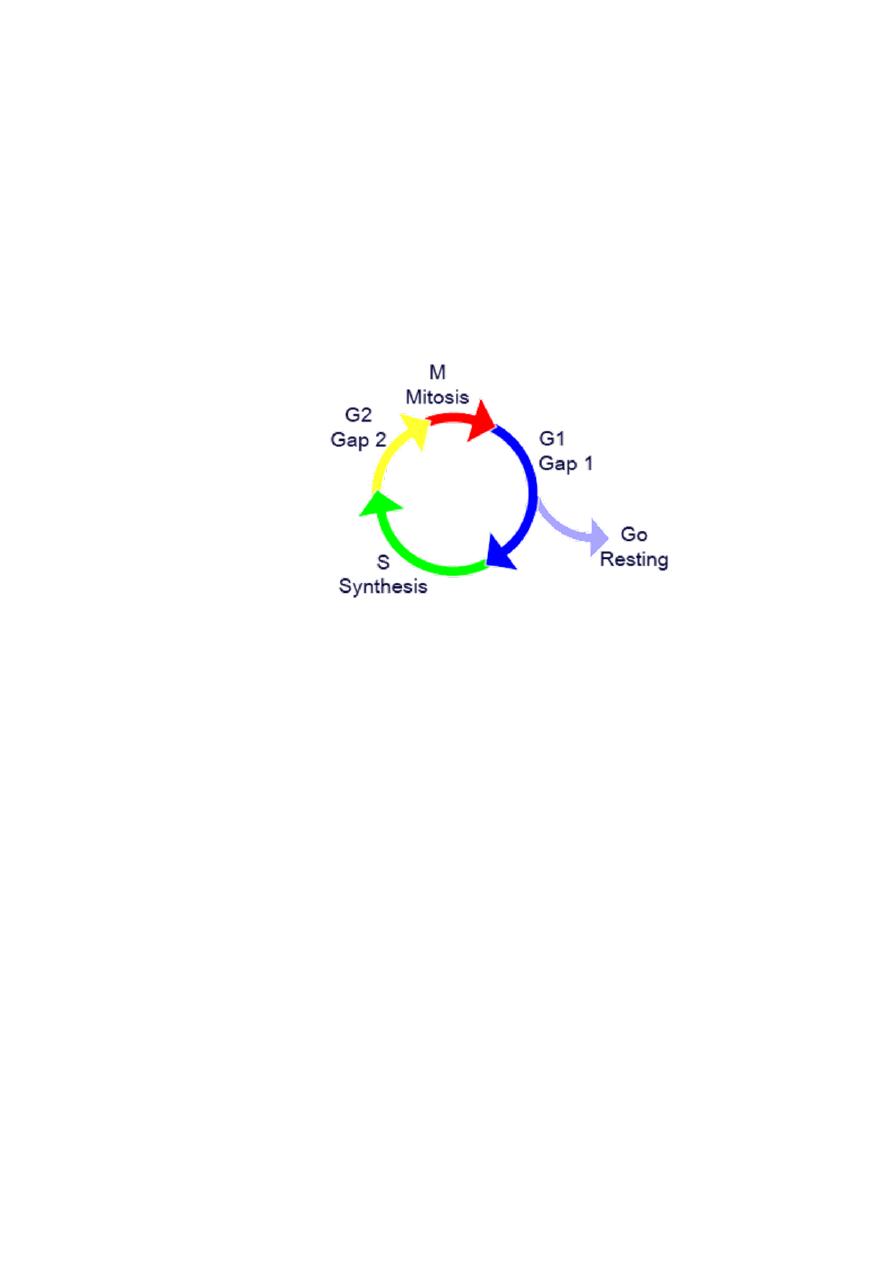
Cell Cycle
•
G
0
: A resLng phase,the cell has stopped dividing.
•
G
1
: Cells increase in size.
•
S : DNA replicaLon occurs.
•
G
2
: Gap between DNA synthesis and mitosis, the cell will conLnue
to grow.
•
M : Cell growth stops ,and cellular energy is focused on the orderly
division into two daughter cells.
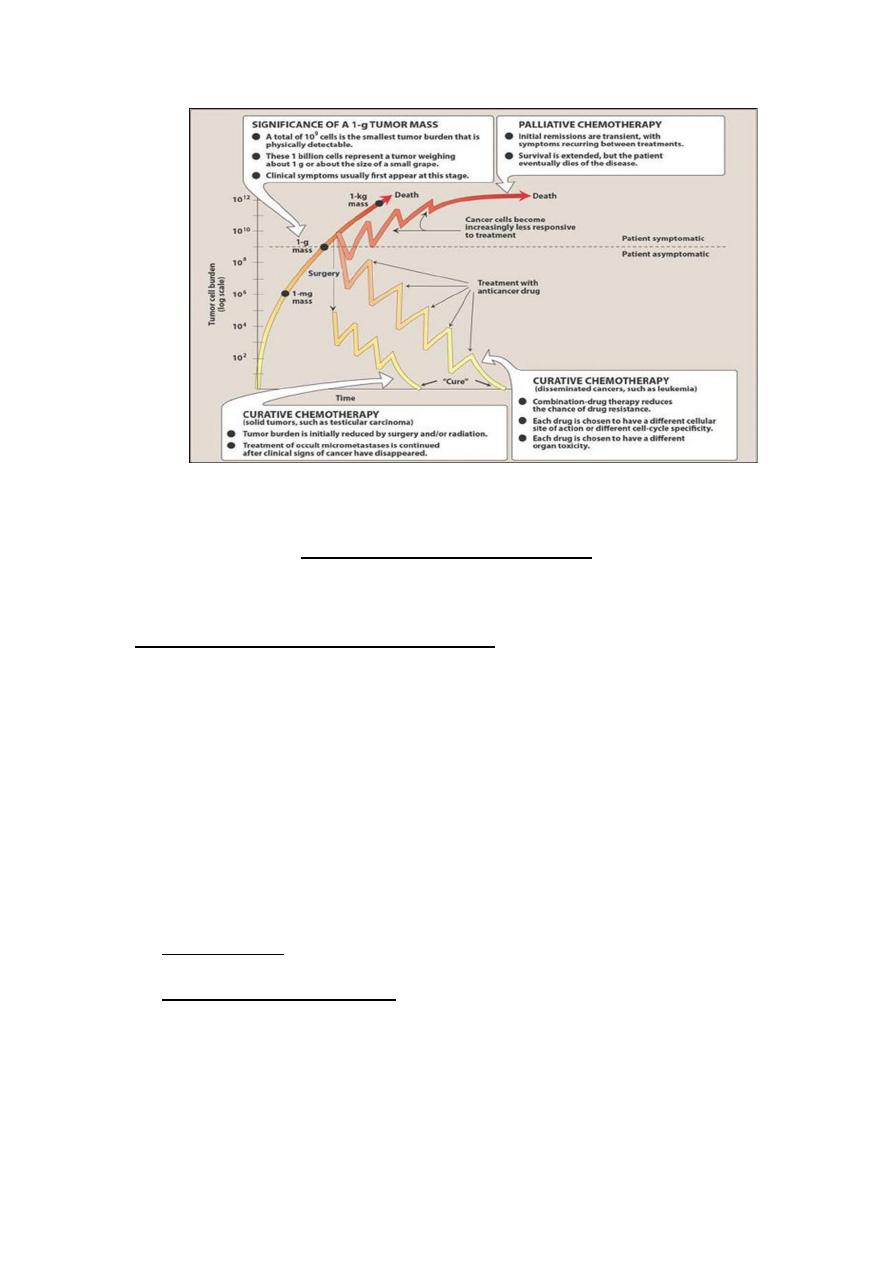
Principles of cancer chemotherapy
1. Goal of treatment:
•
The ul@mate goal of chemotherapy is cure. i.e. long term disease
free survival.
•
If cure is not aZainable, then the goal becomes pallita@on i.e.
allevia@on of symptoms and avoidance of life-threatening toxicity.
2. IndicaLons for treatment:
Chemotherapy is indicated when neoplasms are
disseminated (Spread over a large area)and are not cured by
surgery.
Chemotherapy is also used as a supplimental treatment to
aZack micrometastasis following surgery and radia@on
treatment
CANCERS POTENTIALLY CURABLE WITH CHEMOTHERAPY
ALONE
1. Choriocarcinoma
2.
Hodgkin's lymphoma
3.
Non-Hodgkin's lymphoma (some types)
4.
Tes@cular cancer
5.
Acute lymphoid leukemia
6.
Acute myelogenous leukemia
7.
Ovarian cancer
8.
Small cell lung cancer
3. Tumor suscepLbility and growth cycle:
Rapidly dividing cells are generally more sensi@ve to an@ cancer
drugs. therefore the frac@on of tumor cells that are in replica@ve
stage of their cycle are most suscep@ble.
Non prolifera@ng cells (those are in Go phase) usually survive the
toxic effects of many of these agents.
4. Cell cycle specificity of drugs:
•
The normal and tumor cells differ in the number of cells that
are in various stages of the cycle.
•
Chemotherapeu@c agents that are effec@ve only against
replica@ng cells are called cell cycle specific (CCS) drugs.
•
Others are said to be cell cycle non specific (CCNS) drugs.
•
The non specific drugs have more toxicity in cycling cells
and are useful against tumors that have low percentage of
replica@ng cells.
5. Tumor growth rate:
•
The growth rate of most solid tumors in vivo is
ini@ally rapid, but growth rate decreases as tumor
size increases. Because of unavailability of nutrients
and oxygen.
•
By reducing the tumor burden through surgery or
radia@on promotes the remaining cells growth into
ac@ve prolifera@on and increases their suscep@bility
to chemotherapeu@c agents.

6. Treatment regimens and scheduling:
•
Drugs are administered on the bases of body surface area.
•
Destruc@on of cancer cell by chemotherapeu@c agent follows first
order kine@cs , i.e. given dose destroys constant frac@on of cells.
(Log kill)
•
Combine drug therapy is more successful than single drug
treatment.
•
In combine therapy the drugs must have different toxici@es,
Mechanism of ac@on.
Chemotherapy scheduling and regimens:
The principles of choosing combinaLons of chemotherapy are as
follow
:
•
Each drug is ac@ve against the tumour as a single agent.
•
There are no clinically important drug interac@ons between the
agents.
•
Combina@ons should avoid drugs of the same class or those with
similar modes of ac@on.
•
The drugs should have different dose-limi@ng toxici@es
•
Drugs should have different mechanisms or paZerns of resistance
Principles of cancer chemotherapy
Effects of various treatments on the cancer cell burden:
ﺷﺮﺑﻮ ﺷﻮﯾﺔ ﻣﻲ رح ﯾﺠﯿﻜﻢ ﺳﺎﯾﺪ اﻓﻜﺖ
:D
Problems associated with chemotherapy:
•
Resistance:
a) Inherent
b) Acquired
•
Toxici@es:
Effects on normal rapidly prolifera@ng cells i.e. Buccal mucosa,
Bone marrow, GI mucosa, Hair.
Side Effects
•
Bone marrow suppression:
•
Anemia
•
Neutropenia
•
Thrombocytopenia
•
Effects on GIT:
•
Nausea & Vomi@ng
•
Stoma@@s & mucosi@s
•
Dysphagia
•
Cons@pa@on
•
Diarrhea
•
Effects on skin:
•
Skin dryness
•
Photosense@vity
•
Skin pigmenta@on
•
Hair loss
•
Effects on reproducLve system:
•
Azospermia
•
Amenorrhea
•
Effects on Cardiovascular System:
•
Heart failure
•
cardiomyopathy
•
IHD
• Effects on CN system:
•
Periphral neuropathy
•
Fit
•
Parasthesia
•
Loss of hearing
• Effects on Respiratory System:
•
Respiratory failure
•
Pulminary fibrosis
•
RDS
•
Chemical pneumoni@s
• Effects on GU system:
•
nephropathy
•
Haemoragic cys@@s
•
Renal papillary necrosis
•
Renal failure
• Others
•
Second Malignancies A:er Chemotherapy
•
Hepa@c toxicity
•
Cataract
•
Electrolites imbalance
•
Teratogenicity in pregnancy
•
Hypersense@vity reac@ons
•
extravasa@on
ROUTES OF ADMINISTRATION:
•
Intravenous
•
Most chemotherapeu@c agents are available only in an
intravenous prepara@on, requiring venous access
•
Oral
•
A number of agents are available in oral form, making intravenous
access unnecessary.
•
Intraperitoneal Therapy
•
Intrathecal
•
Leptomeningeal seeding and/or free tumor cells in the
cerebrospinal fluid (CSF) most commonly occur with acute
lymphocy@c, and myelogenous leukemia, lymphomas, and
carcinomas
•
Intraventricular Therapy
•
Intra-arterial Therapy
•
primary and metasta@c to the liver
•
Intravesical therapy
•
BCG for T1 Ca Bladder
•
Wafers eluLng BCNU
•
surgically implanted into resec@on sites have been used as part of
mul@modality therapy for gliomas
•
Intrapleurally
•
for sclerosis of malignant pleural effusions
Chemotherapeutic Agents
•
Cell Cycle Specific Drugs:
•
Antimetabolites
•
Bleomycin peptide antibiotics
•
Vinca alkaloids
•
Cell Cycle non-Specific Drugs:
•
Alkylating agents
•
Antibiotics (Dactinomycin)
•
Cisplatin
Effective for high growth-
fraction-malignancies, such
as hematologic cancers.
Effective for both low-growth
(solid tumors) and high
growth fraction malignancies
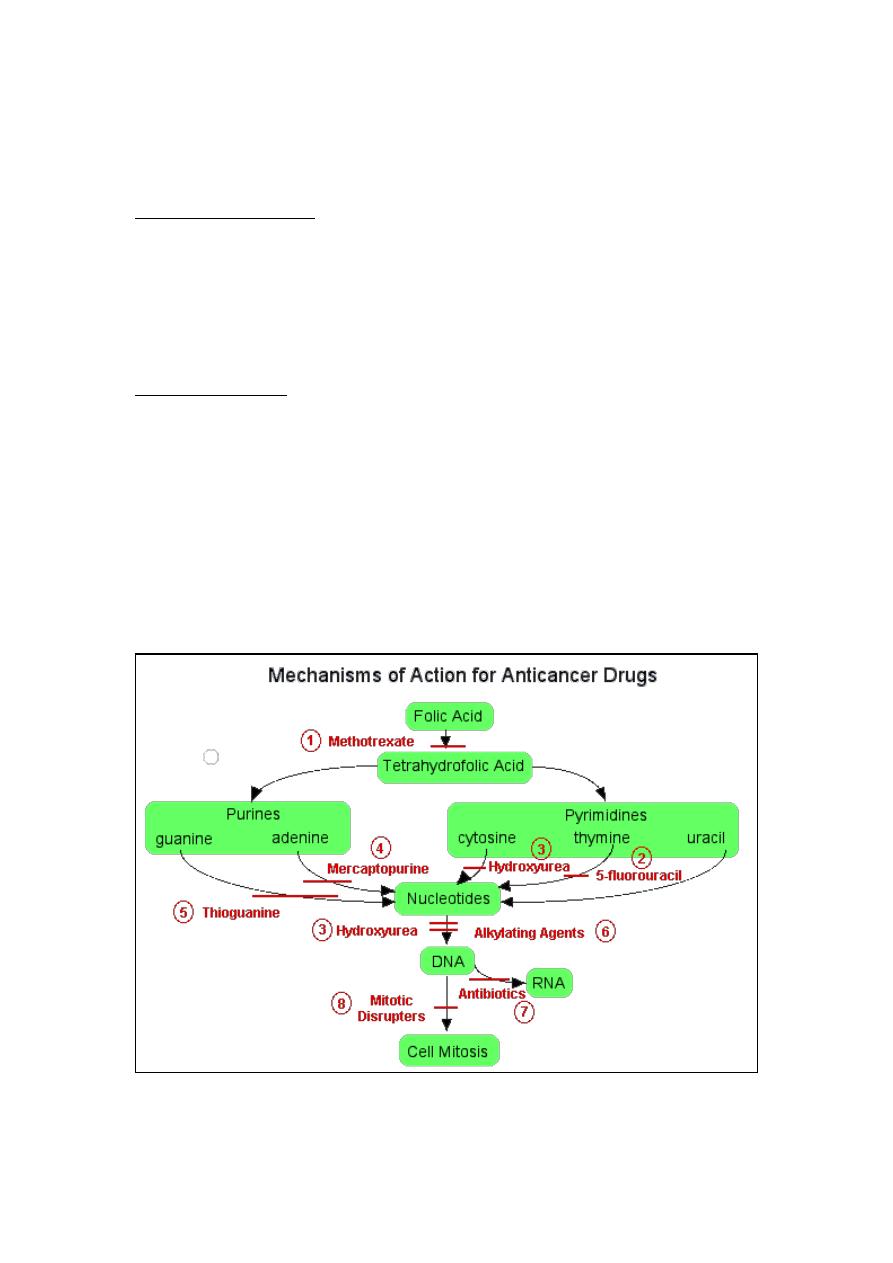
Drugs according to cell-cycle effects
Cell cycle Agents
Cell cycle nonspecific: Nitrogen mustards, aziridines,
nitrosoureas, alkyl alkane
sulfonates, nonclassic alkyla@ng agents, anthracyclines,
ac@nomycins, anthracenediones
Cell cycle specific:
S Bleomycin, an@metabolites, camptothecins, epipodophyllotoxins
G2 Bleomycin, epipodophyllotoxins
M Vinca alkaloids, taxanes
Chemotherapeutic Agents

1-Alkylating agents:
Cyclophosphamaide
Carbopla@n
Cispla@n
Oxalipla@n
Dacarbazine
•
Major interac@on: Alkyla@on of DNA
•
Binds to nucleophilic groups on various cell cons@tuents. Including
DNA
•
These drugs react with carboxyl, sulgydryl, amino, hydroxyl, and
phosphate groups of cellular cons@tuents.
•
Primary DNA alkyla@on site: N7 posi@on of guanine (other sites as
well)
•
Major Toxicity: bone marrow suppression
2.Antimetabolites:
5-Fluoro Uracil
Gemcitabine
Cyterabine
Methotrexate
•
Structurally related to normal compounds that exist within the
cell.
•
Interfere with the availability of normal purine or pyrimidine
nucleo@de precursors, either by inhibi@ng their synthesis or by
compe@ng with them in DNA or RNA synthesis.
•
Their maximal cytotoxic effects are in S-phase and therefore are
cell-cycle specific.
3. Microtubule Inhibitors:
• Vinca Alkaloids
Vincris@ne
Vinblas@ne
Vinorelbine
• Taxanes
Paclitaxel
Docetaxel
•
These are plant-derived substances .
•
Cause cytotoxicity by affec@ng the equilibrium between the
polymerized and depolymerized forms of the microtubules.
•
Vinca alkaloids inhibit microtubule polymeriza@on and increase
microtubule disassembly. The mito@c spindle apparatus is disrupted,
and segrega@on of chromosomes in metaphase is arrested.
4-Antineoplastic Antibiotics:
Bleomycin
Doxorubicin
Dac@nomycin
Daunorubicin
•
Interacts with DNA, leading to disrup@on of DNA func@on.
•
Also Inhibit topoisomerases (I and II) and produce free radicals.
•
Cell-cycle nonspecific.
•
Eg: Ac@nomycin D binds with double-stranded DNA and blocks the
ac@on of RNA polymerase, which prevents DNA transcrip@on.
5.
Hormonal Agents:
Prednisolone
Tamoxifen
Estrogens
Flutamide
Nilutamide
Bicalutamide
•
Commonly involves the use of glucocor@coids.
•
Direct an@tumor effects are related to their lympholy@c
proper@es;.
•
Glucocor@coids can inhibit mitosis, RNA synthesis, and
protein synthesis in sensi@ve lymphocytes.
•
Considered cell-cycle nonspecific .
•
Resistance to a given glucocor@coid may develop rapidly
and typically extends to other glucocor@coids.
6. Targeted therapy:
Rituximab
Trastuzumab
Cetuximab
Bevacizumab
Interleukin
Interferone
ima@nibe
•
Biologic response modifiers (e.g., interferon ± and interleukin 2,)
an@bodies, and targeted agents of several types. In addi@on, gene
therapy and an@sense approaches
•
An@bodies or molecules that are made in the lab rather than by a
person's own immune system.
•
Directed at specific targets and o:en have fewer adverse effects.

•
Designed to recognise and find specific abnormal proteins on
cancer cells.
•
Each monoclonal an@body recognizes one par@cular protein.
•
Three types of monoclonal A-bodies:
1. Trigger the immune system to aZack and kill cancer cells. E.g.
Rituximab (Mabthera)
2. Stop cancer cells from taking up protein E.g. Trastuzumab
(Hercep@n).
3. Carry cancer drugs or radia@on to directly to cancer cells These
are called conjugated MABs. E.g. Ibritumomab (Zevalin)
CANCER CHEMOTHERAPEUTIC DRUGS WITH
RADIATION SENSITIZER PROPERTIES
•
5-Fluorouracil
•
Gemcitabine
•
Cispla@n, carbopla@n
•
Paclitaxel
•
CPT-11, topotecan
•
5-bromodeoxyuridine, 5-iododeoxyuridine
The End
Done By : Hussein Sadun Al-Nuaimy
Rituximab
Trastuzumab
Cetuximab
Bevacizumab
