pathology of female reproductive system
Diseases of vulvaVULVITIS
The five most important infectious agents producing vulvitis are:
human papilloma virus (HPV),
herpes genitalis
gonococcal
syphilis
candidal vulvitis.
TUMORSCondylomas and Vulvar Intraepithelial Neoplasia (VIN)
condylomata acuminata (anogenital warts) is strongly associated with HPV 6 and HPV 11may be papillary and elevated or flat
few millimeters to many centimeters
red-pink to pink-brown
Histologically: perinuclear cytoplasmic
vacuolization with nuclear angular pleomorphism
and koilocytosis
they are not precancerous.
High-Grade (VIN) & Carcinoma of the Vulva
two biologic forms of vulvar carcinoma
1-seen in relatively younger patients, in cigarette smokers
type 16 is present in 75% to 90% of cases
coexisting vaginal or cervical carcinoma, carcinoma in situ.
the tumor tend to be poorly differentiated squamous cell carcinoma
Vulvar carcinoma
2-occurs in older women. it is not associated with HPV,unifocal lesion
the overlying epithelium lacks the typical cytologic changes of VIN,
it may display dyskeratotic cells.
tumors tend to be well differentiated and highly keratinizing.
VAGINITIS
A relatively common clinical problemusually transient
not serious.
produces a vaginal discharge (leukorrhea).
cause by bacteria, fungi& parasites.
ppt factors include DM, systemic antibiotic therapy ,after abortion or pregnancy, or in elderly persons with compromised immune function, and in patients with the acquired immunodeficiency syndrome.
Vaginal intraepithelial neoplasia and squamous cell carcinoma
Occur in women older than age 60 years
A preexisting or concurrent CIN or cervical ca is frequently present.
PREDISPOSING FACTORS:
HPV infection detected in nearly all cases of vaginal intraepithelial neoplasia & more than half of cases of invasive squamous cell carcinoma of the vagina.
Diethylstilbestrol: vaginal clear cell adenocarcinoma, usually encountered in young women whose mothers took diethylstilbestrol during pregnancy.
vaginal adenosis: small glandular or microcystic inclusions appear in the vaginal mucosa appear as red granular foci and are lined by mucus-secreting or ciliated columnar cells. from such inclusions that the rare clear cell adenocarcinoma arises.
CERVICITIS
Extremely commonAssociated with a mucopurulent to purulent vaginal discharge
These inflammations have been variously subdivided into noninfectious and infectious cervicitis.
Many of infectious agents are transmitted sexually like GC, chlamydia trachomatis, Tricho. vaginalis, Herpis simplex type II…….
TUMORS OF THE CERVIXCervical Intraepithelial Neoplasia (CIN) and Squamous Cell Carcinoma
nearly all invasive cervical squamous cell carcinomas arise from precursor epithelial changes referred to as CIN.N.B: not all cases of CIN progress to invasive cancer, and indeed many persist without change or even regress.
since the introduction of the papanicolaou (PAP) smear 50 years ago, the incidence of cervical cancer has decreased.
In populations that are screened regularly, cervical cancer mortality is reduced by as much as 99%.
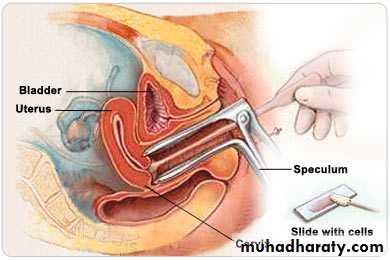
Pap smear
Cervical Intraepithelial NeoplasiaCIN
CIN I: mild dysplasiaCIN II: moderate dysplasia
CIN III: severe dysplasia & carcinoma in situ
low-grade squamous intraepithelial lesions (LSIL)= CIN I
high-grade squamous intraepithelial lesions(HSIL)= CIN II or III
The higher the grade of CIN, the greater the likelihood of progression to cancer.
Epidemiology and Pathogenesis
the peak age incidence of CIN is about 30 yearsthe peak age incidence of invasive carcinoma is about 45 years.
precancerous changes usually take many years, perhaps decades, to evolve into overt carcinomas.
Risk factors for the development of CIN and invasive carcinoma
1-Early age at first intercourse2-multiple sexual partners
3-A male partner with multiple previous sexual partners.
4-persistent infection by "high-risk" papillomaviruses.
higher incidence in lower socioeconomic groups,
Rare among virgins, and the association with multiple pregnancies.
HPV can be detected by molecular methods in nearly all precancerous lesions and invasive cervical carcinoma.
certain high-risk HPV types, including 16, 18, 45&31account for the majority of cervical Ca.
while in condylomas, which are benign lesions, are associated with infection by low-risk HPV types( 6, 11, 42, and 44)
although many women harbor these viruses, only a few develop cancer, suggesting other influences on cancer risk. among the other well-defined risk factors are cigarette smoking and exogenous or endogenous immunodeficiency
Morphology
CIN I or flat condyloma. this lesion is characterized by koilocytotic changes mostly in the superficial layers of the epithelium.koilocytosis, is composed of nuclear hyperchromasia and angulation with perinuclear vacuolization produced by cytopathic effect of HPV.
In CIN II the dysplasia is more severe, with maturation of keratinocytes delayed into the middle third of the epithelium.
It is associated with some variation in cell and nuclear size, heterogeneity of nuclear chromatin and mitoses above the basal layer, extending in to the middle third of the epithelium.
In CIN III ( carcinoma in situ) there is greater variation in cell and nuclear size, marked chromatin heterogeneity, disorderly orientation of the cells, and normal or abnormal mitoses; these changes affect virtually all layers of the epithelium and are characterized by loss of maturation. differentiation of surface cells and koilocytotic changes have usually disappeared
CIN I, II and III
Invasive Carcinoma of the Cervixthe most common cervical carcinomas are squamous cell carcinomas (75%), followed by adenocarcinomas and adenosquamous carcinomas (20%), and small-cell neuroendocrine carcinomas (<5%).
the squamous cell lesions are increasingly appearing in younger women, now with a peak incidence at about 45 years, some 10 to 15 years after detection of their precursors.
the only reliable way to monitor the course of the disease is with careful follow-up and repeat biopsies.
The relative proportion of adenocarcinoma has been increasing in recent decades; glandular lesions are not detected well by pap smear and other screening techniques.
Morphology
invasive carcinomas of the cervix develop in the region of the transformation zone .range from microscopic foci of early stromal invasion to grossly conspicuous tumors encircling the os.
Clinically
Seen in women who have never had a pap smear or who have not been screened for many years.
Vaginal bleeding, leukorrhea, painful coitus (dyspareunia), or dysuria
Mortality is strongly related to tumor stage and, to cell type.
Most patients with advanced disease die as a result of local invasion rather than distant metastasis.