
Medicine
Dr. Zuhair
Neurology
“
Myasthenia Gravis
”
Dr. Zuhair
LECTURE 14

Myasthenia Gravis Dr. Zuhair
3
Myasthenia Gravis
Objectives
To be familiar with presentation of MG
To appreciate the potential danger of MG
To recognize the types of crises in MG
To know about prevention of crises
To know about the initial management of crises in MG.
To know about inpatient follow up
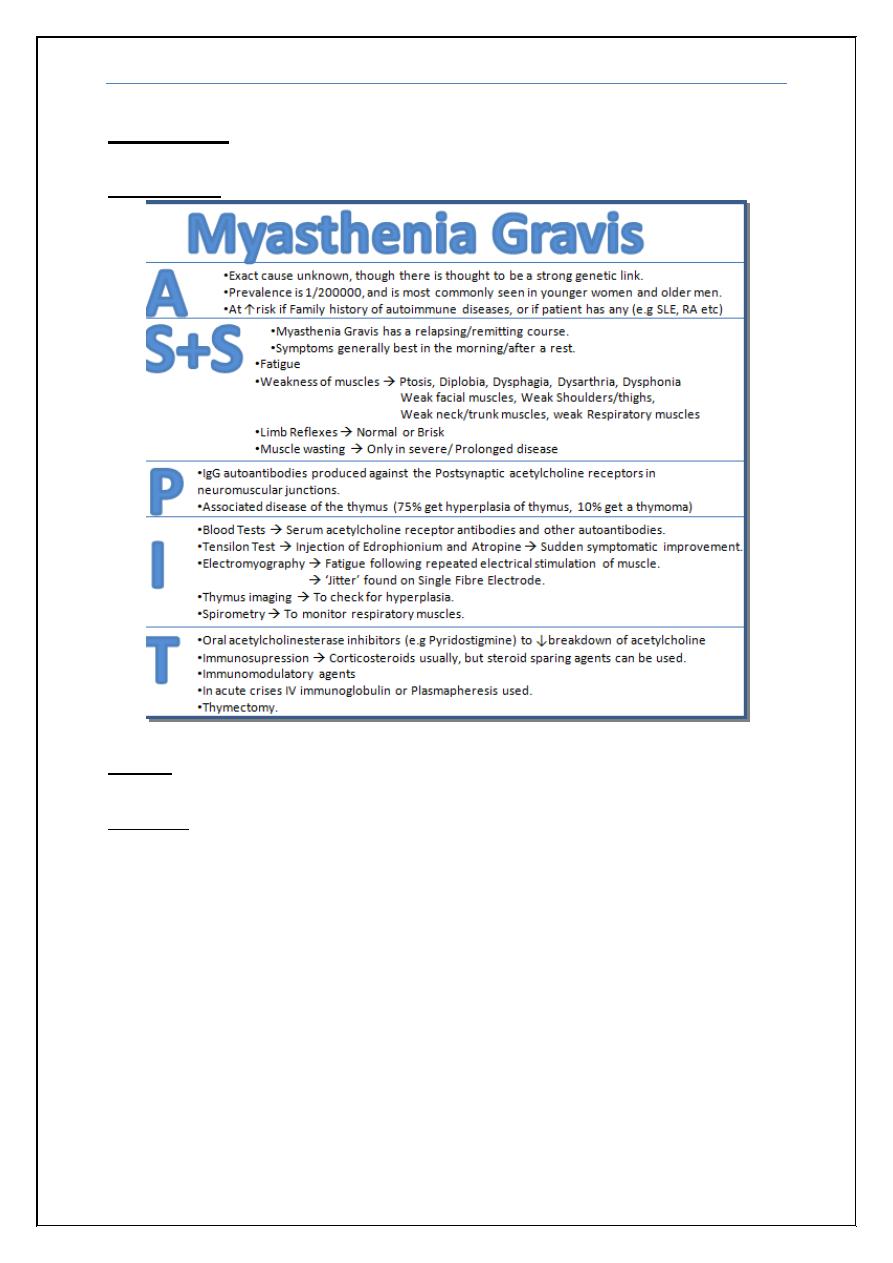
Definition
Myasthenia gravis is a chronic autoimmune neuromuscular disease
characterized by varying degrees of weakness of the skeletal (voluntary)
muscles of the body. The name myasthenia gravis, which is Latin and Greek in
origin, literally means "grave muscle weakness", as it used to be a fatal disease
before drugs development.
Pathophysiology/ Mechanism
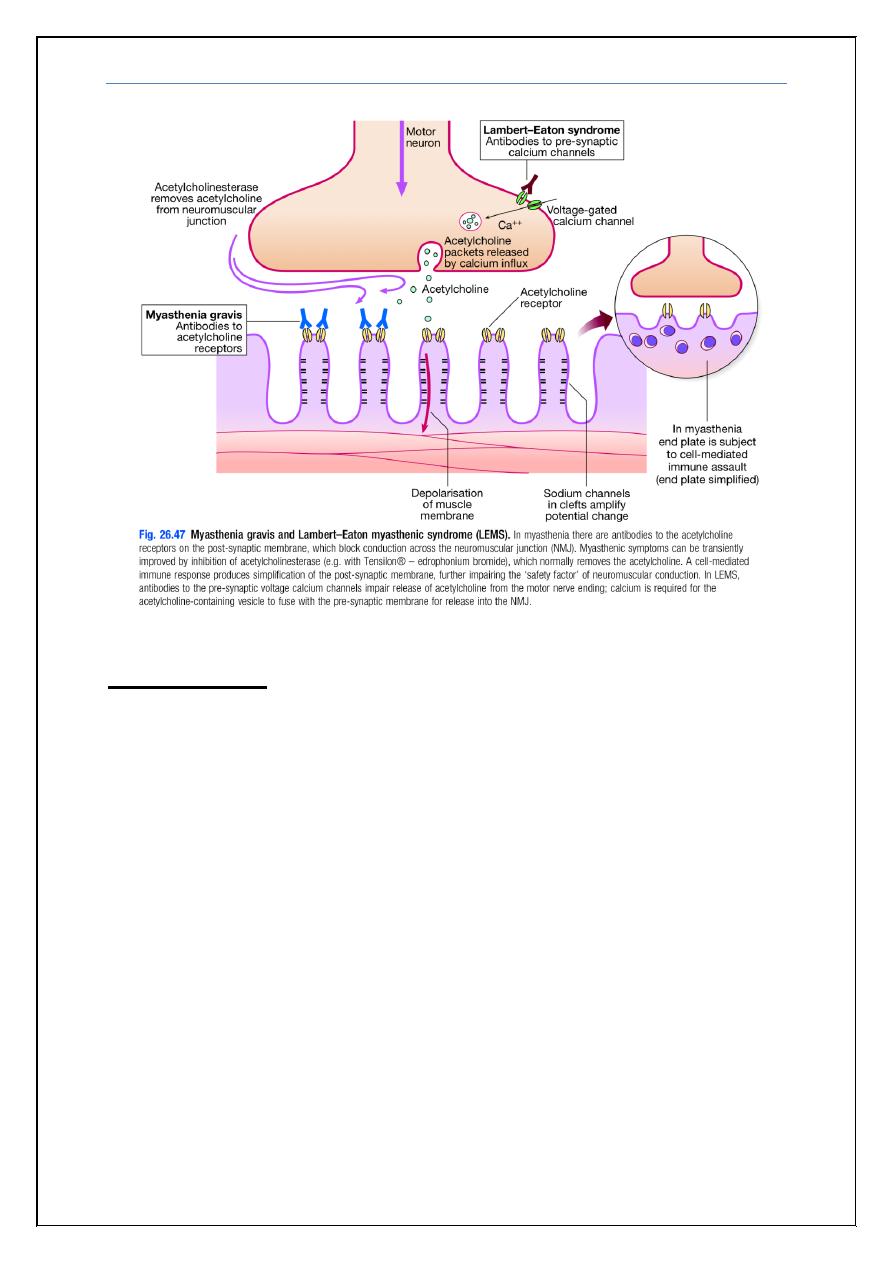
Myasthenia gravis is an autoimmune disease, most commonly caused by
antibodies to acetylcholine receptors in the post-junctional membrane of the
neuromuscular junction, which are found in around 80% of affected patients.
The resultant blockage of neuromuscular transmission and complement-
mediated inflammatory response reduces the number of acetylcholine receptors
and damages the end plate.
About 15% of patients (mainly those with late onset) have a thymoma,
most of the remainder displaying thymic follicular hyperplasia. Myasthenic
patients are at greater risk of associated organ-specific autoimmune diseases. As
with other autoimmune processes, triggers are not always evident, but some
drugs (e.g. penicillamine) can trigger an antibody-mediated myasthenic
syndrome that may persist after drug withdrawal.
Note
: This lecture has been extensively edited by the students and contains much
more information than the one presented by the doctor, if you want you can find the
original unedited lecture in muhadharaty.com as a pdf or a slideshow.
Myasthenia Gravis Dr. Zuhair
4
Clinical picture
Myasthenia gravis usually presents between the ages of 15 and 50 years and
there is a female preponderance in younger patients. In older patients, males
are more commonly affected. It tends to run a relapsing and remitting
course.
The most evident symptom is fatigable muscle weakness; movement is
initially strong but rapidly weakens as muscle use continues. Worsening of
symptoms towards the end of the day or following exercise is characteristic.
There are no sensory signs or signs of involvement of the CNS.
The first symptoms are usually intermittent ptosis or diplopia, but
weakness of chewing, swallowing, speaking or limb movement also occurs.
Any limb muscle may be affected, most commonly those of the shoulder girdle;
the patient is unable to undertake tasks above shoulder level, such as combing
the hair, without frequent rests. Respiratory muscles may be involved and
respiratory failure is an avoidable cause of death. Aspiration may occur if
the cough is ineffectual. Ventilatory support is required where weakness is
severe or of abrupt onset.
Myasthenia Gravis Dr. Zuhair
5
Diagnosis
Because weakness is a common symptom of many other disorders, the
diagnosis of myasthenia gravis is often missed or delayed (sometimes up to two
years) in people who experience mild weakness or in those individuals whose
weakness is restricted to only a few muscles.
The first steps of diagnosing myasthenia gravis include a review of the
individual's medical history, and physical and neurological examinations. The
physician looks for impairment of eye movements or muscle weakness without
any changes in the individual's ability to feel things (intact sensation). If the
doctor suspects myasthenia gravis, several tests are available to confirm the
diagnosis
.
Bed side tests:
1) Tensilon’s: Intravenous injection of the short-acting anticholinesterase,
edrophonium bromide will lead to improvement in muscle function
occurs within 30 seconds and usually persists for 2–3 minutes, but the test
is not universally specific or sensitive.
2) Simpson’s: if the patient looks upward for 20 seconds or more the ptosis
will increase.
Repetitive stimulation during nerve conduction studies:
This test records weakening muscle responses (decremental response) when the
nerves are repetitively stimulated by small pulses of electricity.
Antibodies measurement:
A special blood test can detect the presence of immune molecules or
acetylcholine receptor antibodies. Most patients with myasthenia gravis have
abnormally elevated levels of these antibodies. Recently, a second antibody—
called the anti-MuSK antibody—has been found in about 30 to 40 percent of
individuals with myasthenia gravis who do not have acetylcholine receptor
antibodies.
Single fiber electromyography (EMG)
Can detect impaired nerve-to-muscle transmission.
Computed tomography (CT) or magnetic resonance imaging (MRI)of the chest
Used to identify the presence of a thymoma.
Thyroid function test and Connective tissue screen
Because myasthenic patients are at greater risk of associated organ-specific
autoimmune diseases.
Myasthenia Gravis Dr. Zuhair
6
Crises (types, diagnosis, management and prevention)
Myasthenic:
More common than cholinergic crises
occurs when the muscles
that control breathing weaken to the point that ventilation is inadequate;
creating a medical emergency and requiring a respirator for assisted ventilation
it occurs due to exacerbation of the disease. (it may be the first presentation)
Cholinergic: Rare, due to over dosage of anticholinesterase drugs this will
increase the amount of acetylcholine available. Clinically they presents with
sweating, salivation, bronchial secretions, miosis and bradycardia (The doctor
mentioned that these symptoms can also occur in myasthenic crises).
Diagnosis: These crises can be distinguished by the clinical features and, if
necessary, by the injection of a small dose of edrophonium (Tensilon’s test) if
symptoms improve then it is myasthenic crises.
Management
Myasthenic: RCU, Intubation, IVIg and Plasmapharesis
Cholinergic: RCU and Intubation
Prevention
Immunomodulation
IVIg
Plasmapharesis
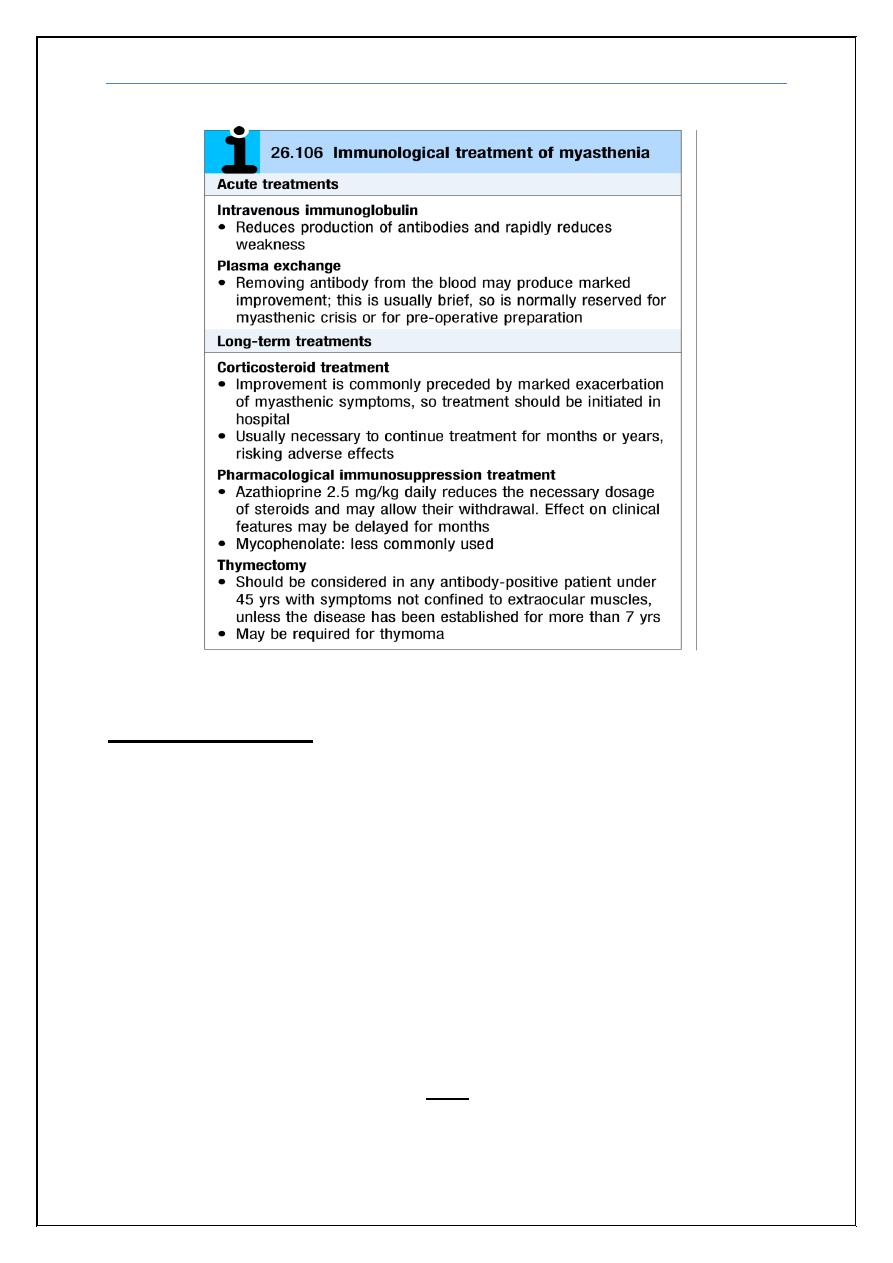
Treatment
The goals of treatment are to maximize the activity of acetylcholine at
remaining receptors in the neuromuscular junctions and to limit or abolish the
immunological attack on motor end plates. The duration of action of
acetylcholine is prolonged by inhibiting acetylcholinesterase. The most
commonly used anticholinesterase drug is pyridostigmine. Muscarinic side-
effects, including diarrhea and colic, may be controlled by propantheline.
Immunosuppressive drugs such as prednisone, azathioprine, cyclosporin,
mycophenolate mofetil, and tacrolimus may also be used. These medications
improve muscle strength by suppressing the production of abnormal antibodies.
Myasthenia Gravis Dr. Zuhair
7
Inpatients follow up
Counting up to 20 in one breath (when patient cant there is danger of
going into crises)
Forced Vital Capacity: 30mL/kg (if less intubate)
Check for cholinergic hyperstimulation
Check for side effects of IVIg (nephritis, septic meningitis and
allergy) and Plasmapharesis (hypocalcemia)
Check for side effects of steroids
Treat infection aggressively (risk of going into crises)
Prevent Veno-Thromboembolic phenomena (by low molecular weight
heparin).
End
Myasthenia Gravis Dr. Zuhair
8
Appendix
:
In summary:
Cases
:
Case (1)
A 21-year-old female comes to the office for the evaluation of fatigue and weakness. She
first noticed these symptoms nine months ago. She says, "I can't exercise a lot anymore
because I get fatigued very easily, but after resting for a while, I feel better, and my
fatigue disappears." She then describes a recent episode of weakness while swimming in a
pool, where she experienced double vision (especially when she did not look straight
ahead), difficulty raising her eyelids, and swallowing problems. What is the most likely
diagnosis?
A. Amyotrophic lateral sclerosis
B. Myasthenia gravis
C. Brain tumor
D. Multiple sclerosis
E. Duchenne muscular dystrophy
Myasthenia Gravis Dr. Zuhair
9
Explanation
Myasthenia gravis is most common in women between the ages of 18 and 25. Patients
typically present with intermittent dysarthria, dysphagia, drooping eyelids (ptosis), and
diplopia. Generalized weakness often develops (trunk, arms, and legs) within a year of onset.
Weakness tends to worsen as the day progresses. The resolution of muscular weakness with
rest is a hallmark feature of myasthenia gravis.
So the answer is B
Case (2)
A 37 -year-old white female with myasthenia gravis presents to the office with a fever and
cough productive of yellow-green sputum. She has been on pyridostigmine for the past few
months. She refuses to have a thymectomy. Her pulse is 90/min, blood pressure is 120/76 mm
Hg, respirations are 18/min, and temperature is 38.9C (102F). Her respiratory effort is
weak. Pulse oximetry reveals 86% oxygen saturation on room air. There is a consistent
decline on serial measurement of vital capacity. Which of the following is the most
appropriate next step in management?
A. Increase the dose of pyridostigmine
B. Treatment with edrophonium
C. Treatment with atropine
D. Treatment with prednisolone
E. Endotracheal intubation
Explanation:
The above patient is most likely suffering from myasthenia crisis. Myasthenia crisis is a life-
threatening condition that is characterized by weakness of the respiratory and pharyngeal
muscles. The treatment of all patients includes endotracheal intubation and withdrawal of
anticholinesterases for several days. The most common cause of myasthenic crisis is an
intercurrent infection, and in such cases antibiotics are an important part of management. All
patients with suspected myasthenic crisis should have bedside pulmonary function tests
monitored, such as vital capacity and tidal volume.
So the answer is E
Case (3)
A 56-year-old Caucasian male presents with ptosis, diplopia and limb weakness. These
symptoms worsen in the evening and with exercise, and improve with rest. He also has
fatigue, which is worse in the evening. He denies any tingling or numbness. On
examination, he cannot sustain an upward gaze, and his eyelids tend to drift downward
Which of the following is the best initial treatment for this patient?
A. Pyridostigmine
B. Edrophonium
C. Atropine
D. Prednisone
E. Intravenous immunoglobulins
Myasthenia Gravis Dr. Zuhair
10
Explanation:
There are three treatment options available for the treatment of myasthenia gravis. These
include acetylcholinesterase inhibitors (anticholinesterases), immunosuppressive agents
and thymectomy. Anticholinesterases provide symptomatic benefit, but do not induce
remission. Immunosuppressive agents and thymectomy may induce remission. The choice of
treatment depends on the patient's age and the clinical scenario.
Oral anticholinesterase is usually the initial treatment of choice for myasthenia gravis.
It produces its useful effect by increasing the availability of acetylcholine at the
neuromuscular junction, where the number of acetylcholine receptors is reduced due to
acetylcholine receptor antibodies. Pyridostigmine or neostigmine is used for treatment
purposes. Side effects include abdominal cramps, fasciculations and muscular weakness.
So the answer is A
Case (4)
A 65-year-old bedridden woman is brought in with complaints of weight loss, weakness
and malaise. Her past medical history includes chronic obstructive pulmonary disease
(diagnosed fifteen years ago) and hypertension of ten years' duration. She quit smoking two
years ago but previously smoked three packs of cigarettes daily since she was 20 years of
age. Her vital signs are stable. Her physical examination reveals severe weakness in her
proximal muscles and loss of deep tendon reflexes. Chest x-ray shows a right upper lung
mass with mediastinal lymphadenopathy. Creatine phosphokinase (CPK) level is normal.
Which of the following is the most likely cause of her weakness?
A. Autoantibodies against post synaptic receptors
B. Immune mediated muscle inflammation
C. Upper and lower motor neuron degeneration
D. Multicentric CNS inflammation and demyelination
E. Antibodies to voltage gated calcium channels
Explanation:
This patient's history (i.e. heavy smoking. weight loss) and physical findings (i.e. proximal
muscle weakness. malaise. lung mass) are suggestive of Myasthenic or Lambert-Eaton
syndrome which can occur in association with small cell carcinoma of the lung. Lambert-
Eaton syndrome is caused by autoantibodies that are directed against the voltage-gated
calcium channels in the presynaptic motor nerve terminal. This leads to the defective release
of acetylcholine thereby leading to proximal muscle weakness. Electrophysiological studies
confirm the diagnosis (the muscle response to motor nerve stimulation should increase with
repetitive stimulation). Treatment consists of plasmapheresis and immunosuppressive drug
therapy
So the answer is E
