Transport Process Affecting Renal Clearance
Renal clearance refers to the ability of the kidneys to remove molecules from the blood plasma by excreting them in the urine.Molecules and ions dissolved in the plasma can be filtered through the glomerular capillaries and enter the glomerular capsules. Then, those that are not reabsorbed will be eliminated in the urine; they will be “cleared” from the blood.
The process of filtration, a type of bulk transport through capillaries, promotes renal clearance. The process of reabsorption—involving membrane transport by means of carrier proteins—moves particular molecules and ions from the filtrate into the blood, and thus reduces the renal clearance of these molecules from the blood.
There is another process that affects renal clearance, a membrane transport process called secretion. In terms of its direction of transport, secretion is the opposite of reabsorption—secreted molecules and ions move out of the peritubular capillaries into the interstitial fluid, and then are transported across the basolateral membrane of the tubular epithelial cells and into the lumen of the nephron tubule. Molecules that are both filtered and secreted are thus eliminated in the urine more rapidly (are cleared from the blood more rapidly) than molecules that are not secreted.
Renal handling with substances:
Renal clearance provides a useful way of quantifying the excretory function of the kidneys and can be used to quantify the rate at which blood flows through the kidneys as well as the basic functions of the kidneys.Inulin, a polysaccharide which is not produced in the body, is found in the roots of certain plants and must be administered intravenously to a patient to measure GFR. It is freely filtered, no absorption or secretion and not metabolized and non-toxic but its use is for research purposes only. The rate of inulin clearance is equal to the GFR which is about 125ml/min.
Substance is
exampleRenal clearance rate
Not filtered
proteins
zero
Filtered not reabsorbed or secreted
inulin
Equal to GFR
Filtered but partially reabsorbed
Urea
Less than GFR
Filtered but completely reabsorbed
Glucose
Zero
Filtered , reabsorbed, and secreted
K+
Variable
Other substances used to measure GFR but less accurate like plasma creatinine which is mildly secreted along the proximal tubule. Creatinine is a by-product of muscle metabolism and is cleared from the body fluids almost entirely by glomerular filtration. Therefore, the clearance of creatinine can also be used to assess GFR. Because measurement of creatinine clearance does not require intravenous infusion into the patient, this method is much more widely.
Tubular load:
Each substance is absorbed according to transport system, so once the transport system reaches a maximum, the substance will appear in urine (not re-absorbed). The renal plasma threshold is the minimum plasma concentration of a substance that results in the excretion of that substance in the urine. An important example is the urine glucose. In normal people; urine glucose is zero because plasma glucose concentrations normally remain below this threshold value. The renal plasma threshold for glucose is 180 to 200 mg per 100 ml. This means that at plasma glucose above 200mg/min glucose will start to appear in urine (a condition called glycosuria) and this is seen in uncontrolled diabetes mellitus.
Hyperglycemia (increased plasma glucose level) is caused by the inadequate secretion or action of insulin. When this hyperglycemia results in glycosuria, the disease is called diabetes mellitus. A person with uncontrolled diabetes mellitus also excretes a large volume of urine because the excreted glucose carries water with it as a result of the osmotic pressure it generates in the tubules. This condition should not be confused with diabetes insipidus, in which a large volume of dilute urine is excreted as a result of inadequate ADH secretion.
The tubular maximum (Tm) is the maximum capacity of the tubule to execrate a substance. The Tm for glucose is 320 mg/min. this number represents the maximum capacity of the tubules to execrate glucose and any increase of tubular glucose above this number no increase will appear in glucose execration. This means that if the plasma glucose is 400mg/ml or even higher the renal glucose will stop at 320.
Diabetes insipidus:
A disease associated with the inadequate secretion or action of ADH. When the secretion of ADH is adequate, but a genetic defect in the ADH receptors or the aquaporin channels renders the kidneys incapable of responding to ADH, the condition is called nephrogenetic diabetes insipidus. Without proper ADH secretion or action, the collecting ducts are not very permeable to water, and so a large volume (5 to 10 L per day) of dilute urine is produced.
The dehydration that results causes intense thirst, but a person with this condition has difficulty drinking enough to compensate for the large volumes of water lost in the urine. In this case the specific gravity and the osmolarity of the urine are very low.
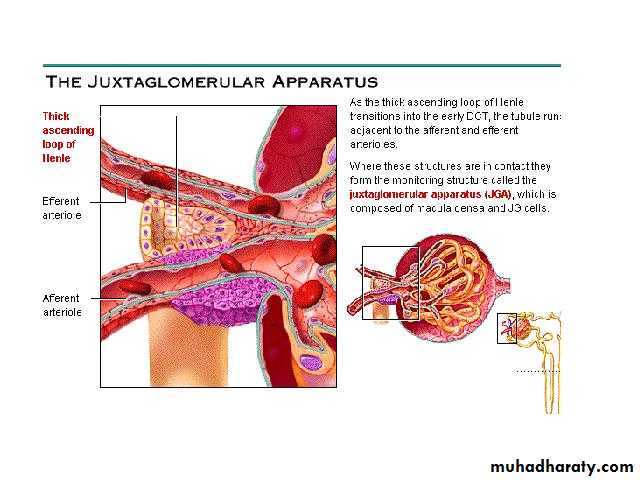
Juxtaglomerular Apparatus
Two parts:1. The region in each nephron where the afferent arteriole comes into contact with the last portion of the thick ascending limb of the loop, there are Granular cells within the afferent arteriole secrete the enzyme renin into the blood; this enzyme catalyzes the conversion of angiotensinogen (a protein) into angiotensin I (a ten-amino-acid polypeptide).
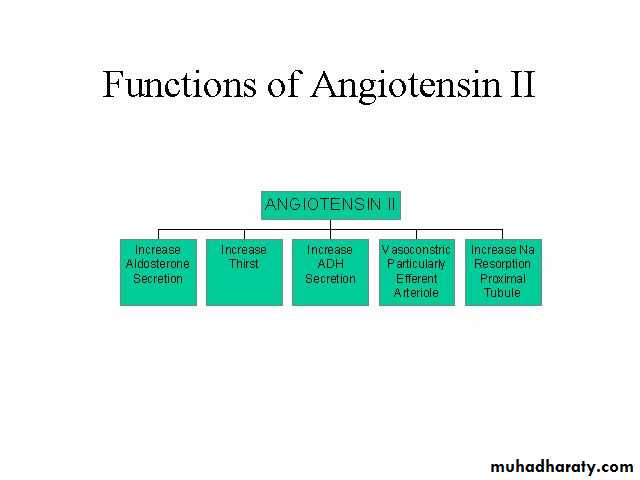
Secretion of renin into the blood thus results in the formation of angiotensin I, which is then converted to angiotensin II (an eight-amino-acid polypeptide) by angiotensin-converting enzyme (ACE). This conversion occurs primarily as blood passes through the capillaries of the lungs, where most of the converting enzyme is present. Angiotensin II, in addition to its other effects, stimulates the adrenal cortex to secrete aldosterone. Thus, secretion of renin from the granular cells of the juxtaglomerular apparatus initiates the reninangiotensin- aldosterone system. Conditions that result in increased renin secretion cause increased aldosterone secretion and, by this means, promote the reabsorption of Na+ from cortical collecting duct into the blood.
2. The region of the ascending limb in contact with the granular cells of the afferent arteriole is called the macula densa.
There is evidence that this region helps to inhibit renin secretion when the blood Na+ concentration is raised.
The cells of the macula densa respond to the Na+ in the filtrate delivered to the distal tubule. When the plasma Na+ concentration is raised, or when the GFR is increased, the rate of Na+ delivered to the distal tubule is also increased. Through an effect on the macula densa, this increase in filtered Na+ inhibits the granular cells from secreting renin. Aldosterone secretion thus decreases, and since less Na+ is reabsorbed in the cortical collecting duct, more Na+ is excreted in the urine.
Regulation of Renin Secretion
Renin which converted to angiotensin II is like aldosterone in dealing with plasma Na+.
An inadequate dietary intake of salt (NaCl) or hyponatremia of any cause is always accompanied by a fall in blood volume. The fall in blood volume and the fall in renal blood flow that result cause increased renin secretion.
Increased renin secretion is believed to be due in part to the direct effect of blood pressure on the granular cells, which may function as baroreceptors in the afferent arterioles. Renin secretion is also stimulated by sympathetic nerve activity, which is increased by the baroreceptor reflex when the blood volume and pressure fall.
An increased secretion of renin acts, via the increased production of angiotensin II, to stimulate aldosterone secretion. Consequently, less sodium is excreted in the urine and more is retained in the blood.