Physiology Dr. Hanan Luay
The Reproductive systemObjectives:
Discuss the development of gonads?
What are the common chromosomal abnormalities?
What are the common hormonal abnormalities?
There are 46 chromosomes: in males, 22 pairs of autosomes plus an X chromosome and a Y chromosome; in females, 22 pairs of autosomes plus two X chromosomes. As a consequence of meiosis during gametogenesis, each normal ovum contains a single X chromosome, but half the normal sperms contain an X chromosome and half contain a Y chromosome .When a sperm containing a Y chromosome fertilizes an ovum, an XY pattern results and the zygote develops into a genetic male. When fertilization occurs with an X-containing sperm, an XX pattern and a genetic female result (so the sex of the resulting zygot is determined by the fertilizing sperm).
The differentiation of the primitive gonads into testes or ovaries in utero is genetically determined in humans, but the formation of male genitalia depends upon the presence of a functional, secreting testis; in the absence of testicular tissue, development is female. There is evidence that male sexual behavior and, in some species, the male pattern of gonadotropin secretion are due to the action of male hormones on the brain in early development.
Development of the Gonads
On each side of the embryo, a primitive gonad arises from the genital ridge. The gonad develops a cortex and a medulla. Until the sixth week of development, these structures are identical in both sexes i.e undifferentiated called bipotential gonads which contains primitive germ cells and has both male and female primordial genital ducts. After the 6th week the differentiation started. In genetic males, the medulla develops during the seventh and eighth weeks into a testis, and the cortex regresses. Leydig and Sertoli cells appear, and testosterone and mullerian inhibiting substance are secreted. In genetic females, the cortex develops into an ovary and the medulla egresses. It will not secret estrogen inutero, so the secondary sex organs will develop without any hormonal influence.
In a normal female fetus, the mullerian duct system then develops into uterine tubes (oviducts) and a uterus. In the normal male fetus, the wolffian duct system on each side develops into the epididymis and vas deferens. The external genitalia are similarly bipotential until the eighth week.When there are functional testes in the embryo, male internal and external genitalia develop. The Leydig cells of the fetal testis secrete testosterone (androgens), and the Sertoli cells secrete mullerian inhibiting substance (MIS; also called mullerian regression factor, or MRF). MIS causes regression of the mullerian ducts, and testosterone fosters the development of the vas deferens and related structures from the wolffian ducts. The testosterone metabolite induces the formation of male external genitalia and male secondary sex characteristics.Note that the determination of the internal sex organs is not under the influence of androgens, that’s why if we introduce androgen into a genetically female fetus, this does not influence the female pattern of the internal sex organ, but it will affect the external sex organ and it will show a male pattern.
ABERRANT SEXUAL DIFFERENTIATIONChromosomal Abnormalities
Abnormalities of sexual development could be caused by genetic or hormonal abnormalities or other teratogenic causes.
An established defect in gametogenesis is nondisjunction, a phenomenon in which a pair of chromosomes fails to separate, so that both go to one of the daughter cells during meiosis.
Examples of these abnormalities: 1- a syndrome called gonadal dysgenesis or, alternatively, ovarian agenesis or Turner's syndrome. In these individuals there is an XO chromosomal pattern, the gonads are rudimentary or absent, so that female external genitalia develop .Stature is short, webbing of the neck, other congenital abnormalities are often present, and no maturation occurs at puberty.
2- A syndrome known as seminiferous tubule dysgenesis or Klinefelter's syndrome. Individuals with the XXY pattern, the most common sex chromosome disorder, have the genitalia of a normal male. Testosterone secretion at puberty is often great enough for the development of male characteristics. However, the seminiferous tubules are abnormal, and there is a higher than normal incidence of mental retardation.
3-The XXX ("superfemale") pattern, it is more common in general population, since it does not seem to be associated with any characteristic abnormalities.
4-The YO combination is probably lethal and incompatible with life.
Nondisjunction or simple loss of a sex chromosome can occur during the early mitotic divisions after fertilization. The result of faulty mitoses in the early zygote is the production of a mosaic, an individual with two or more populations of cells with different chromosome complements. True hermaphroditism, the condition in which the individual has both ovaries and testes, is probably due to XX/XY mosaicism and related mosaic patterns, although other genetic aberrations are possible. Chromosomal abnormalities also include transposition of parts of chromosomes to other chromosomes. Sex chromosome abnormalities are, of course, not the only abnormalities associated with disease states; nondisjunction of several different autosomal chromosomes is known to occur. For example, nondisjunction of chromosome 21 produces trisomy 21, the chromosomal abnormality associated with Down's syndrome (mongolism). The additional chromosome 21 is normal, so Down's syndrome is a pure case of gene excess causing abnormalities. In most instances, nondisjunction occurs in the ovary rather than the testis and the incidence of Down's syndrome increases with advancing age of the mother. Hormonal Abnormalities
Development of the male external genitalia occurs normally in genetic males in response to androgen secreted by the embryonic testes.
Genetic females exposed to androgens from some other source during the eighth to the thirteenth weeks of gestation, may develop male genetalia. The syndrome that results is female pseudohermaphroditism. A pseudohermaphrodite is an individual with the genetic constitution and gonads of one sex and the genitalia of the other. After the thirteenth week, the genitalia are fully formed, but exposure to androgens can cause hypertrophy of the clitoris. Its causes either due to congenital virilizing adrenal hyperplasia ,or it may be caused by androgens administered to the mother.
Malepseudohermaphroditism:development of female external genitalia in genetic males. It occurs when the embryonic testes are defective. Because the testes also secrete MIS (mullerian inhibiting substance or mullerian regression factor), genetic males with defective testes have female internal genitalia.
Another cause of male pseudohermaphroditism is androgen resistance, in which, male hormones cannot exert their full effects on the tissues. One form of androgen resistance is a 5α-reductase deficiency, in which the enzyme responsible for the formation of the active form of testosterone is decreased.
Male pseudohermaphroditism also occurs when there is a congenital deficiency of 17α-hydroxylase (congenital blockage of the formation of pregnenolone from which testosterone formed)
This androgen resistance may also due to mutations in the androgen receptor gene and the resulting defects in receptor function ranges from minor to severe. Mild defects cause infertility with or without gynecomastia .
When the loss of receptor function is complete, the testicular feminizing syndrome, now known as complete androgen resistance syndrome, results. In this condition, MIS is present and testosterone is secreted at normal or even elevated rates. The external genitalia are female, but the vagina ends blindly because there are no female internal genitalia. Individuals with this syndrome develop enlarged breasts at puberty and usually are considered to be normal women until they are diagnosed when they seek medical advice because of lack of menstruation .i.e female external genetalia, male internal genetalia. Female reproductive system
Female reproductive functions can be divided into two major phases: (1) preparation of the female body for conception and pregnancy, and (2) the period of pregnancy itself.
Ovaries:
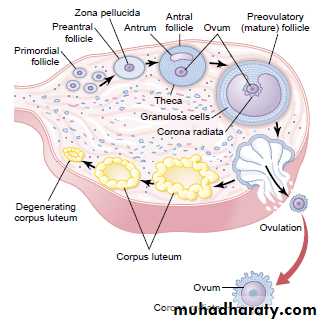
From the sixth week of intrauterine life the embryonic ovaries develop which contain the primordial follicles which are about 7000000 follicles, then the number regress during the next stages of life .the female needs only one ovum in each menstrual cycle.
Functions of the ovarian hormones—the ovary secrets 3 hormones:
Estrogens
Progestins
Relaxin
ESTROGENS: It is a steroid synthesized in the ovaries mainly from cholesterol and secreted by the ovarian theca interna cells, corpus luteum, fetoplacental units and small amounts by the adrenal cortices and the testes.
There are three estrogens present in significant quantities in the plasma of the human female: b-estradiol,estrone, and estriol, but The estrogenic potency of b- estradiol is more than the others, it is considered the major estrogen.
They are transported in the blood bound mainly with plasma albumin and with specific estrogen binding globulins.
During childhood, estrogens are secreted only in minute quantities, but at puberty, the quantity in the female under the influence of the pituitary gonadotropic hormones increases.
Functions of the Estrogens:
A primary function of the estrogens is to cause cellular proliferation and growth of the tissues of the sex organs and other tissues related to reproduction.
Effect of Estrogens on the Uterus and External Female Sex Organs.
Estrogens change the type cervical mucosa and change the vaginal epithelium from a cuboidal into a stratified type (more resistant to infection), the external genitalia enlarge. The size of the uterus will increase and the excitability of its muscle will increase also. It also cause marked proliferation of the endometrial stroma (especially in the first half of the menstrual cycle)
Effect of Estrogens on the Fallopian Tubes: it causes increase in the mobility of the fallopian tubes , also increase in the mobility and number of cilia which beat toward the uterus, and helps propel the fertilized ovum in that direction.
Effect of Estrogens on the Breasts.
It causes development of the stroma and the ductile tissue of the breast in addition to that it causes breast growth and gives the external appearance of the mature female breast (deposition of fat in the breasts). But its effect on the alveoli of the breast is to lesser extent because their final growth is under the effect of progesterone and prolactin.
Effect of Estrogens on the Skeleton.
It stimulates bone growth and inhibits osteoclastic activity. Also it causes uniting of the epiphyses with the shafts of the long bones. This effect of estrogen in the female is much stronger than the similar effect of testosterone in the male. As a result, growth of the female usually ceases several years earlier than growth of the male. A female eunuch who is devoid of estrogen production usually grows several inches taller than a normal mature female because her epiphyses do not unite at the normal time
After menopause and because of estrogen deficiency there will be decrease of the bone matrix (increase in osteoclastic activity) and osteoporosis usually occurs.
Effect of Estrogens on Protein Deposition. Estrogens cause a slight increase in total body protein since it stimulate sexual organ tissue and bone growth. Also it increases the whole-body metabolic rate slightly.
Female sexual characteristics: estrogen causes deposition of fat in the breasts and subcutaneous tissues, also in the buttocks and thighs (broad hip), which is characteristic of the feminine figure.
Effect of Estrogens on the Skin. Estrogens cause the skin to develop a texture that is soft and usually smooth, also it causes high ratio of scalp hair to the body hair. It makes sebaceous gland secretions more fluid and thus inhibits formation of blackheads and acne.
Effect of Estrogens on Electrolyte Balance. It Causes sodium and water retention by the kidney tubules, that’s why the female has increase in body weight just before the menstrual cycle, also during pregnancy there is retention of fluids because of the high estrogen.
Effects on the CNS
It exerts this action by a direct effect on certain neurons in the hypothalamus. Estrogens increase the proliferation of dendrites on neurons and the number of synaptic knobs.
Estrogen also causes decrease in the plasma cholesterol level, that’s why the incidence of ischemic heart disease in female is higher after menopause.
Progestins:
The most important of the progestins is progesterone. In the normal nonpregnant female, progesterone is secreted in significant amounts only during the latter half of each ovarian cycle (secretory phase), when it is secreted by the corpus luteum. Progesterone is also secreted by the placenta during pregnancy, especially after the fourth month of gestation. Small amounts of progesterone are excreted by the adrenal cortex and testes.Within a few minutes after secretion, it binds to plasma proteins then almost all the progesterone is degraded by the liver to other steroids that have no progestational effect. The major end product of progesterone degradation is pregnanediol which is excreted in urin after conversion to glucoronide. One can estimate the rate of progesterone formation in the body from the rate of this excretion.
Functions of Progesterone
Effect of Progesterone on the Uterus.It promotes secretory changes in the uterine endometrium during the latter half of the monthly female sexual cycle, thus preparing the uterus for implantation of the fertilized ovum. Also it decreases the frequency and intensity of uterine contractions, thereby helping to prevent expulsion of the implanted ovum. It decreases the frequency and intensity of uterine contractions (decrease the excitability of the uterine cells and their sensitivity to oxytocin), thereby helping to prevent expulsion of the implanted ovum. Therefore females with low progesterone are liable for abortion so we have to give them progestertone.
Effect of Progesterone on the Fallopian Tubes.
It promotes increased secretion by the mucosal lining of the fallopian tubes.
Effect of Progesterone on the Breasts.
Progesterone promotes development of the lobules and alveoli of the breasts, causing the alveolar cells to proliferate, enlarge, and become secretory in nature (but milk secretions will not occur until stimulated by prolactin). Progesterone also causes the breasts to swell (secretory development of alveoli and fluid in subcutaneous tissues).-Progesterone is a thermogenic hormone responsible for rising temperature at time of ovulation.
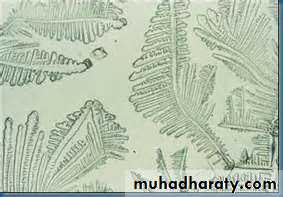
Estrogen makes the cervical mucosa thinner and more alkaline, these changes promotes survival and transport of sperms, while progesterone makes the secretion thick and the mucosa cellular, so the mucosa is thinnest at time of ovulation and rise in an arborizing fern like pattern when a thin layer spread on the slide while after ovulation and during pregnancy, it become thick and fail to form the fern like pattern.
3-Relaxin:
It is the third hormone secreted by from the corpus luteum of pregnancy .it relaxes the symphysis pubis and causes softening and relaxation of the cervix during pregnancy .it may also be secreted by the placenta and the uterus.Menstrual cycle:
Puberty and MenarchePuberty means the onset of adult sexual life.
Menarche means the beginning of the cycle of menstruation.
The period of puberty is caused by a gradual increase in gonadotropic hormone secretion by the pituitary, the onset of puberty and menstruation between ages 11 and 16 years in girls (average, 13 years).
Menstrual cycle is the regular cyclic changes which occur from puberty till menopause .the cycle extends from the first day of the period to the first day of the next.
The primordial follicles which were in the ovary from birth begin to ripe under the effect of FSH. There will be accelerated growth of 6 to 12 primary follicles each month. After a week or more of growth— but before ovulation occurs—one of the follicles begins to outgrow all the others; the remaining 5 to 11 will be atretic (regression of growth). The single follicle reaches a diameter of 1 to 1.5 centimeters at the time of ovulation and is called the mature follicle.
As the follicle grows there will be increase in ovarian secretion of estrogen ,and when the level of estrogen increases, it feeds back to the anterior pituitary and stimulate the release of FSH and LH (positive feedback effect) .By the day 13 of the cycle, the circulating level of LH increases sharply(it increases 2 days before ovulation), this LH surge is accompanied to lesser extent by an increase of FSH secretion also, this combination of gonadotropins bring about the final maturation of the of the ovarian follicles and ovulation . Ovulation in a woman who has a normal 28-day female sexual cycle occurs 14 days after the onset of menstruation. As the follicle ruptures, the ovum expelled into the abdominal cavity and trapped by the fimbrial ends of the fallopian tubes, where the fertilization occurs, and the fertilized ovum will be transported to the uterus where it becomes implanted.
After ovulation, the granulose and theca interna cells lining the follicles proliferate and replaced by luteal cells (filled with lipids which give the yellowish color) forming what is called corpus luteum which secrets estrogen and progesterone. So in the second half of the menstrual cycle the rise in estrogen is from the corpus luteum .This high level of estrogen and progesterone will feedback to the anterior pituitary and inhibit the release of FSH and LH (negative feedback effect), and loss of these hormones finally causes the corpus luteum to degenerate completely, So no more maintenance of the corpus luteum and no more maintenance of the lining endometrium, so shedding of the endometrium with drops of blood sudden cessation of secretion of estrogen, progesterone, by the corpus luteum removes the feedback inhibition of the anterior pituitary gland, allowing it to begin secreting increasing amounts of FSH and LH again. FSH and LH initiate the growth of new follicles, beginning a new ovarian cycle.
The period between the ovulation and the next cycle is usually 14 days, so any change in the period occurs in the first half of the cycle (i.e. the time between the start of the cycle and the ovulation is variable between women).
If the pregnancy occurs the corpus luteum persists (it persists because of the action of human chorionic gonadotrophinhCG secreted by the embryonic tissues) and continue to secret estrogen and progesterone, but after the 12th week the fetoplacental unit takes the function.
After fertilization the fertilized ovum reaches the uterine cavity in 3-4 days .During this time many or several mitotic divisions occur (it becomes what is called blastocyt about 100 cells), but not reach very large size because the opening of the fallopian tube is small but if it enlarges in the tube for any reason there will be ectopic pregnancy. But in normal conditions the fertilized ovum implanted in the uterine cavity in the 7th or 8th day after fertilization. Implantation results from the action of trophoblast cells that secrete proteolytic enzymes that digest the adjacent cells of the uterine endometrium.
After implantation the ovulation and menstruation is prevented by the secretion of human chorionic gonadotropin by the newly developing embryonic tissues, the secretion of this hormone can first be measured in the blood 8 to 9 days after ovulation or 6 days after fertilization (or in urine 14 days after fertilization), shortly after the blastocyst implants in the endometrium. Then the rate of secretion rises rapidly to reach a maximum at about 10 to 12 weeks of pregnancy and decreases back to a lower value by 16 to 20 weeks. It continues at this level for the remainder of pregnancy.
The function of human Chorionic Gonadotropin (hCG) is to prevent involution of the corpus luteum at the end of the monthly female sexual cycle. Instead, it causes the corpus luteum to secrete even larger quantities of its sex hormones—progesterone and estrogens—for the next few months.
Regarding the lining of the uterus, it passes through the following stages: (1) proliferation of the uterine endometrium; (2) development of secretory changes in the endometrium; and (3) desquamation of the endometrium, which is known as menstruation.
Proliferative Phase (Estrogen Phase) of the Endometrial Cycle, Occurring Before Ovulation
Under the influence of estrogens, secreted in increasing quantities by theovary during the first part of the monthly ovariancycle, the stromal cells and the epithelial cellsproliferate rapidly the endometrium increases greatly in thickness, owing to increasing numbers of stromal cells and to progressive growth of the endometrial glands and new blood vessels into the endometrium.
Secretory Phase (Progestational Phase) of the Endometrial Cycle, Occurring After Ovulation
Progesterone causes marked swelling and secretory development of the endometrium. The glands increase in tortuosity. Also, the cytoplasm of the stromal cells increases; lipid and glycogen deposits increase greatly in the stromal cells; and the blood supply to the endometrium further increases with the blood vessels becoming highly tortuous. The whole purpose of these endometrial changes is to prepare large amounts of stored nutrients to provide appropriate conditions for implantation of a fertilized ovum.
If the ovum is not fertilized, about 2 days before the end of the monthly cycle, the corpus luteum in the ovary suddenly involutes, and the ovarian hormones (estrogens and progesterone) decrease to low levels of secretion, Menstruation follows which lasts usually from 4-7 days (necrosis in the endometrium, especially of the blood vessels → bleeding about 40 ml of blood).