بسم الله الرحمن الرحيم
Prof. Dr. Huda Al-khateeb
Head of Histology Section/Dept. of AnatomyHead of Quality Assurance & Academic Performance
College of Medicine/Univ. of Baghdad
SKIN
To study layers of skin and the types of cells present in them.
objectives15–20% of total body weight
What is the heaviest organ in the body?1.5–2 m2
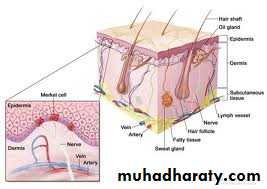
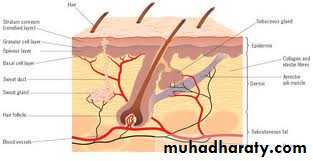
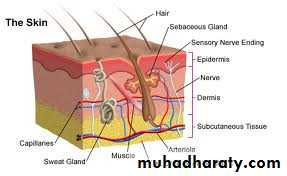
What is the largest organ in the body?Composed of:
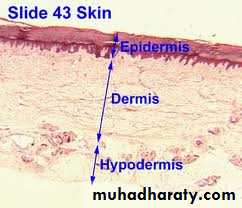
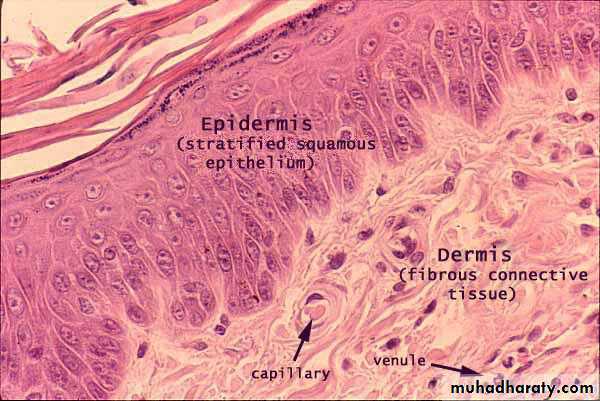
(1) the epidermis, an epithelial layer of ectodermal origin(2) the dermis, a layer of mesodermal connective tissue origin
the integument (L. integumentum, covering) or cutaneous layer
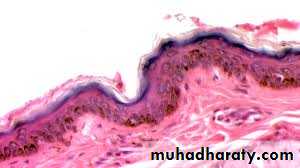
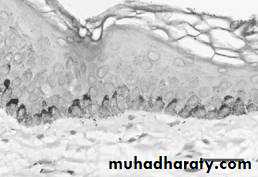
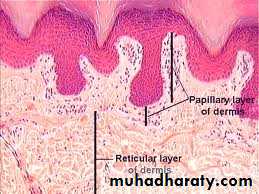
The boundries between dermis and epidermis is irregular
* projections of the dermis called papillae* inter-digitate with evaginations of the epidermis known as epidermal ridges.
Dermo-epidermalJunction
Beneath the dermis lies the
superficial fascia (of gross anatomy)subcutaneous tissue or hypodermis (Gr. hypo, under, + derma, skin), a loose connective tissue that may contain pads of adipocytes.
Hypodermis binds skin loosely to the underlying tissues
hypodermis
Thick skin
(Palm & Sole)Thin skin
(Rest of the body)Skin
Protective.
(1)physical barrier against thermal and mechanical insults such as frictional forces and against most potential pathogens.(2)Microorganisms that do penetrate skin alert resident lymphocytes and antigen-presenting cells of skin and an immune response is mounted.
(3)The dark pigment melanin in epidermis protects cells against ultraviolet radiation.
(4)permeability barrier against excessive loss or uptake of water.
Skin's selective permeability allows some lipophilic drugs such as certain steroid hormones and medications to be administered via skin patches. .
Functions of skin
Sensory. Many types of sensory receptors allow skin to constantly monitor the environment and various mechanoreceptors with specific locations in skin are important for the body's interactions with physical objects.
Functions of the skin
Thermoregulatory. A constant body temperature is normally more easily maintained thanks to the skin's insulating components (eg, the fatty layer and hair on the head) and its mechanisms for accelerating heat loss (sweat production and a dense superficial microvasculature).
Functions of the skin
Metabolic. Cells of skin synthesize vitamin D3, needed in calcium metabolism and proper bone formation, through the local action of UV light on the vitamin's precursor. Excess electrolytes can be removed in sweat and the subcutaneous layer stores a significant amount of energy in the form of fat.
Functions of the skin
stratified squamous keratinized epithelium
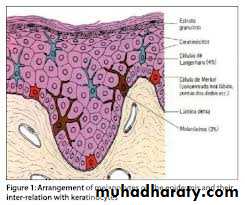
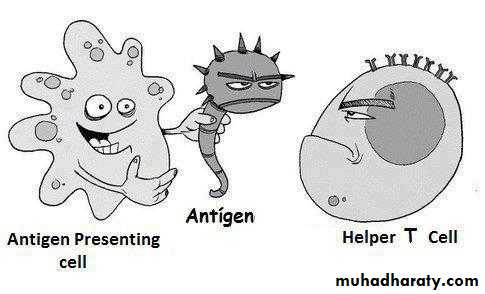
keratinocytes Major cells :Other cells are Non-keratinocytes :
(1)pigment-producing melanocytes,
(2)antigen-presenting Langerhans cells,
(3) tactile epithelial cells Merkel cells
Epidermis
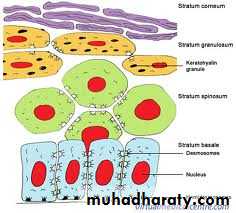
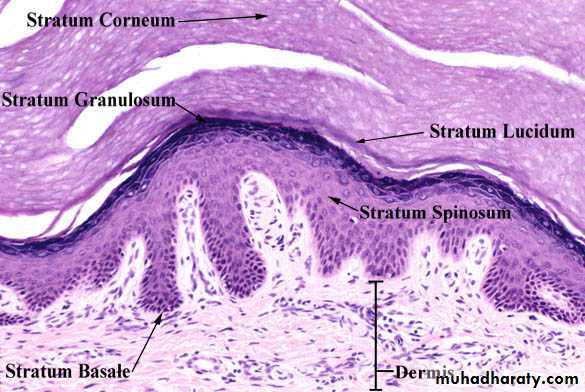
Composed of 5 layers (Keratinocytes):
Stratum basaleStratum spinosum
Stratum granulosum
Stratum lucidum
Stratum corneum
Thick skin epidermis
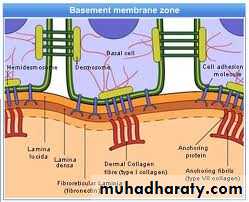
(1) single layer of basophilic columnar cells on the basement membrane at the dermo-epidermal junction.
(2)Hemidesmosomes in the basal plasma lemma bind these cells to the basal lamina
(3)Desmosomes bind the cells together from their lateral wall .
(4)This layer is characterized by intense mitotic activity and is responsible for constant production of epidermal cells.
(5)The human epidermis is renewed about every 15–30 days, depending on age, the region of the body, and other factors.
(6)All keratinocytes in the stratum basale contain intermediate filaments composed of keratins.
Stratum basale
(1)the thickest epidermal layer, consists of polyhedral cells having central nuclei.
(2)Stratum basale + lower layers of stratum spinosum are called the stratum germinativum.(3)The keratin filaments form bundles called tonofibrils which terminate at desmosomes.
(4)Cytoplasm has short cellular extensions around the tonofibrils, leading to the appearance of many short spines or prickles at the cell surfaces.
(5)It is thicker in areas subjected to continuous friction and pressure (such as the soles of the feet)
stratum spinosum
In adults, one third of all cancers are of the skin. Most of these derive from cells of the basal or spinous layers, producing, respectively, basal cell carcinomas and squamous cell carcinomas.
Skin cancer shows an increased incidence in fair-skinned individuals residing in regions with high amounts of solar radiation.
MEDICAL APPLICATION
(1) consists of 3–5 layers of flattened polygonal cells.
(2)Their cytoplasm is filled with intensely basophilic keratohyaline granules. These structures are not membrane-bound and consist of dense masses.(3)Other characteristic features are the membrane-coated lamellar granules, (seen by TEM)composed of various lipids. Lamellar granules undergo exocytosis, discharging their contents into the intercellular spaces of the stratum granulosum. this lipid-rich material produces sheets that envelop the cells (epidermal barrier against the loss of water from skin and barrier to penetration by most foreign materials).
stratum granulosum
(1)is only seen in thick skin
(2) it consists of a thin, translucent layer of extremely flattened eosinophilic cells.(3)The nuclei and organelles have been lost
(4) the cytoplasm consists almost only of densely packed keratin filaments embedded in an electron-dense matrix.
(5) Desmosomes are still evident between adjacent cells.
Stratum lucidum
(1)consists of 15–20 layers
(2) flattened, nonnucleated keratinized cells whose cytoplasm is filled with filamentous keratins.
(3) thickened plasma membranes
*These cells are called squames or horny, cornified cells
* These cells are continuously shed at the surface of the stratum corneum.
Stratum corneum
(1)No stratum lucidum (4 layers only)
(2) Stratum spinosum, granulosum and corneum are thinnerThin skin epidermis
Psoriasis, a common skin disease, there is an increase in the number of proliferating cells in the stratum basale and the stratum spinosum as well as a decrease in the cycle time of these cells. This results in
(1)greater epidermal thickness
(2) more rapid renewal of epidermis
(3)abnormal keratinization with a defective skin barrier.
MEDICALAPPLICATION
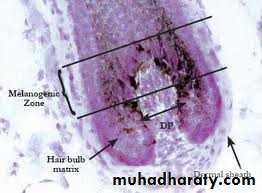
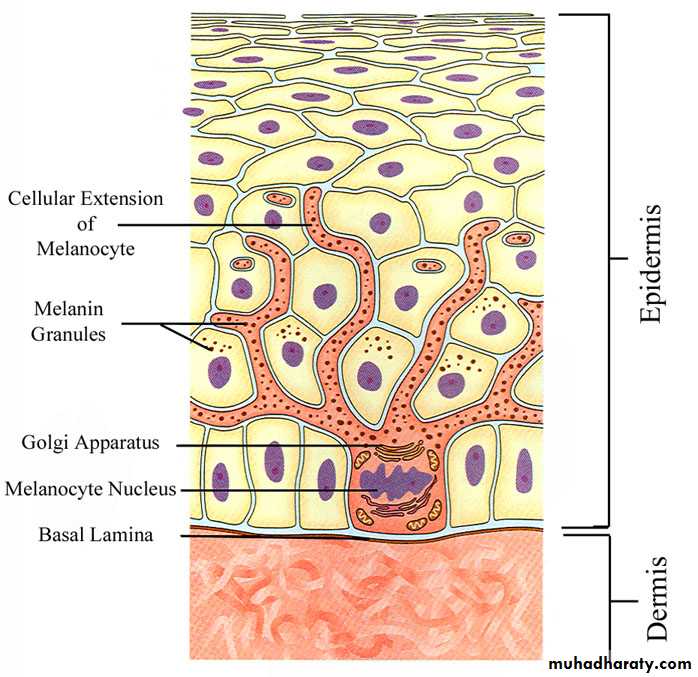
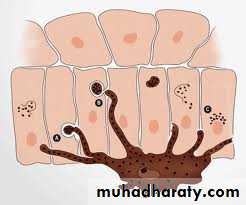
(1)specialized cells of the epidermis found among the cells of stratum basale and in the hair root.
(2)From tyrosine, they synthesize melanin (brownish black pigment ) and store it in vesicles called melanosomes
(3)They are neural crest derivatives which migrate into the developing epidermis' stratum basale.
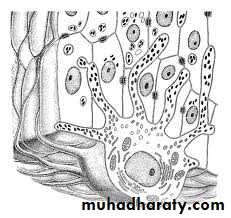
Melanocytes
(4)They have rounded cell bodies and long irregular dendritic extensions from each melanocyte branch into the epidermis, running between the cells of the basal and spinous layers.
(5)They form hemidesmosomes with the basal lamina, but no desmosomes with adjacent keratinocytes.
(6)Ultrastructurally, a melanocyte is a pale-staining cell with numerous small mitochondria, short cisternae of rough endoplasmic reticulum (RER), and a well-developed Golgi apparatus.
Melanocytes
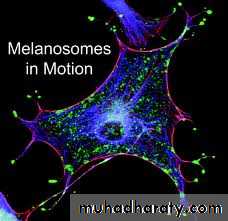
Tyrosinase converts tyrosine into melanin within melanocytes.
Melanin accumulates in vesicles until they form mature granules called melanosomes.Once formed, melanin granules are transported to tips of the melanocyte's dendrites.
The associated keratinocytes in both the basal and spinous layers phagocytose the tips of these dendrites.
Within each keratinocyte they accumulate as a supranuclear cap which absorbs and scatters sunlight, protecting nuclear DNA from the deleterious effects of UV radiation.
Melanin
What are the factors that influence the skin color?
the result of several factors,
(1)the most important of which are the keratinocytes' content of melanin(2) carotene
(3) the number of blood vessels in the dermis
Color of the skin
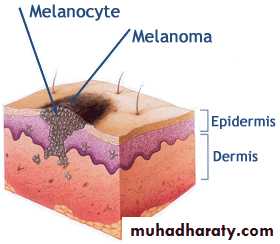
Malignant melanoma is an invasive tumor of melanocytes. Dividing rapidly, malignantly transformed melanocytes penetrate the basal lamina, enter the dermis, and invade the blood and lymphatic vessels to gain wide distribution throughout the body.
MEDICAL APPLICATION
Albinism, a hereditary inability of the melanocytes to synthesize melanin, is caused by the absence of tyrosinase activity or the inability of cells to take up tyrosine. As a result, the skin is not protected from solar radiation by melanin, and there is a greater incidence of (skin cancers).
The degeneration and disappearance of entire melanocytes causes a patchy loss of pigment in the skin disorder called vitiligo.
MEDICAL APPLICATION
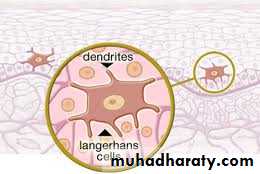
(1)usually most clearly seen in the stratum spinousum.
(2) Cytoplasmic processes extend from these dendritic cells between keratinocytes of all the layers, forming a fairly dense network in the epidermis .(3)They are bone marrow–derived.
(4)capable of binding, processing, and presenting antigens to T lymphocytes, thus providing an immunological component to the skin's overall protective function.
Langerhans Dendritic Cells
(1) mechanoreceptors (sense of touch)
(2)Small neurosecretory granules (related to diffuse neuroendocrine system)(3)Derived from neural crest cells
(4) located in the basal epidermal layer and at the bases of hair follicles.
(5)The basolateral surfaces of the cells contact expanded terminal discs of unmyelinated sensory fibers that penetrate the basal lamina.
Tactile (Merkel) Cells
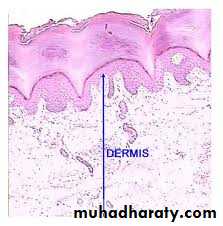
(1)The dermis is the connective tissue , that supports the epidermis and binds it to the subcutaneous tissue (hypodermis).
(2)The thickness of the dermis varies according to the region of the body, and reaches its maximum of 4 mm on the back.
(3)A basement membrane is always found between the stratum basale and the dermis.
(4)The basement membrane consists of the basal lamina and the reticular lamina and can usually be seen with the light microscope. (5)Nutrients for keratinocytes must diffuse into the avascular epidermis from the dermis vasculature through this basement membrane.
Dermis
The dermis contains two layers with rather indistinct boundaries:
(1)The thin papillary layer, which constitutes the major part of the dermal papillae, is composed of loose connective tissue, with fibroblasts and other connective tissue cells, such as mast cells and macrophages. Extravasated leukocytes are also seen. From this layer, anchoring fibrils of type VII collagen insert into the basal lamina and bind the dermis to the epidermis.(2)The reticular layer is thicker, composed of irregular dense connective tissue (mainly bundles of type I collagen), and has more fibers and fewer cells than the papillary layer. A network of elastic fibers is also present, providing elasticity to the skin. Spaces between the collagen and elastic fibers are filled with proteoglycans rich in dermatan sulfate.
Dermis
(1)With age, collagen fibers thicken and collagen synthesis decreases. Elastic fibers steadily increase in number and thickness, so the elastin content of human skin increases approximately fivefold from fetal to adult life.
In old age, extensive cross-linking of collagen fibers, the loss of elastic fibers, and degeneration of these fibers due to excessive exposure to the sun (solar elastosis) cause the skin to become more fragile, lose its suppleness, and develop wrinkles.
(2)In Ehlers-Danlos syndromes, there is a considerable increase in skin and ligament extensibility caused by defective collagen-fibril processing.
.
MEDICAL APPLICATION
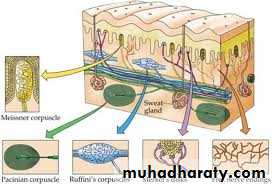
The connective tissue of the skin contains a rich network of blood and lymphatic vessels.
Blood vessels that nourish the cells of skin form two major plexuses :(1) deep at the interface between hypodermis and dermis
(2)superficially between the papillary and reticular dermal layers (subpapillary plexus) sends branches into the dermal papillae and supplies a rich, nutritive capillary network just below the epidermis.
In addition to the nutritive function, dermal vasculature has a thermoregulatory function which involves numerous arteriovenous anastomoses located between the two major plexuses.
Lymphatic vessels begin as closed sacs in the dermal papillae and converge to form two plexuses located with the blood vessels.
Vessels
sensory receptors are present in skin, including
The unencapsulated receptors include the following:(1) Tactile discs associated with the epidermal tactile cells, which function as receptors for light touch.
(2) Free nerve endings in the papillary dermis and extending into lower epidermal layers, which respond primarily to high and low temperatures, pain, and itching, but also function as tactile receptors.
(3)Root hair plexuses, a web of sensory fibers surrounding the bases of hair follicles in the reticular dermis that detects movements of the hairs.
Sensory Receptors
The following encapsulated receptors are tactile mechanoreceptors:
(1) Tactile corpuscles (Meissner corpuscles) are elliptical structures, in the fingertips, palms and soles. They detect light touch.(2)Lamellated (Pacinian) corpuscles are large oval structures, found deep in the reticular dermis or hypodermis, with an outer capsule and 15 to 50 thin, concentric lamellae of flat Schwann-type cells and collagen surrounding a highly branched, unmyelinated axon. They are specialized for sensing coarse touch, pressure (sustained touch), and vibrations.
(3)Krause corpuscles and Ruffini corpuscles are other encapsulated, pressure-sensing mechanoreceptors in dermis, but are more poorly characterized structurally