The central nervous system (CNS)
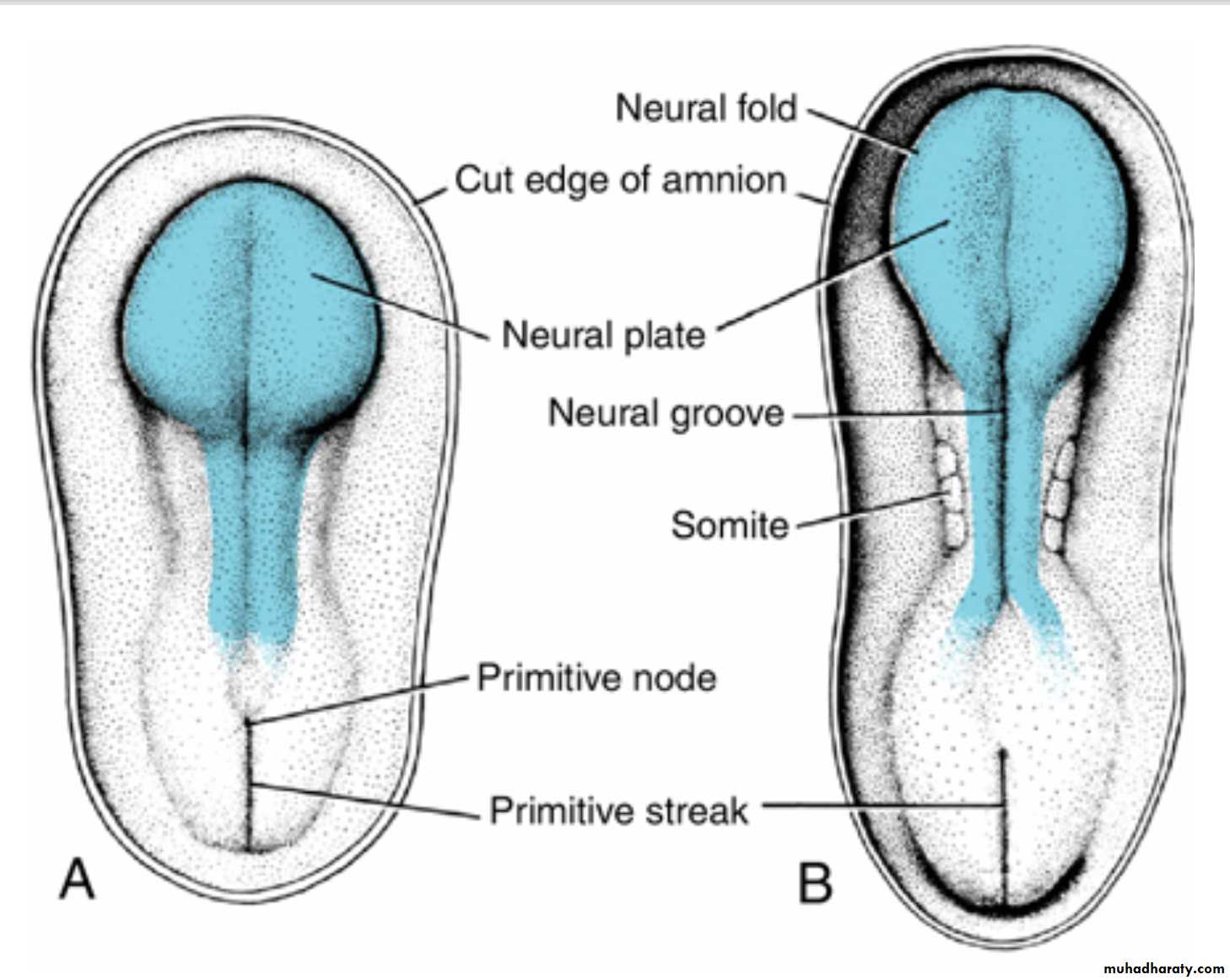
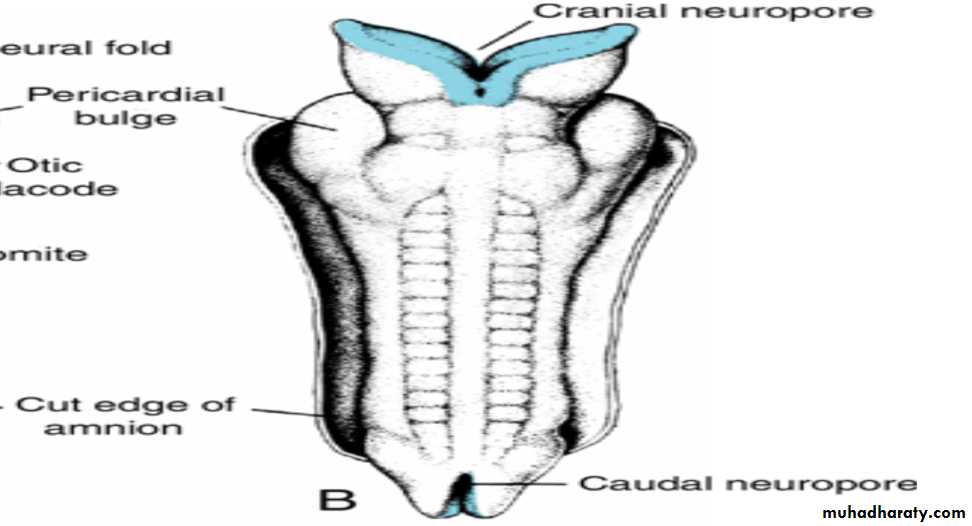
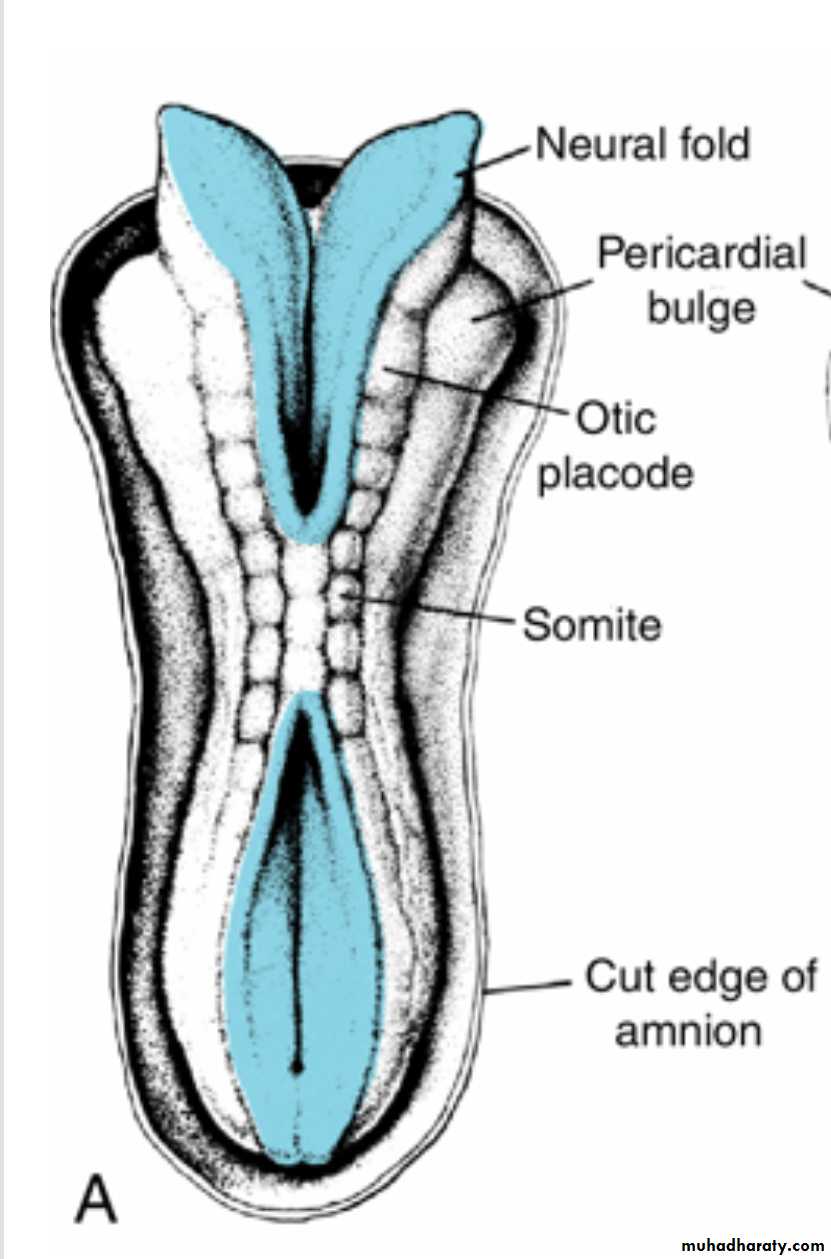
The neural plateappears at the beginning of the third week
as a slipper-shaped plate of thickened ectoderm,in the mid-dorsal region in front of the primitive node.
Neural tube
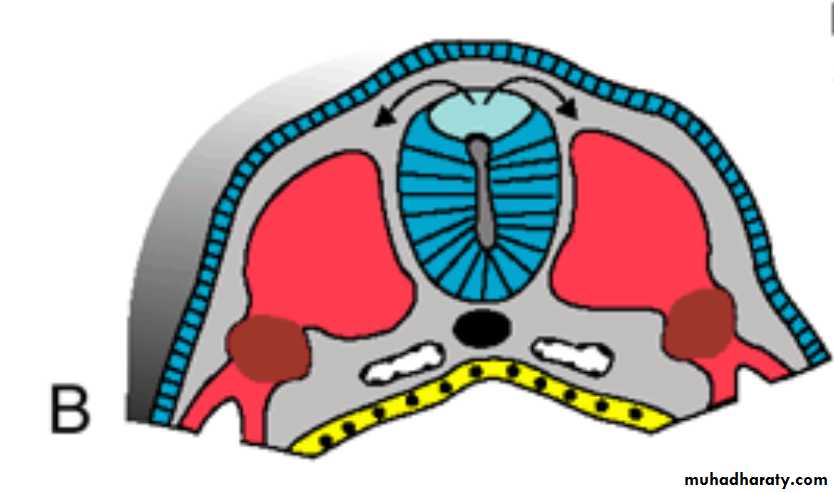
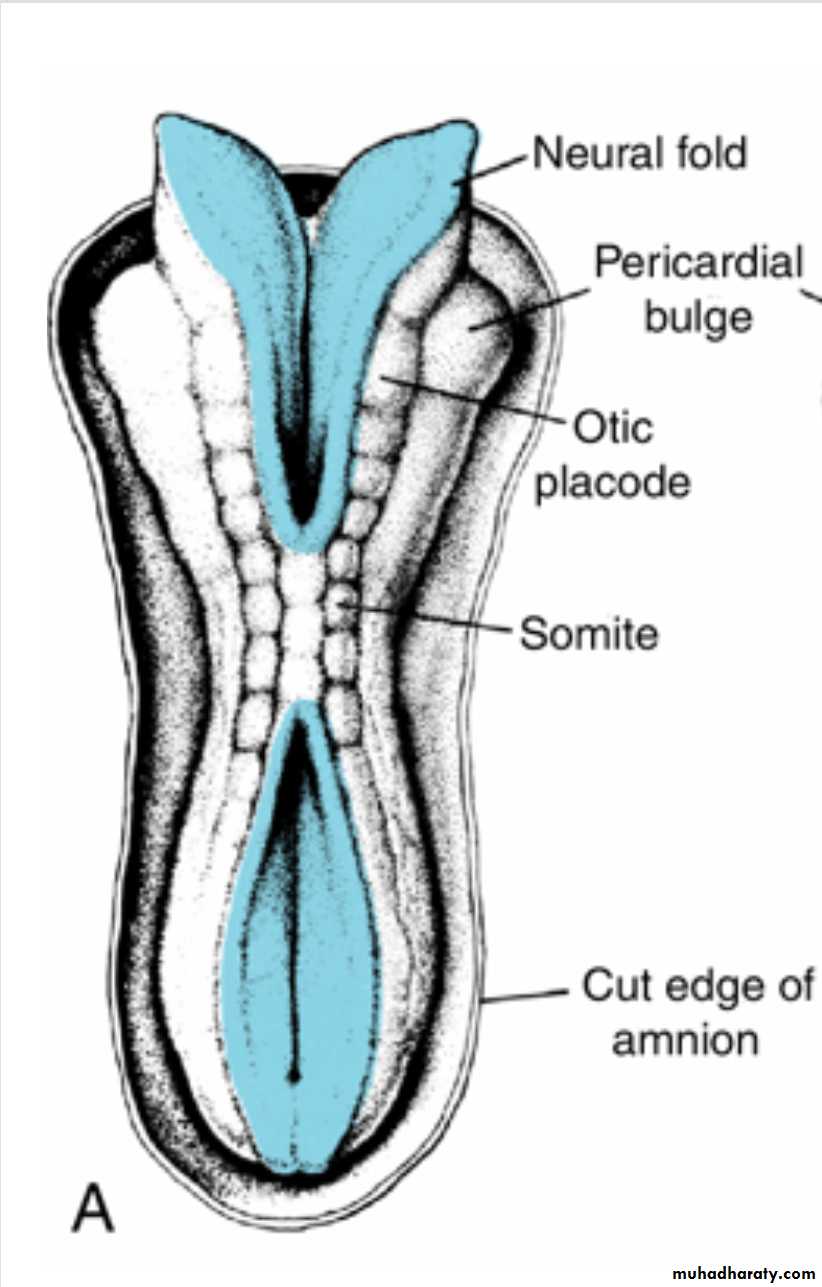
The lateral edges of the neural plate soon elevate to form the neural folds.With further development, the neural folds continue to elevate, approach each other in the midline, and finally fuse, forming the neural tube.
cranial and caudal neuropores
Fusion begins in the cervical region and proceeds in cephalic and caudal directions.
Once fusion is initiated, the open ends of the neural tube form the cranial and caudal neuropores that communicate with the overlying amniotic cavityClosure of the cranial neuropore
proceeds cranially from the initial closure site in the cervical region and from a site in the forebrain that forms later.
Neural tube
Final closure of the cranial neuropore occurs at the 18- to 20-somite stage (25th day);closure of the caudal neuropore occurs approximately 2 days later.
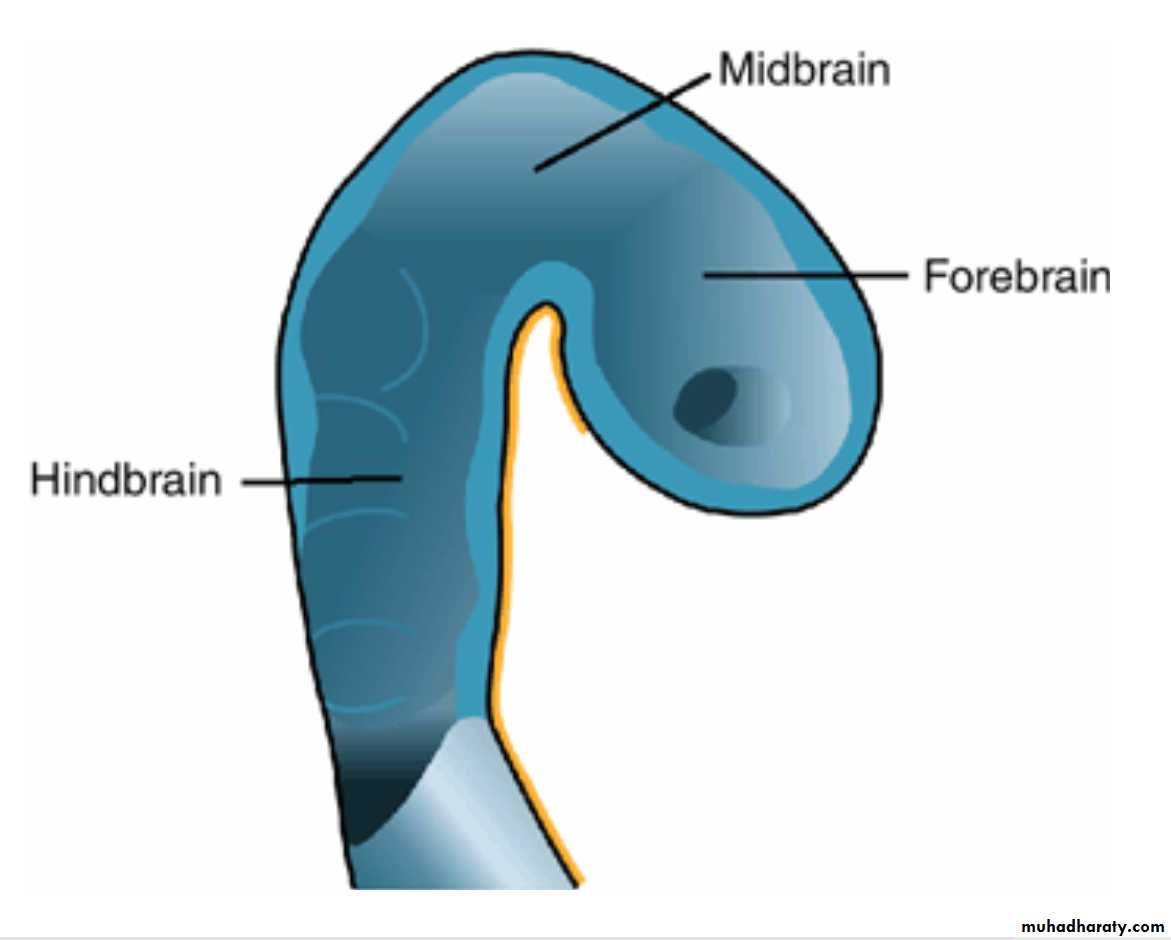
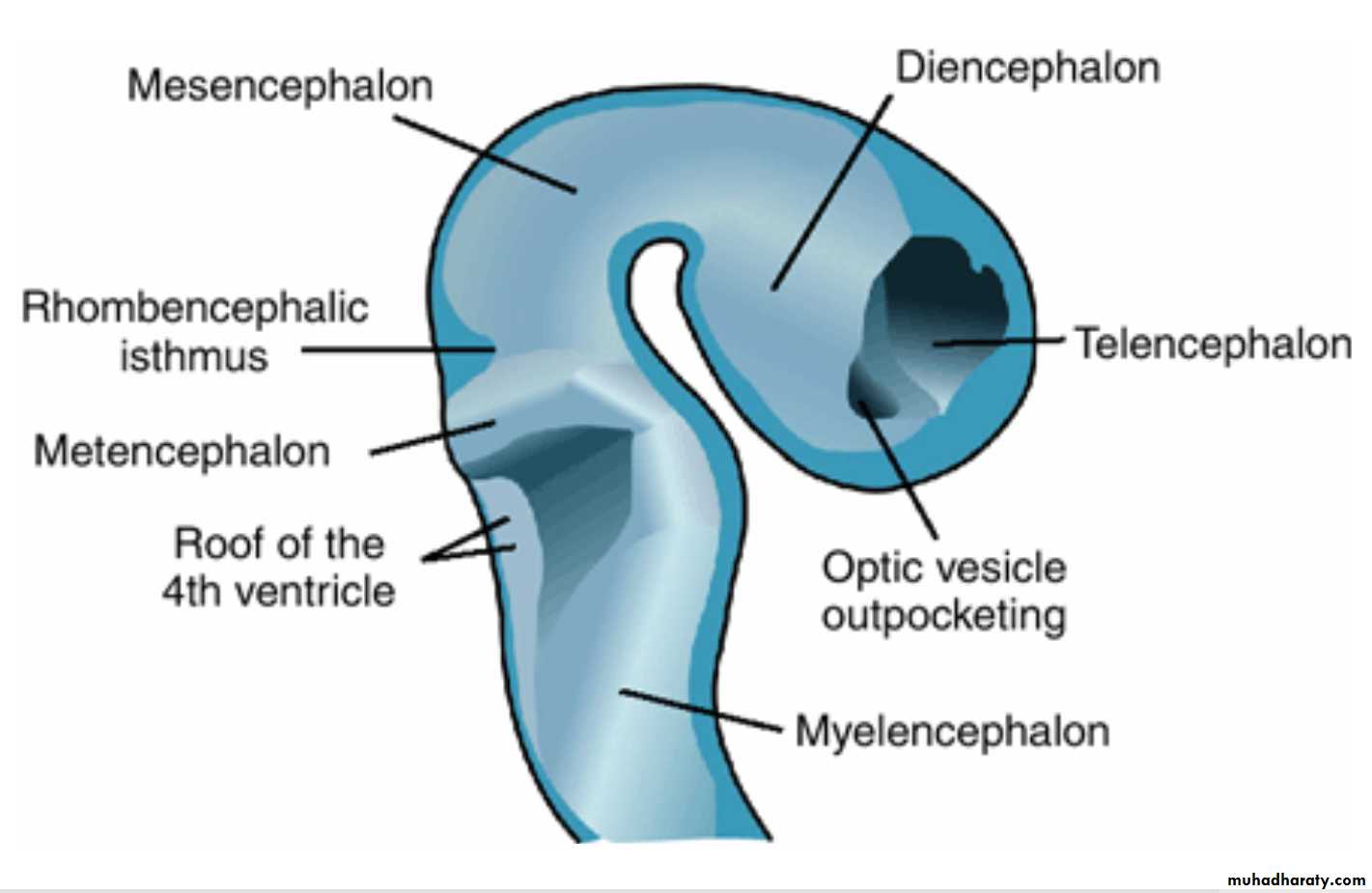
The cephalic end of the neural tube shows three dilations, the primary brain vesicles:
(a) theProsencephalon, or forebrain;(b) the Mesencephalon, or midbrain; and
(c) the Rhombencephalon, or hindbrain.
Simultaneously the cephalic end of the neural tube forms two flexures:
(a) the cervical flexure at the junction of the hindbrain and the spinal cord and
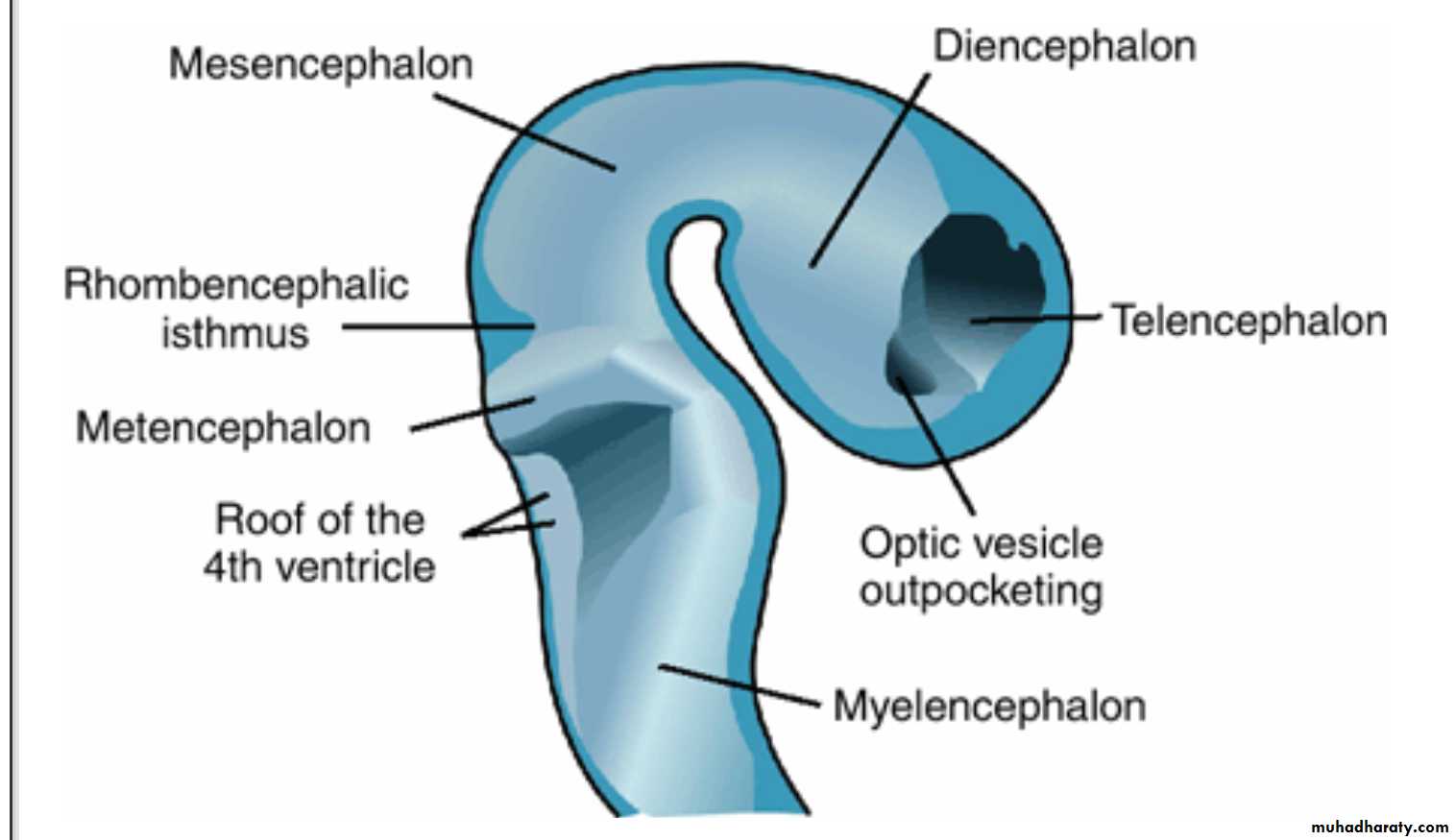
(b) the cephalic flexure in the midbrain region.When the embryo is 5 weeks old, the prosencephalon consists of two parts
(a (the Telencephalon, formed by a midportion and two lateral outpocketings, the primitive cerebral hemispheres, and) B( the Diencephalon, characterized by outgrowth of the optic vesicles
rhombencephalic isthmus
A deep furrow separates the mesencephalon from the rhombencephalon
Rhombencephalon also consists of two parts)a)the Metencephalon, which later forms the pons and cerebellum, and
(b)the myelencephalonThe boundary between these two portions is marked by the pontine flexure.
The lumen of the spinal cord (the central canal) is continuous with that of the brain vesicles
The cavity of the rhombencephalon is the fourth ventricle,
that of the diencephalon is the third ventricle, and
those of the cerebral hemispheres are the lateral ventricles.
The lumen of the mesencephalon connects the third and fourth ventricles. This lumen becomes very narrow and is then known as the aqueduct of Sylvius.
The lateral ventricles communicate with the third ventricle through the interventricular foramina of Monro.
Spinal Cord
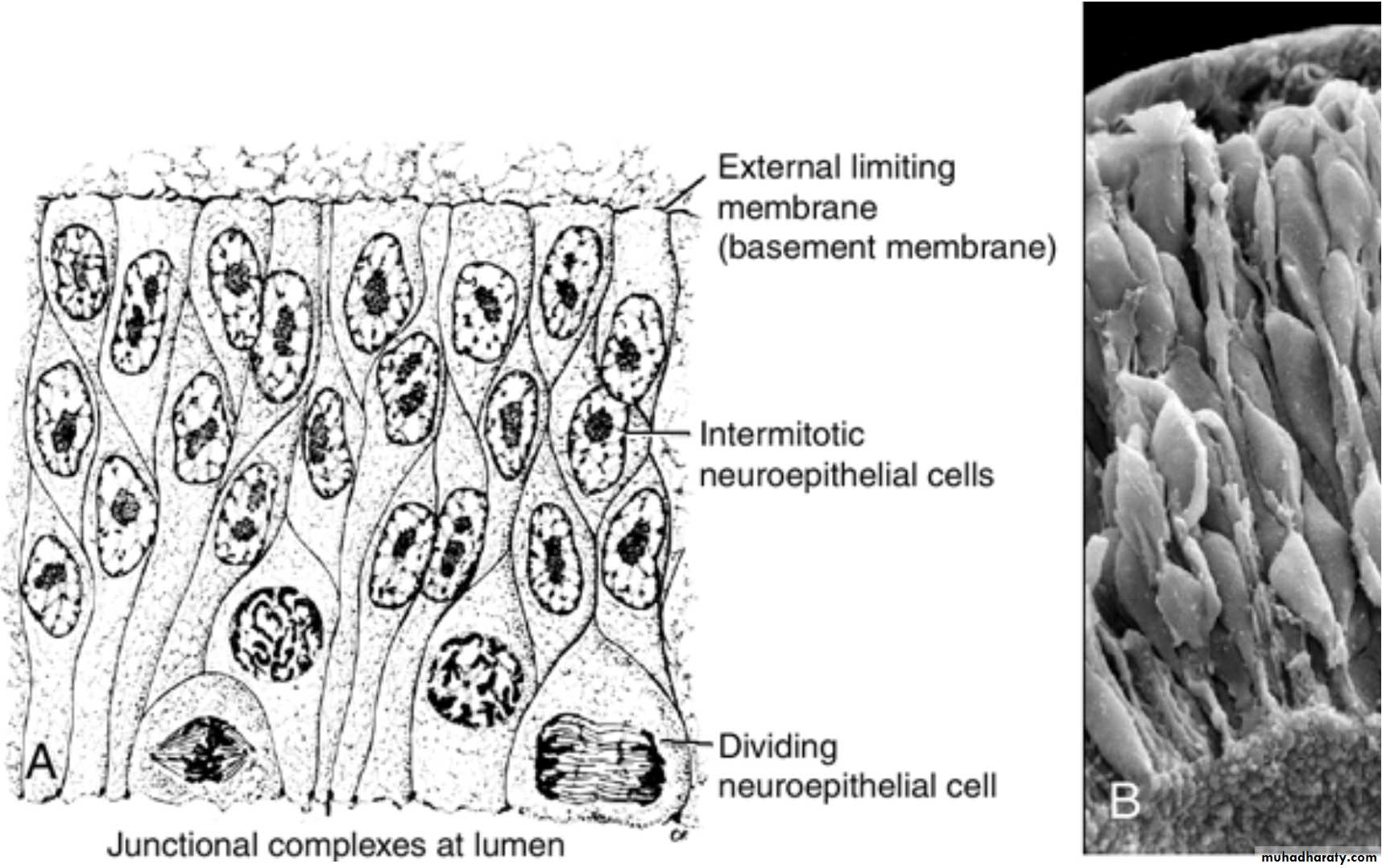
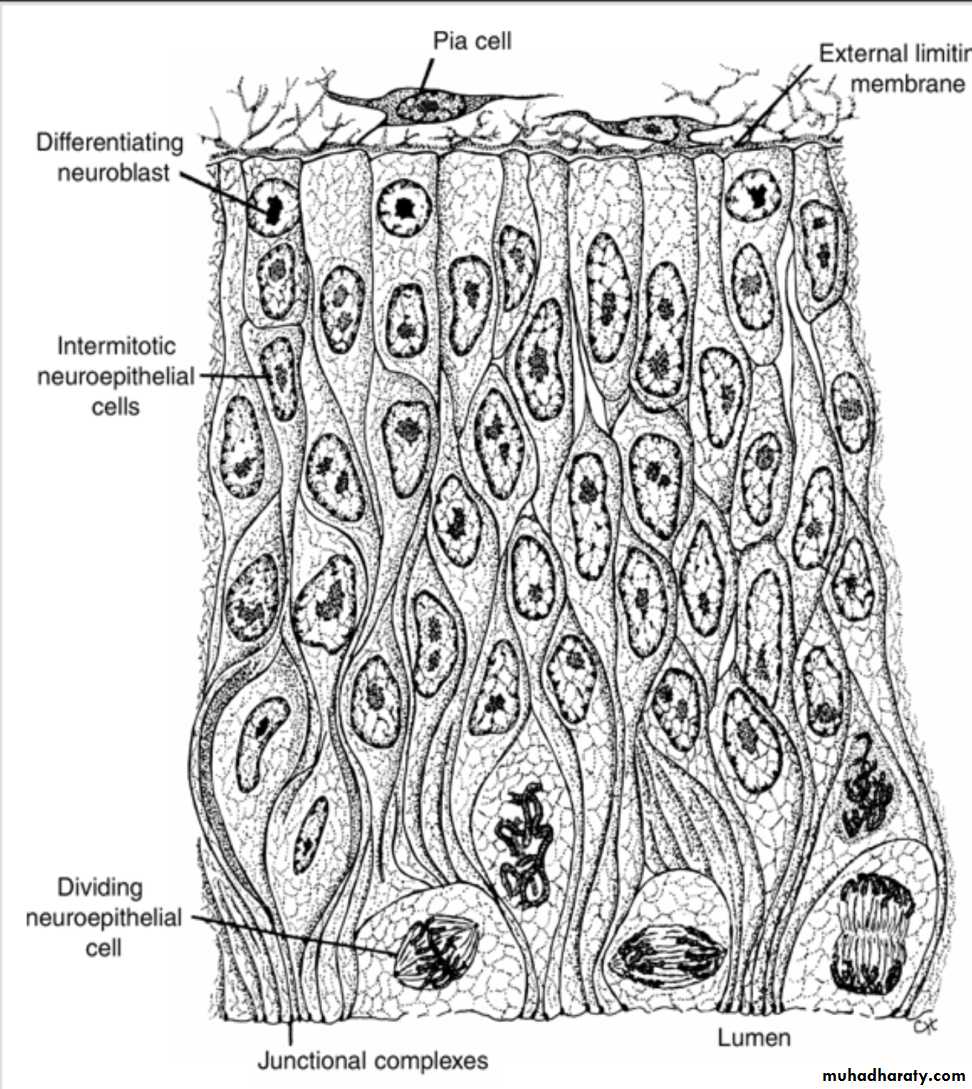
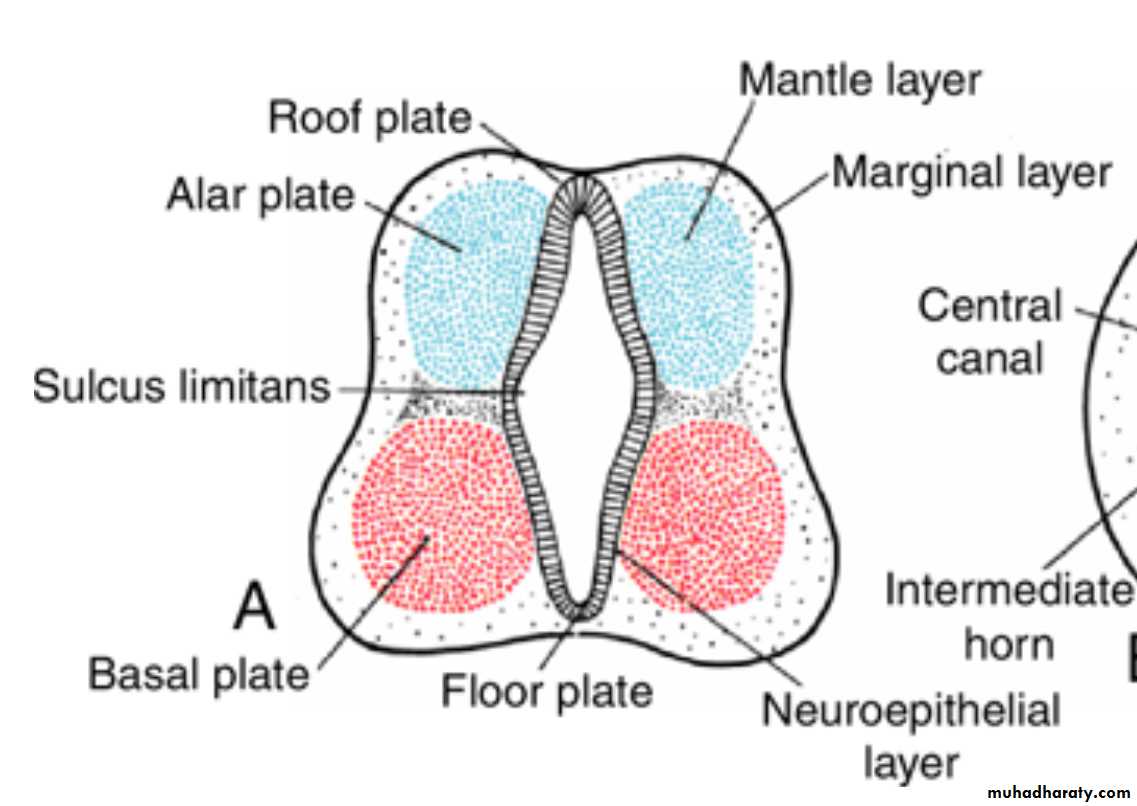
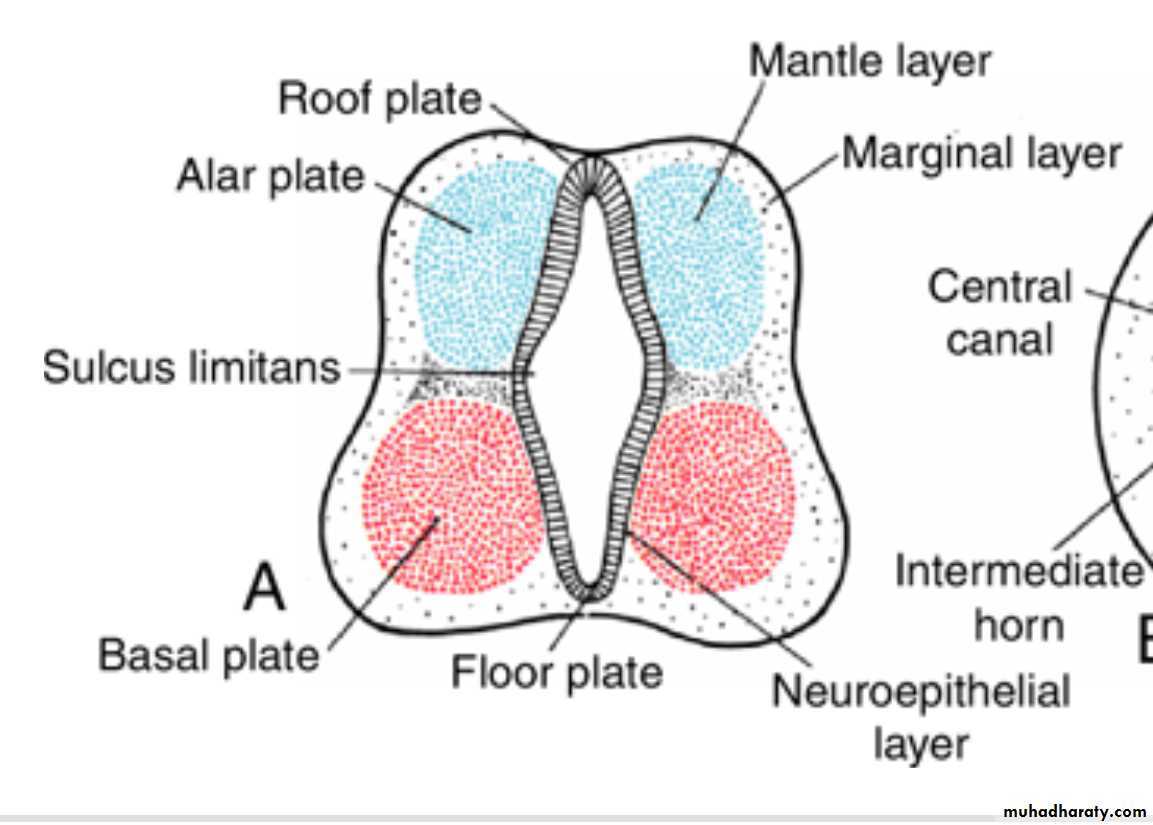
Neuroepithelial, Mantle, and Marginal Layersneuroepithelial layer (neuroepithelium)
The wall of a recently closed neural tube consists of neuroepithelial cells which extend over the entire thickness of the wall and form a thick pseudostratified epithelium .Junctional complexes at the lumen connect them.
During the neural groove stage and immediately after closure of the tube, they divide rapidly, producing more and more neuroepithelial cells.
Mantle layer
Once the neural tube closes, neuroepithelial cells begin to give rise to another cell type characterized by a large round nucleus with pale nucleoplasm and a dark-staining nucleolus. These are the primitive nerve cells, or neuroblastsThey form the Mantle layer, a zone around the neuroepithelial layer.
The mantle layer later forms the gray matter of the spinal cord.
The outermost layer of the spinal cord, the Marginal layer
contains nerve fibers emerging from neuroblasts in the mantle layer.As a result of myelination of nerve fibers, this layer takes on a white appearance and therefore is called the white matter of the spinal cord.
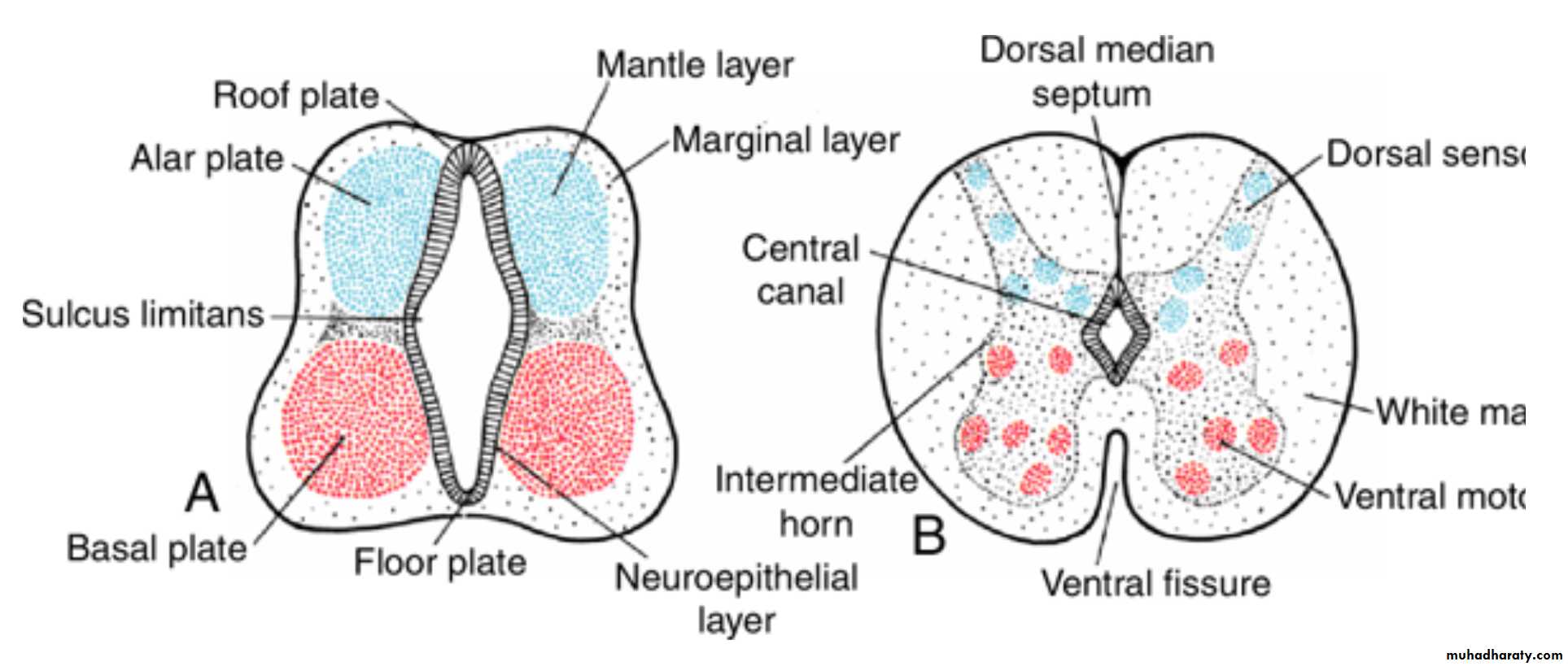
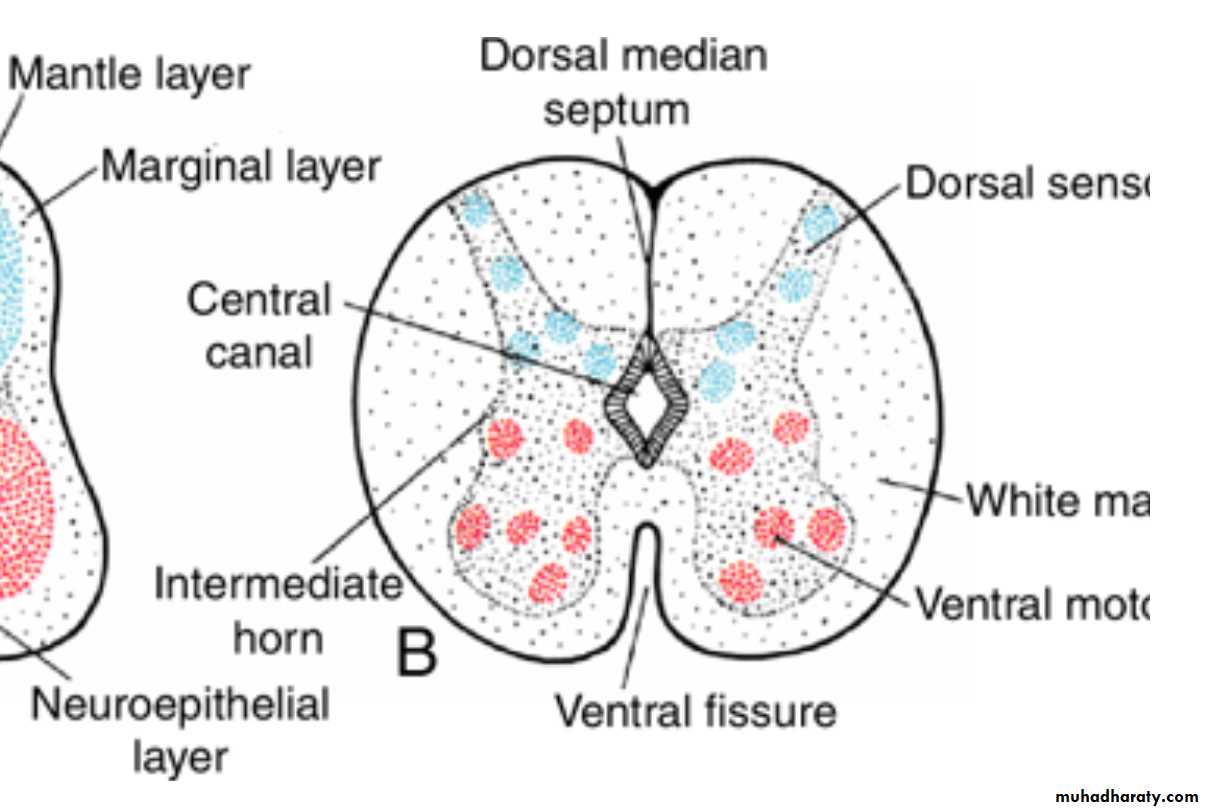
Basal, Alar, Roof, and Floor Plates
As a result of continuous addition of neuroblasts to the mantle layer, each side of the neural tube shows a ventral and a dorsal thickening.The ventral thickenings, the Basal plates, which contain ventral motor horn cells, form the motor areas of the spinal cord;
the dorsal thickenings, the Alar plates, form the sensory areas.
A longitudinal groove, the sulcus limitans, marks the boundary between the two.
Roof and floor plates
are the dorsal and ventral midline portions of the neural tube respectively,
They do not contain neuroblasts;they serve primarily as pathways for nerve fibers crossing from one side to the other.
Intermediate horn
In addition to the ventral motor horn and the dorsal sensory horn, a group of neurons accumulates between the two areas and forms a small intermediate horn .This horn, containing neurons of the sympathetic portion of the autonomic nervous system, is present only at thoracic (T1–T12) and upper lumbar levels (L2 or L3) of the spinal cord.
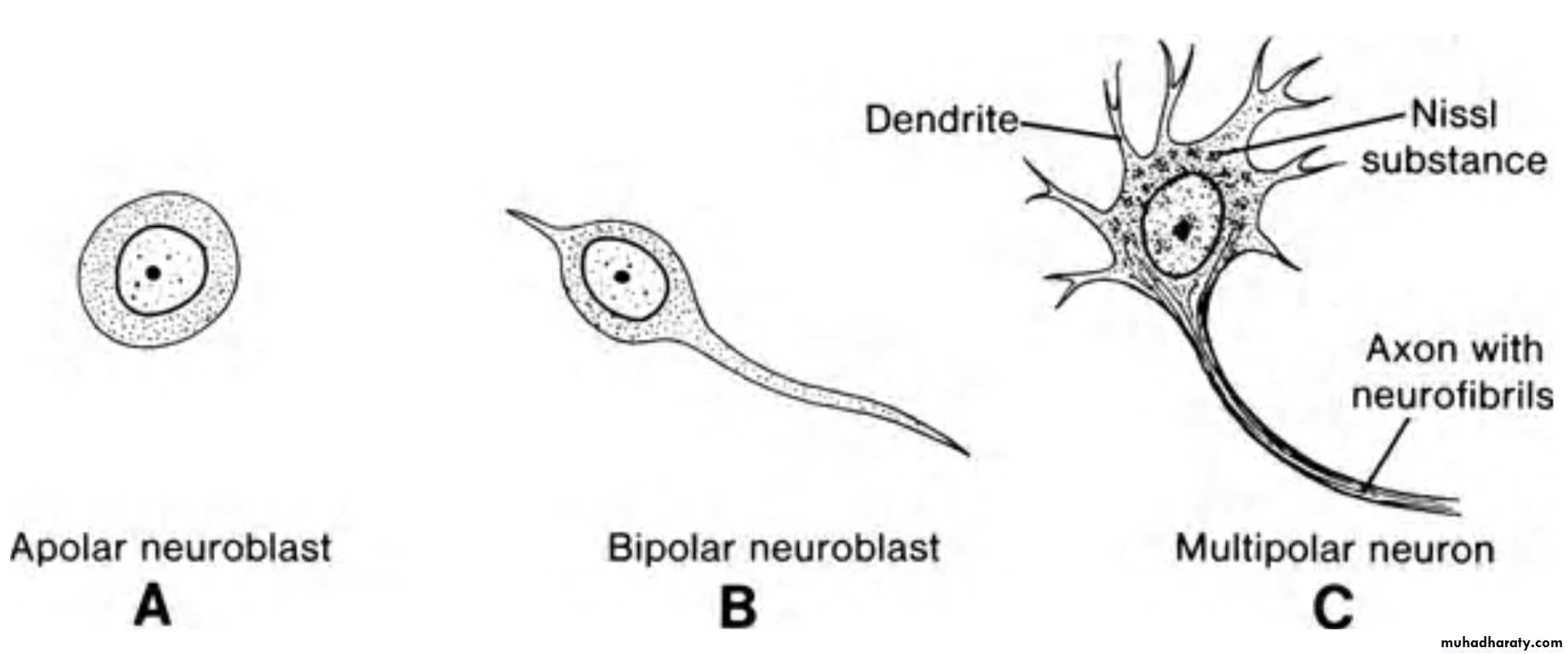
Histological Differentiation Nerve Cells
Neuroblasts, or primitive nerve cellsarise exclusively by division of the neuroepithelial cells. Initially they have a central process extending to the lumen (transient dendrite), but when they migrate into the mantle layer, this process disappears, and neuroblasts are temporarily round and apolar (A).
With further differentiation, two new cytoplasmic processes appear on opposite sides of the cell body, forming a bipolar neuroblast ( B ).
The process at one end of the cell elongates rapidly to form the primitive axon, and the process at the other end shows a number of cytoplasmic arborizations, the primitive dendrites (C). The cell is then known as a multipolar neuroblast and with further development becomes the adult nerve cell or neuron. Once neuroblasts form, they lose their ability to divide.
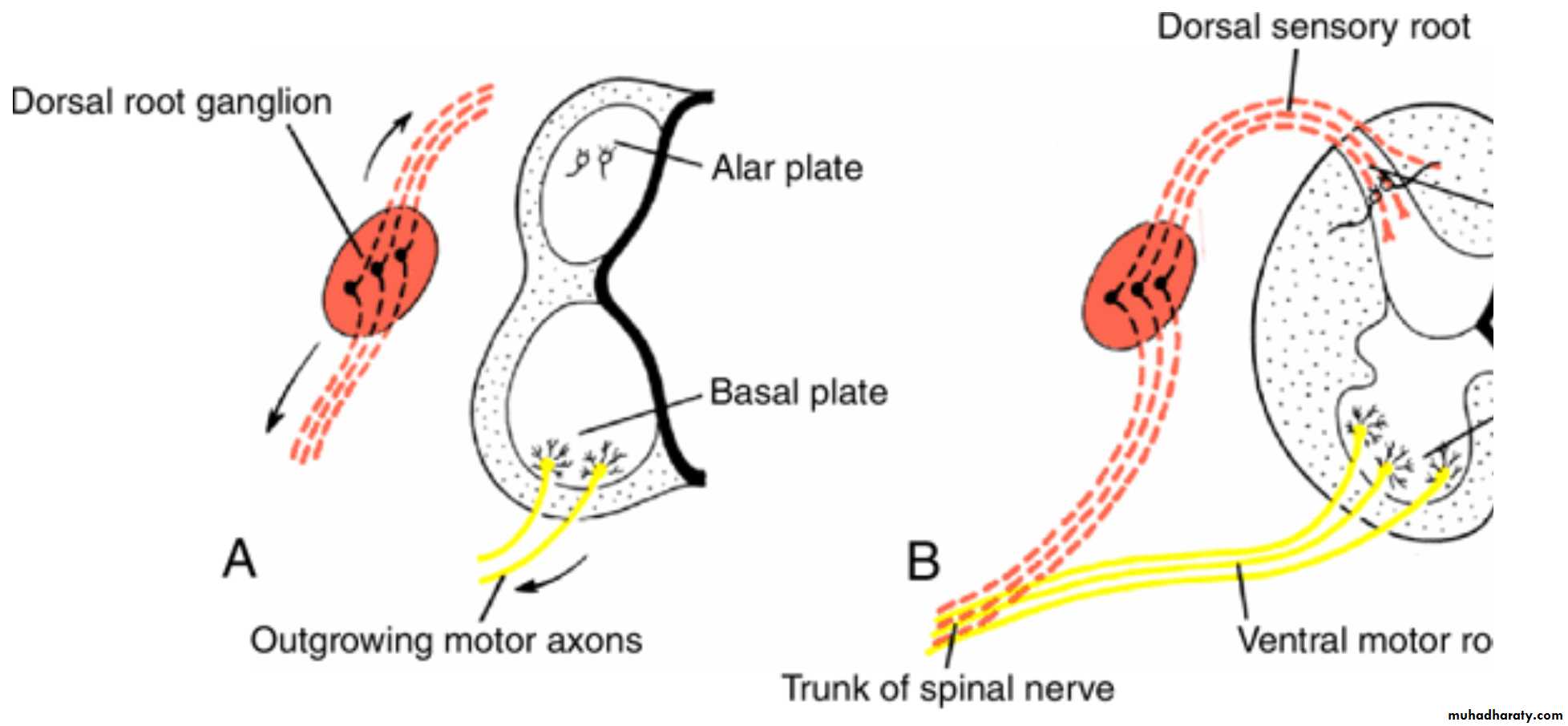
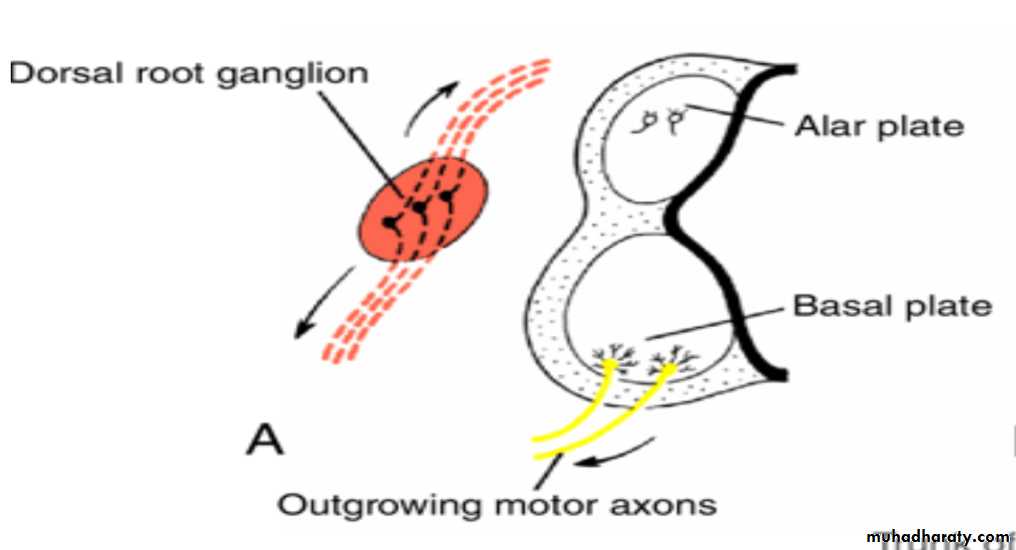
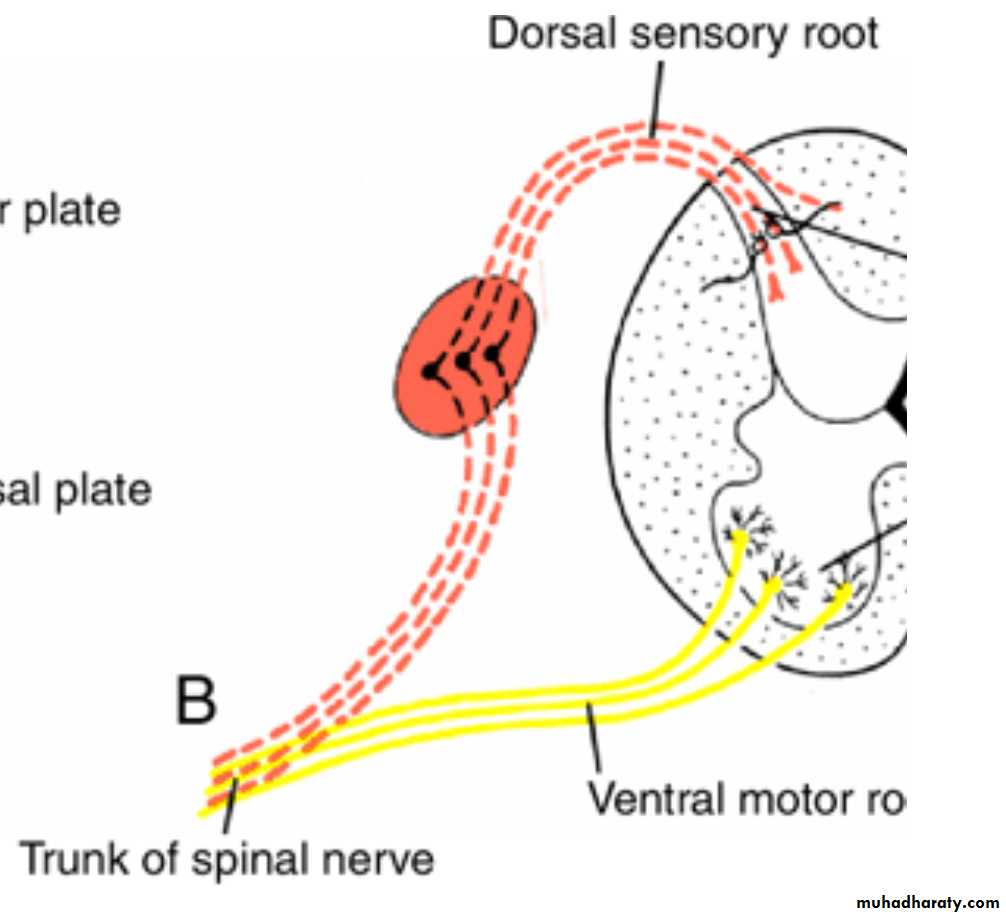
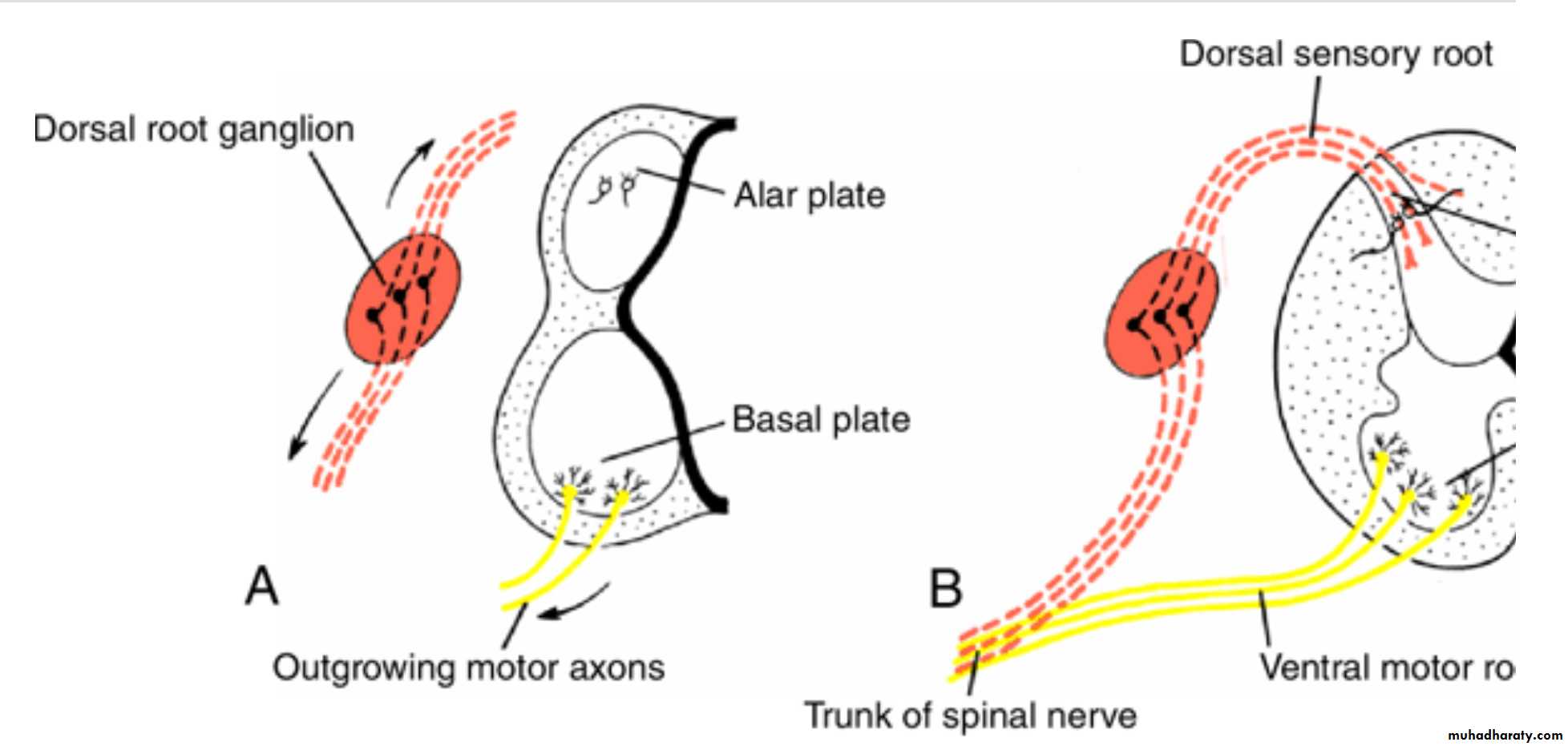
ventral motor and dorsal sensory roots of the spinal nerve
Axons of neurons in the basal plate break through the marginal zone and become visible on the ventral aspect of the cord. Known collectively as the ventral motor root of the spinal nerve, they conduct motor impulses from the spinal cord to the muscles.
Axons of neurons in the dorsal sensory horn (alar plate) behave differently from those in the ventral horn. They penetrate into the marginal layer of the cord, where they ascend to either higher or lower levels to form association neurons.
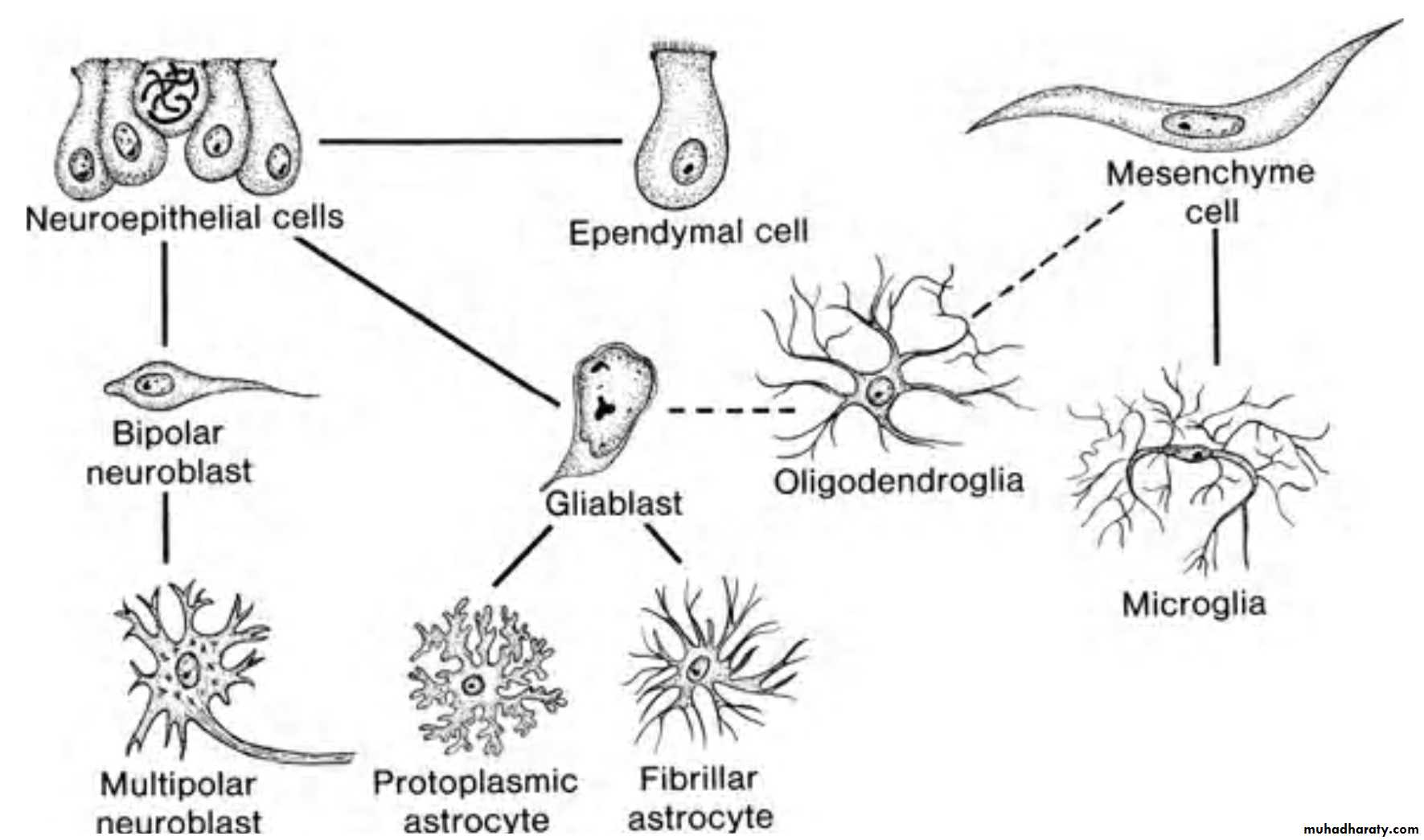
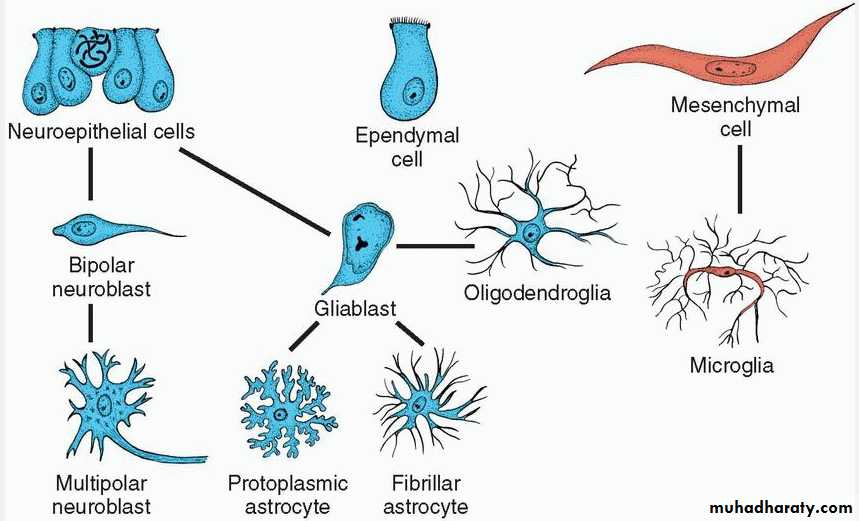
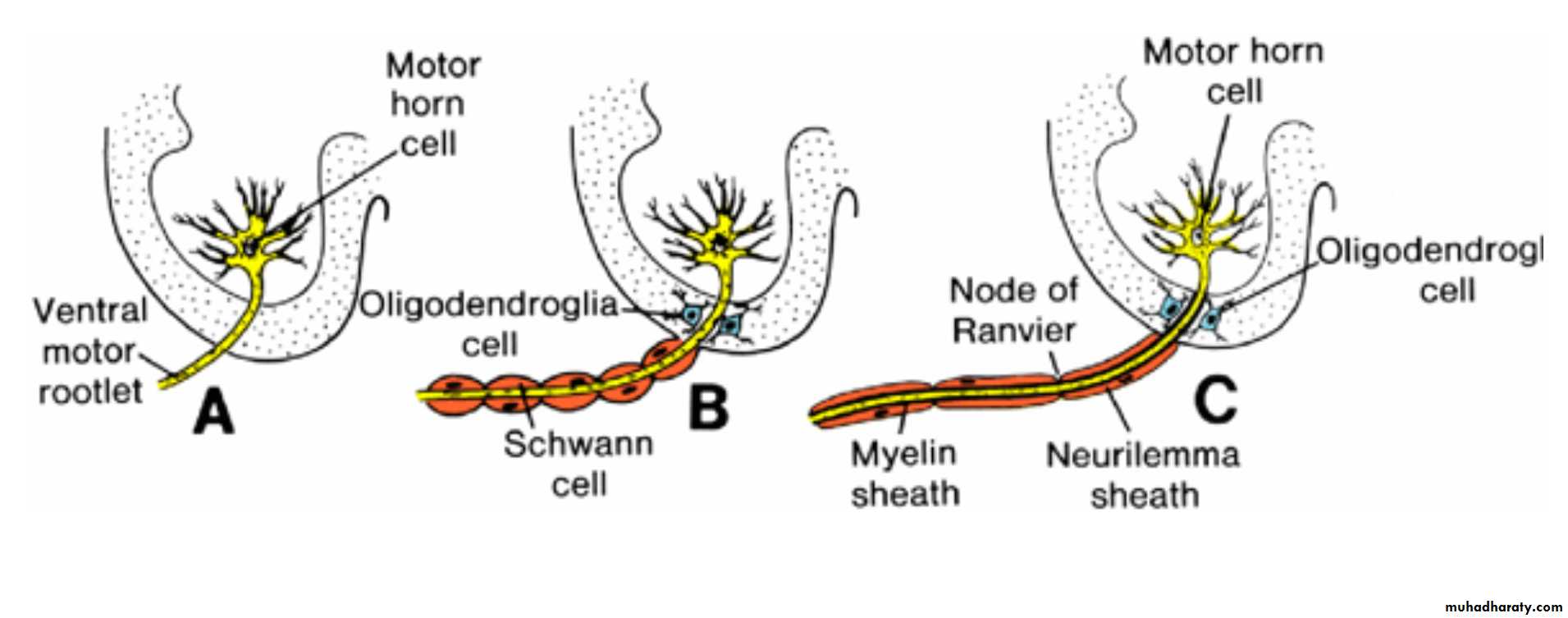
Glial Cells
The majority of primitive supporting cells, the gliablasts, are formed by neuroepithelial cells after production of neuroblasts ceases.Gliablasts migrate from the neuroepithelial layer to the mantle and marginal layers.
In the mantle layer, they differentiate into protoplasmic astrocytes and fibrillar astrocytes.
Glial Cells
Oligodendroglial cell derived from gliablasts. This cell, which is found primarily in the marginal layer, forms myelin sheaths around the ascending and descending axons in the marginal layer.In the second half of development, a third type of supporting cell, the microglial cell, appears in the CNS. This highly phagocytic cell type is derived from mesenchyme.
When neuroepithelial cells cease to produce neuroblasts and gliablasts, they differentiate into ependymal cells lining the central canal of the spinal cord.
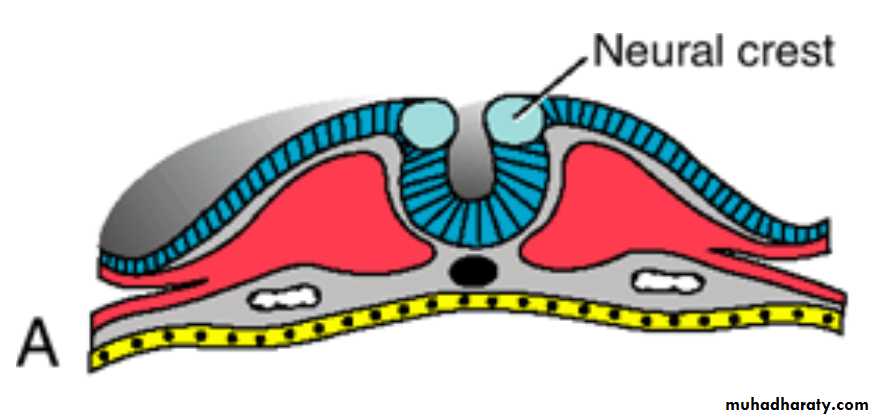
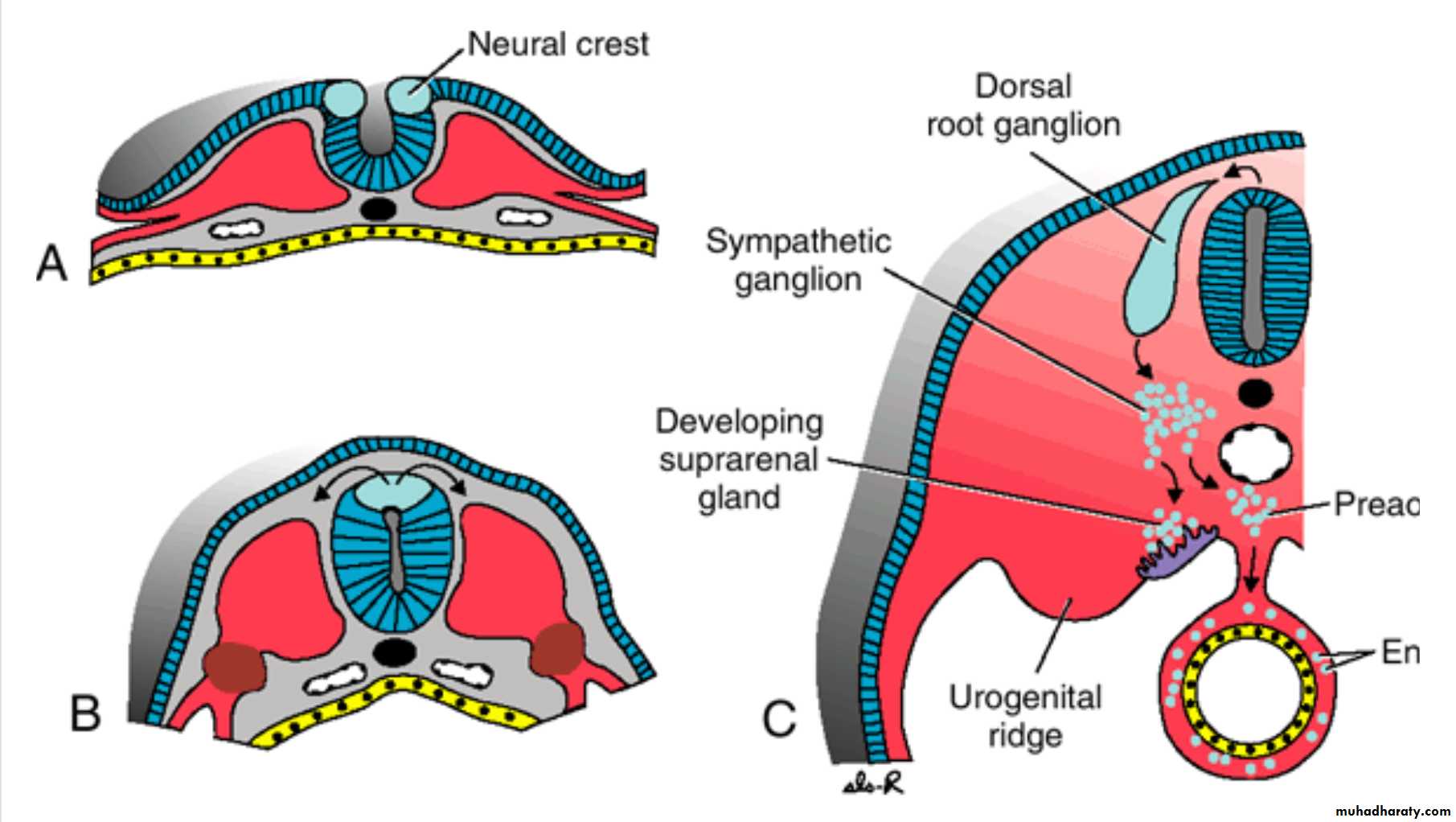
Neural Crest Cells
During elevation of the neural plate, a group of cells appears along each edge (the crest) of the neural folds.
These Neural crest cells are ectodermal in origin and extend throughout the length of the neural tube.
Crest cells migrate laterally and give rise to
(1) sensory ganglia (dorsal root ganglia) of the spinal nerves and other cell types.neuroblasts of this ganglia derived from neural crest cells and give rise to the dorsal root neurons.
(2) sympathetic neuroblasts, Schwann cells, pigment cells, odontoblasts, meninges, and mesenchyme of the pharyngeal arches.
Neural Crest Cells
During further development, neuroblasts of the sensory ganglia form two processes.(1)The centrally growing processes penetrate the dorsal portion of the neural tube. In the spinal cord, they either end in the dorsal horn or ascend through the marginal layer to one of the higher brain centers. These processes are known collectively as the dorsal sensory root of the spinal nerve .
(2)The peripherally growing processes join fibers of the ventral motor roots and thus participate in formation of the trunk of the spinal nerve. Eventually, these processes terminate in the sensory receptor organs.
Spinal Nerves
Motor nerve fibers begin to appear in the fourth week,
arising from nerve cells in the basal plates (ventral horns) of the spinal cord.These fibers collect into bundles known as ventral nerve roots.
Dorsal nerve roots form as collections of fibers originating from cells in dorsal root ganglia (spinal ganglia). Central processes from these ganglia form bundles that grow into the spinal cord opposite the dorsal horns. Distal processes join the ventral nerve roots to form a Spinal nerve .
Almost immediately, spinal nerves divide into dorsal and ventral primary rami. Dorsal primary rami innervate dorsal axial musculature, vertebral joints, and the skin of the back. Ventral primary rami innervate the limbs and ventral body wall and form the major nerve plexuses (brachial and lumbosacral).
Myelination
Schwann cells myelinate the peripheral nerves.
Beginning at the fourth month of fetal life, many nerve fibers take on a whitish appearance as a result of deposition of myelin, which is formed by repeated coiling of the Schwann cell membrane around the axon .The myelin sheath surrounding nerve fibers in the spinal cord has a completely different origin, the oligodendroglial cells .
Myelination
Although myelination of nerve fibers in the spinal cord begins in approximately the fourth month of intrauterine life, some of the motor fibers descending from higher brain centers to the spinal cord do not become myelinated until the first year of postnatal life.
Tracts in the nervous system become myelinated at about the time they start to function.
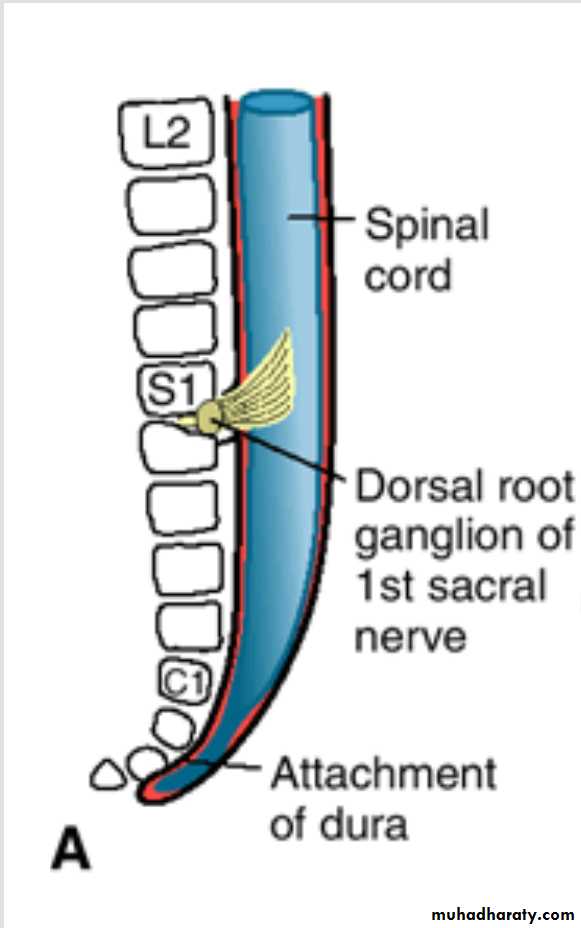
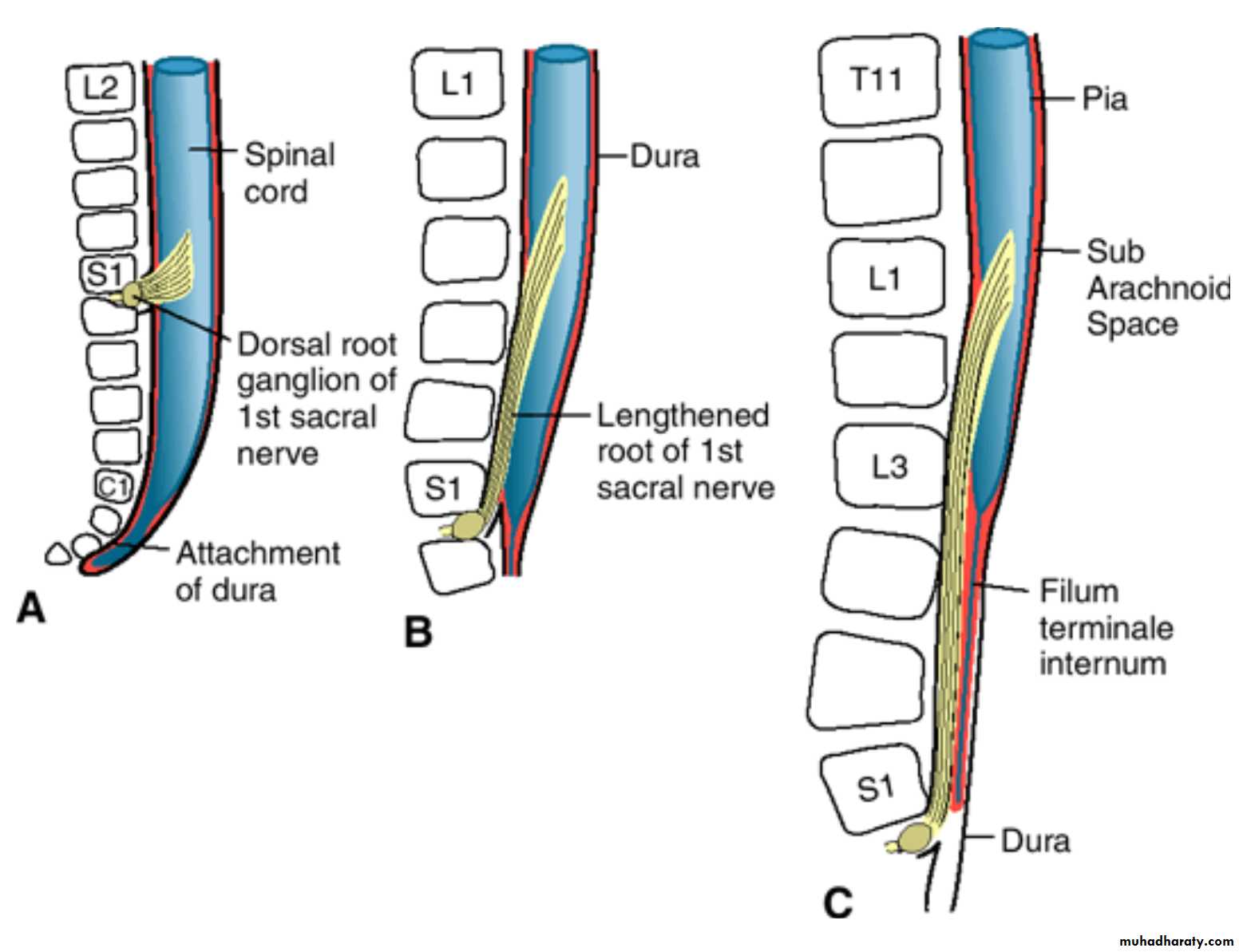
Positional Changes of the Cord
In the third month of development, the spinal cord extends the entire length of the embryo, and spinal nerves pass through the intervertebral foramina at their level of origin.Positional Changes of the Cord
With increasing age, the vertebral column and dura lengthen more rapidly than the neural tube, and the terminal end of the spinal cord gradually shifts to a higher level.
At birth, this end is at the level of the third lumbar vertebra.
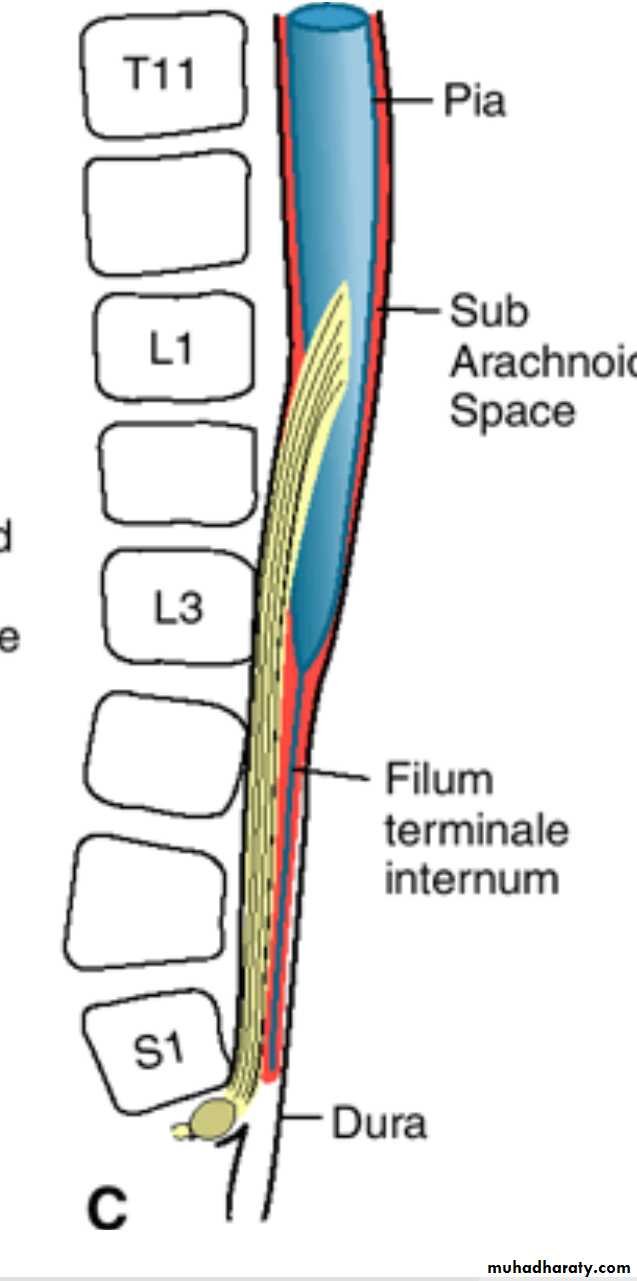
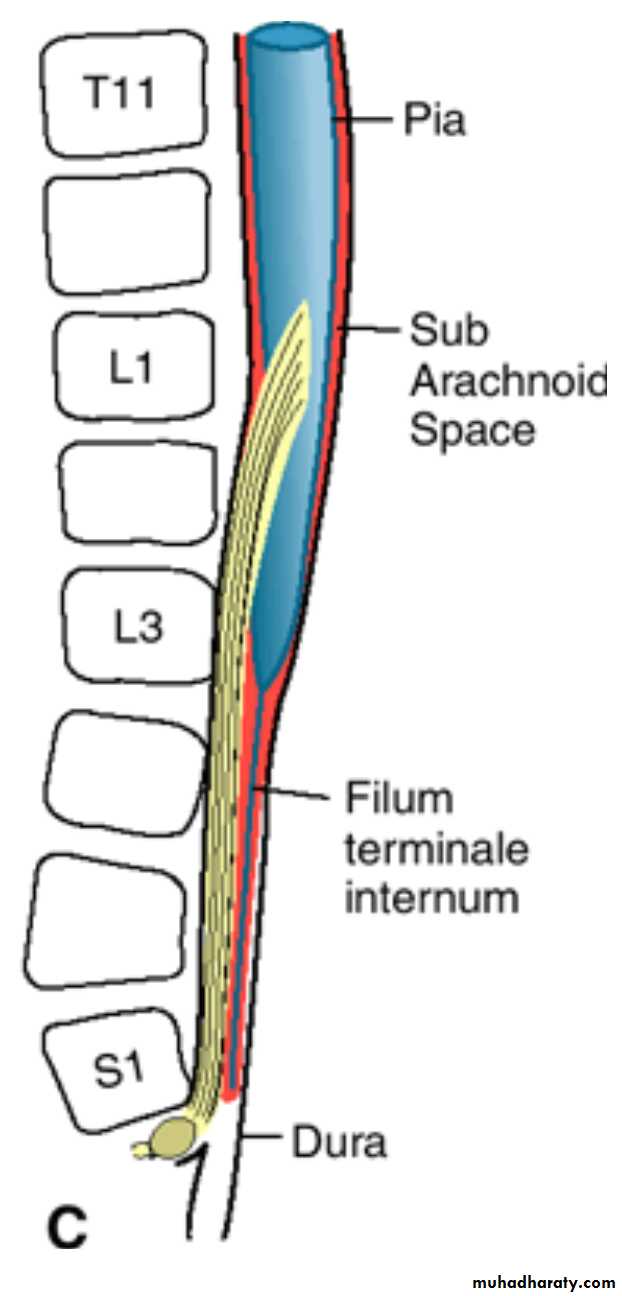
Positional Changes of the CordAs a result of this disproportionate growth,
spinal nerves run obliquely from their segment of origin in the spinal cord to the corresponding level of the vertebral column.The Dura remains attached to the vertebral column at the coccygeal level.
Positional Changes of the Cord
In the adult, the spinal cord terminates at the level of L2 to L3, whereas the dural sac and subarachnoid space extend to S2.
Below L2 to L3, a threadlike extension of the pia mater forms the filum terminale, which is attached to the periosteum of the first coccygeal vertebra and which marks the tract of regression of the spinal cord.
Nerve fibers below the terminal end of the cord collectively constitute the cauda equina.
When cerebrospinal fluid is tapped during a lumbar puncture, the needle is inserted at the lower lumbar level, avoiding the lower end of the cord.
Clinical Correlates Neural Tube Defects
Most defects of the spinal cord result from abnormal closure of the neural folds in the third and fourth weeks of development.neural tube defects
may involve the meninges, vertebrae, muscles, and skin.Spina bifida is a general term for NTDs affecting the spinal region. It consists of a splitting of the vertebral arches and may or may not involve underlying neural tissue.
Two different types of spina bifida occur:
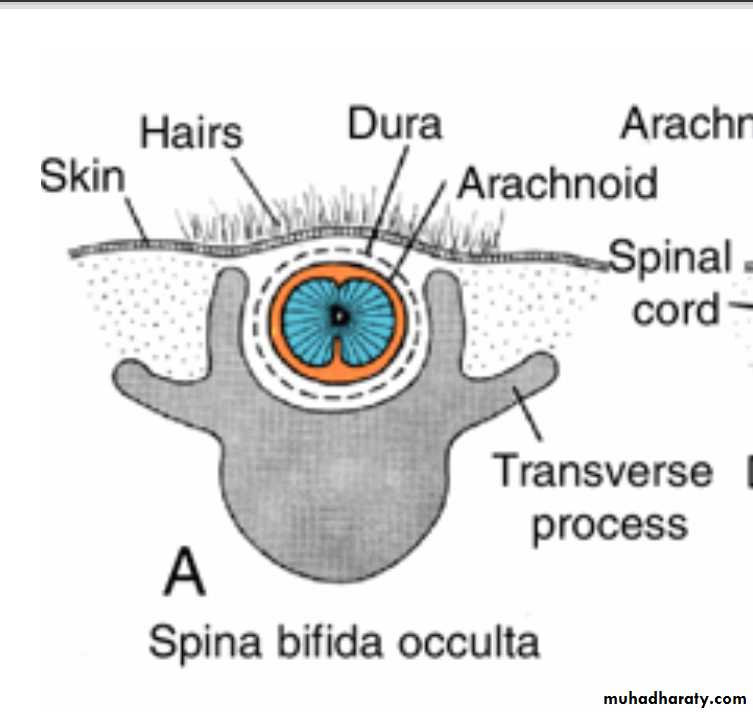
(1) Spina bifida occulta is a defect in the vertebral arches that is covered by skin and usually does not involve underlying neural tissue .It occurs in the lumbosacral region (L4–S1) and is usually marked by a patch of hair overlying the affected region.
The defect is due to a lack of fusion of the vertebral arches
Two different types of spina bifida occur
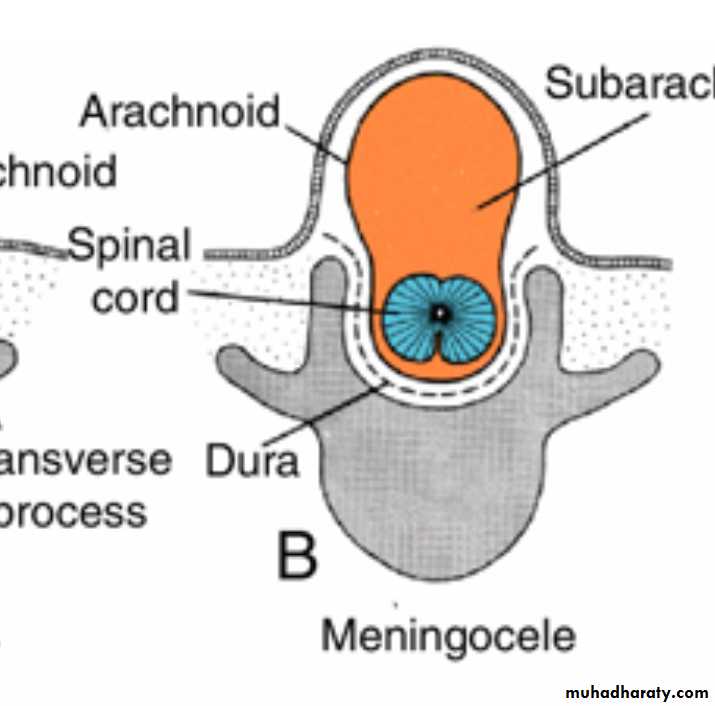
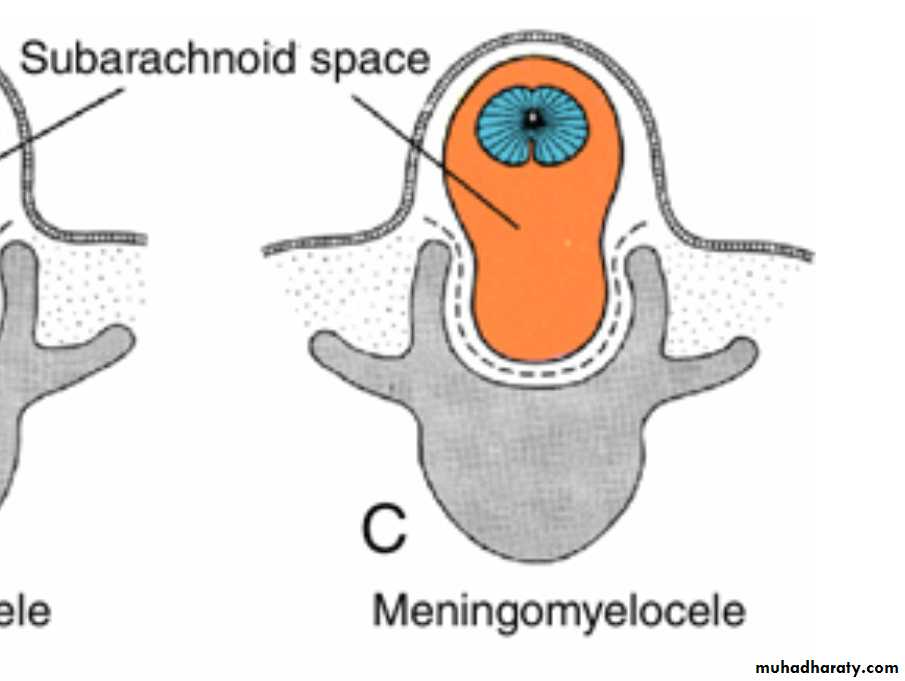
(2) Spina bifida cystica is a severe NTD in which neural tissue and/or meninges protrude through a defect in the vertebral arches and skin to form a cystlike sac .
Most lie in the lumbosacral region and result in neurological deficits, but they are usually not associated with mental retardation.
In some cases, only fluid-filled meninges protrude through the defect (spina bifida with Meningocele) ;in others neural tissue is included in the sac (spina bifida with meningomyelocele).
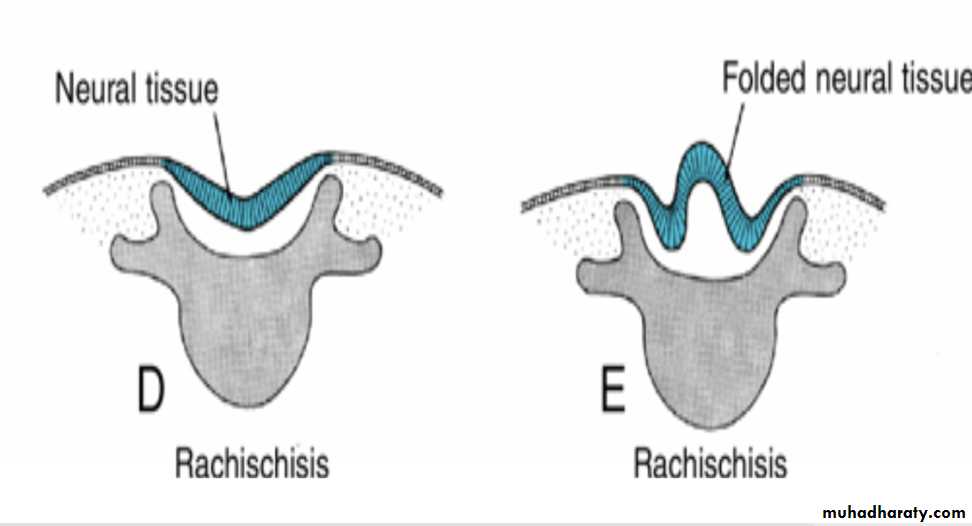
Occasionally, the neural folds do not elevate but remain as a flattened mass of neural tissue (spina bifida with myeloschisis or rachischisis.
Hydrocephaly develops in virtually every case of spina bifida cystica because the spinal cord is tethered to the vertebral column. As the vertebral column lengthens, tethering pulls the cerebellum into the foramen magnum, cutting off the flow of cerebrospinal fluid.
Spina bifida cystica
can be diagnosed prenatally by ultrasound and by determination of α-fetoprotein levels in maternal serum and amniotic fluid.The vertebra can be visualized by 12 weeks of gestation, and defects in closure of the vertebral arches can be detected.
A new treatment for the defect is to perform surgery in utero at approximately 28 weeks of gestation. The baby is exposed by cesarean section, the defect is repaired, and the infant is placed back in the uterus. Preliminary results indicate that this approach reduces the incidence of hydrocephalus, improves bladder and bowel control, and increases motor development to the lower limbs.
Spina bifida cystica
Hyperthermia, valproic acid, and hypervitaminosis A produce NTDs, as do a large number of other teratogens
Recent evidence proves that Folic acid (folate) reduces the incidence of NTDs by as much as 70% if 400 µg is taken daily beginning 2 months prior to conception and continuing throughout gestation.