Gangrene
By: Dr. Housam SousanORIGIN
The word "gangrene" comes from the Greek "ganggraina" denoting "an eating sore that ends in mortification".MEDICAL DEFFINITION:
GangreneThe death of body tissue due to the loss of blood supply to that tissue, sometimes permitting bacteria to invade it and accelerate its decay.
Death and decay of body tissue caused by insufficient blood supply, Usually following disease, infection, injury, blood vessel disease, or surgery.
NNNNNNNNN
Gangrene is a complication of necrosis “ N cell death N ” characterized by the decay of body tissues, which become black and appearing “rotten”.It is caused by infection or ischemia, such as a thrombosis.
GANGRENE… WHAT IS IT???
It is usually the result of critically insufficient blood supply.Often associated with diabetes and long-term smoking.
Condition is most common in the lower extremities.BASICALLY YOUR BLOOD SUPPLY GETS CUT OFF AND YOUR TISSUE DECIDES TO DIE
Causes of gangrene
A serious injuryBlood vessel disease (such as arteriosclerosis, hardening of the arteries, in arms or legs)
Diabetes
Suppressed immune system (for example, from HIV, chemotherapy and Radiotherapy, Uraemia, Jaundice)
Infection
Surgery
Age
Smoking (Burger’s Disease)
Types of gangrene
There are five main types of gangrene
1) Dry gangrene.2) Wet gangrene.
3) Gas gangrene.
4) Internal organ gangrene.
5) Necrotizing fascitis.
Types and Where
Dry Gangrene= affects bodies extremitiesarteries get blocked= tissue slowly dies
Affected body parts feel cold and turn dark, it will dry and wither/eventually falling off
Mostly affects extremities such as fingers and toes
Wet Gangrene= occurs with injury and infection
Injury restricts blood flow to certain areas
Blood can’t flow to tissue so can’t fight infection= infection sets in,
Swelling from infection= even less blood flow= fast spreading gangrene=life threatening
Become swollen, discolored, and smelly.
Necrotising Fasciitis= Caused by serious bacterial infection, sometimes referred to as flesh-eating bacteria
Bacteria enters a cut and spreads quickly, releases toxins
Block blood to surrounding skin, causing death of skin
Mostly attacks people with very low immune systems
Gas Gangrene= just like Necrotising except develops deep in body ex) muscles (mostly from surgical wounds)
Releases gasses and toxins to kill living tissue, then spreads
Loves to be in low oxygen areas
Types/Where continued
Internal Gangrene=affects internal organs
Blood flow to internal organ is blocked.
Happens when complications occur with a hernia.
Usually affects organs such as intestines, gallbladder, or appendix.
A variant of wet gangrene, has less obvious initial symptoms because the wet gangrene occurs in the internal organs. The patient may be very ill (septic) with gangrene but show few if any visual symptoms that are characteristic for wet gangrene.
TYPES OF GANGRENE
DRY GANGRENEWET GANGRENE
GAS GANGRENEDRY GANGRENE
Dry gangrene begins at the distal part of the limb due to ischemia and often occurs in the toes and feet of elderly patients due to arteriosclerosis.Dry gangrene spreads slowly until it reaches the point where the blood supply is adequate to keep tissue viable.
The affected part is dry, shrunken and dark black, resembling mummified flesh.
affected area-cold numb red to brown to black and shriveled.
DRY GANGRENE
If the blood flow is interrupted for a reason other than severe bacterial infection, the result is a case of dry gangrene.People with impaired peripheral blood flow, such as diabetics, are at greater risk of contracting dry gangrene.
DRY GANGRENE
The early signs are a dull ache and sensation of coldness in the affected are.If caught early, the process can sometimes be reversed by vascular surgery.
If necrosis sets in, the affected tissue must be removed and treated like a case of wet gangrene.
DRY GANGRENE
DRY GANGRENE
DRY GANGRENE
YUCKY!!!
WET GANGRENEWet gangrene occurs in naturally moist tissue and organs such as the mouth, bowel, lungs, cervix, and vulva.
Bedsores occurring on body parts such as the sacrum, buttocks and heels (not in “moist” areas) are also categorized as wet gangrene infections.
WET GANGERNE
In wet gangrene, the tissue is infected by microorganisms, which cause tissue to swell and emit a fowel odour.Wet gangrene usually develops rapidly due to blockage of venous and/or arterial blood flow.
The affected part is saturated with stagnant blood which promotes the rapid growth of bacteria.
swollen- decays, extremely painful, smelly, oozing then turns black and affected person develops a fever
WET GANGRENE SMELLS!!!
THAT SMELLS LIKE PURE GASOLINE!!!WET GANGRENE
The toxic products formed by bacteria are absorbed causing systemic manifestation of bacteria and finally death.The affected part is soft, putrid, rotten
and dark.The darkness in wet gangrene occurs due to the same mechanism as in dry gangrene.
WET GANGREEN
WET GANGRENE
WET GANGRENE
WET GANGRENE
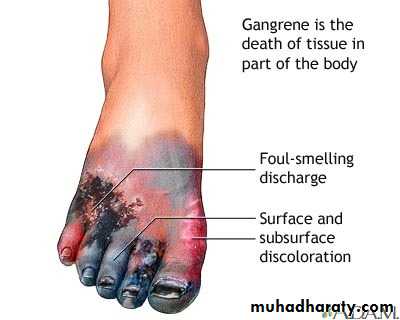
Symptoms and Signs
Discoloration (blue or black if skin is affected; red or bronze if the affected area is beneath the skin)Foul-smelling discharge.
Loss of feeling in the area.
Confusion
Fever
General ill feeling,
Low blood pressure (Septic Shock).
Persistent or severe pain.
GAS GANGRENE
Is a type of wet gangrene caused by the bacteria known as Clostridia. Clostridia are a type of infection-causing bacteria that grow only in the absence of oxygen.
Gas gangrene is a bacterial infection that produces gas within tissues.
It is a N deadly N form of gangrene usually caused by bacteria.Infection spreads rapidly as the gases produced by bacteria expand and effect healthy tissues.
GAS GANGRENE
Gas gangrene is caused by a environmental bacteria.These Bacteria are mostly found in soil in
their spore form.
These environmental bacteria enter the muscle through a wound and cause necrotic tissue and powerful toxins.
brownish red discharge oozes, Gas produced by Clostridia may produce a crackling sensation, painful, then high fever and increase in heart rate
GAS GANGRENE
These toxins destroy nearby tissue, generating gas at the same time.
Gas gangrene can cause necrosis, gas production, and sepsis.
Progression to toxemia and shock is often very rapid.
Because of its ability to quickly spread to surrounding tissues, gas gangrene should be treated as a medical emergency.
Palpation of the affected tissues gives a feeling of crepitus or crackling which is diagnostic.
X-Ray of the affected tissues shows classical air bubbles.
GAS GANENE
GAS GANGRENE
GAS GANGRENE
GAS GANGRENE
SPECIFIC GANGRENES
Noma is a gangrene of the face.Necrotizing fasciitis affects the deeper layers of the skin.
Fournier gangrene usually affects the male genitals.NOMA
Is a gangrenous disease leading to tissue destruction of the face, especially the mouth and cheek.Risk factors include severe protein mal nutrition (Marasmis and Kwashioker) and unsanitary conditions.
NOMA
NOMA
NECROTIZING FASCIITIS
Commonly known as flesh-eating disease or flesh-eating bacteria.Rare infection of the deeper layers of skin and easily spread within the subcutaneous tissue
NECROTIZING FASCIITIS
NECROTIZING FASCIITIS
FOURNIER GANGRENE
A type of necrotizing infection usually affecting the soft tissues of the male genitals.In the majority of cases it is a mixed infection caused by both aerobic and anaerobic bacteria
FOURNIER GANGRENE
FOURNIER GANGRENE
FOURNIER GANGRENE
OUCH!!!
Melaney’s GangreneA type of necrotizing infection usually affecting the abdominal wall in immune compromised patients.
In the majority of cases it is a mixed infection caused by both aerobic and anaerobic bacteria
NECROTIZING FASCIITIS
Tests & diagnosis
*Arteriogram (special x-ray to see any blockages in the blood vessels) to help plan treatment for blood vessel disease*Blood tests (white blood cell (WBC) count may be high)
*CT scan to examine internal organs
*Culture of the tissue or fluid from wounds to identify bacterial infection*Examining tissue under the microscope to look for cell death
*Surgery to find and remove dead tissue*X-rays
PrognosisThe outlook depends on where the gangrene is in the body, how much gangrene there is, and the person's overall condition. If treatment is delayed, the gangrene is extensive, or the person has other significant medical problems, they may die.
TREATMENT
Antibiotics are available at hospitals.Administration of pressured oxygen.
“Maggot Therapy” (popular in WW1)
An operation to improve blood supply to the area
Amputation of the affected limb.
Removal of affected area (Extensive wound debridement) which may need repeated sessions.
Prolonged wound healing or the need for reconstructive surgery, such as skin grafting.
Treatment in the intensive care unit (for severely ill patients)
TREATMENT
As early as 1028 fly maggots were commonly used prevent or arrest necrotic spread.
Some species of maggots consume only dead flesh, leaving nearby living tissue unaffected.
This practice largely died out after the introduction of antibiotics.
Maggot therapy has regained some credibility and is sometimes employed with great efficacy in cases of chronic tissue necrosis.
MEDICAL MAGGOTS
MAGGOT TREATMENT
TREATMENT
Usually surgical with amputation necessary in many cases.Antibiotics alone are not effective because they do not penetrate ischemic muscles sufficiently.
TREATMENT
The best treatment for gangrene is revascularization, the restoration of blood flow to the affected area.Can reverse some of the effects of necrosis and allow healing.
The method of treatment is generally determined depending on location of affected tissue and extent of tissue loss.
Prevention
Gangrene may be prevented if it is treated before the tissue damage is irreversible.Wounds should be treated properly and watched carefully for signs of infection (such as spreading redness, swelling, or drainage) or failure to heal.
People with diabetes or blood vessel disease should routinely examine their feet for any signs of injury, infection, or change in skin color and seek care as needed.