The Lymphatic System and Lymph Nodes
(1) Removes water, electrolytes, low-molecular-weight moieties (polypeptides,
cytokines, growth factors) and macromolecules (fibrinogen, albumin,
globulins, coagulation and fibrinolytic factors) from the interstitial fluid (ISF)
and returns them to the circulation.
Functions
:
(2) Permits the circulation of lymphocytes and other immune cells.
(3) Intestinal lymph (chyle) transports cholesterol, long-chain fatty acids,
triglycerides and the fat-soluble vitamins (A, D, E and K) directly to the
circulation, bypassing the liver.
Resting 1SF is negative (—2 to —6 mmH2O), whereas lymphatic pressures
are positive, indicating that lymph flows against a small pressure gradient. It is
believed that prograde lymphatic flow depends upon three mechanisms:
1. Transient
increases in interstitial pressure
secondary to muscular contraction and
external compression.
Mechanisms of lymph transport
:
2. The sequential contraction and relaxation of
lymphangions.
(Valves partition the
lymphatics into segments).
3. The prevention of reflux due to
valves
.
Lymphangions are believed to respond to increased lymph flow in much the
same way as the heart responds to increased venous return in that they increase their
contractility and stroke volume. Contractility is also enhanced by noradrenaline,
serotonin, certain prostaglandins and thromboxanes, and endothelin- 1. Lymphatics
may also modulate their own contractility through the production of nitric oxide and
other local mediators. Transport in the thoracic and right lymph ducts also depends
upon intrathoracic (respiration) and central venous (cardiac cycle) pressures.
Therefore, cardiorespiratory disease may have an adverse effect on lymphatic
function.
In summary, in the healthy limb, lymph flow is largely due to intrinsic lymphatic
contractility, although this is augmented by exercise, limb movement and external
compression. However, in lymphoedema, when the lymphatics are constantly
distended with lymph, these external forces assume a much more important
functional role.
Acute Lymphangitis
Definition:
It is infection spreading from a skin (wound, abrasion, laceration)
through the draining superficial lymphatic vessels to the draining lymph nodes. It is
usually seen in the extremities (upper and lower limbs).
Causative Microorganisms:
1) Group A B-haemolytic streptococci (streptococcus
pyogenes), 2) Staphylococcus aureus.
(1)
Red blushes or streaks in the skin
(correspond to inflamed lymphatics)
extending from the source of infection to the regional LNs.
Clinical Presentation:
(2)
Regional LNs
are enlarged and tender and may suppurate with abscess
formation, occasionally the infection bypasses one group to affect another at a
higher level (e.g, if the point of infection is the foot, an abscess may form in the
external iliac group of LNs rather than the superficial (lower) and deep inguinal
groups and because the point of infection may have healed and been forgotten,
by the time the mass appears it may be mistaken for an (appendix abscess).
(1)
Bed rest
(to reduce lymphatic drainage) with elevation of the affected limb (to
reduce swelling).
Treatment:
(2)
Antibiotics
. Failure to improve within 48 hours suggests inappropriate
antibiotic therapy, or the presence of undrained pus, or the presence of an
underlying systemic disorder (malignancy, immunodeficiency).
(3)
Drainage of an abscess
if it has formed.
(1)
Post-lymphatic oedema
. due to permanent lymphatic obstruction after
resolution of acute lymphangitis leading to persistent oedema. These patients
are prone to so-called acute inflammatory episodes (AlEs).
Complications:
(2)
Chronic lymphangitis
. Follows repeated attacks of acute lymphangitis.
(3)
Bacteraemia or Septicaemia
.
LYMPHOEDEMA
Definition
:
It is abnormal limb swelling due to the accumulation of increased
amounts of high protein ISF secondary to defective lymphatic drainage in the
presence of (near) normal net capillary filtration. So it is accumulation of fluid in
the interstitial spaces (extracellular fluid compartment), in the limbs it accumulates
mainly in the subcutaneous tissues.
1) Gradually
increasing circumference of the affected limb
(huge enlargement) with
multifolding of the skin.
Clinical Presentation
:
2) In the early stages the lymphoedema is
pitting
on pressure thus it simulates
ordinary oedema, but with time lymphoedema characteristically becomes Non-
pitting lymphoedema due to subcutaneous thickening with fibrous tissue being
worsened by recurring low grade lymphangitis and cellulitis. (Recurrent acute
infective episodes). In the early stages, lymphoedema will ‘pit’ and the patient
will report that the swelling is down in the morning. This represents a reversible
component to the swelling, which can be controlled. Failure to do so allows
fibrosis, dermal thickening and hyperkeratosis to occur.
3) Unlike other types of oedema, Iymphoedema characteristically involves the
foot
.
The contour of the ankle is lost through infilling of the submalleolar depressions,
a ‘buffalo hump’ forms on the
dorsum of the foot, the toes appear ‘square’ due to confinement of footwear, and
the skin on the dorsum of the toes cannot be pinched due to subcutaneous
fibrosis (Stemmer’s sign) Lymphoedema usually spreads proximally to knee
level and less commonly affects the whole leg.
4)
Lymphangiomas
are dilated dermal lymphatics that ‘blister’ onto the skin
surface. The fluid is usually clear but may be bloodstained and, in the long term,
they thrombose and fibrose, forming hard nodules and raising concerns about
malignancy. If lymphangiomas are < 5 cm across, they are termed
lymphangioma circumscriptum
, and if they are more widespread, they are termed
lymphangioma diffusum
. If they form a reticulate pattern of ridges then it has
been termed
lymphoedema ab igne
. Lymphangiomas frequently weep
(lymphorrhoea, chylorrhoea), causing skin maceration and they act as a portal for
infection.
5)
Lymphangiosarcoma
was originally described in post-mastectomy oedema
(Stewart—Treves syndrome) and affects around 0.5% of patients at a mean onset
of 10 years. However, lymphangiosarcoma can develop in any longstanding
lymphoedema, but usually takes longer to manifest (20 years). It presents as

single or multiple bluish/red skin and subcutaneous nodules that spread to form
satellite lesions that may then become confluent.
6)
Ulceration, non-healing bruises, and raised purple-red nodules
should lead to
suspicion of malignancy.
7)
Constant dull ache, even severe pain or Burning and bursting
sensations or Pins
and needles.
8)
Sensitivity to heat
.
9)
General tiredness and debility
.
10)
Skin problems
, including dehydration, flakiness, weeping, excoriation and
breakdown. Chronic eczema, fissuring, verrucae and papillae (warts) are
frequently seen in advanced disease. Ulceration is unusual, except in the
presence of chronic venous insufficiency.
11)
Immobility, leading to obesity and muscle wasting
.
12)
Backache and joint problems
.
13)
Fungal infection
of the skin (dermatophytosis) and nails (onychomycosis)
Athlete’s foot.
Pathophysiology:
The 1SF compartment (10-12 litres in a 70-kg man) constitutes 50% of the
wet weight of skin and subcutaneous tissues and, in order for oedema to be
clinically detectable, its volume has to double. About 8 litres (protein concentration
approximately 20-30g/L, similar to ISF) of lymph is produced each day and travels
in afferent lymphatics to lymph nodes. There, the volume is halved and the protein
concentration doubled, resulting in 4 litres of lymph re-entering the venous
circulation each day via efferent lymphatics. In one sense, all oedema is
lymphoedema in that it results from an inability of the lymphatic system to clear the
ISF compartment. However, in most types of oedema this is because capillary
filtration rate is pathologically high and overwhelms a normal lymphatic system,
resulting in the accumulation of low-protein oedema fluid. In contrast, in true
lymphoedema, when the primary problem is in the lymphatics, capillary filtration is
normal and the oedema fluid is relatively high in protein. Of course, in a significant
number of patients with oedema there is both abnormal capillary filtration and
abnormal lymphatic drainage. Lymphoedema
results from
lymphatic 1-aplasia, 2-
hypoplasia, 3-dysmotility (reduced contractility with or without valvular
insufficiency), 4-obliteration by inflammatory, infective or neoplastic processes, or
5-surgical extirpation. Whatever the primary abnormality, the resultant physical
and/or functional obstruction leads to lymphatic hypertension and distension, with
further secondary impairment of contractility and valvular competence.
Lymphostasis and lymphotension
lead to the accumulation in the ISF of fluid,
proteins, growth factors and other active peptide moieties, glycosaminoglycans and
particulate matter, including bacteria. As a consequence, there is increased collagen
production by fibroblasts, an accumulation of inflammatory cells (predominantly
macrophages and lymphocytes) and activation of keratinocytes. The end result is
protein-rich oedema fluid, increased deposition of ground substance, subdermal
fibrosis and dermal thickening and proliferation. Lymphoedema, unlike all other
types of oedema, is confined to the epifascial space. Although muscle
compartments may be hypertrophied owing to the increased work involved in limb
movement, they are characteristically free of oedema.
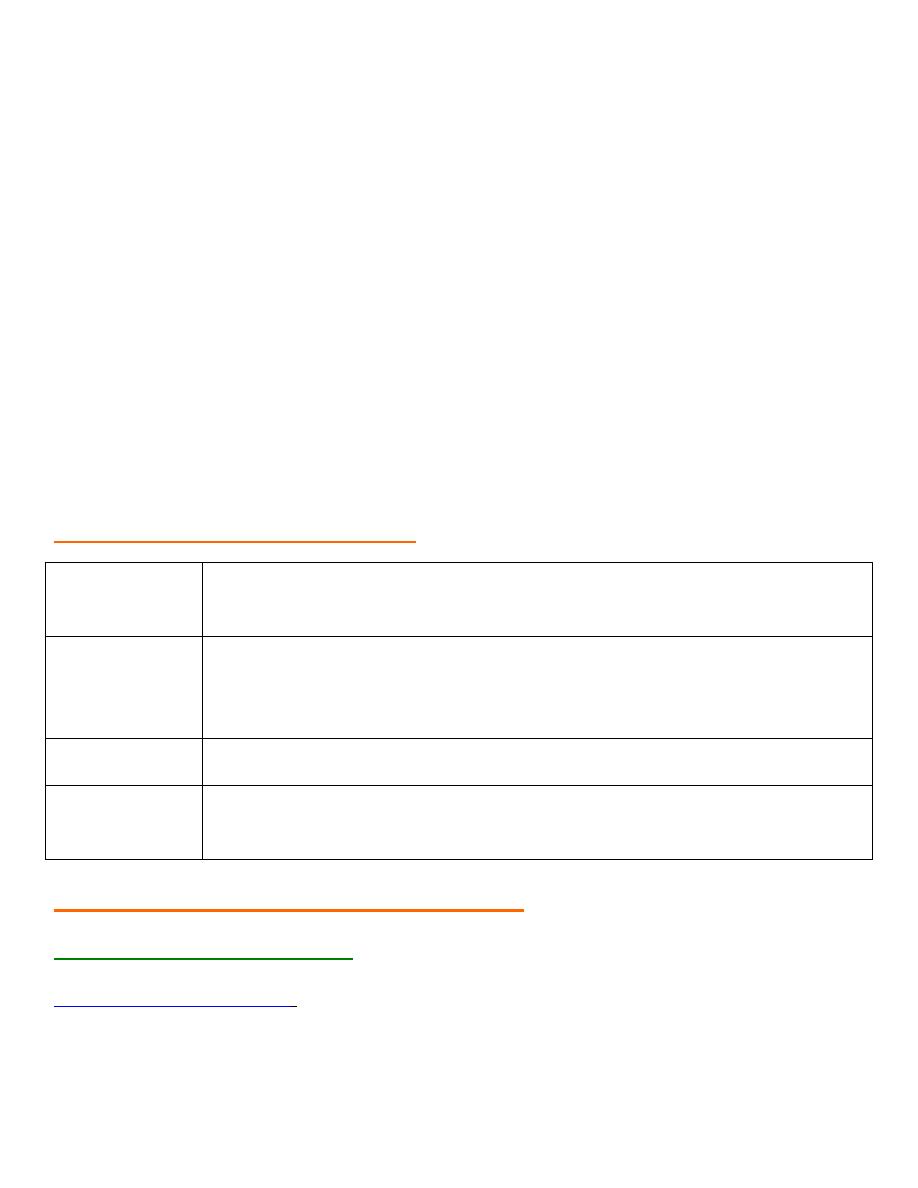
Ordinary Oedema
Lymphoedema
Pitting.
Nonpitting(due to excessive collagen
deposition).
Involves epifascial, subfascial and
muscle compartments.
Is confined to the epifascial space only.
capillary filtration rate is
pathologically high and overwhelms a
normal lymphatic system, resulting in
the accumulation of low-protein
oedema fluid.
capillary filtration is normal but there is an
abnormal lymphatic drainage system and
the oedema fluid is relatively high in
protein.
In general, primary lymphoedema progresses more slowly than secondary
lymphoedema. Two main types of lymphoedema are recognised:
Classification
1- Primary lymphoedema
, in which the cause is unknown (or at least uncertain
and unproved), but often presumed to be due to (congenital lymphatic dysplasia),
Primary lymphoederna is usually further subdivided on the basis the presence of
family, age of onset and lymphangiographic findings:
a - Congenital
(onset < 2 years old).
· Sporadic.
· Familial (Milroy’s disease).
b - Praecox
(onset 2 - 35 years old).
· Sporadic.
· Familial (Meige’s disease).
c - Tarda
(onset after 35 years old).
2- Secondary lymphoedema
, in which there is a clear underlying cause, such as
inflammation, malignancy or surgery.
1- Infection
.
a - Parasitic infection (filariasis).
b - Fungal infection (tinea pedis).
2- Exposure to foreign body material
(silica particles).
3- Malignancy
.
a- Primary lymphatic malignancy.
b- Metastatic spread to lymph nodes.
4- Surgery
. Excision of LNs.
5- Radiotherapy
. to groups of lymph nodes.
6- Trauma
. (particularly degloving injuries).
7- Venous complications
.
a- Superficial thrombophlebitis.
b- Deep venous thrombosis.
Grade
(
Brunner
)
Clinical classification of lymphoedema
Clinical features
Subclinical
(latent)
I
Oedema pits on pressure and the swelling largely, or completely
disappears on elevation and bed rest.
II
Oedema does not pit and does not significantly reduce upon elevation.
Ill
Oedema is associated with irreversible skin changes, i.e. fibrosis,
papillae.
Differential diagnosis of the swollen limb
(1) Non-vascular or lymphatic
1- Cardiac failure from any cause.
1) General disease states
.
2- Liver failure.
3- Hypoproteinaemia due to nephrotic syndrome, malabsorption, protein- losing
enteropathy.
4- Hypothyroidism (myxoedema).
5-Allergic disorders, including angioedema and idiopathic cyclic oedema.
6-Prolonged immobility and lower limb dependency.
2) Local disease processes
. (Ruptured Baker’s cyst, Myositis ossificans, Bony or
soft-tissue tumours, Arthritis, Haemarthrosis, Calf muscle haematoma, Achilles
tendon rupture).
3) Retroperitoneal fibrosis
.May lead to arterial,venous and lymphatic abnormalities.
4) Gigantism
. (Rare, all tissues are uniformly enlarged).
5) Drugs
. Corticosteroids (oestrogens, progestagens), Monoamine oxidase
inhibitors (phenylbutazone, methyldopa, hydralazine, nifedipine).
6) Trauma
. Painful swelling due to reflex sympathetic dystrophy
7) Obesity
. (Lipodystrophy, Lipoidosis).
(2)Venous
:
1) Deep venous thrombosis
.(There may be an obvious predisposing factor, such as
recent surgery,The classical signs of pain and redness may be absent).
2) Post-thrombotic syndrome
. (Swelling, usually of the whole leg, due to
iliofemoral venous obstruction,Venous skin changes, secondary varicose veins on
the leg and collateral veins on the lower abdominal wall,Venous claudication may
be present).
3) Varicose veins
. Simple primary varicose veins are rarely the cause of significant
leg swelling.
4) Klippel—Trenaunay syndrome and other malformations
. (Rare) Present at birth
or develops in early childhood, Comprises an abnormal lateral venous complex,
capillary naevus, bony abnormalities, hypo(a)plasia of deep veins and limb
lengthening, Lymphatic abnormalities often coexist.
5) External venous compression
. Pelvic or abdominal tumour including the gravid
uterus, Retroperitoneal fibrosis.
6) lschaemia—Reperfusion
.
Following lower limb revascularisation for chronic
ischaemia.
(3) Arterial
1) Arteriovenous malformation
. May be associated with local or generalised
swelling
2) Aneurysm
. (Popliteal, Femoral, False aneurysm following (iatrogenic) trauma).
1- Lyrnphangiosarcoma (Stewart—Treve’s syndrome).
2- Kaposi’s sarcoma (human immunodeficiency virus, HIV).
3- Squamous cell carcinoma.
4- Liposarcoma.
5- Malignant melanoma .
6- Malignant fibrous hisfiocytoma.
7- Basal cell carcinoma.
8- Lymphoma.
Malignancies associated with lymphoedema
INVESTIGATION OF LYMPHOEDEMA
(1) Routine tests
:
1-Full blood count, 2-Urea and electrolytes, creatinine. 3- Liver function tests. 4-
Chest radiography. 5-Blood smear for microfilariae.
(2) Lymphangiography
:
1- Direct lymphangiography
involves the injection of contrast medium into a
peripheral lymphatic vessel and subsequent radiographic visualisation of the vessels
and nodes. It remains the ‘gold standard’ for showing structural abnormalities of
larger lymphatics and nodes. However, it can be technically difficult, it is
unpleasant for the patient, it may cause further lymphatic injury and, largely, it has
become obsolete as a routine method of investigation. Few centres now perform this
technique and those that do generally reserve it for preoperative evaluation of the
rare patient with megalymphatics who is being considered for bypass or fistula
ligation.
2-Indirect lymphangiography
involves the intradermal injection of water- soluble,
non-ionic contrast into a web space, from where it is taken up by lymphatics and
then followed radiographically, It will show distal lymphatic but not normally
proximal lymphatics and nodes.
(
3) Isotope Lymphoscintigrcaphy
:
This has largely replaced lymphangiography as the primary diagnostic technique in
cases of clinical uncertainty. Radioactive technetium-labelled protein or colloid
particles are injected into an interdigital web space and specifically taken up by
lymphatics, and serial radiographs are taken with a gamma camera. The technique
provides a qualitative measure of lymphatic function rather than quantitative
function or anatomical detail.
(4) Computerised Tomography
A single, axial computerised tomography (CT) slice through the midcalf has been
proposed as a useful diagnostic test for lymphoedema (coarse, non-enhancing,
reticular ‘honeycomb’ pattern in an enlarged subcutaneous compartment), venous
oedema (increase volume of the muscular compartment), and lipoedema (increased
subcutaneous fat). CT can also be used to exclude pelvic or abdominal mass lesions.
(
5) Magnetic resonance imaging
Magnetic resonance imaging (MRI) can provide clear images of lymphatic channels
and lymph nodes, and can be useful in the assessment of patients with lymphatic
hyperplasia. MRI can also distinguish venous and lymphatic causes of a swollen
limb.
(6) Ultrasound
Ultrasound can provide useful information about venous function.
MANAGEMENT OF LYMPHOEDEMA
(1) Relief of pain
On initial presentation, 50% of patients with lymphoedema complain of significant
pain. The pain is usually multifactorial and its severity and underlying cause(s) will
vary depending on the aetiology of the lymphoedema. For example, following
treatment for breast cancer, pain may arise from the swelling itself, (radiation and
surgery induced) nerve (brachial plexus and intercostobrachial nerve), bone
(secondary depositis, radiation necrosis) and joint disease (arthritis, bursitis,
capsulitis), and recurrent disease
.
Use of
(1)non-opioid(
NSAIDs
) and (2)
opioid analgesics
, (3)
corticosteroids
,
(4)
tricyclic antidepressants
, (5)
muscle relaxants
, (6)
anti-epileptics
, (7)
nerve blocks
,
(8)
physiotherapy
, (9)
adjuvant anti-cancer therapies
(chemo-, radio- and hormonal
therapy).
(2) Control of swelling
Physical therapy for lymphoedema comprising
1-bed rest
,
2-elevation
,
3-bandaging
,
4-compression garments, 5-massage and 6-exercises. The current preferred term is
decongestive lymphoedema therapy (DLT)
and comprises two phases. The first is a
short
intensive period
of therapist-led care and the second is a
maintenance phase
in
which the patient uses a self-care regimen with occasional professional intervention.
The intensive phase comprises skin care, manual lymphatic drainage (MLD) and
multi-layer lymphoedema bandaging (MLLB), and exercises.
(3) Skin care
1- Protect hands when washing up or gardening; wear a thimble when sewing.
2- Never walk barefoot and wear protective footwear outside.
3- Use an electric razor to depilate.
4- Never let the skin become macerated.
5- Treat cuts and grazes promptly (wash, dry, application of antiseptic and a
plaster).
6- Use insect repellent sprays and treat bites promptly with antiseptics and
antihistamines.
7- Seek medical attention as soon as limb becomes hot, painful or more swollen.
8- Do not allow blood to be taken from, or injections to be given into the affected
arm (and avoid blood pressure measurement).
9- Protect the affected skin from sun (shade, high factor sun block).
10- Consider taking antibiotics if going on holiday.
(
3) Manual lymphatic drainage
Aim to evacuate fluid and protein from the 1SF space, and stimulate lymphangion
contraction. The therapist should perform MLD daily; they should also train the
patient (and/or carer) to perform a simpler, modified form of massage, termed
simple lymphatic drainage (SLD). In the intensive phase, SLD supplements MLD
and, once the maintenance phase is entered, SLD will carry on as daily massage.
(4) Multilayer lymphoedema bandaging and compression garments
Elastic bandages
provide compression, produce a sustained high resting pressure
and ‘follow in’ as limb swelling reduces. However, the sub-bandage pressure does
not alter greatly in response to changes in limb circumference consequent upon
muscular activity and posture. By contrast, short-stretch bandages exert support
through the production of a semi-rigid casing where the resting pressure is low but
changes quite markedly in response to movement and posture. It is generally
believed that non-elastic multilayer lymphoedema bandaging (MLLB) is preferable
(and arguably safer) in patients with severe swelling during the intensive phase of
DLT, whereas compression (hosiery, sleeves) is preferable in milder cases and
during the maintenance phase. Whether the aim is to provide support or
compression, the pressure exerted must be graduated (100% ankle/foot, 70% knee,
50% midthigh, 40% groin) and, of course, the adequacy of the arterial circulation
must be assessed.
Compression garments
form the mainstay of management in most clinics. The
control of lymphoedema requires higher pressures (30—40 mmHg arm, 40—60
mmHg leg) than are typically used to treat CVI. The patient should put the stocking

on first thing in the morning before rising. Donning and doffing lymphoedema
grade stockings is difficult and many patients find them intolerably uncomfortable,
especially in warm climates.
Pneumatic compression devices
, Unless the device being used allows the sequential
inflation of multiple chambers up to > 50 mmHg, it will probably be ineffective for
lymphoedema.
(5) Exercise.
Lymph formation is directly proportional to arterial inflow and 40% of lymph is
formed within skeletal muscle. Vigorous exercise, especially if it is anaerobic and
isometric, will tend to exacerbate lymphoedema and patients should be advised to
avoid prolonged static activities, for example carrying heavy shopping bags or
prolonged standing. In contrast, slow, rhythmic, isotonic movements (e.g.
swimming) and massage will increase venous and lymphatic return through the
production of movement between skin and underlying tissues (essential to the
filling of initial lymphatics) and augmentation of the muscle pumps. Exercise also
helps to maintain joint mobility. Patients who are unable to move their limbs benefit
from passive exercises.
(6) Limb Elevation
.
When at rest, the lymphoedematous limb should be positioned with the foot/hand
above the level of the heart. A pillow under the mattress or blocks under the bottom
of the bed will encourage the swelling to go down overnight.
(7) Drugs
.
The
benzpyrones
are a group of several thousand naturally occurring substances, (
flavonoids) they reduce capillary permeability, improve microcirculatory perfusion,
stimulate interstitial macrophage proteolysis, reduce erythrocyte and platelet
aggregation, scavenge free radicals and exert an anti-inflammatory effect
.
Oxerutins
(paroven)
.
Diuretics
are of no value in pure lymphoedema. Their chronic use is associated
with side-effects, including electrolyte disturbance, and should be avoided.
(8) Surgery
Only a small minority of patients with lymphoedema benefit from surgery.
1- Bypass procedures
The rare patient with proximal ilioinguinal lymphatic obstruction and normal distal
lymphatic channels might benefit, from lymphatic bypass. Methods:
1-Omental pedicle.
2-Skin bridge (Gillies).
3-Anastomosing lymph nodes to veins (Neibulowitz).
4-Ileal mucosal patch (Kinmonth).
5-Direct lymphovenous anastomosis.
2- Limb reduction procedures
These are indicated when a limb is so swollen that it interferes with mobility and
livelihood. These operations are not ‘cosmetic’ in the sense that they do not create a
normally shaped leg and are usually associated with significant scarring.
1-Sistrunk
. A wedge of skin and subcutaneous tissue is excised and the wound
closed primarily. This is most commonly carried out to reduce the girth of the thigh.
2-Homans
. First skin flaps are elevated, to allow the excision of a wedge of skin
and a larger volume of subcutaneous tissue down to the deep fascia from beneath
the flaps, which are then trimmed to size to accommodate the reduced girth of the
limb and closed primarily. This is the most satisfactory operation for the calf. The
main complication is skin flap necrosis. There must be at least 6 months between
operations on the medial and lateral sides of the limb and the flaps must not pass the
midline to avoid skin flap necrosis. This procedure has also been used on the upper
limb, but is contraindicated in the presence of venous obstruction or active
malignancy.
3-Thompson
One denuded skin flap is sutured to the deep fascia and buried beneath
the second skin flap (the so-called ‘buried dermal flap’). This procedure has become
less popular as pilonidal sinus formation is common. The cosmetic result is no
better than that obtained with the Homans’ procedure and there is no evidence that
the buried flap establishes any new lymphatic connection with the deep tissues.
4-Charles
This operation was initially designed for filariasis and involved
circumferential excision of all the skin and subcutaneous tissues (lymphoedematous
tissue) down to and including the deep fascia, with coverage using split-skin grafts.
This leaves a very unsatisfactory cosmetic result and graft failure is not uncommon.
However, it does enable the surgeon to reduce greatly the girth of a massively
swollen limb(allows the surgeon to remove very large amounts of tissue and is
particularly useful in patients with severe skin changes).
