29 years old female evaluated in the emergency department for two days history of blurred vision,diplopia,slurred speech, followed by bilateral upper extremity weakness.examination of the patient ,the patient was alert,,awake fully oriented,afebrile,blood pressure 90/60,pulse rate 50/min,and respiratory rate 12/min,pupiledilated,with bilateral VI nerve palsy and she cannot abduct her arm against resistance.brain CT and cerebrospinal fluid examination normal
Which of the following is the most likely diagnosis
a-botulismb-Guillain –Barre syndrome
c- stroke
d-poliomylitis
e- meningitis
Botulism
Clostridium botulinum
Gram positiveObligate anaerobic bacillus
Spores
Ubiquitous
Resistant to heat, light, drying and radiation
Specific conditions for germination
Anaerobic conditions
Warmth (10-50oC)
Mild alkalinity
Neurotoxins
eight different types: A through GDifferent types affect different species
All cause flaccid paralysis
Only a few nanograms can cause illness
Binds neuromuscular junctions
Toxin: Destroyed by boiling
Spores: Higher temperatures to be inactivated
History
1793, Justinius Kerner“Wurstgift”
“Botulus” = Latin for sausage
1895, Emile von Ermengem
Isolated organism during Belgium outbreak
Transmission
IngestionOrganism
Spores
Neurotoxin
Wound contamination
Inhalation
Person-to-person not documented
Categories of Human Botulism
• Foodborne botulism• Infant botulism
• Wound botulism
• Adult infectious botulism
Foodborne Botulism
Preformed toxin ingested from contaminated foodMost common from
home-canned foods
Asparagus, green beans, beets, corn, baked potatoes, garlic, chile peppers, tomatoes;
Improperly fermented fish (Alaska); type E
Infant Botulism
Most common form in U.S.Spore ingestion
Germinate then toxin released and colonize large intestine
Infants < 1 year old
94% < 6 months old
Spores from varied sources
Honey, corn syrup
Wound Botulism
1951 Wound botulism was described for the first time.is rare and organism gets into an open wound
Develops under anaerobic conditions
organism typically comes from ground-in dirt or gravel
It does not penetrate intact skin
Adult Clinical Symptomes
Nausea, vomiting, diarrheaCranial nerve involvement, which almost always marks the onset of symptoms, usually produces
Double vision
Difficulty speaking or swallowing
Descending Symmetrical flaccid paralysis
Respiratory muscle paralysisParalytic ileus, severe constipation
urinary retention are common.
Typically, they have no fever or it is rare
Patients are usually alert and orientedPtosis is frequent; the pupillary reflexes may be depressed
fixed or dilated pupils are noted in half of patients.
The gag reflex may be suppressed,
have intact deep tendon reflexes
Sensory findings are usually absent.
Infant Clinical Signs
ConstipationLethargy
Poor feeding
Weak cry
Bulbar palsies
Failure to thrive
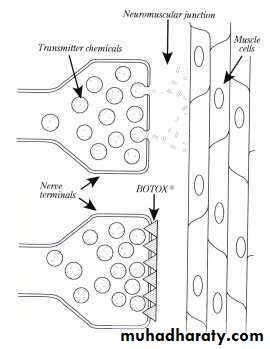
Mechanism of Toxin
Neurotoxin 0 binds to neurons 0internalized 0
prevents release of acetyl choline (neurotrasmitter)Diagnosis
A diagnosis of botulism is clinical and must be considered in patients withsymmetric descending paralysis
who are afebrile
and mentally intact
Toxin in serum, stool, gastric aspirate, suspected food
Culture of stool or gastric aspirate
Takes 5-7 days
Electromyography also diagnostic
Differentiate from?
Guillain-Barré syndromea and its variants, especially Miller-Fisher variant paralysisHistory of antecedent infection
paresthesias often ascending
early areflexia;
EMG findings
Myasthenia gravis:
Recurrent paralysis
EMG findings
Stroke
Paralysis often asymmetricabnormal CNS image
Lambert-Eaton syndrome
EMG: Increased strength with sustained contractionevidence of lung carcinoma
CNS infections, especially of the brainstem
TreatmentIntensive care immediately
Patients should be hospitalized and monitored closely, both clinically and by spirometry, pulse oximetry, and measurement of arterial blood gases for incipient respiratory failure
equine antitoxin should be administered as soon as possible after specimens are obtained for laboratory analysis
Treatment
In food-borne casepurging the gut with cathartics ,enemas, and emetics to remove unabsorbed toxin also may be of value.