Allergic Diseases
ByProf. Dr. Zainalabideen A. Abdulla,
MRCPI , Ph.D, FRCPath.
Allergic Diseases
Objectives of the lecture1. To the most important allergic diseases,
and their clinical features, investigation,
diagnosis and management.
2. To elaborate on anaphylaxis as a medical
emergency.
3. To show you some important images for
the above mentioned aspects.
Reference
Davidson’s Principle & Practice of Medicine
Allergic Diseases
Allergy is a medical term which means that the patient develops symptoms upon contact with allergens to which he/she is sensitized.
Atopy (= placelessness, unclassifiable) is inappropriate (exaggerated) IgE antibody production to harmless environmental substances (allergens) in a genetically predisposed individual but not necessarily develops symptoms (silent).
So, atopy is a condition for the development of allergy but is not itself allergy (i.e. you need to be atopic to become allergic, but not all atopic people develop allergy).
Prevalence of Allergic Diseases
Allergic diseases affect about 15-20% of the population. A child whose parents do not suffer from allergy has a 15% chance of becoming allergic; if the mother is allergic the risk increases to 60% and if both parents are allergic the risk is 80% (i.e. sometimes allergies can jump a generation).Pseudo-allergy/anaphylactoid reactions These conditions are with similar symptoms to allergy but are not caused by IgE and occur commonly in non-atopic people (with no history of allergy in the family). They are caused by the release of histamine and results in a spectrum of symptoms vary from rash to anaphylaxis. They are usually caused by aspirin, NSAIDs (e.g. Ibuprofen), opiates, and I.V. radiocontrast media.
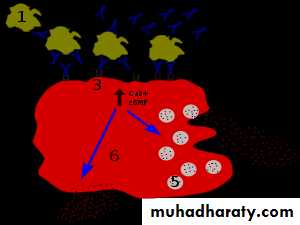
Pathology and predisposition to allergic diseases
** Refer to you immunology lecture/type I hypersensitivity.“Hygiene hypothesis” may explain the susceptibility to development of allergy. Infections in early life may protect from development of allergy (i.e. good sanitation and health care may lead to a penalty of development of allergy). Genetic predisposition, mechanisms of IgE exaggerated production, ability of epithelial barrier to protect against entrance of allergic agents, and environmental factors such pollution and cigarette smoke, are all contributory factors to the development of allergic diseases.
Common allergic disease
1. Urticaria and angioedema.2. Atopic dermatitis
3. Allergic conjunctivitis
4. Allergic rhinitis (hay fever)
5. Allergic asthma
6. Food allergy
7. Drug allergy
8. Allergy to insect venom
9. Anaphylaxis/ Anaphylactoid
General clinical assessment
1. The nature of symptoms and specific triggers of allergy. Potential allergens in the home and workplace should be identified.
2. The time lag between exposure to a potential allergen and onset of symptoms (allergic reaction occurs within minutes after exposure to allergens).
3. Enquiry about other concomitant allergic conditions (past or present),
4. Family history of allergic diseases.
5. Drug history should be taken including compliance, side effects, and complementary therapies. Differentiate drug allergy from side effects, overdose and intolerance of the drugs.
Urticaria (nettle rash, hives)
Is an area of focal dermal oedema secondary to transient increase in capillary permeability. It lasts < 24 hours (vs > 24 hours in urticarial vasculitis due to hepatitis B, SLE or idiopathic). This can be clarified by drawing around a weal with a pen and examining the patient 24 hours later. When present for <6 weeks it is an acute urticaria (may be associate with angioedema of lips, face or throat), and for >6 weeks it s a chronic urticaria. Urticaria is characterized by itching.Management urticaria
1. Non-sedative antihistamine (e.g. loratidine, fexofenadine or cetrizine).2. If no response, add H2-blocker such as cimetidine or ranitidine.
3. Mast cell stabilizers or leukotriene inhibitors (montelukast “singulair or lukotas” 10 mg tablet once daily, Zafirlukas 20-40 mg once daily) may also be used.
4. Systemic corticosteroids are widely used, but are of little benefit.
Angioedema
Angioedema is the episodic, localized, non-pitting swelling of submucous or subcutaneous tissues. It affects most commonly the face, extremities and genitalia. When involves the larynx/ tongue or intestine, it may cause life-threatening respiratory obstruction or abdominal pain and distension respectively. Angioedema is characterized by pain without itching.
Types of angioedema
1. Allergic reaction to specific triggers; treated with anti-histamine2. Idiopathic angioedema; treated with anti-histamine
3. Hereditary angioedema; treated with modified androgen derivative (danazol), pure C1INH infusion, or fresh frozen plasma
4. ACE-inhibitor (ACEI) associated angioedema ; stop the medication
Anaphylaxis
Anaphylaxis is a potentially life- threatening, systemic allergic reaction caused by degranulation of mast cells and release of vasoactive amines. Death may occur if the patient has a preexisting asthma or adrenaline (epinephrine) administration is delayed.Clinical assessment
The severity, time between exposure to allergens and onset of the symptoms, potential triggers and route of exposure (e.g. drugs, foods, latex, insect venom...etc) should assessed since the clinical features depends on these factors. If an allergen is inhaled the major symptom is frequently wheezing. Venom or drug exposure should be differentiated from their direct toxic effects.
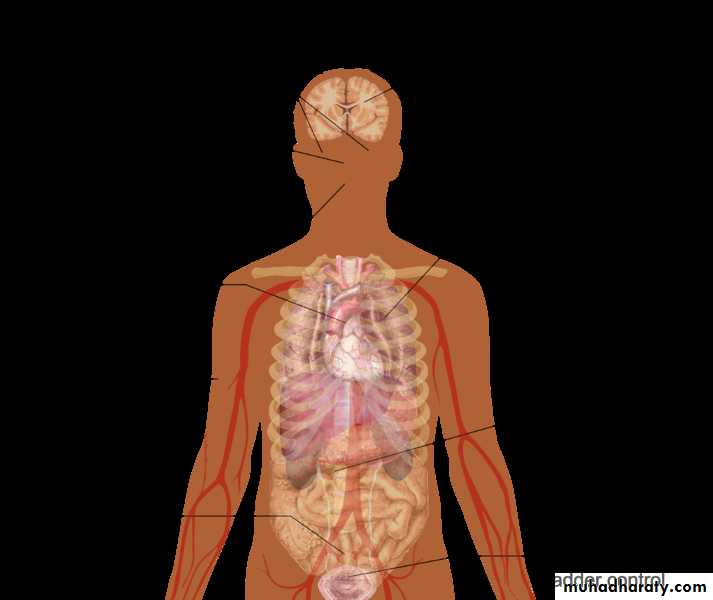
Clinical manifestations of anaphylaxis Anaphylaxis starts in few minutes up to one hour.
Symptoms : Impending doom (death), loss of consciousness, shortness of breath, generalized skin rash with itching mainly of the palms, soles and genitalia, and abdominal pain /diarrhoea.On examination: Laryngeal obstruction, stridor, tachypnoea, angioedema of lips, eyes and mucous membranes, flushing and sweating, and urticaria with discrete erythematous wheels with raised margins, hypotension, wheeze, and tachycardia or cardiac arrhythmias.
Management of Anaphylaxis
Anaphylaxis is an acute medical emergency, and should be handled immediately:1. Prevent further contact with allergen (e.g. removal of bee sting).
2. Ensure airway (may need endo-tracheal intubation).
3. Administration of I.M. adrenaline immediately: 0.3 – 1.0 ml of 1:1000 solution, repeat at 5-10 min. intervals if response is inadequate.
4. Administration of antihistamine: e.g. chlorphenamine 10 mg I.M. or slow I.V. injection.
5. Administration of corticosteroids: e.g. hydrocortisone 200 mg I.V. (prevents rebound symptoms)
6. Supportive treatments including:
A. Nebulised beta2-agonist to decrease brochocontriction [e.g.
salbutamol (ventolin), terbutaline (bricanyl)[.
B. I.V. fluid to restore or maintain B.P. (6 liters might be needed).
C. Oxygen
D. Keep the patient in an Intensive Care Unit (ICU) for 12 hours.
Cont./…Management of anaphylaxis
II. Recovered patients should be referred for specialist assessment. The aim is to identify the trigger factor, educate the patient for avoidance, and possible immunotherapy.
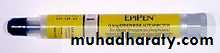
III. Self-injectable adrenaline (EpiPen) should be prescribed for patients suffered from previous anaphylaxis and they their families/carers should be instructed on its use. MedicAlet (or card) bracelet carried by the patient may also be useful.
General investigations for allergic diseases
Skin prick testIt is the “gold standard’’ of allergy testing. Droplets of diluted common allergens with a negative control are placed on the forearm, and are punctured through with a sterile lancet. After 15 min. a local weal and flare Antihistamine drugs should be discontinued 4 days before testing
Specific IgE tests
These tests can be done by ELISA, or previously by RIA (RAST).
Total serum IgE and eosinophilia
Raised or normal IgE level may present in allergy. Eosinophilia is common in atopic individuals, but >20% may be due to non-atopic causes.
Challenge test
It is a supervised exposure to allergens and usually performed special centres. It is useful in the investigation of occupational asthma or food allergy.
Mast cell tryptase
The peak of serum level is after 1-2 hours of exposure, and remains elevated for 24 hours afterwards. Usually it is measured at the time of the reaction, and 3 and 24 hours afterwards.
General management of allergy
1. Avoidance in the main step in the management.2. Antihistamine (block H1 receptors) in particular the long acting, non-sedating preparations are used for treatment and prophylaxis.
3. Corticosteroids decrease pro-inflammatory cytokines. They can also be used topically to minimize side effects.
4. Sodium cromoglicate (mast cells membrane stabilizers); used only for prophylaxis against asthma (“Intal” inhaler), allergic rhinitis (“Rynacrom” nasal spray), and allergic conjunctivitis (“Opticrom” eye drops).
5. Antigen-specific immunotherapy (hypo-sensitization/ de-sensitization) is carried out by subcutaneous injection of increasing amount of the sensitizing allergen. It is used for the treatment of allergic rhinitis, allergic asthma and stinging hypersensitivity, but not for food allergy, or chronic urticaria/angioedema.
6. Omalizumab (Xolair) is humanized monoclonal antibody (IgG1) that inhibits the binding of IgE to mast cells and basophils.