
vitamins

Vitamins
organic substances with key roles in certain metabolic pathways;
they are required in small amounts in food because they are
not synthesized in the body .
body stores is varied
vit12 and vitA need years to deplete the stores
folate and tiamine need weeks stores
Vitamins are
fat-soluble (vitamins A, D, E and K)
water-soluble (vitamins of the B complex group and vitamin
C).

Thiamin (vitamin B1)
• Function:
thiamin pyrophosphate (TPP), is an essential cofactor in
carbohydrate metabolism.
1. TPP is involved in the oxidative decarboxylation of
acetyl CoA in mitochondria.
2 .In the Krebs cycle, TPP is the key enzyme for the
decarboxylation of α-ketoacid.
Has role in peripheral nerve conduction(unknown mech.)
Thiamin (vitamin B1)
Source
many foodstuffs:
cereals, legumes, pork, as well as beef meat.
Coffee ,tea, raw fish (
thiaminase
) decrease the vitam.
milled and polished rice have little vitB1
Body stores are small and signs of deficiency quickly develop
with inadequate intake. (1 month)
Deficiency:
1. Cells cannot metabolize glucose aerobically ; this is
likely
to affect the nervous system .
2 .There is accumulation of pyruvic and lactic acids,
which produce vasodilatation and increased cardiac
output.
Causes:
1. poor diatary itake, in severe prolonged hyper -
emesis gravidarum .
3 . where the only food consumed is polished rice .
2 . In chronic alcohol-dependent patients ( absorption)
4. Chronic illness as cancer
Clinical feature
• Non specific at early stage : anorexia, fatigue, irritability
• Dry beriberi
1. Symmetrical peripheral neuropathy: Sensory and motor
pain and parasthesia
2.Cerebral involvement :
Wernicke-encephalopathy
. This syndrome, which
consists of mental impairment, cerebellar ataxia,
ophthalmoplegia and horizontal nystagmus .
Korsakoff syndrome
: loss of new memory
,confabulation
• Wet beriberi
high output failure (3 months)
peripheral neuropathy

Diagnosis :
measurement of the circulating thiamin concentration
enzymatic assay of transketolase activity.
Treatment :
• In acute thiamine deficiency with either cardiovascular or
neurologic signs, 100 mg/d of thiamine should be given
parenterally for 7 days, followed by 10 mg/d orally until there
is complete recovery. Cardiovascular and ophthalmoplegic
improvement occurs within 24 h.
• Other manifestations gradually clear, Wernicke-Korsakoff
syndrome may be permanent or persist for several months.
• NB. vitB1 must be replaced in alcoholic patient after feeding

Riboflavin (B2 )
• Riboflavin is a flavoprotein that is a cofactor for many
oxidative reactions in the cell for energy production.
Source :
widely distributed all plant and animal sources
milk, dairy products , cereals(main
source)
Meat , fish , egg , legumes(good source)
Diagnosis :
serum or urinary level
Deficiency :
Almost is dietary

Riboflavin (B2 )
Deficiency cause:
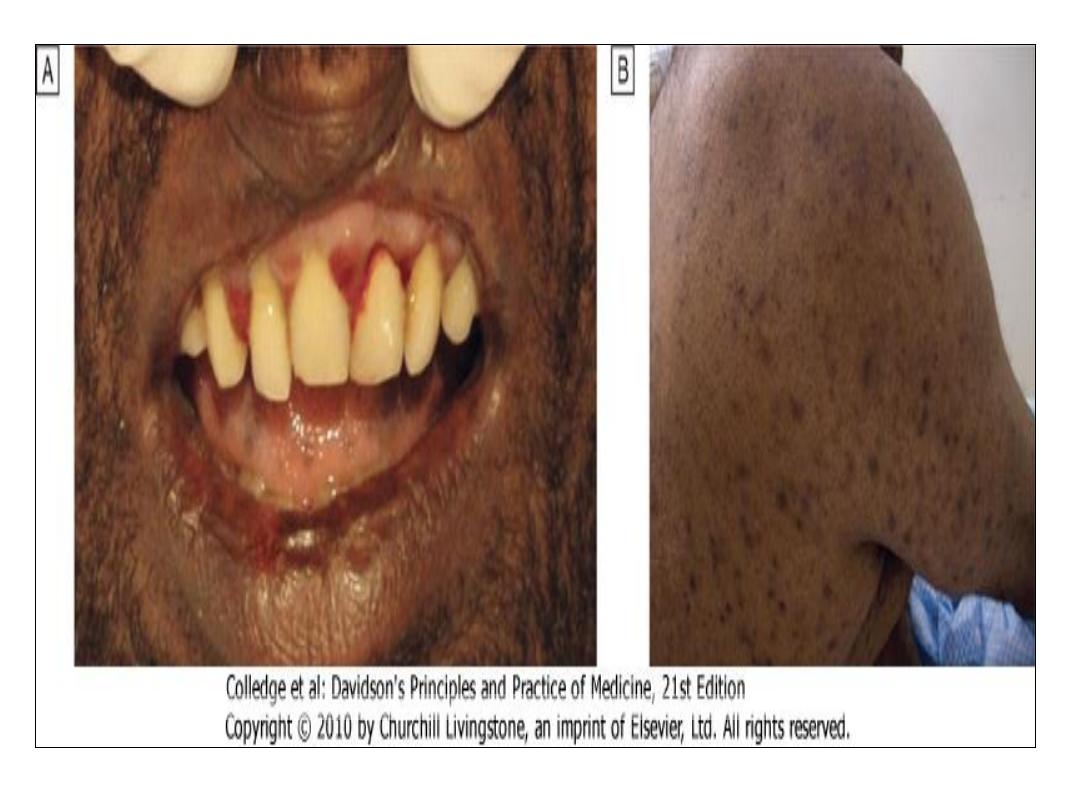
mucocutaneous lesion
1. Angular stomatitis or cheilosis
2. red, inflamed tongue
3. seborrhoeic dermatitis, particularly involving the face (around
the nose) and the scrotum or vulva.
4.Conjunctivitis with vascularization of the cornea .
5. Anemia
6. Personality changes
Treatment
Riboflavin 10 mg daily, usually given as the vitamin B complex.

Niacin (B3)
• This is the name for the two chemical forms, nicotinic acid and
nicotinamide .
• Many oxidative steps in the production of energy and in DNA
repair
source
• Niacin is found in many foodstuffs, including plants, meat and
fish. Niacin can be synthesized in humans from Eggs and milk
contain tryptophan.

Niacin (B3)
Causes of deficiency
:
1. Dietary deficiency (corn based diet).
2. In generalized malabsorption (rare).
3. In Hartnup's disease. (Tryptophan renaland git. absorp.
Defect)
4. In alcohol-dependent patients who do not eat.
5. In the carcinoid syndrome and, tryptophan is needed for
serotonine.
6.Isoniazid therapy can lead to a deficiency of vitamin B6, which
is needed for the synthesis from tryptophan.

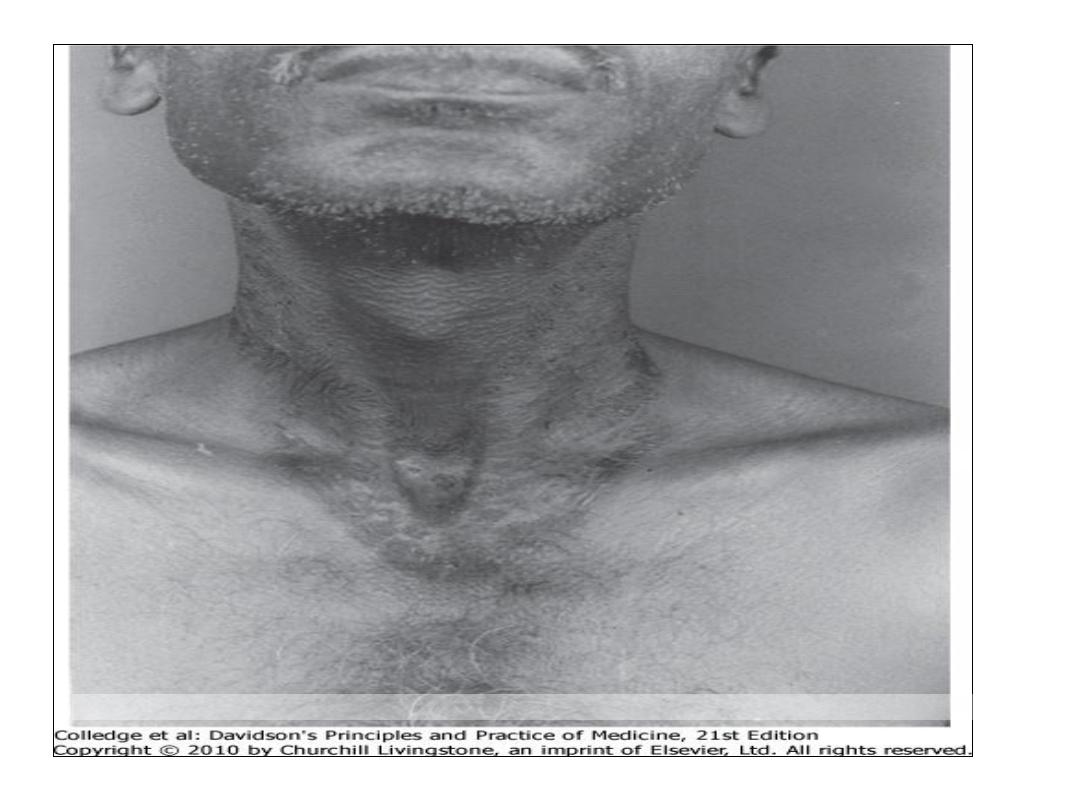
Clinical features
Pellagra :
dermatitis
,
diarrhoea
and
dementia
.
early non specific symptoms anorexia, weakness, irritability
bright red glossitis and angular stomatitis
1.
Dermatitis.
Scaling pigmented skin rash exposed to sunlight,
casal s necklace
1.
Diarrhea.
Due to proctitis. esophagitis and dysphagia(non
infective inflammation)
3.
Dementia
. This occurs in chronic disease. In milder cases
there are symptoms of depression.
Hallucinations and acute psychosis are seen
with more severe cases.
Downloaded from: StudentConsult (on 29 October 2011 12:19 AM)
© 2005 Elsevier

Niacin (B3)
Diagnosis
this is based on the clinical features with assesing the urinary
excretion of the 2 pyridone and 2 methyl nicotinamide.
Treatment
Nicotinamide (approximately 300 mg daily by mouth) with a
maintenance dose of 50 mg daily.
Response rapid(24h)
NB. vitB3 used in RX of hyperlipidemia

Vitamin B6
•
Vitamin B6 exists as pyridoxine, pyridoxal and
pyridoxamine.
•
cofactor of many enzymes involved in the metabolism of
many amino acids.
•
neurotransmitters synthesis
•
heme synthesis.
•
Vitamine metabolism as niacin
Source:
is found widely in plant and animal foodstuffs.

Vitamin B6
Cause of deficiency:
1.
Dietary deficiency
is extremely rare.
2.
Some drugs
(e.g. isoniazid,
hydralazine,methyldopa,
penicillamine) interact
with pyridoxal phosphate,
producing B6
deficiency.

Vitamin B6
Clincal features
: mucsal changes
1.
The peripheral neuropathy occurring after isoniazid
usually responds to vitamin B6. personality changes
,depression, confusion.
2.
Microcytic hypochromic anaemia occasionally responds
to vitamin B6 .
Treatment:
a daily dose of 100 mg should not be exceeded.
NB. vitB6 used as antiemetic especially in the pregnancy

Vitamin B12
The main function of B12 is the methylation of homocysteine to
methionine with the demethylation of methyl THF
polyglutamate to THF.
Source:
• humans are ultimately dependent on animal sources. It is
found in meat, fish, eggs and milk, but not in plants.
• The average adult stores some 2-3 mg, mainly in the liver, and
it may take 2 years or more after absorptive failure before B12
deficiency develops.

Deficiency:
1.
Low dietary intake
, Vegans
2.
Impaired absorption
:
• Stomach : Pernicious anaemia ,Gastrectomy ,Congenital
deficiency of intrinsic factor
• Small bowel: Ileal disease or resection ,Bacterial overgrowth
Fish tapeworm (Diphyllobothrium latum)
3.
Abnormal utilization
:Congenital transcobalamin II
deficiency
Clinical features
1. Anaemia of megaloblastic type
2. A red sore tongue (glossitis) and angular stomatitis are
sometimes present.
3. The neurological changes,
a.
polyneuropathy progressively
involving the peripheral
nerves
b. the posterior and eventually the lateral columns of the
spinal cord
(subacute combined degeneration
)
symmetrical paraesthesiae in the fingers and toes,
early loss of vibration sense and proprioception, and ataxia
progressive weakness and Paraplegia may result.
c.
Dementia, psychiatric problems
, e.g. depression,
hallucinations, delusions, and optic atrophy also
occur.

Investigations
1.
Haematological findings show the features of a megaloblastic
anaemia
2. Bone marrow shows the typical features of megaloblastic
erythropoiesis
( .
3. Serum bilirubin may be raised as a result of ineffective
erythropoiesis.
4. Serum vitamin B12 is usually well below 160 ng/L, which is
the lower end of the normal range.
Treatment
Hydroxocobalamin 1000 μg can be given intramuscularly.
improvement of the polyneuropathy may occur over 6-12
months,
but long-standing spinal cord damage is irreversible.

Folates
• are present in food as in the reduced dihydrofolate or
tetrahydrofolate (THF).
• act with vit B12 as coenzymes in the transfer of single carbon
units in amino acid metabolism and DNA synthesis.
Source:
• Dietary intake Folate is found in green vegetables
• Cooking causes a loss of 60-90% of the folate .
Causes of folate deficiency
1.
Nutritional
major cause
Poor intake
• Old age
• Poor social conditions
• Starvation
• anorexia
Gastrointestinal disease,
• partial gastrectomy
• small bowel disease , coeliac disease, Crohn's disease
Antifolate drugs
• Anticonvulsants :
– phenytoin
• Methotrexate
2.
Excess utilization
Physiological
• Pregnancy
• Lactation
Pathological
• Haematological disease with excess red cell production, e.g.
haemolysis
• Malignant disease with increased cell turnover
• Inflammatory disease
• Haemodialysis or peritoneal dialysis (loss with the fluid)

Clinical features
• asymptomatic
• symptoms of anaemia or of the underlying cause.
• Glossitis can occur.
• CNS manifestations does not occur .
Investigations
The haematological findings are those of a megaloblastic
anaemia .
low levels of serum folate (4-18 μg/L).
Treatment of folate deficiency
• giving 5 mg of folic acid daily for about 4 months to replace
body stores.
• Any underlying cause, e.g. coeliac disease, should be treated .
• Prophylactic folic acid is recommended for all women
planning a pregnancy. ( neuronal tube defect)
• Prophylactic folic acid is also given in chronic haematological
disorders where there is rapid cell turnover.

Vitamin C Ascorbic acid
• It is involved in the
hydroxylation
of proline to hydroxyproline,
which is necessary for the formation of
collagen
.
Source:
• Vitamin C is present in all fresh fruit and vegetables.
Deficiency:
1. is seen mainly in the
elderly
and single people who do
not eat vegetables.
2. Increase need in the trauma, burn infection
3. drugs as steroid, indomethacin, aspirin, tetracycline

Vitamin C Ascorbic acid
Clinical features :
scurvy
• Per follicular hemorrhages
• Swollen, spongy gums with bleeding and
superadded infection
• Spontaneous hemorrhage(git, joint,
peritoneum)
• Failure of wound healing
Downloaded from: StudentConsult (on 29 October 2011 12:19 AM)
© 2005 Elsevier

Diagnosis
• Plasma ascorbic acid is very low in obvious deficiency and a
vitamin C level of less than 11 μmol/L indicates vitamin C
deficiency.
Treatment
Initially the patient is given 200 mg of ascorbic acid daily and
encouraged to eat fresh fruit and vegetables.
NB
.
Vitc in large amount used in upper respiratory tract
infection
Vitamin A(retinol)
• Metabolites
: are retinaldehyde and retinoic
acid
• Function:
retinaldehyde
is important of vision
retinoic acid
for the cell growth and
differentiation
retinoids
synthetic molecule
also plays a role in
iron utilization
humeral immunity
T cell–mediated immunity
natural killer cell activity
phagocytosis
Vitamin A(retinol)
Metabolism:
• The
liver
contains 90% of the vitamin A is bound to retinol-
binding protein
transthyretin
trimolecular
complex
specific cell-surface receptors
bound to a series of cellular retinol-binding proteins, function
as transporting agents as well as co-
ligands
for enzymatic
reactions.
• Retinoic acid
is a ligand for certain nuclear receptors that act
as transcription factors.( retinoid-mediated gene
transcription)

Vitamin A(retinol)
• Retinoids
receptors for cell proliferation and
differentiation
used
in : promyelocytic leukemia
cystic acne
• Dietary source:
animal source
: liver and fish(excellent source)
plant source
: dark-green vegetable and fruits

Vitamin A(retinol)
Deficiency:
1.
chronic dietary deficit
(developing countries) In
Southern Asia, Sub-Saharan Africa, some areas of Latin America
inadequate intakes of animal food sources seasonal unavailability of
vegetables, colored fruits.
More than
125 million
preschool-age children with vitamin A deficiency,
~
4 million
have an ocular manifestation of deficiency .
At least a
quarter
of a million children each year developed blindness.

Vitamin A(retinol)
2. Malabsorption:
(developed countries)
celiac disease, short bowel syndrome
3. Zinc deficiency:
interfere with vitA mobilization from the liver
4. Alcohol :
interfere with conversion of retinol to retinaldehyde
in the retina (dehydrogenase)
5. Drugs :
interfere with the absorption of vitA
neomycin, cholestyramine

Vitamin A(retinol)
Clinical features
• Milder stages of
night blindness
(loss of dark adaptatio)
• conjunctival xerosis
(dryness)
(xerophalmia)
• Bitot's spots
(white patches of keratinized epithelium
appearing on the sclera)
• Keratomalacia
(softening of the cornea) leads corneal
ulceration and necrosis result in corneal scarring that
blinds.
• increased risk of mortality from diarrhea, dysentery,
measles, malaria, and respiratory disease.

Downloaded from: StudentConsult (on 29 October 2011 12:19 AM)
© 2005 Elsevier

Vitamin A(retinol)
Diagnosis:
1. Serum retinol level
2. Test of dark adaptation
3. Impression cytology of the conjunctiva
4. Store assessment by liver BX

Vitamin A(retinol)
Treatment:
30mg IM
or 60mg orally then
60mg
of vitA after 6 months
15mg
orally for 1 month in patient with malabsorp.
Vitamin A supplementation can markedly reduce risk of child
mortality (23–34%) where deficiency is widely prevalent.
NB.
Used in patient with M3 leukemia and cystic acne

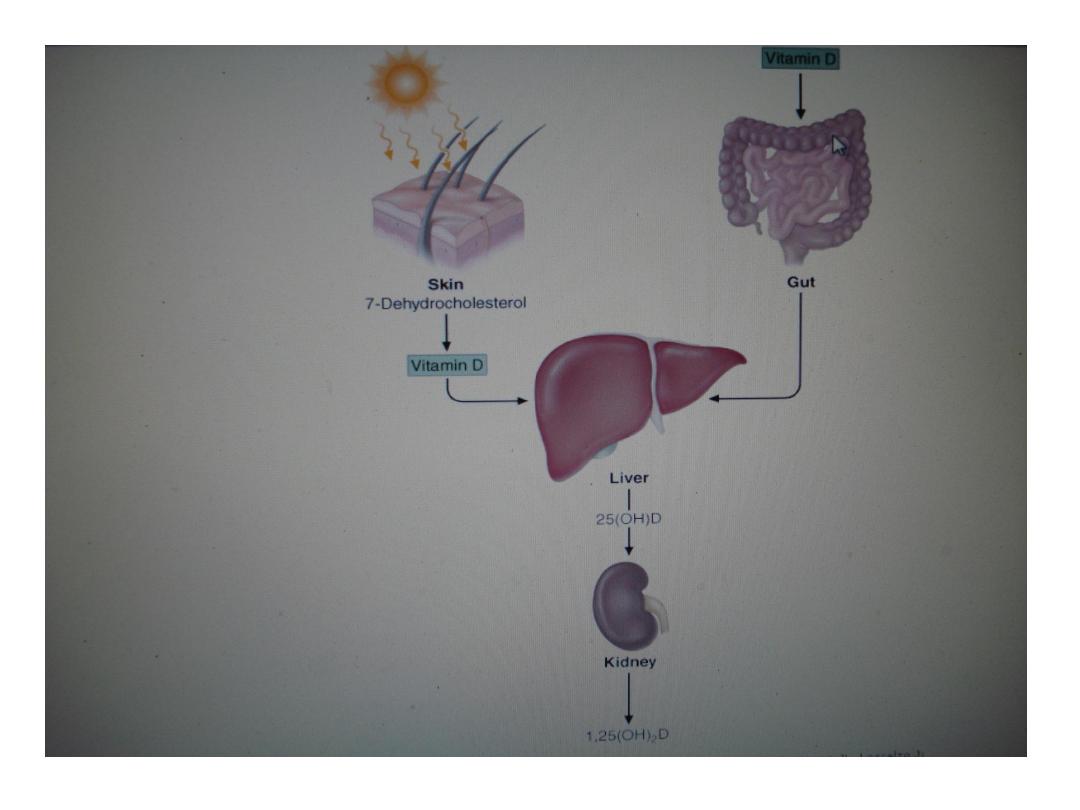
Vitamin D
Synthesis and Metabolism:
• steroid
hormone
involved in mineral ion homeostasis regulation,
can be synthesized endogenously In response to ultraviolet
radiation of the skin, a photochemical cleavage from 7-
dehydrocholesterol.
• In the United States and Canada
animal sources
(vitD3) dairy products, fish oils, egg
yolks.
plant sources
(vitamin D
2
)
cereals
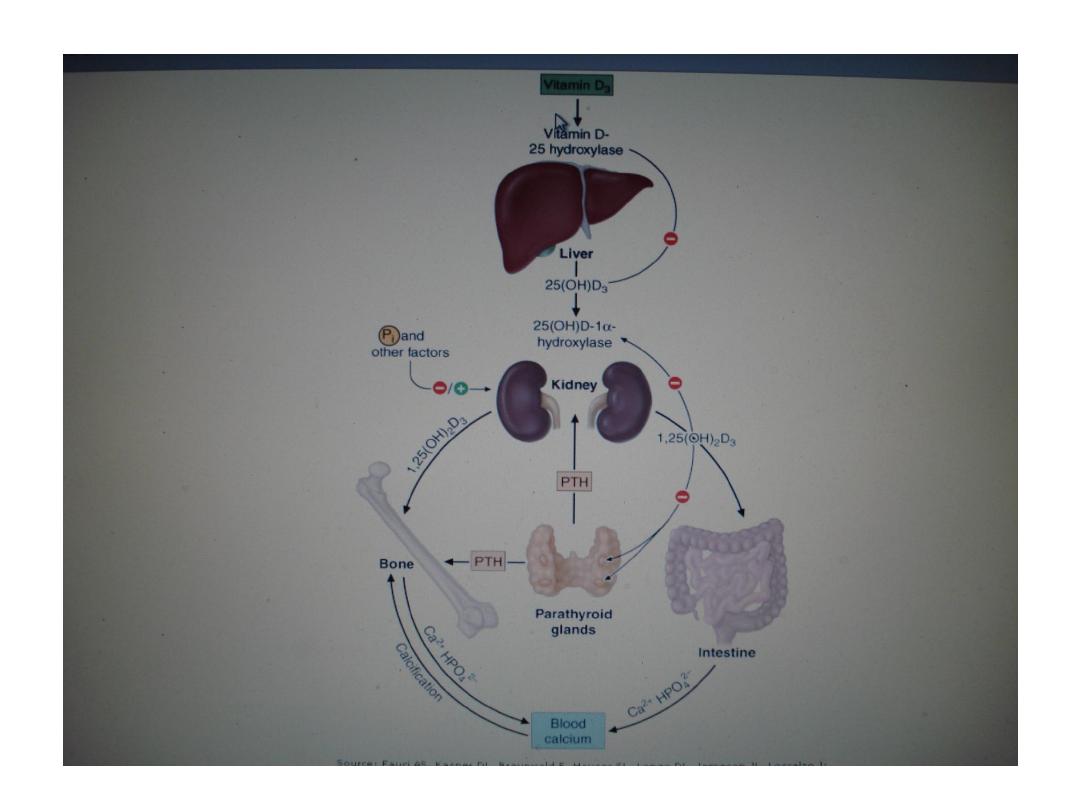

Vitamin D
Causes of the deficiency :
Vitamin D deficiency
Impaired cutaneous production
Dietary absence
Malabsorption
Accelerated loss of vitamin D
Increased metabolism (barbiturates, phenytoin,
rifampin)
Impaired enterohepatic circulation

Causes of decrease action
Impaired 25-hydroxylation
Liver disease
Isoniazid
Impaired 1-hydroxylation
Hypoparathyroidism
Renal failure
Ketoconazole
1-hydroxylase mutation
X-linked hypophosphatemic rickets
Target organ resistance
Vitamin D receptor mutation
Phenytoin

Vitamin D
Clinical features:
1. Mild to moderate deficiency is
asymptomatic
2.
Osteomalacia
(defective bone mineralization)
Muscle and bone pain
Malaise
Fragility fracture( pseudofractures)
Proximal myopathy ( wadling gait, diff. climbing stairs)
Bone tenderness
3.
Rickets
( growth retardation, bone deformities)

Vitamin D
Diagnosis:
1. Biochemical tests
decrease serum 25(OH)D (< 37 nmol/L)
low or normal s. Ca. , ph.
increasing PTH levels
increase alkaline phosphatase
2. Radiological tests
of oteomalacia
decrease in cortical thickness
osteopenia of the skeleton
pseudofractures, or Looser's zones in the ribs and pelvis
and long bones and vertebra
3. Bone biopsy
Vitamin D
Treatment:
(
50,000 IU
weekly for 3–12 weeks), followed by maintenance
therapy (800 IU daily). Calcium supplementation should
include 1.5–2.0 g/d of elemental calcium
Daily intake of
(400 IU)
is often insufficient to prevent
deficiency.
800 IU of vitamin D
, with calcium supplementation,
decreases the risk of hip fractures in elderly women. .

Vitamin E ( tocopherols)
Function:
• acts as
antioxidant
and radical
scavenger
, which protects
low-density lipoproteins (LDLs) and polyunsaturated fats
in membranes from oxidation.
Absorption and Metabolism:
• After absorption, vitamin E is taken up from
chylomicrons
by the liver, and a hepatic tocopherol transport protein
mediates intracellular vitamin E transport and
incorporation into very low-density lipoprotein
(VLDL)
.

Vitamin E ( tocopherol)
Dietary source:
• The RDA for vitamin E is 15 mg/d
• widely distributed in the food supply
high
in sunflower oil, soybean and corn oils.
meats, nuts, and cereal grains
small amounts
in fruits and vegetables.
• Vitamin E pills
containing doses of 50–1000 mg are
ingested by a large fraction of the U.S. population.

Vitamin E ( tocopherol)
Causes of the deficiency:
1.
Dietary deficiency
of vitamin E does not exist.
2. severe and prolonged
malabsorptive diseases
.
celiac disease, small-intestinal resection.
3. prolonged
cholestasis
may develop vitamin E
4. Children with
abetalipoproteinemia
cannot absorb or
transport vitamin E.
5. A
familial form
of isolated vitamin E deficiency (defect
in the tocopherol transport protein).

Vitamin E ( tocopherols)
Clinical features:
axonal degeneration of the large myelinated axons and results
in
posterior column
and
spinocerebellar
symptoms.
Peripheral neuropathy
ataxic gait (Decreased vibration and position Sensations)
Ophthalmoplegia
skeletal myopathy
pigmented retinopathy
Diagnosis
: of low blood levels of tocopherol

Vitamin E ( tocopherols)
Treatment
:
• 800–1200
mg of tocopherol per day.
• Vitamin E
has been suggested to increase sexual
performance, and to slow the aging process, but evidence
for these properties
is lacking
.
• High doses (60–800 mg/d)
of vitamin E have been shown
in controlled trials to improve parameters of immune
function and to reduce colds in nursing home residents.
• but intervention studies using vitamin E to prevent
cardiovascular disease or cancer have
not
shown efficacy.
Vitamin k
Function:
• vitamin K
1
,
phylloquinone, from vegetable and animal
sources
• vitamin K
2
, menaquinone, which is synthesized by
bacterial flora and found in hepatic tissue.
• required for the
carboxylation
of glutamic acid, which is
necessary for calcium binding to -carboxylated proteins
such as prothrombin (factor II); factors VII, IX, and X;
protein C; protein S).
• Warfarin
preventing the conversion of vitamin K to its
active hydroquinone form.

Vitamin k
Dietary Sources:
•
green leafy vegetables
(spinach)
also present in margarine and liver.
vegetable oils rich :olive, soybean oils.
• The average daily intake by Americans is estimated to be
approximately
100 Mg/d
.

Vitamin k
Causes of the deficiency
:
1. chronic
small-intestinal disease
(e.g., celiac disease,
Crohn's disease).
2.
cholestatic
liver disease.
3. Broad-spectrum
antibiotic
treatment.
3.
drug
therapy, the antiobesity drug orlistat
Vitamin k
The diagnosis:
• elevated
prothrombin time
or reduced clotting factors,
• vitamin K may also be measured directly.
Treatment:
• Vitamin K deficiency is treated using a parenteral dose of
10
mg.
• For patients with chronic malabsorption,
1–2 mg/d
of vitamin K should
be given orally, or
1–2 mg/week
can be taken parenterally .
