[2012]
DRUGS FOR HEART
FAILURE
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
3
CHF usually occurs when the cardiac output is inadequate to meet the
metabolic needs of the body.
In CHF, the ventricular dysfunction may be primarily systolic (i.e.
inadequate force generation to eject blood normally as in ischemicc heart
disease) or it is may be diastolic (inadequate relaxation to permit normal filling
as a result of hypertrophy or stiffness of the myocardium).
CHF due to sytolic dysfunction usually respond to inotropic drug e.g.
digoxin while CHF due to diastolic dysfunction does not respond optimaly to
these drugs.
Rarely high output failure occurs whereby needs of the body are so great
inspite of the C.O. this form of failure poorly responds to +ve inotropic drugs.
Treatment is by correcting the underlying cause.
the primary symptoms of all types of CHF include: tachycardia, decreased
exrecise tolerance, SOB, peripheral and pulmonary edema, cardiomegaly.
The decreased execise tolerance and easy fatigability are due to C.O. while
other manifestations are due to compensatory mechnisms.
Physiology Of Cardiac Muscle Contraction:
Contraction of the cardiac muscle is due to movement of actin and myosin
in cardiac sarcomers during systole resulting from the interaction of Ca
+
with
actin troponin tropomyosin system.
This activator Ca
+
comes from 2 sources:
1. From outside the cell, enter during plateau phase of action potential
through voltage gated Ca
+
channels.
2. Release of Ca
+
from the sarcoplasmic reticulum which depend on the
amount stored in the SR and the amount of trigger Ca
+
that enter the cell.
Therefore the contraction of cardiac muscle is directly related to the
concentration of the free cystolic Ca
+
.
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
4
Removal of Ca
+
: Na-Ca exchanger: which exchange Ca with Na thus any
change in the intracellular concentration of Na will affect the cellular levels of
Ca
+
.
1. Uptake by SR, more than 99% of Ca
+
is stored in the SR and mitochondria.
Pathophysiology of Cardiac Performance:
It's a function of 4 primary factors:
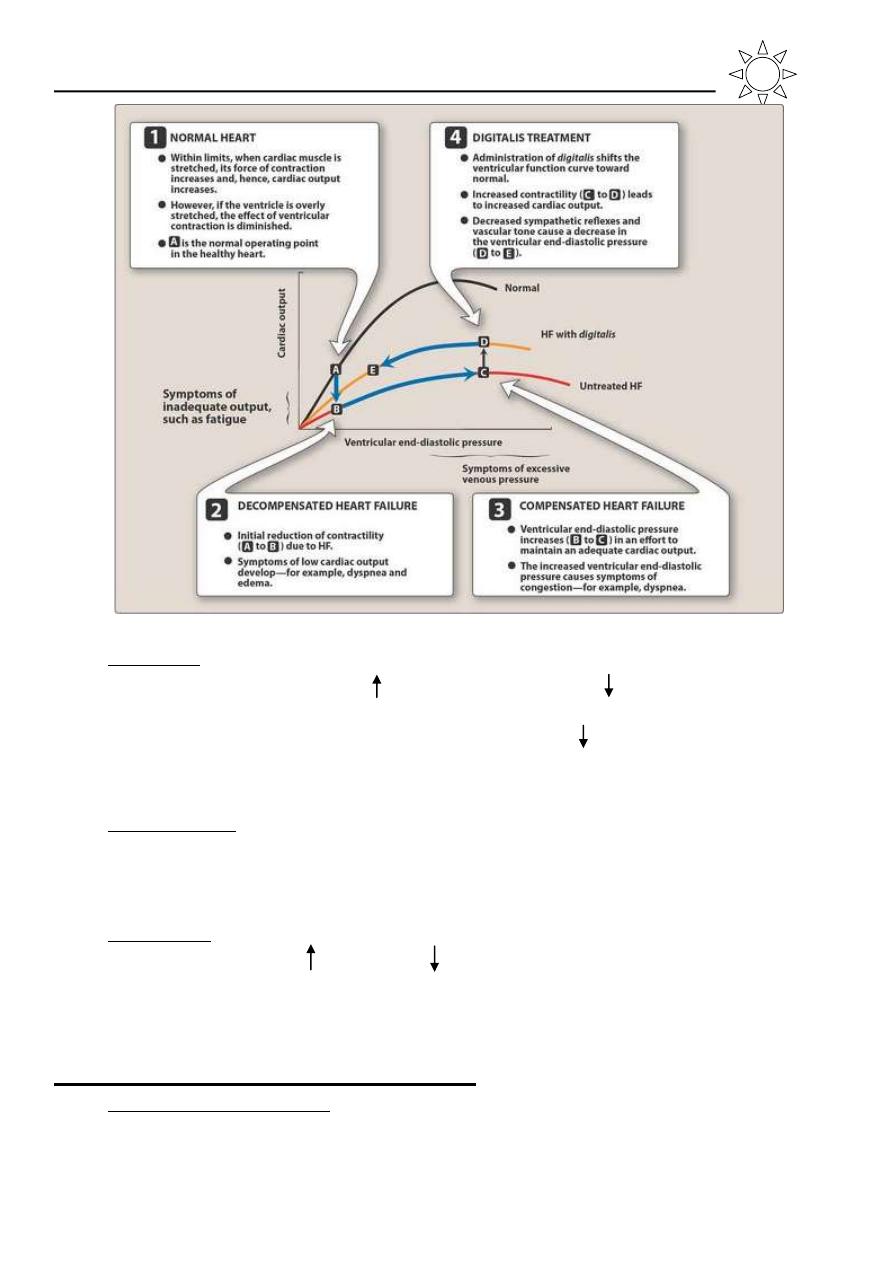
1. Preload: is the volume of the blood that fills the ventricles in diastole, when
it is , it causes overfilling of the heart which the work load.
Starling law: within limits, the ventricular performance is related to the
degree of myocardial stretching.
When left ventricular performance (e.g. stroke volume or C.O.) is
plotted as a function of L.V. filling pressure (preload), then the resulting
curve is called L.V. function curve… therefore when preload is leads to
in ventricular stretching and will enhance the ventricular function.
The limit is End Diastolic Pressure (EDP) of 15 mmHg when there is
plateau of performance.
On the other hand marked stretching causes marked deterioration of
ventricular function and EDP of 20 mmHg or more results in pulmonary
congestion.
In HF, preload usually because of in blood volume and venous tone.
Reduction of preload is the goal of salt restriction and diuretic therapy.
Vasodilators also reduce preload by redistributing the blood into
peripheral veins away from the heart.
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
5
2. Afterload: is the systemic vascular resistance against the heart must pump
the blood, this is frequently in CHF which leads to C.O.
This sets the stage for the use of the drugs that or reduce arterial tone in
CHF.
3. Contractility: in patients with chronic low output failure, there is reduction
in the intrinsic contractility of myocardium resulting in reduction of pump
performance; here comes the role of +ve inotropic drug.
4. Heart rate: which is the major determinant of C.O. (i.e., C.O. = S.V. x Ht.
rate). The heart rate as the S.V. , this is the 1
st
compensatory mechanism
to maintain the C.O.
Compensatory Mechanisms in CHF:
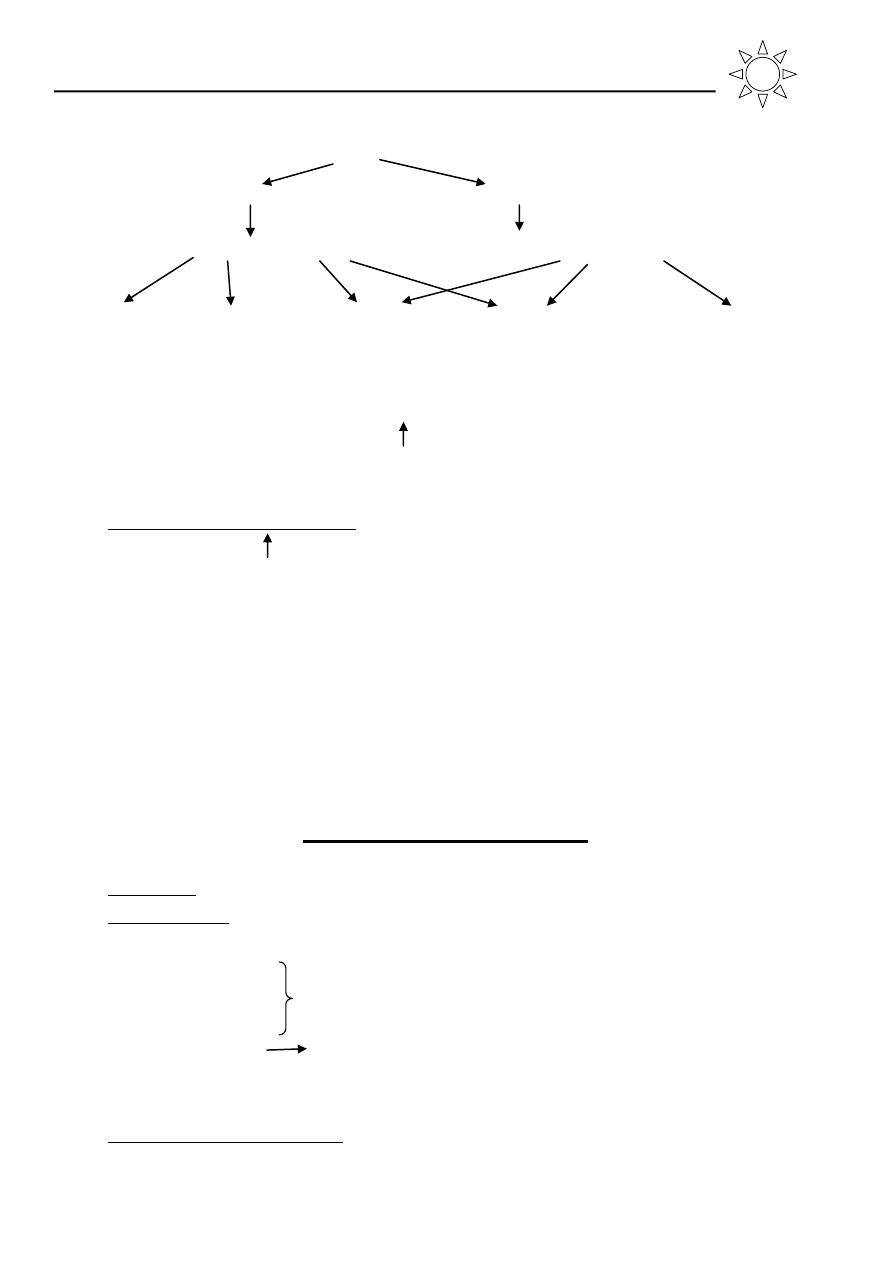
1. Neuro-hormonal reflex involves:
a. The sympathetic nervous system
b. The renin-angiotensin-aldosterone system
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
6
↓C.O.
↓Carotid sinus firing ↓Renal blood flow
↑Sympathetic discharge ↑renin ↑angiotensin II and ↑aldosterone
Force Rate Preload Afterload Remodeling*
*remodeling: change the shape (geometry) of the ventricles
These compensatory mechanisms the work of the heart and can further
contribute to the decline in the cardiac function.
2. Myocardial hypertrophy: is the most important intrinsic compensatory
mechanism, the in myocardial mass helps to maintain cardiac performance
in the phase of pressure or volume overload. However, after initial
beneficial effect, hypertrophy can lead to ischemic changes, impairment of
diastolic filling and alteration in ventricular geometry (remodeling) due to
proliferation of abnormal myocardial cells and C.T. which die at the
accelerated rate leaving the remaining myocardial cells subject to even
greater overload.
Drugs used to treat CHF
1. Diuretics: loop diuretics and thiazides AND SPIRONOLACTONE.
2. Vasodilators:
a. ACE inhibitors (arteries and veins and angiotensin receptor blockers
b. Hydralazine
c. Minoxidil
Arteries
d. Isosorbide
mainly veins
e.
Brain natriuretic peptide(BNP) Nesiritide
f.
Endothelin antagonists Bosentan ,tezosentan
3. Cardiac inotropic agents
a. Cardiac glycosides (digoxin, digitoxin)
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
7
b. β-adrenergic agonist (dobutamine, dopamine)
c. Phospho diesterase inhibitors (amrinone, milrinone)
4. Beta-blockers: most patients with chronic stable heart failure respond
favorably to certain β-blockers (carvedilol, metoprolol) inspite of the fact
that these drugs can ppt. acute decompensation of cardiac function.
Remodeling: the term applied to dilation (other than that due to passive
stretch) and slow structural changes that occur in the stressed myocardium.
Considering (c) in cardiac inotropic agents, they cAMP by inhibiting
phosphodiesterase iso enzyme III which in turn Ca
+
entry during the A.P.,
they also have significant vasodilatory effect, they are used for acute heart
failure, their toxicity prevents long term use which includes B.M. toxicity,
liver toxicity and also cardiac arrhythmia.
Cardiac Glycosides:
All the commonly used cardiac glycosides of which digoxin is considered
as the prototype, combine a steroid nucleus with unsaturated 5 mem. lactone ring
and a series of sugars linked to the C3 of the nucleus. For the effect on the heart,
we need the steroid nucleus and the lactone ring. The sugar series differ from
each other and affect the pharmacokinetics of the drug.
Source: fox glove digitalis lanata and D.purpurea, squill (med. sea onion),
strophanthus gratus and other tropical and temperate zone plants, Certain toads
have cardiac glycosides in their skin glands.
D.purpurea D.lanata S.gratus
Digoxin Digoxin Ouabain
Digitoxin Lanatocide Strophanthline
Deslanoside
The most important property of cardiac glycoside is their +ve inotropic
effect (i.e. increase the force of myocardial contraction and C.O. at a
reduced metabolic cost).
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
8
Pharmacological Effect on Heart Contractility:
Mechanical effects: in the force of contraction by in both the velocity of
myocardial contraction and the max. force that is developed.
in cardiac contractility leads to the following:
1. in C.O. to resemble that of normal heart.
2. EDP or volume thus the efficacy of contraction and therefore ejection
fraction is increased.
3. The resulting improvement in the circulation will lead to sympathetic
activity and peripheral resistance.
4. in heart rate because of these effects by in vagal tone.
5. Improvement in renal blood flow
6. O
2
demand will be ultimately .
Note: there is renal blood flow because of improved circulation.
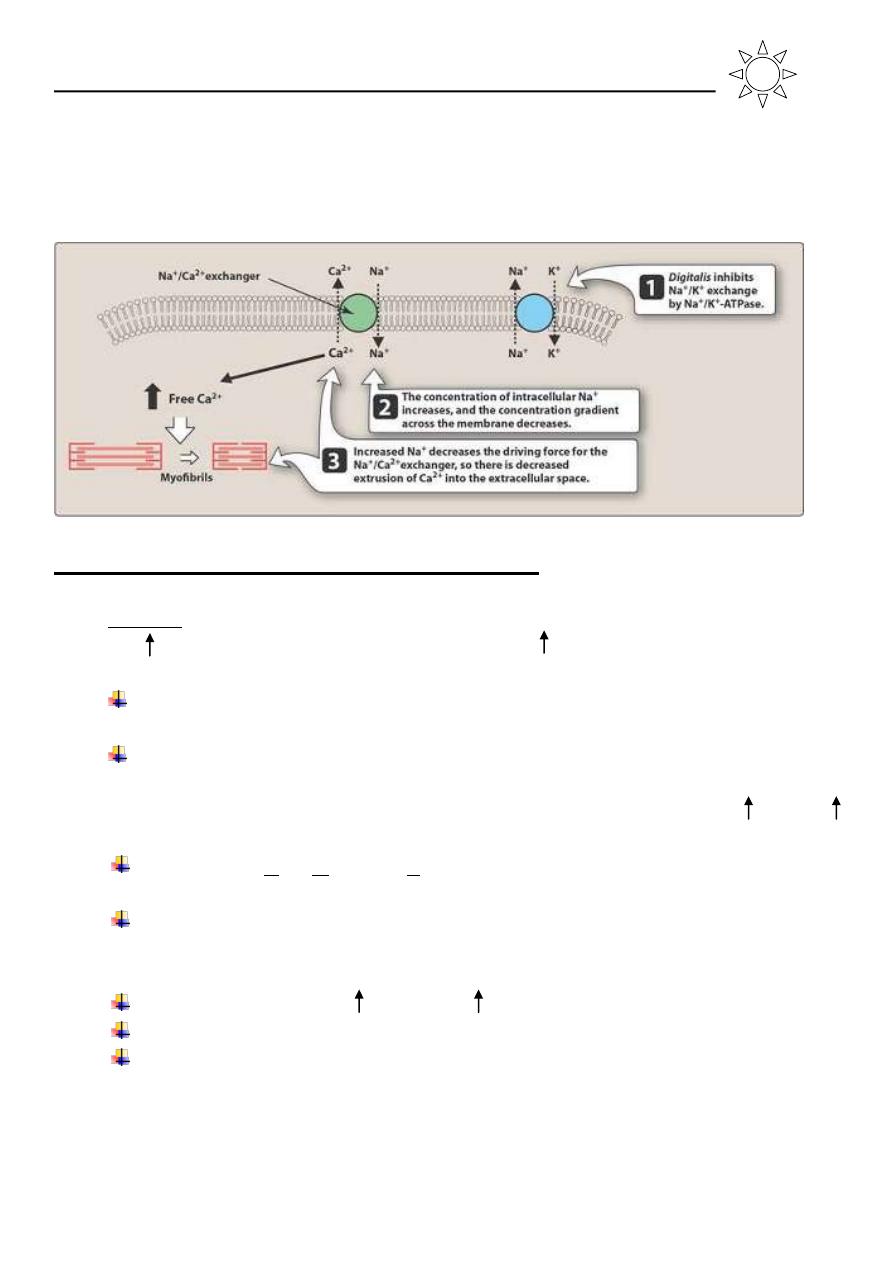
Mechanism of Action:
Cardiac glycosides combine reversibly with the Na
+
-K
+
ATPase of the
cardiac cell memb., resulting in inhibition of pump activity and this causes in
Na
+
conc. inside the cell which favors the transport of Ca
+
into cell via Na
+
-Ca
+
exchanger and thus intracellular Ca
+
resulting in an in the systolic force of
contraction.
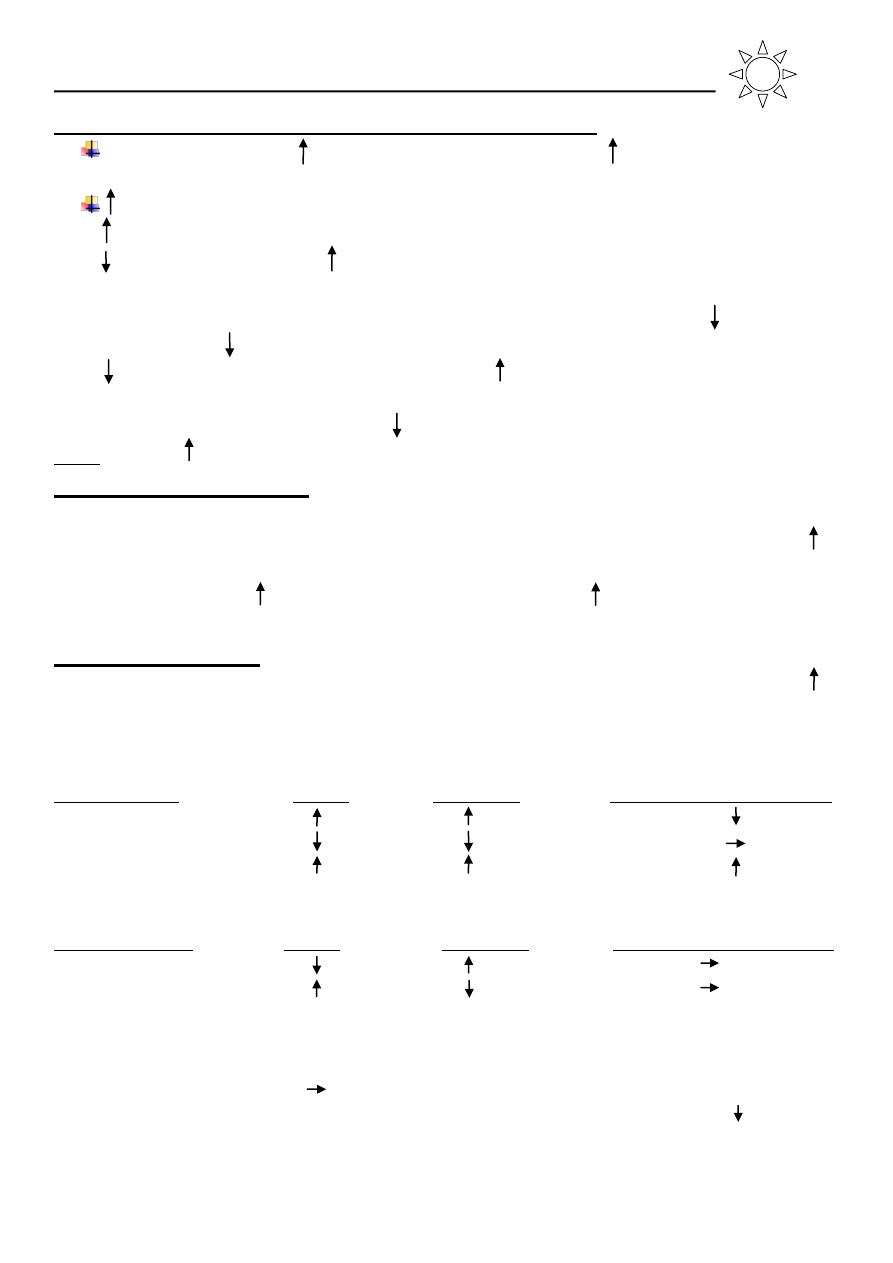
Electrical Effects:
In the intact subject it is a mixture of direct and indirect actions (due to in
the vagal tone). In the lower portion of the dose range parasymp. effects
dominate (mainly on the atria). As the dose increases , more of the symp. effects
come into play:
Direct Effect Atrial AV node
Vent. And purkinjie fibers
ERP
Conduction velocity
Automaticity
Indirect Effect Atrial AV node
Vent. And purkinjie fibers
ERP
Conduction velocity
Adverse effects extra systole AV block PVC and Bigmeny
Arrhythmia Tachycardia AV nodal VT and VF
tachycardia
ECG changes PR interval is ↑ T and ST is depressed
QT
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
9
ERP: effective refractive period PVC: premature ventricular count
VT: ventricular Tachycardia Bigmeny: one normal and one ectopic beat
VF= ventricular fibrillation
Therapeutic Uses:
1. Cardiac failure by the direct action on contractility, they are of great value
in the treatment of severe left ventricular systolic failure after initiation of
diuretics and ACE inhibitors, only if the patient has AF well it becomes 1
st
choice.
2. Atrial fibrillation: by the vagal effect on the AV node reducing conduction
velocity, thus it is slowing the ventricular rate (i.e. digoxin does not revert
the atrial fibrillation to the normal sinus rhythm).
3. Atrial flutter: by the vagal action on the AV node to reduce the rate and
also by shortening the refractory period of the atrial muscle to convert
flutter to fibrillation in which the ventricular rate is more readily controlled.
4. Paroxysmal Atrial Tachycardia (PAT) by the vagal effect frequently
respond to digoxin, adenosine, and Ca
+
channels blockers are the best now.
Contraindications:
Cardiac temponade, constrictive pericarditis, high output CHF,
Hypertrophic Obstructive Cardiac Myopathy (HOCM), wolf-parkinson- white
syndrome.
Kinetics:
Because digitalis is frequently prescribed on long term therapy and because
of the low margin of safety of the drug (lethal dose is only 5-10 times the
minimum effective dose).
The drugs also have a long t
1/2
, so they require a careful attention to their
pharmacokinetics.
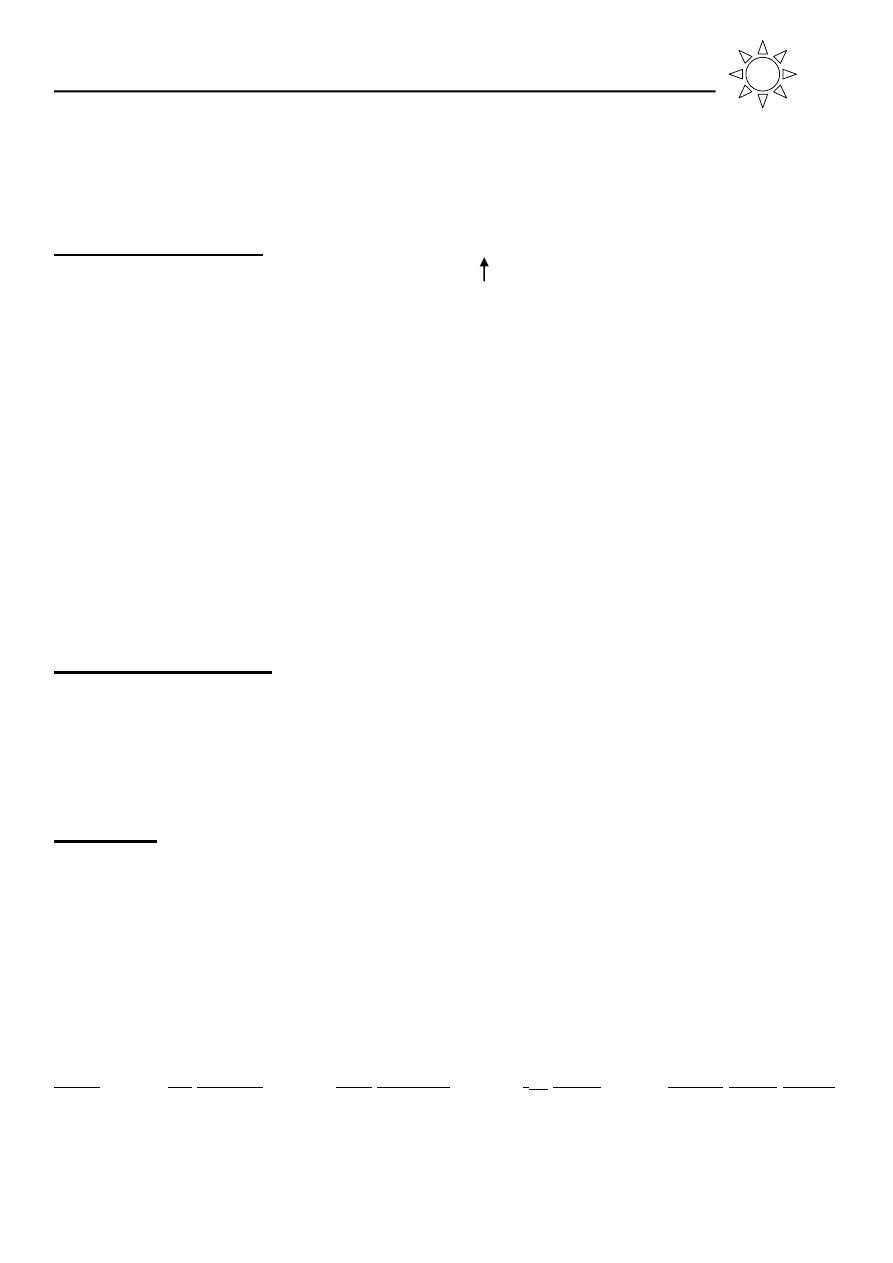
Drug GI absorb. Ptn. Binding t
1/2
PMR serum conc. ng/ml
Digoxin ≈ 75% <30% 36 hr./kidney 0.5-2.5 / toxic>2
Digitoxin 90-100% 97% 5-7 days/liver 10-35 / toxic>35
*PMR: principle metabolic route
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
1
0
Administration and Dosage:
You should not exceed the safety therapeutic range, the slow approach of
digitalization is the safest method.
If a more rapid effect is needed, then you can give a loading dose divided
into 3-4 doses over 24 hours then followed by maintenance dose.
Slow digitalization or maintenance doses of digoxin is 0.125-0.5 mg while
loading dose is 0.5-0.75 mg every 8 hrs (3 daily) then followed by
maintenance dose.
Digoxin can be used I.V. but it's dangerous.
Factors predisposing to digoxin toxicity:
1. Electrolyte disturbance:
a. Hypokalemia: may be produced by diuretics, steroids, vomiting and
diarrhea.
It can precipitate serious arrhythmia and this can be prevented by supplying
K
+
or the use of K
+
sparing diuretics.
b. Hypercalcemia and hypomagnesemia: also predispose to digoxin
toxicity.
2. Drugs: quinidine and verapamil by displacement digoxin from binding site.
quinidine also competes with digoxin for renal excretion, other drugs may
digoxin concentration and potential for toxicity include: Amiodarone,
tetracycline, erythromycin, and other drugs that cause hypokalemia.
3. Hypothyroidism, hypoxia, renal failure, myocarditis are also predisposing
factors for dig. toxicity.
Adverse Effects:
When the serum concentration is above therapeutic range then signs of
digoxin toxicity will appear and these are:
1. Anorexia earliest sign.
2. Nausea, vomiting, diarrhea (nausea and vomiting due to stimulation of
CTZ).
3. Headache, malaise, fatigue, neuralgia, confusion, agitation, and even
convulsions.
4. Vision change: include change in color perception, yellow vision
xanthopsia, hollows on dark objects.
5. Gynecomastia (rare) because it contains steroid nucleus
6. Cardiac toxicity
Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
1
1
a. PVC: premature ventricular contraction: bigeminy, VT, VF.
b. AV dissociation and block complete heart block.
c. PAT and non-paroxysmal often with AV block.
d. SA block and sinus arrhythmia.
e. Digoxin can virtually cause every variety of arrhythmia.
Delayed after depolarization are responsible for most types of dig.
arrhythmias.(occurring during phase 4 due to entry of calcium)
Principles of Rx of digitalis toxicity:
1. Cardiac glycosides and K
+
depleting drugs are discontinued.
2. KCl is administered orally or by slow I.V. infusion if hypokalemia is
present (unless there is AV block), Mg
+
deficiency may accompany
hypokalemia and Mg
+
replacement may be necessary.
3. Cholestyramine binds to cardiac glycoside and has been used to fasten their
elimination.
4. A digoxin specific Ab fragment (FAB) from immunized sheep is non-
immunogenic and it is available for Rx of life threatening toxicity.
5. Rx of digoxin induced cardiac arrhythmias
a. Atropine to control sinus bradycardia.
b. Lidocaine (the best) for VT also procainamide can be used.
c. Propranolol can be used for ventricular and supra ventricular
tachycardia unless there is AV block.
d. Phenytoin can be given for ventricular and atrial arrhythmia.
e. Electrical conversion is often hazardous in the treatment of digoxin
induced arrhythmia because it can ppt. VF. Only used when there is
VF.
Acute heart failure treatment in short:
1. Oxygen supply and rest.
2. Morphine.
3. Diuretics mainly fursemide (I.V.).
4. Nitrates.
5. Β-agonist Dobutamine may be used.
6. Digoxin but risk of arrhythmia due to hypoxia.
7. Sometimes the patient may have an element of bronchospasm and we may
give aminophylline.

Pharmacology / Dr. Samer
Lec. 40
College of Medicine Baghdad University
1
2
