1
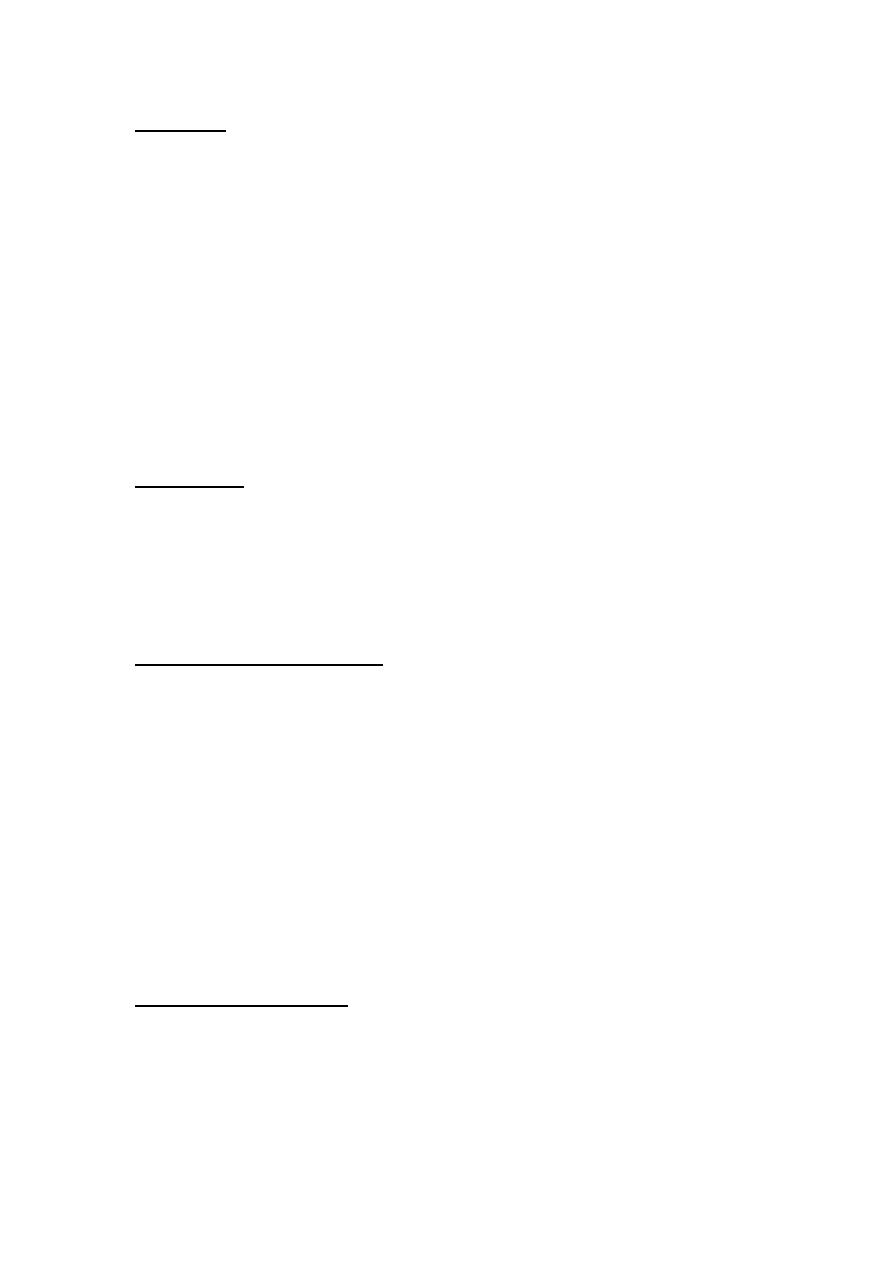
Anxiolytic & hypnotic drugs
Lec:3
Dr. Mohammed Rashad
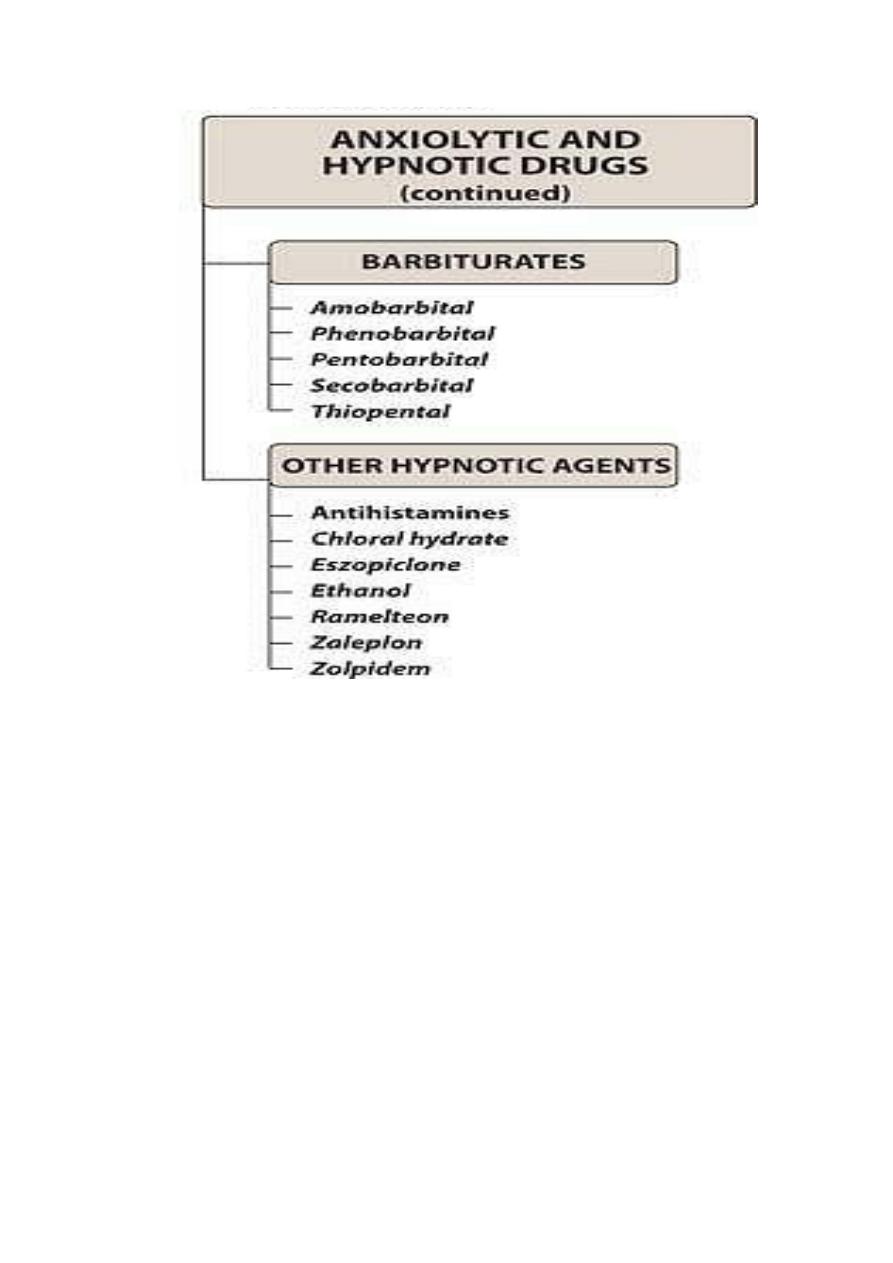
Benzodiazepines (BDZ) :
- long acting (1-3 days) , clorazepate ,chlor diazepoxide , diazepam ,
flurazepam, quazepam .
- intermediate acting (10-20 hs ) , alprazolam , lorazepam , estazolam ,
temazepam .
- short acting (3-8 hs ), medazolam , oxazepam , triazolam .
* ( benzodiazepine antagonist flumazenil ) .
* other anxiolytic drugs ( hydroxyzine , antidepressents ) .
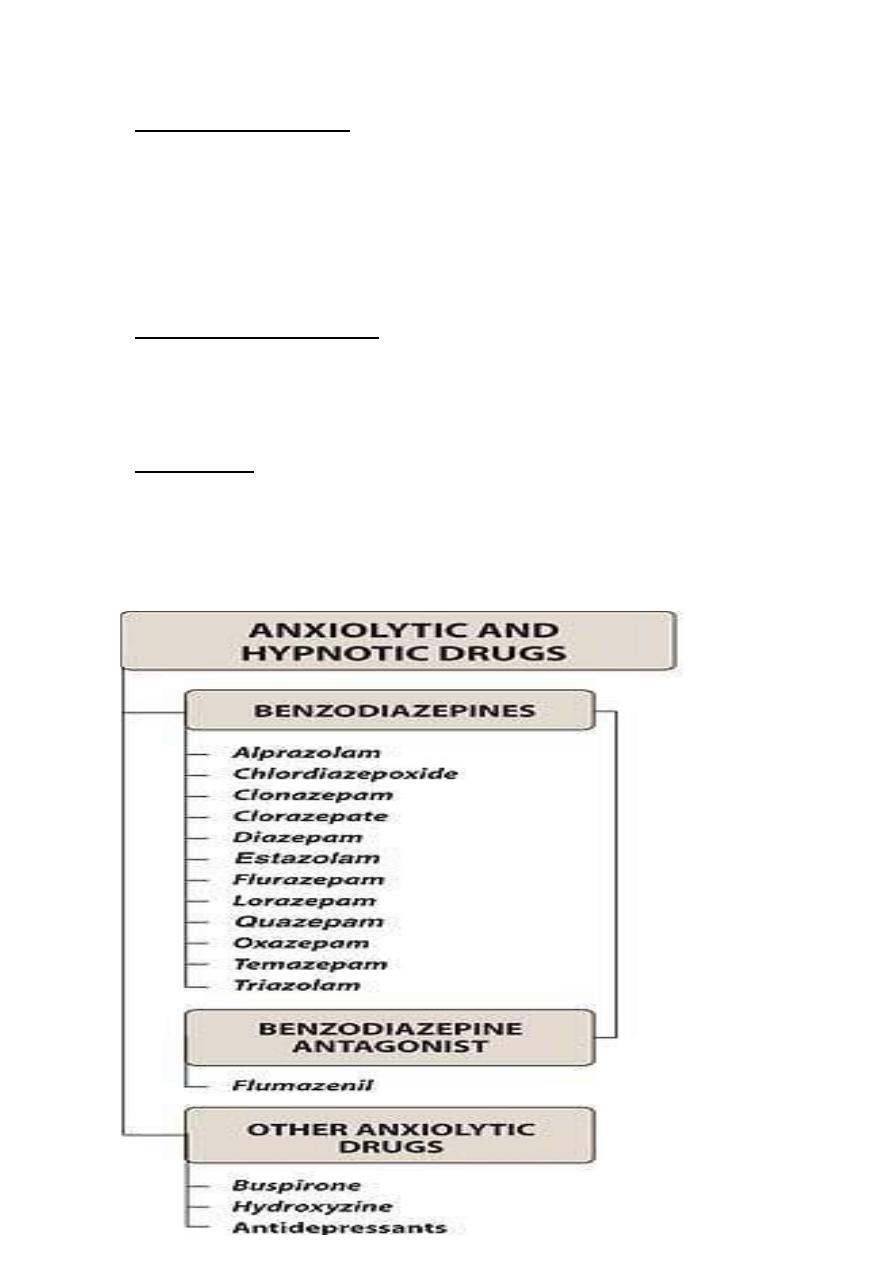
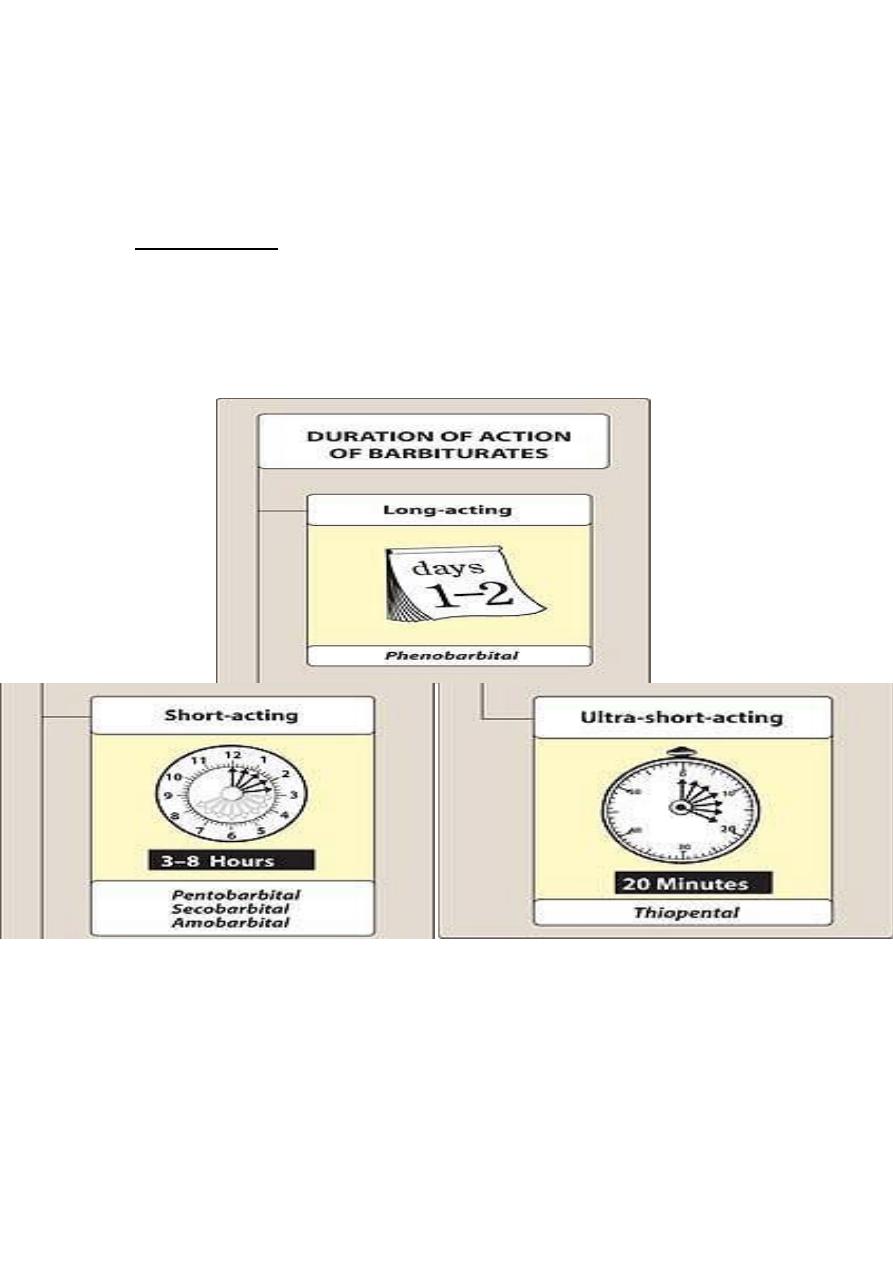
Barbiturates :
long acting (1-2 days) : Phenobarbital . -
-short acting (3-8 hs): pentobarbital , amobarbital , secobarbital .
- ultra-short acting (20 minutes ) : thiopental .
* other hypnotic agents :
-zolpidem , zaleplon , ramelteon , eszopiclone .
-chloral hydrate .
-alcohol .
-antihistamines .
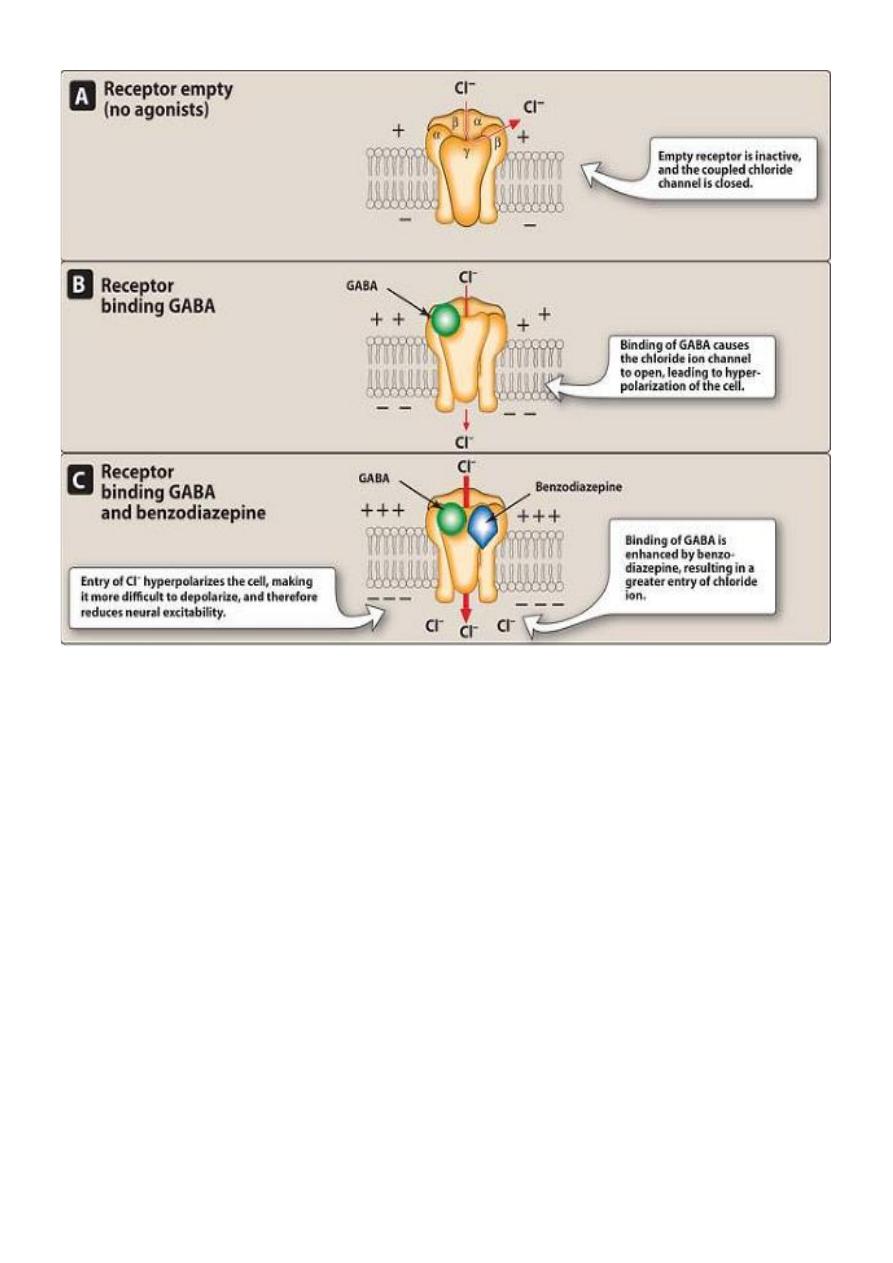
Mechanism of action of BDZs :
-
Empty receptor is inactive , & the coupled chloride channel
-
Is closed.
2
-
Binding of GABA causes cl ion channel to open
→hyperpolarization of the cell.
-
Binding of GABA is enhanced by BDZs →greater entry of cl ion.
-
Entry of cl ion hyperpolarizes the cell, making it more difficult to
be depolarized & therefore reduce neuronal excitability.
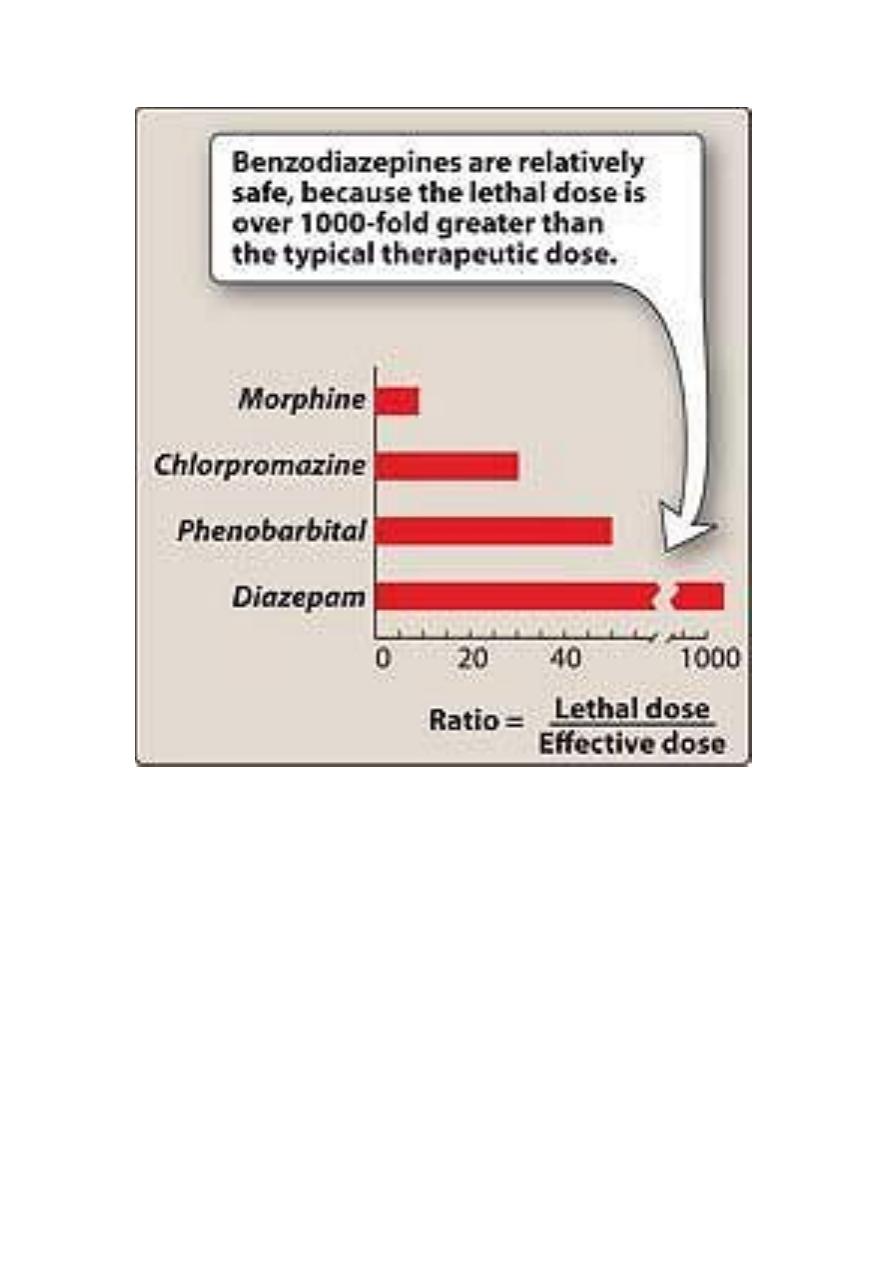
Ratio of safety = lethal dose ∕effective dose
BDZ : 1000 relatively safe , chlorpromazine 50 , morphine 10 .
Pharmacological actions of BDZs :
1- Reduction of anxiety: the BDZS are anxiolytics. at low doses they
inhibit neuronal circuit in limbic system .
2- Sedative and hypnotic actions : all BDZs have some sedative
properties and some of them have hypnotic properties (at high doses).
3- Anterograde amnesia: temporary impairment of memory (Alpha 1 &
GABAa receptors).
4- Anticonvulsant: for status epilepticus & seizure disorders (Alpha 1 &
GABAa receptors).
5- Muscle relaxant: at high dose
- Relax spasticity of skeletal muscle by ↑presynaptic inhibition in spinal
cord (alpha 1 & GABAa receptors).
- Baclofen (muscle relaxant affect GABAb).
Therapeutic uses of BDZ :
1- Anxiety disorders : For all types of anxiety, and not to alleviate the
normal stress of life.
- For severe anxiety and only for short periods.
3
- The long acting agents preferred in anxiety that require long period of
treatment.
- Alprazolam is effective for short and long period of treatment, for panic
disorders (30% withdrawal).
2- Muscular disorders:
- Sk. Muscle spasms (as in muscle strain).
- Spasticity from degenerative disorders (m.s. & cerebral palsy).
3- Seizures :
- Clonazepam for treatment of epilepsy (p.m.)
- Diazepam & lorazepam (drug of choice) for status epilepticus and
grandmal epilepsy.
- Chlorazepam , diazepam and oxazepam for treatment of alcohol
withdrawal
- And ↓ risk of withdrawal related seizures.
4- Sleep disorders :
- All BDZs are sedatives (calming effect) and some are hypnotic agents.
- BDZs (drug of choice) for insomnia:
• ↓latency time to falling asleep.
• ↓awakening during night.
• ↑total sleeping time.
5- Amnesia:
Short acting agents for premedication & unpleasant procedures (dental ,
endoscopic, bronchoscopic and angioplasty → amnesia , conscious
sedation & anxiety ↓).
- Midazolam (injectable only) for induction of anesthesia.
4
A-Flurazepam ( long acting BDZ):
Pharmacological action.
-↓sleep induction time.
-↓no. of awakenings.
-↑duration of sleep.
* causes little rebound insomnia.
* maintains its effectiveness 4 weeks .
Kinetics:
The t1∕2 of flurazepam and its metabolites is 85 hs →day time sedation
& accumulation.
(residual sedation = hangover ) .
B- Temazepam ( intermediate acting BDZ ) :
- For patients (with) frequent wakening.
- Peak sedative effect 1-3 hs after oral administration, therefore, it
should be given 1-2 hs before bed time.
C-Triazolam ( short acting BDZ ) :
- It is used to induce sleep (difficulty in going) .
- Tolerance occurs within few days → withdrawal→ rebound insomnia.
NOTE: Hypnotics either intermittently or for 2-4 weeks .
Pharmacokinetics:
• The BDZs are lipophilic → rapidly & completely - absorbed &
distributed throughout the body.

5
The longer acting agents form active metabolites with long T1∕2 , so
clinical durations of action do not always correlate with actual T1∕2 , this
may be due to receptor dissociation rates in CNS and subcutaneous
redistribution elsewhere.
- All BDZs cross the placental barriers & appear in breast milk. → ±
depress the CNS of newborn & infant.
- Most BDZs →hepatic metabolism →to active compounds .
-urine excretion as glucuronoids or oxidized metabolites
Dependence:
- Psychological and physical dependence of BDZs occur with high dose
over a prolonged periods.
- Abrupt discontinuation → withdrawal symptoms
- ( confusion , anxiety , agitation , restlessness , tension , insomnia , &
rarely seizure ) .
- short acting BDZs →more abrupt & severe withdrawal reaction more
than long acting BDZs ( in which withdrawal symptoms may occur slowly
& last no. of days after discontinuation of therapy .
Adverse effects:
- Drowsiness and confusion ( most common side effects )
- Ataxia ( at high dose & precludes activities that require fine motor
coordination such as driving .
- cognitive impairment ( ↓long-term recall & acquisition of new
knowledge .
6
Triazolam:
$ most potent oral BDZs .
$ most rapid elimination .
S ∕ E : rapid development of tolerance .
- Early morning insomnia .
- Daytime anxiety .
- Amnesia confusion snd drawsiness .
Precautions:
- Liver disease.
- Acute narrow-angle glucoma .
- Alcohol & other CNS depressants ±→ lethal drug over dose .
Benzodiazepine Antagonist :
Flumazenil = GABA receptor antagonist.
-
only i.v. , rapid onset & short duration
(T1⁄ 2( 1 hs ) .
- Frequent dose may ppt. withdrawal in dependent patient or causes
seizures in patients on BDZs therapy for epilepsy.
- Most common side effects : nausea , vomiting & agitation .
Other anxiolytic agents :
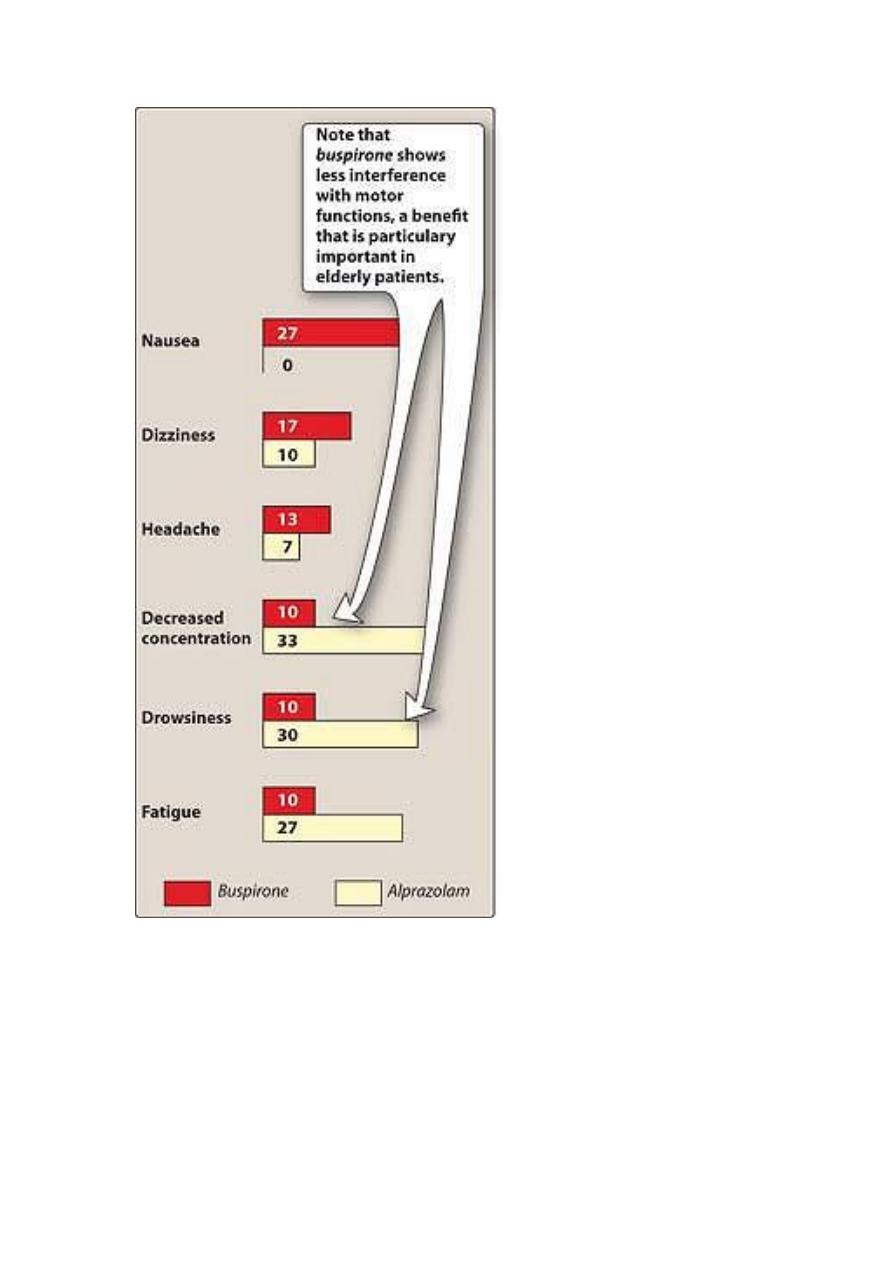
Buspirone ( NBDZs anxiolytics ) : has affinity to ( 5HT1A , 5HT2A ,D2 ) .
7
Therapeutic advantages:
1- Useful in long term therapy for GAD & chronic anxiety with symptoms
of irritability & hostility.
2- Does not potentiate the CNS depression of alcohol.
3- Low potential for addiction
Therapeutic disadvantages :
- Slow onset of action than BDZs.
- No muscle relaxation or anticonculsant activity.
Hydroxyzine :
- Highly sedative antihistamine with antiemetic activity.
- Useful for anxiety in patients with history of drug abuse.
- Useful for sedation prior to dental procedures or surgery.
8
9
11
11
12
13
Barbiturates:
Today they have been replaced by BDZs because they induce :
- Very severe withdrawal symptoms.
- Respiratory depression.
- Enzyme induction.
Mechanism of action:
- Barbs potentiate GABA action by prolonging the duration of cl ion
channels openings .
- Block excitatory glutamate receptors .
- Block sodium channels by anesthetic concentration . All these
molecular actions decrease neuronal activity .
Pharmacological actions :
1- depression of CNS :
Sedation hypnosis anesthesia coma& death
+ ++ +++ ++++
Thus the degree of depression of CNS depends on the dose .
- they have no analgesic action & ± exacerbate pain .
- chronic use → tolerance .
2- respiratory depression : inhibition of hypoxic response to CO2 &
overdose →respiratory depression & death .
3- enzyme induction : chronic use →↓action of many drugs that utilize
p450 .
14
Therapeutic uses :
1-anesthesia : thiopental ( ultra-short acting ; i.v for induction of
anesthesia ) .
2- anticonvulsant :
- Phenobarbital for ( tonic clonic seizure , status epilepticus , eclapsia ) .
- Phenobarbital ( drug of choice ) for treatment of febrile seizure.
S\E: depress cognitive performance in children
3- anxiety:
- mild sedatives for ( anxiety , nervus tension , insomnia ) .
( replaced by bdzs )
Pharmacokinetics : oral→ absorption→ liver metabolization →wide
distribution → urine excretion .
( from brain →splanchnic area→ sk. muscle →finally to adipose tissue .
Adverse effects :
1- CNS: ( drowsiness , impaired concentration , mental & physical
sluggishness ) . This effect synergized with alcohol .
2- drug hangover : hypnotic dose .
- feeling of tiredness after waking .
- impaired ability to function normally .
- occasionally , nausea & dizziness .
3- physical dependence : abrupt withdrawal is more severe than opiates
.
- tremors , anxiety , weakness , restlessness , N&V seizures , delirium &
cardiac arrest→ death .
15
Precautions :
- barbs ( enzyme inducer) →↓ effect of drugs that are metabolized by
p450 hepatic enzyme .
- barbs increase porphyrins synthesis → C\I in patients with acute
intermittent porphyria .
Barbs poisoning : over dose → death from ;
( respiratory & central cardiovascular depression ) →shock .
- treatment : no specific antagonist .
- artificial respiration .
- GI evacuation .
-hemodialysis .
- alkalinization of urine .
Other hypnotic agents : ( non bdzs hypnotics ) :
- zaleplon .
- zolpidem : few residual effects .
Therapeutic advantages :
- show minimal withdrawal effects .
- exhibit minimal rebound insomnia .
- little or no tolerance occur with prolonged use .
Therapeutic disadvantages :
- have no anticonvulsant or muscle relaxing properties .
- adverse effects : nightmares , agitation , headache , GI upset , dizziness
, day time drowsiness ,)
16
Eszopiclone : effective for up to 6 months .
Ramelteon : selective agonist at MT1 , MT2 ( melatonine ) .
Light ++ retina → signal to SCN ( hypothalamus ) →signal to pineal gland
→inhibits melatonine release →dark → ++ melatonin→ sleep .
Therapeutic advantages :
1- the potential for abuse is minimal with minimal dependence or
withdrawal effects .
2- the drug can be administered long-term .
3- for patients with increased sleep latency .
Therapeutic disadvantages :
1- dizziness , somnolence & fatigue .
2- increased prolactin levels .
Chloral hydrate
( trichloroacetaldehyde )
- acetaldehyde CL3 →( liver ) ethanol CL3 .
- The onset of sleep induction is 30 minutes & the duration 6 hs .
- irritant to GIT → epigastric distress & unpleasant taste sensation .
-
it synthesized with ethanol .
Antihistamines : non prescription sedative antihistamines as doxylamine
are effective in mild insomnia .
S\E : anticholinergic side effects .
Ethanol ( ethyl alcohol ) : has anxiolytic & sedative effects but its toxic
potential outweigh its benefits .
17
- alcoholism is a serious medical & social problem , CNS depressant
→sedation →hypnosis ( if large dose ) .
- thus a shallow dose – response curve
( wide dose range → sedation ) .
- oral absorption & total body H2O is volume of distribution ; liver
metabolism ; kidneys & lung execretion .
- it produce severe CNS depression with bdzs , antihistamines , barbs .
- chronic consumption : 1- severe liver disease . 2- gastritis . 3-
cardiomyopathy . 4- nutritional deficiency .
Treatment of alcohol withdrawal :-
1- bdzs ( treatment of choice ) .
2- carbamazepine : for convulsion episodes during withdrawal .
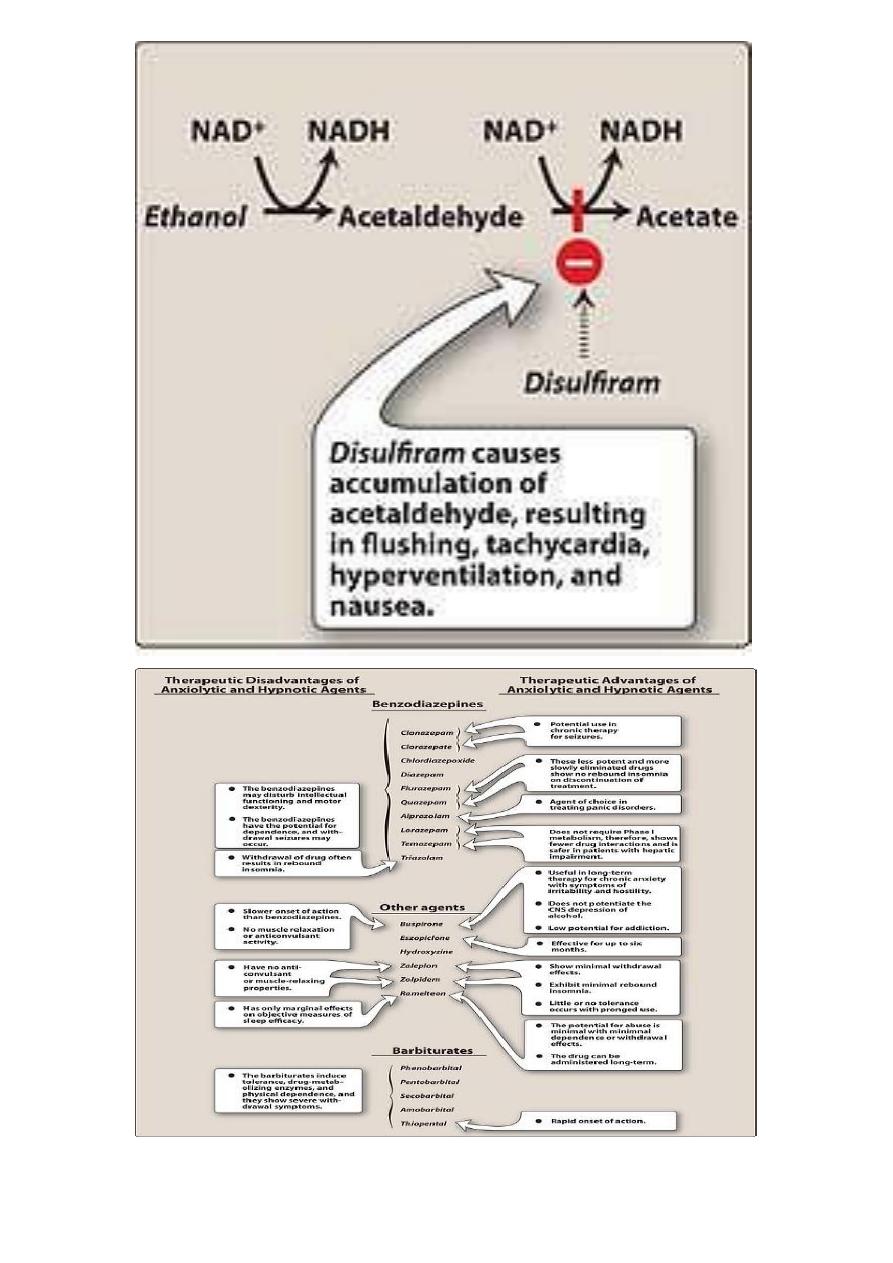
1- disulfiram :
Ethanol → ( by alcohol dehydrogenase )→ acetaldehyde →
( by aldehyde dehydrogenase ) → Acetate .
-(disulfiram ) inhibits aldehyde dehydrogenase → accumulatiom of
acetaldehyde in blood → flushing , hypoventilation , tachycardia &
nausea .
- some use in patient serioudly desiring to stop alcohol ingestion .
- the patient abstains from alcohol to prevent unpleasant effect of
disufiram .
- induced acetaldehyde accumulation
2-Naltrexone :
long acting opiate antagonist ( oral ,injectable)
18
- FDA approved for alcohol dependence conjunction with supportive
psychotherapy
( better tolerated than disulfiram ) .
3- Acamprosate:
yet poorly understood mechanism .
- it is utilized in alcohol dependence treatment programs in conjunction
with supportive psychotherapy .

19
21
