Parkinsonism
Dr.Nasser A. H. Al-Harchan
Dr.Nasser A. H. Al-Harchan
Asst. Prof. of Pharmacology
College of Medicine
Baghdad University

introduction
Parkinson’s
Parkinson’s disease
disease (PD)
(PD)
is a degenerative, progressive neurologic
disorder characterized by lesions of the basal ganglia that
produce abnormalities in motor activities.
Clinical
Clinical syndrome
syndrome
l
Tremor at rest
l
Rigidity
l
Ataxia
l
Bradykinesia
l
Disorder of consciousness,recognization,remembrance,and
show dementia.

Etiology
• reduction in the activity of inhibitory dopaminergic neurons in the
substantia nigra and corpus striatum parts of the brain's basal ganglia
system that are involved in motor control. This results in a decrease in
dopamine in these nerve tracts.
Causes:
1- Genetic factors do not play a dominant role.
2- Environmental factor
3- Secondary parkinsonism: viral encephalitis or multiple small vascular
lesions.
4. Drugs such as the phenothiazines and haloperidol, that block
dopamine receptors in the brain' may also produce parkinsonian
symptoms.
5- Iatrogenic parkinsonism
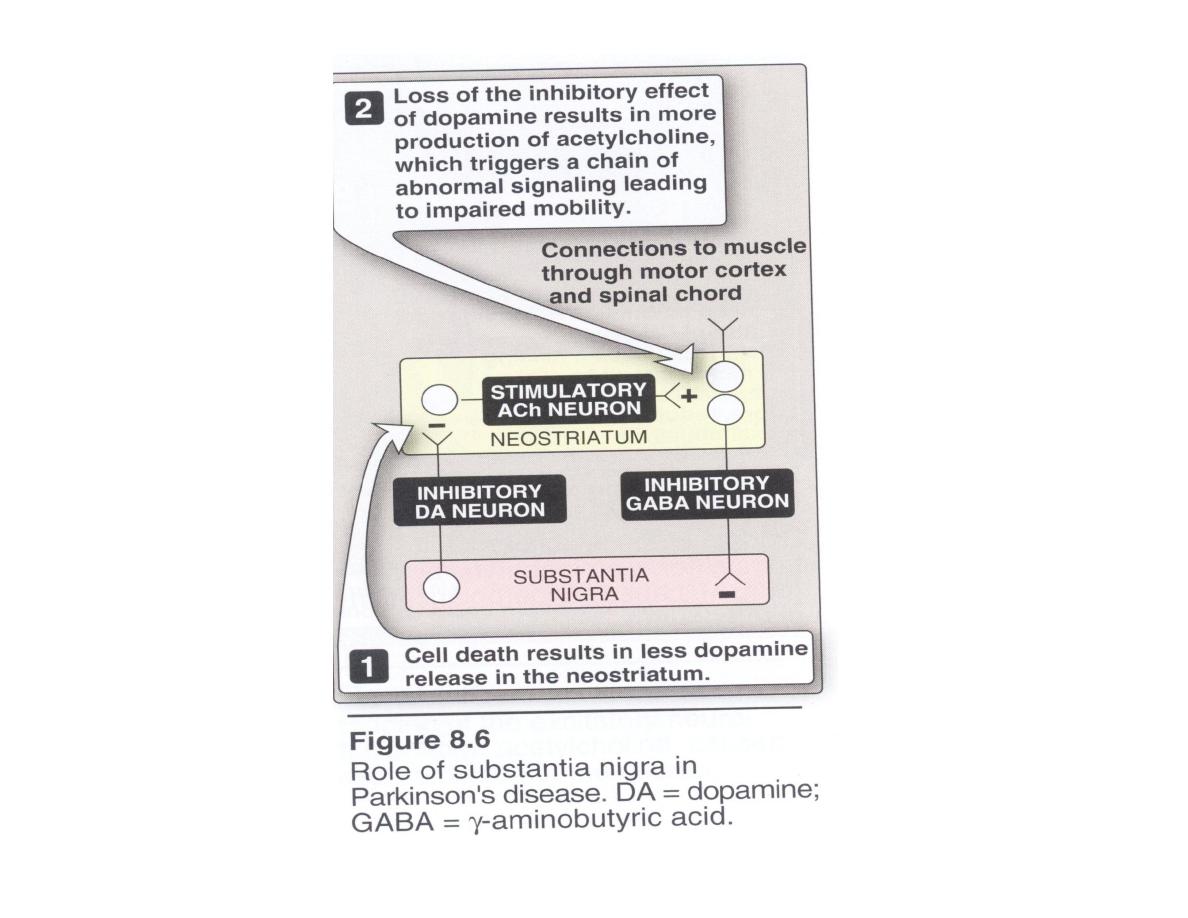
Substantia nigra:
is the source of dopaminergic neurons that terminate in the
striatum that fire tonically.
Neostriatum:
• the neostriatum is connected to the sustantia nigra by neurons that secrete the
inhibitory transmitter GABA at their termini in the substantia nigra.
• cells of the substantia nigra send neurons back to the neostriatum, secreting the
inhibitory transmitter dopamine at their termini.
• This mutual inhibitory pathway normally maintains a degree of inhibition of the
two separate areas.
• In Parkinson disease, destruction of cells in the substantia nigra results in the
degeneration of neuron responsible for secreting dopamine in the neostriatum.
• Thus, the normal modulating inhibitory influence of dopamine on cholinergic
neurons in the neostriatum is significantly diminished, resulting in
overproduction of acetylcholine. This triggers a chain of abnormal signaling,
resulting in loss of the control of muscle movements.

Strategies in Treatment
• The symptoms of parkinsonism due to :
• an imbalance between the excitatory cholinergic
neurons and the greatly diminished number of
inhibitory dopaminergic neurons.
• Therapy is aimed at:
• A- restoring dopamine in the basal ganglia.
• B- antagonizing the excitatory effect of
cholinergic neurons, thus reestablishing the
correct dopamine/acetylcholine balance.
Levodopa and carbidopa
Levodopa
is a metabolic precursor of dopamine.
• It restores dopamine levels in the extrapyramidal centers
(substantia nigra) that atrophy in parkinsonism.
• In patients with early disease, the number of residual
dopaminergic neurons in the substantia nigra is adequate for
conversion of
levodopa
to dopamine. Thus, the patient rarely
complains that the drug effects "wear off."
• With time, the number of neurons decreases, and fewer cells
are capable of taking up exogenously administered
levodopa
and
converting it to dopamine for subsequent storage and release.
Consequently, motor control fluctuation develops.
Mechanism of action
Levodopa:
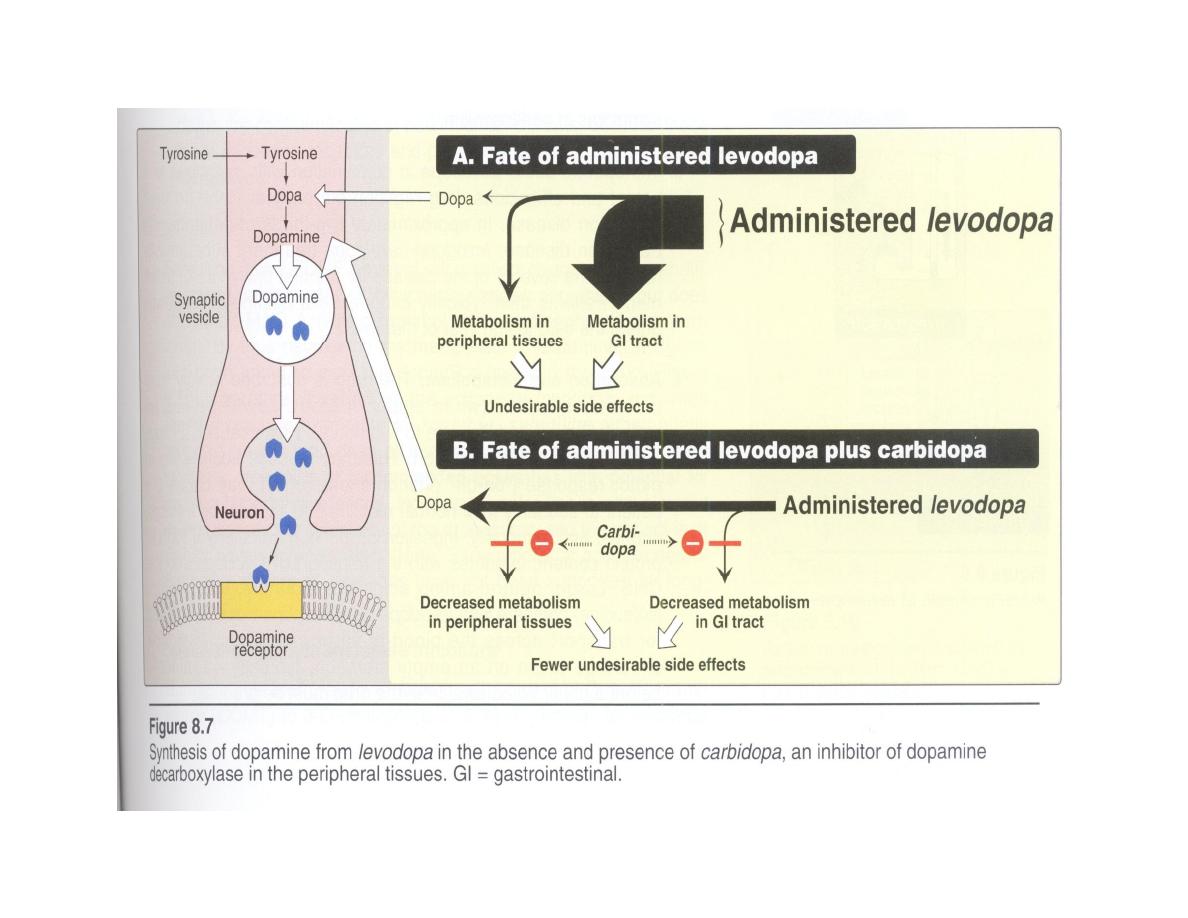
. Dopamine itself does not cross the blood-brain barrier, but its
immediate precursor,
levodopa, is
readily transported into the CNS and is
converted to dopamine in the brain.
• Large doses of
levodopa
are required, because much of the drug is
decarboxylated to dopamine in the periphery, resulting in side effects that
include nausea, vomiting, cardiac arrhythmias, and hypotension.
Carbidopa:
The effects of
levodopa
on the CNS can be greatly enhanced by
coadministering
carbidopa
, a dopa decarboxylase inhibitor that does not cross
the blood-brain barrier.
Carbidopa
diminishes the metabolism of
levodopa
in the gastrointestinal (GI)
tract and peripheral tissues; thus, it increases the availability of
levodopa
to the
CNS.
The addition of
carbidopa
1.lowers the dose of
levodopa
needed by four- to five-fold
2.decreases the severity of the side effects of peripherally formed dopamine
.

2. Actions:
Levodopa
decreases the rigidity, tremors, and other symptoms
of parkinsonism.
3. Therapeutic uses:
levodopa-carbidopa
treatment reduces the severity of the disease for the first
few years of treatment.
4. Absorption and metabolism:
v
The drug is absorbed rapidly from the small intestine (when empty of food).
v
Levodopa
has short half-life (one to two hours), which causes fluctuations in
plasma concentration. This may produce fluctuations in motor response ("on-
off" phenomenon).
v
Ingestion of meals with a high in protein content, interferes with the transport
of
levodopa
into the CNS.
v
Large, neutral amino acids (leucine and isoleucine) compete with
levodopa
for absorption from the gut and for transport across the blood-brain barrier.

.
Adverse effects:
Peripheral effects:
v
GIT: Anorexia, nausea, and vomiting occur because of stimulation of the
emetic center.
v
CVS: Tachycardia and ventricular extrasystoles result from dopaminergic
action on the heart. Hypotension may also develop.
v
Eye: Adrenergic action on the iris causes mydriasis,
v
Blood: blood dyscrasias and a positive reaction to the Coombs test.
v
Saliva and urine are a brownish color because of the melanin pigment
produced from catecholamine oxidation.
CNS effects:
vFlactuation in response (on-off phenomenon)
v
Visual and auditory hallucinations.
v
abnormal involuntary movements (dyskinesia) may occur. These CNS effects
are the opposite of parkinsonian symptoms and reflect the overactivity of
dopamine at receptors in the basal ganglia.
v
Levodopa
can also cause mood changes, depression, and anxiety
.
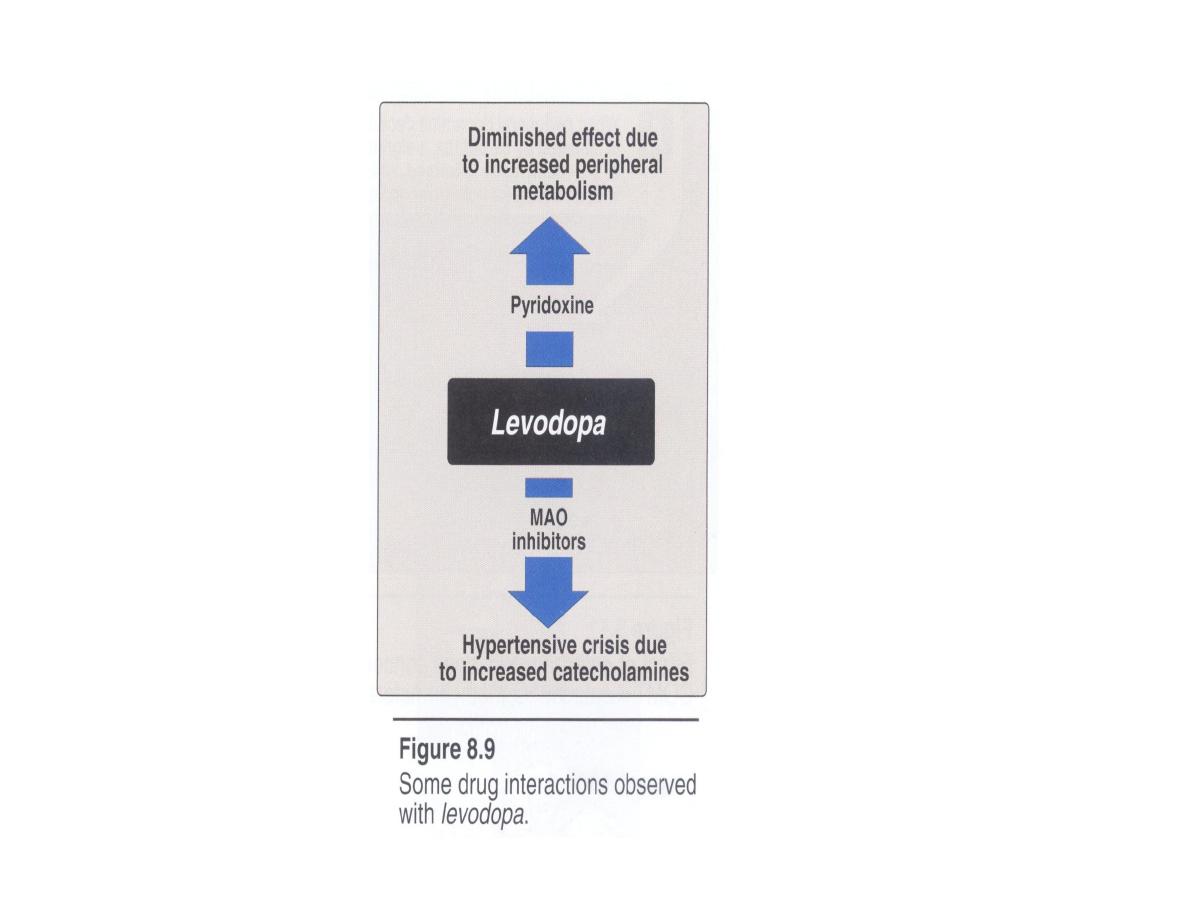

Interactions:
• The vitamin pyridoxine (B6) increases the peripheral breakdown of
levodopa
and diminishes its effectiveness.
• Concomitant administration of
levodopa
and monoamine oxidase (MAO)
inhibitors, such as
phenelzine,
can produce a hypertensive crisis.
• In many psychotic patients,
levodopa
exacerbates symptoms, possibly
through the buildup of central amines.
• In patients with glaucoma, the drug can cause an increase in intraocular
pressure.
• Cardiac patients should be carefully monitored because of the possible
development of cardiac arrhythmias.
• Antipsychotic drugs are contraindicated in parkinsonian patients, because
these block dopamine receptors and produce a parkinsonian syndrome
themselves.
Dopamine receptor agonists
1- Ergot derivatives,
bromocriptine
and
pergolide,
2- Non-ergot drugs,
ropinirole
and
pramipexole.
Advantages:
• Have durations of action longer than that of
levodopa
• Are effective in patients exhibiting fluctuations in their
response to
levodopa.
• less risk of dyskinesias and motor fluctuations when
compared to patients started with
levodopa
therapy.
Bromocriptine and pergolide
Bromocriptine
and
pergolide
both ergotamine (vasoconstrictor action)
derivatives, are dopamine receptor agonists.
•
Pergolide
is the more potent of the two.
• The dose is increased gradually during a period of two to three months.
Side effects: Hallucinations, confusion, delirium, nausea, and orthostatic
hypotension are more common than levodopa, whereas dyskinesia is less
prominent.
• In psychiatric illness, they may cause the mental condition to worsen.
• In patients with a history of myocardial infarction
cardiac problems may
develop.
• In patients with peripheral vascular disease, a worsening of the vasospasm
occurs, and
• In patients with peptic ulcer, there is a worsening of the ulcer.
• have the potential to cause pulmonary and retroperitoneal fibrosis.
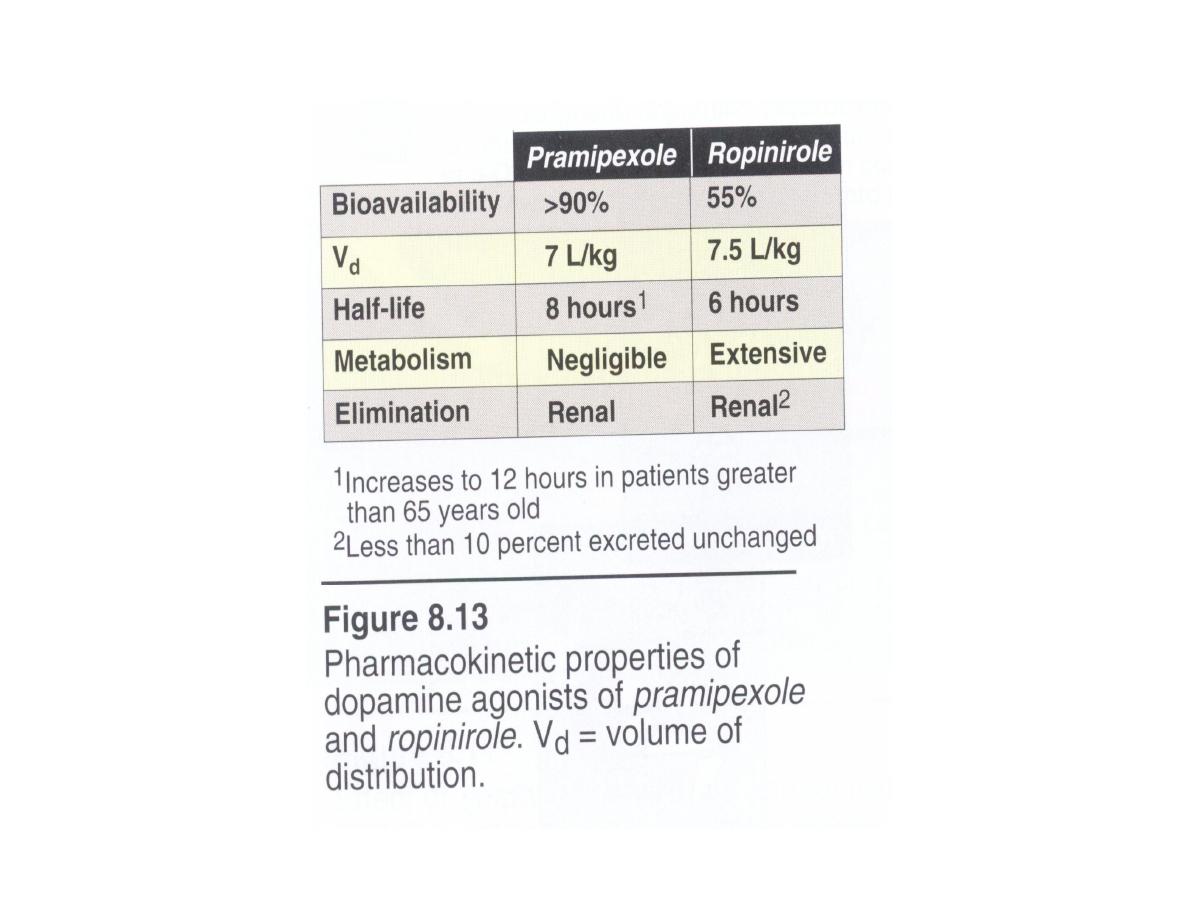
Pramipexole and ropinirole
•
Pramipexole
and
ropinirole
are non-ergot agonists at dopamine receptors.
• They alleviate the motor deficits in both
levodopa-naive
patients and patients
with advanced Parkinson disease taking
levodopa.
• They delay the need to employ
levodopa
therapy in early Parkinson, and may
decrease the dose of
levodopa
in advanced Parkinson.
Unlike the ergotamine derivatives:
1-
pramipexole
and
ropinirole
do not exacerbate peripheral vasospasm, nor do
they cause fibrosis.
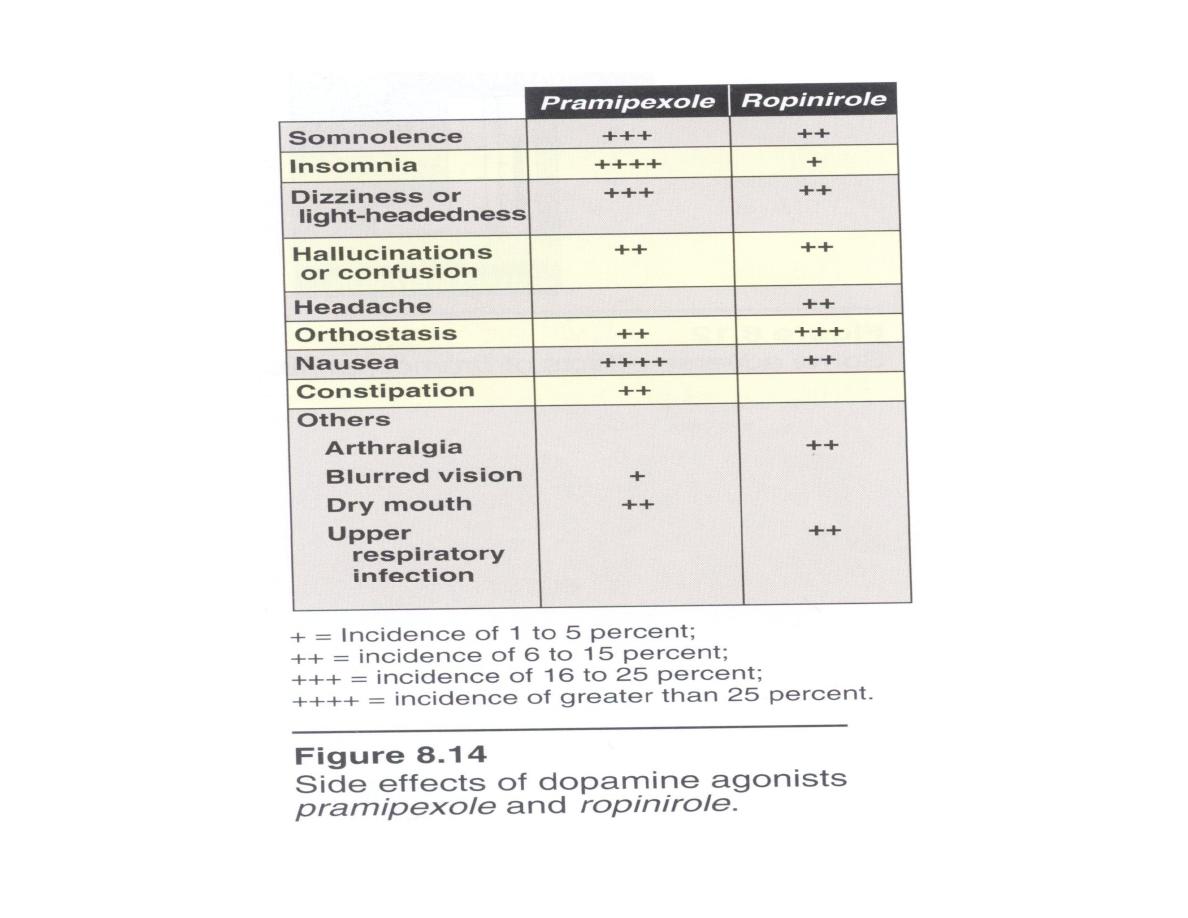
2- Nausea, hallucinations, insomnia, dizziness, constipation, and orthostatic
hypotension are among the more distressing side-effects of these drugs;
3- dyskinesias are less frequent than with
levodopa.
4-
pramipexole depend
on renal function for its elimination, so,
Cimetidine,
which inhibits renal tubular secretion of organic bases, increases the half-life of
pramipexole
by forty percent.
5- The fluoroquinolone antibiotics shown to inhibit the metabolism of
ropinirole.
Amantadine
• It was accidentally discovered that the antiviral drug
amantadine
effective in
the treatment of influenza.
•
Amantadine
increasing the release of dopamine, blocking cholinergic
receptors, and inhibiting the N-methyl-D-aspartate (NMDA) type
glutamate receptors.
• CNS: restlessness, agitation, confusion, hallucinations, and acute toxic
psychosis.
• Orthostatic hypotension, urinary retention, peripheral edema, and dry mouth
also may occur.
•
Amantadine
is less efficacious than
levodopa,
and Tolerance develops
more readily.
• The drug has little effect on tremor, but is more effective than the
anticholinergics against rigidity and bradykinesia.
Selegiline
selectively inhibits MAO B (which metabolizes dopamine), but does not
inhibit MAO A (which metabolizes norepinephrine and serotonin).
Thus decreasing the metabolism of dopamine à increase dopamine
levels in the brain.
v
It enhances the actions of
levodopa
v
when administered together,
it
reduces the required dose of
levodopa.
v
If
selegiline is
administered at high doses, the selectivity of the drug is
lost, and the patient is at risk for severe hypertension.
v
Has a neuroprotective effect by suppressing the formation of oxidative
metabolites of dopamine (antioxidant).
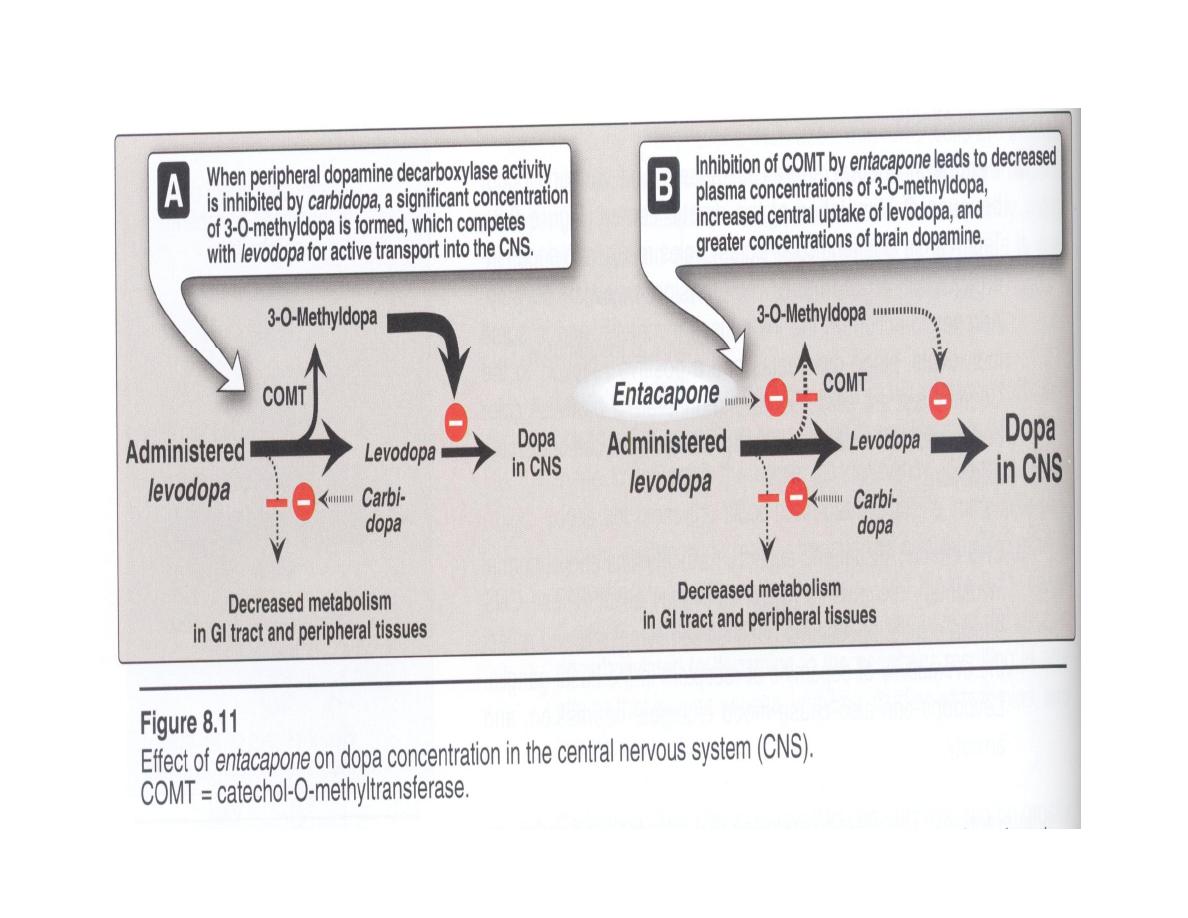
Catechol-O-methyltransferase inhibitors
• the methylation of
levodopa
by catechol-0-methyltransferase (COMT) to 3-
0-methyldopa is a minor pathway for
levodopa metabolism.
•
when peripheral dopamine decarboxylase activity is inhibited by carbidopa,
a significant concentration of 3-0-methyldopa is formed that competes with
levodopa for active transport into the CNS.
•
inhibition of COMT by
entacapone or tolcapone
leads to decreased
plasma concentrations of 3-0-methyldopa, increased central uptake of
levodopa, and greater concentrations of brain dopamine.
•
Both reduce the symptoms of "wearing-off" phenomena seen in patients on
levodopa-carbidopa.
•
Entacapone and tolcapone are nitrocatechol derivatives that selectively and
reversibly inhibit COMT.
Oral absorption of both drugs occurs readily and is not
influenced by food.
• They are extensively bound to plasma albumin (>98 percent),
with limited volumes of distribution.
•
Tolcapone
penetrates the blood-brain barrier and inhibits
COMT in the CNS.
•
Tolcapone
has a long duration of action.
• Both drugs are extensively metabolized
• Dosage may need to be adjusted in patients with moderate or
severe cirrhosis.
Pharmacokinetics
Adverse effects
• diarrhea, nausea, anorexia,
• postural hypotension
• dyskinesias, hallucinations, and sleep disorders
• fulminating hepatic necrosis is associated with
tolcapone
use.
Antimuscarinic agents
•
The antimuscarinic agents are much less efficacious than
levodopa
and play
only an adjuvant role in antiparkinsonism therapy.
benztropine, trihexyphenidyl,
and
biperiden
• All these drugs can induce mood changes,`xerostomia and visual problems.
• They interfere with gastrointestinal peristalsis, and are contraindicated in
patients with glaucoma, prostatic hypertrophy or pyloric stenosis.
• Blockage of cholinergic transmission produced effects similar to augmentation
of dopaminergic transmission.
• Adverse effects are similar to those caused by high doses of
atropine—for
example, pupillary dilation, confusion, hallucination, urinary retention, and dry
mouth.

٦٢
THANK YOU
THANK YOU
