ANTIHyperlipidemiC DRUGS
Lipids are transported in the blood by being incorporated within
lipoproteins.
Lipoproteins are macromolecular disc like complexes of lipids and
specific proteins called apoproteins. These apoproteins are crucial
in the regulation of lipoprotein metabolism (they act as enzymes,
cofactors or cell receptor ligands). Distinct classes of lipoproteins
are found depending on the variation in lipid and apoprotein
composition.
Chylomicrons and their remnant contain apoprotein ß48 which is
formed in the intestine. Apoprotein ß100 is synthesized in the liver
and are found in (VLDL, IDL, LDL and lipoprotein a)
Lipoproteins that convey lipids into the artery wall.
Plasma cholesterol and triglyceride are clinically important
because they are major treatable risk factors for atherosclerosis
and cardiovascular diseases. Hypertriglyceridemia also
predispose to acute pancreatitis.
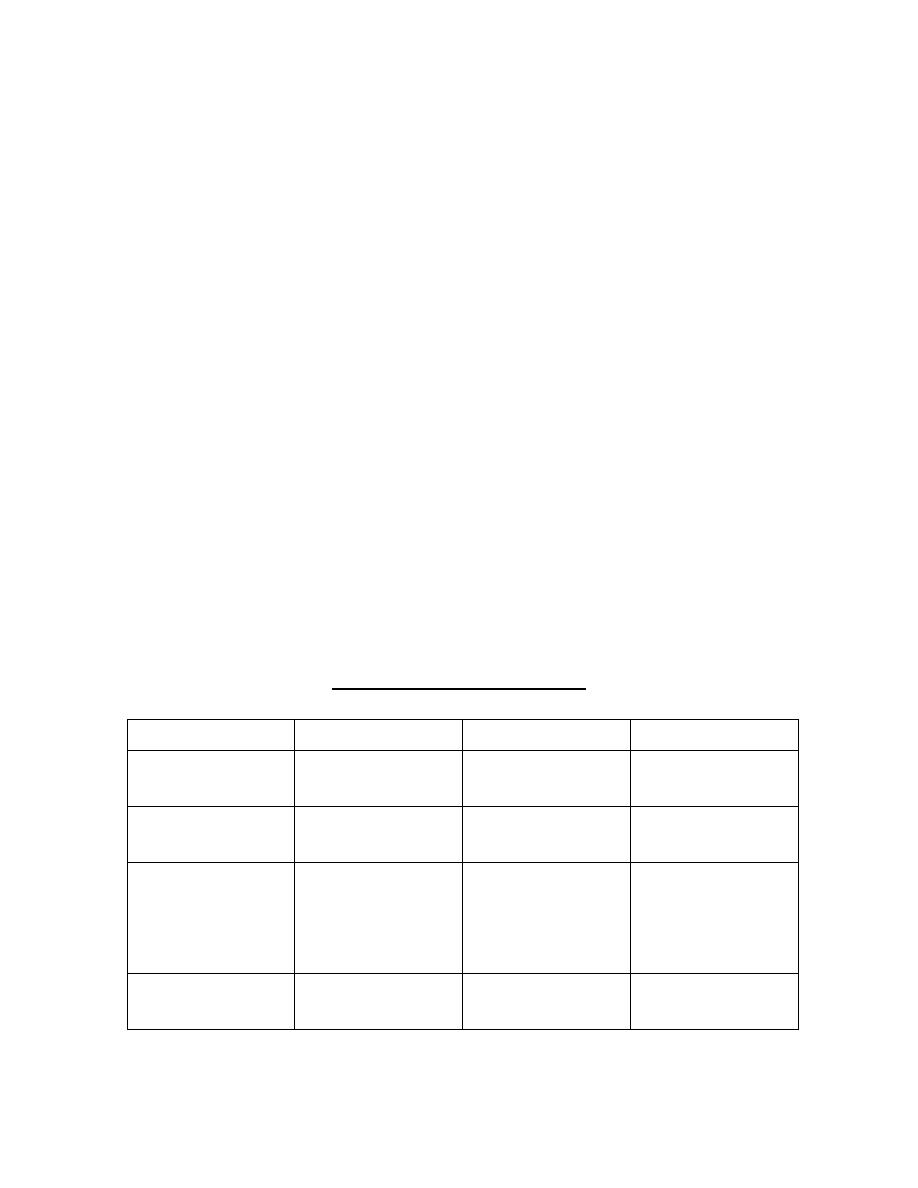
Adult treatment guidelines
Desirable
Borderline
High
Tc
<200(5.2)
200-239(5.2-
6.2)
>240(6.2)
LDL
<130(3.4)
130-159(3.4-
4.1)
>160(4.1)
HDL
Men
Women
>40(1.04)
>50(1.3)
TG
<150(1.7)
150-199(1.7-
2.3)
>200(2.3)
Optimal levels of LDL is <100 and to 60-70 in patients with CAD.
High risk patients should aim levels: HDL >38, fasting TG < 180
and Tc < 150 mg/dl.
Levels of Tc, TG, and HDL should be obtained after 12 hours
fasting.
To permit calculation of LDL:
LDL=Tc - HDL-(TG/2.3 mmol/l)
Lipid levels in mg/dl can be converted to mmol/l by dividing by 38
for cholesterol and 88 for TG.
* This formula becomes unreliable when TG exceeds 4mmol/l (350
mg/dl)
Lipoprotein Disorders:
Primary lipid abnormalities may be diagnosed after exclusion of
secondary lipid disorders.
The numerical Fredrickson classification (type I-V) is no longer in
use instead primary lipid disorders are classified according to the
predominant lipid problem
Hypercholesterolemia
Hypertriglyceridemia
Mixed hyperlipidemia
Causes of secondary hyperlipidemia:
1) Secondary hypercholesterolemia (common causes)
hypothyroidism, pregnancy, cholestatic liver disease,
drugs(diuretics, steroids, androgens), nephritic
syndrome (early nephrosis)
2) Secondary Hypertriglyceridemia (common causes): DM
(type2) ,chronic renal disease(uremia, severe
nephrosis), abdominal obesity, excess alcohol,
hepatocellular disease and drugs(ß-blockesr,
corticosteroids, estrogens).
Management:
Lipid lowering therapies have a key role in the secondary and
primary prevention of CVS disease. Assessment of absolute risk,
treatment of all modifiable risk factors and optimization of life
style factors especially diet and exercise are central to the
management.
Non pharmacological treatment:
1- Reduce intake of saturated fat to less than 7-10% of total
energy.
2- Reduce intake of cholesterol to less than 250mg/day.
3- Reduce sources of saturated fat and cholesterol by low fat
dietary products and low glycemic index carbohydrates.
4- Consumption of vegetable, fruits, legumes & fish.
5- Supplementary intake of fish oil (contain n3 FA) & dietary
fibers.
6- Achieve ideal body weight and increase activity and exercise.
7- Reduce or stop alcohol intake, also stop smoking.
Pharmacological treatment:
Predominant hypercholesterolemia:
1) Statins (HMG CoA reductase inhibitors).
2) Nicotinic acid (vit.B3) Niacin.
3) Cholesterol absorption inhibitors (Ezetimibe)
4) Bile acid sequestrating resins.
*start with statin (Ezetimibe if intolerant)
So: statin ± Ezetimbe ± Resin or Niacin.
Predominant Hypertriglyceridemia:
1) Fibrates.
2) Highly polyunsaturated n=3 fatty acids.
* start with fibrates (fish oil if intolerant)

So: fibrates ± fish oil ± Niacin.
Mixed hyperlipidemia:
Combination therapy is often required
Statin + fish oil is safer and effective when TG are not so
high.
Fibrates + cholesterol absorption inhibitors
Statin + Niacin
Statin + Fibrates
In the last two combinations the risk of myopathy is greater.
Drugs:
3-hydroxy-3-methylglutaryl (HMG) Coenzyme A (CoA) reductase
inhibitors commonly known as Statins.
In order of potency as LDL lowering agents these are:
Rosuvastatin and Atorvastatin→Simvastatin → Pravastatin →
Lovastatin → Fluvastatin.
*Pravastatin & Fluvastatin are active as such Lovastatin &
Simvastatin are hydrolysed to the active drug.
Mechanism of action:
These drugs inhibit cholesterol synthesis by competing effectively
to inhibit the HMG CoA reductase the rate limiting step in the
cholesterol synthesis thus depleting the intracellular supply of
cholesterol.This depletion leads to increased activity and number
of LDL receptors which increase the clearance of LDL and it's
precursor IDL and causing secondary reduction in LDL synthesis.
As a result Statins reduce LDL by up to 60% reduce TG up to 40%
and ↑HDL up to 10%.
The therapeutic benefits also include plaque stabilization.
Improvement of coronary endothelial function,inhibition of
platelet thrombus formation,and anti inflammatory activity.
• The population who may benefit from statins is large and are
‘rationed’ according to the following priorities:
– 1
st
choice: for pts following MI or with angina, even for
pts with ‘normal’ total cholesterol levels
– 2
nd
choice: patients with a 30% ten year risk of
cardiovascular disease (e.g. hypertension/diabetes)
with a total cholesterol > 5mM
• Jan 2006 – NICE: recommends statins for primary
prevention in patients with CV risk >20%
• Statins should be considered for all patients at high risk of
cardiovascular disease irrespective of cholesterol?
• The combination of: Statin + aspirin + b-blocker + ACE :
independently and additively reduce risk in secondary
prevention with a 75% reduction in risk.
Adverse effects: these drugs are well tolerated & safe. Side effects
are rare. These include:
Liver function test abnormalities which returns to normal
after stopping the drug.
Muscle: Myalgia, increased CK Myositis & infrequently
rhabdomyolysis.
Drug interactions:
Fibrates and Niacin when combined with Statins →↑the incidence
of myopathy.
Statins →↑ Warfarin levels.Also interactions with ciclosporin
,itraconazol ,fibrates and protease inhibitiors
Contraindications:
Pregnancy and lactation
They shouldn't be used in children.
Nicotinic acid (Niacin):
Mechanism of action:
In pharmacological doses (in grams) Niacin reduces peripheral

FA release (by inhibiting lipolysis in adipose tissue) into the
circulation which the liver utilizes for TG synthesis. This TG is
required for VLDL synthesis in the liver also LDL is deived from
VLDL in the plasma.
Therefore a reduction in the VLDL production leads to ↓LDL
levels; the result therefore is ↓Tc and TG while HDL is increased.
Niacin also ↑ the secretion of tissue plasminogens activator and ↓
levels of plasma fibrinogen.
These effects of Niacin reverse some of the endothelial cell
dysfunction contributing to thrombosis associated with
hypercholesterolemia and atheroseclerosis.
Adverse effects:
a- Flushing (intense cutaneous flush) and pruritis which is
reduced or prevented by administration of aspirin prior to
Niacin because it's prostaglandin mediated.
b- Other side effects include: gastric irritation, abnormal liver
function test, exacerbation of Gout & hyperglycemia.
Fibrates: are fabric acid derivative Fenofibrate and Gemfibrozil
Fenofibrate is a prodrug and is more effective than Gemfibrozil.
Mechanism of action:
Fibrates stimulate Peroxisome proliferator activated receptor
alpha (PPAR)-α which controls the expression of gene products
that mediate the metabolism of TG & HDL.As a result synthesis of
FA , TG & VLDL is reduced while lipoprotein lipase activity
which catabolizes TG is enhanced, in addition the promoter
regions of genes such as apolipoprotein I and ATP binding
cassette A1, are up regulated leading to ↑HDL, consequently
Fibrates reduce TG up to 50%, and ↑HDL by 20% but LDL
changes are variable.
Adverse effects:
Exhibit a similar profile & frequency of side effects as Statins
including Myalgia, Myositis and abnormal liver function test.
Fibrates cause mild GIT disturbances & ↑risk of cholelithiasis and
prolong the action of anticoagulants.
Cholesterol absorption inhibitors:
Ezetimibe:
Mechanism of action:
These inhibit the intestinal mucosa transporter NPC
1
L
1
that
absorbs dietary and biliary cholesterol. The resultant depletion of
hepatic cholesterol up regulates hepatic LDL receptor activity.
This mechanism is synergistic with statins,
LDL is reduced by 17%, TG is reduced by 6% While HDL is
increased by 1.3%
Bile acid sequestrating Resins:
Cholestyramine-Colestipol and Colesevelam:
Mechanism of action:
These are anion exchange resins that bind negatively charged bile
acids & bile salts in the small intestine. The complex is excreted in
feces & therefore preventing the bile acids from returning to the
liver through the enterohepatic circulation. As a result the liver
increases its de novo bile acid synthesis from hepatic cholesterol.
The resultant depletion of hepatic cholesterol up regulates LDL
receptor activity and reduces LDL in a manner similar to statins
(and also synergistic to statins). These drugs cause substantial
decrease in LDL and modest increase in HDL but minimal effects
on TG.
Cholestyramine is also used to relieve pruritis due to accumulation
of bile acids in patients with biliary obstruction.
Adverse effects:
A) GIT disturbance such as constipation, nausea & flatulance
B) Impairment of absorption of fat soluble vitamins (A,E,D,K).
C) Interference with absorption of many drugs therefore these

drugs should be given at least 2 hours before resin.
Highly poly unsaturated long chain (n=3) fatty acids
(Fish oil)(omega fatty acids)
Eicosapentanoic acid (EPA) and Docosahexanoic acid (DHA)
comprise 30% of the fatty acids in fish oil. EPA & DHA are
potent inhibitors of VLDL TG formation.
Intake of 2gm of n3 fatty acid (equal to 6gm of most forms of
fish oil) per day lower TG in a dose dependant manner. Up to
50% reduction of TG can be achieved with 15gm fish oil per
day. Changes in LDL & HDL are variable.Fish oil also inhibit
platelet aggregation and have been shown to decrease mortality
from CHD(coronary heart disease).
Fish oil is safe and well tolerated.
