Human Immunodeficiency Virus
(HIV)
(
AIDS
)
Acquired Immunodeficiency
Syndrome
AIDS
HIV-1
wor
ld wide
HIV-2
west Africa
HISTORY
RETROVIRIDAE FAMILY
• Retro
=
reverse
• 2
medically important groups:
1-
Oncovirus
=
sar
coma
&
leuk
emia
v.(e.g:HTLV)
2-
Lentivirus
human(
HIV
)
animal(
visna v
.)
3-
spumaviruses
non
human pathogens.
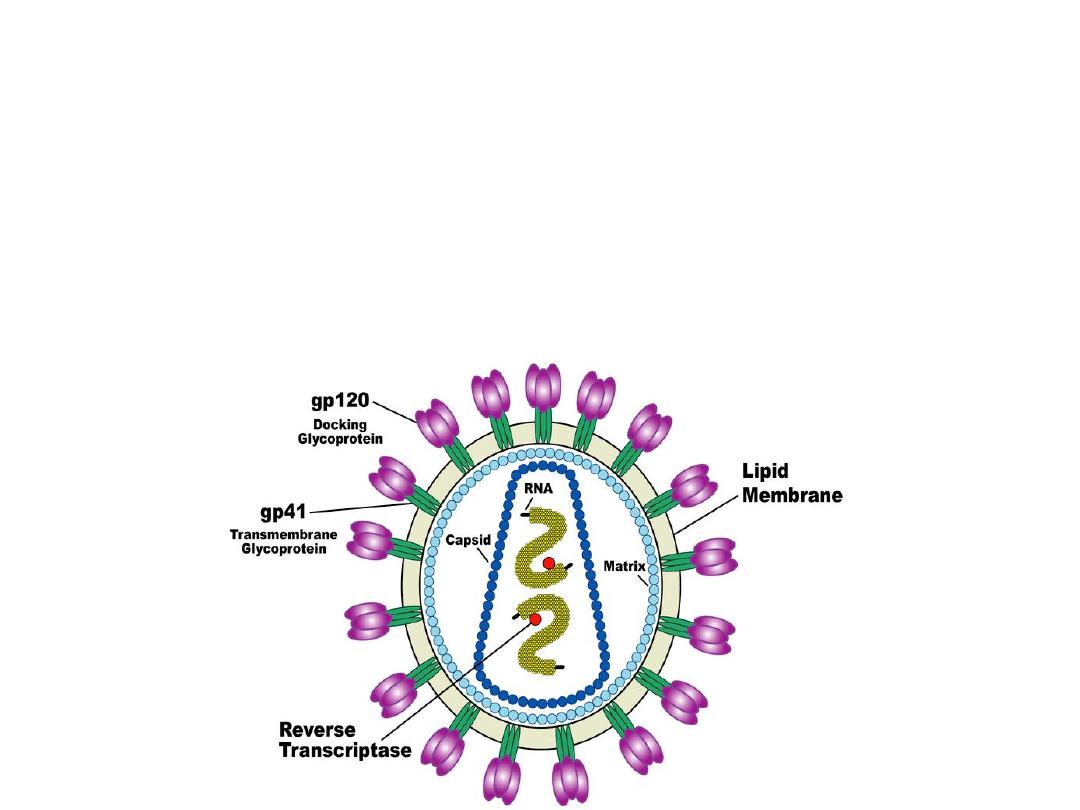
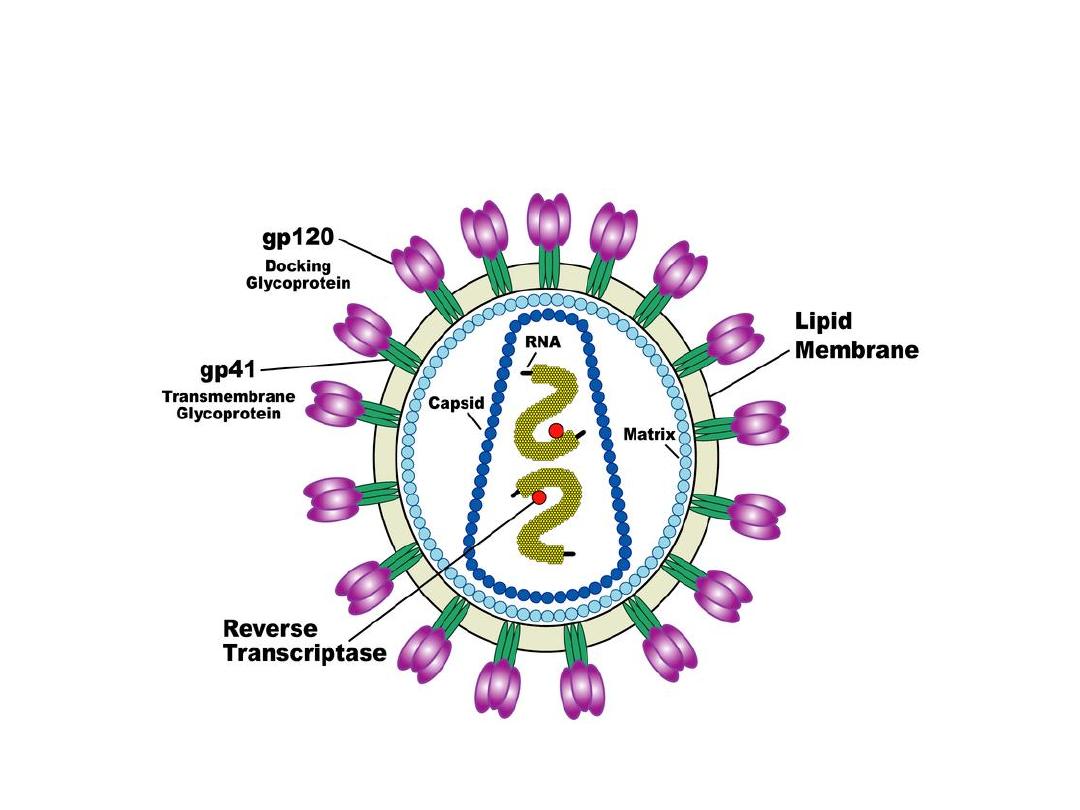
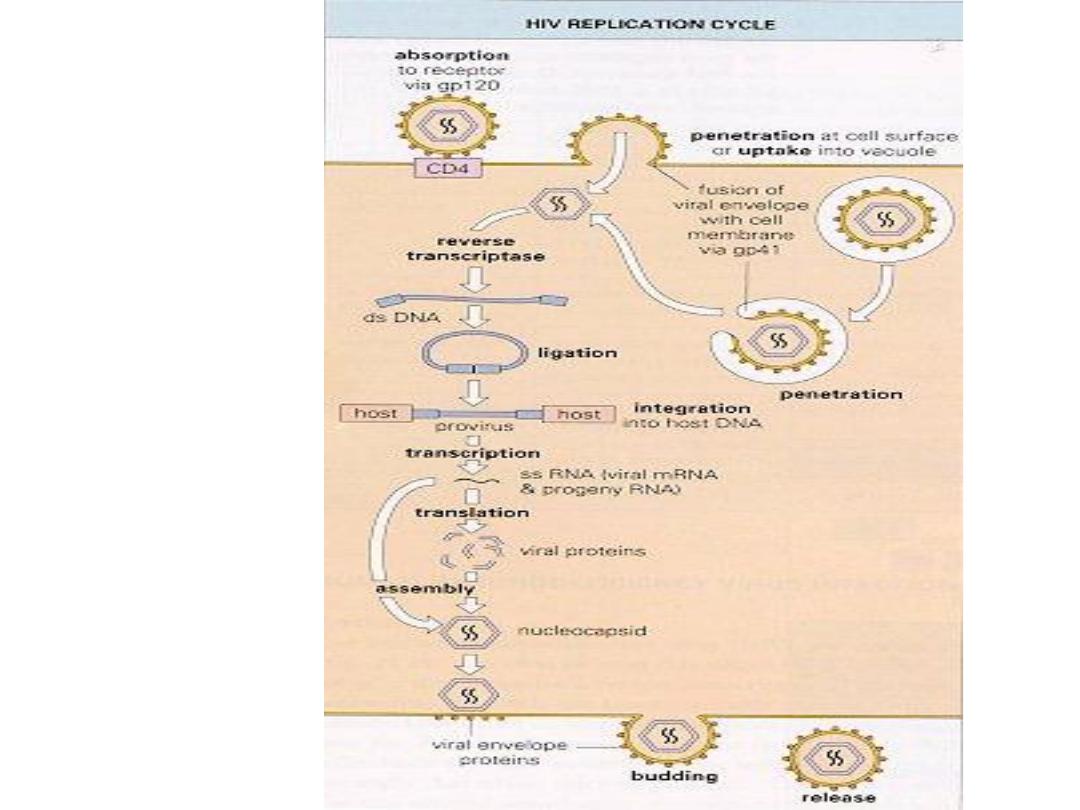
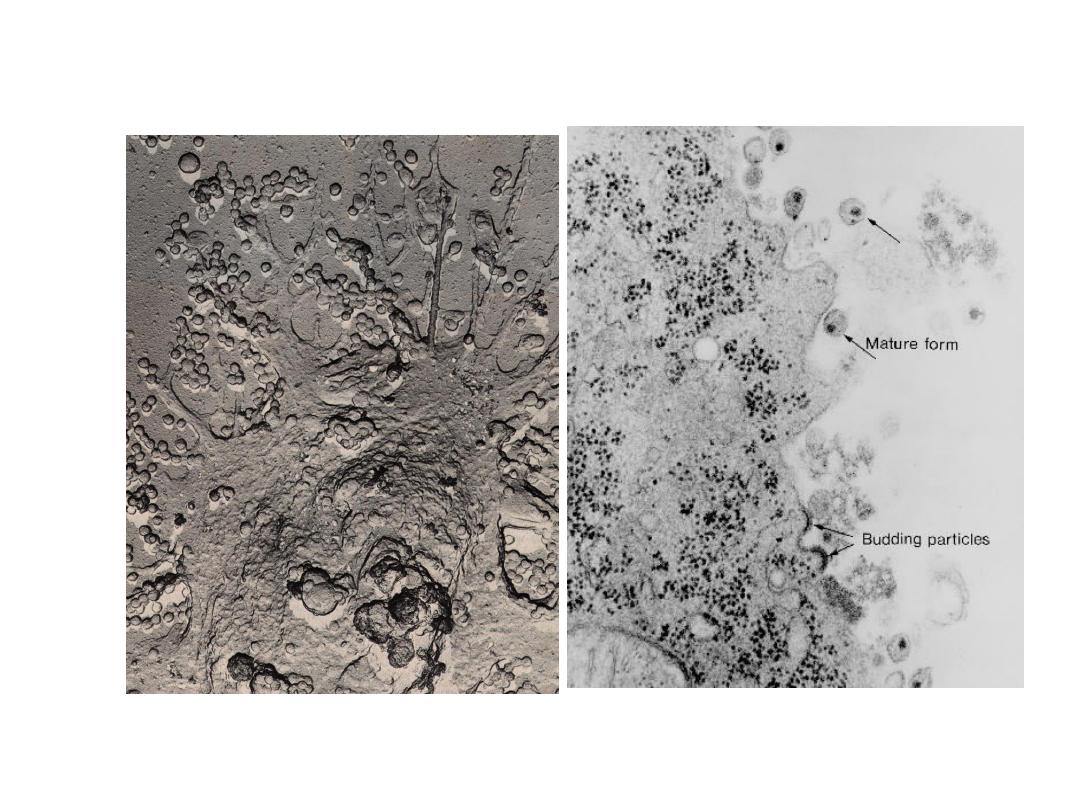
Virion Structure
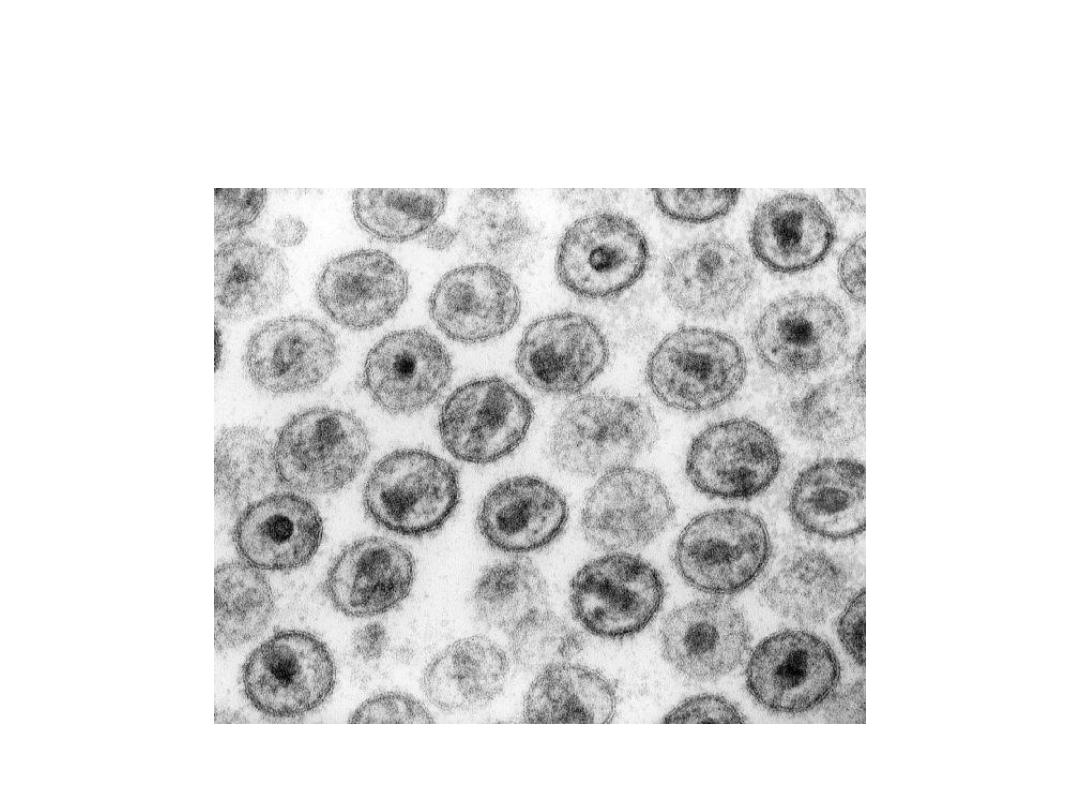
• virion is ~120nm in diameter, spherical
• Lipid membrane –host derived and contains viral glycoproteins – gp120 and gp41
• Matrix protein (p17) surrounds the conical--‐shaped capsid (p24),which encloses
two copies of the single--‐stranded RNA genome(diploid genome).
• Nucleocapsid proteins p6 and p7 interact with the RNA to prevent degradation by
nucleases
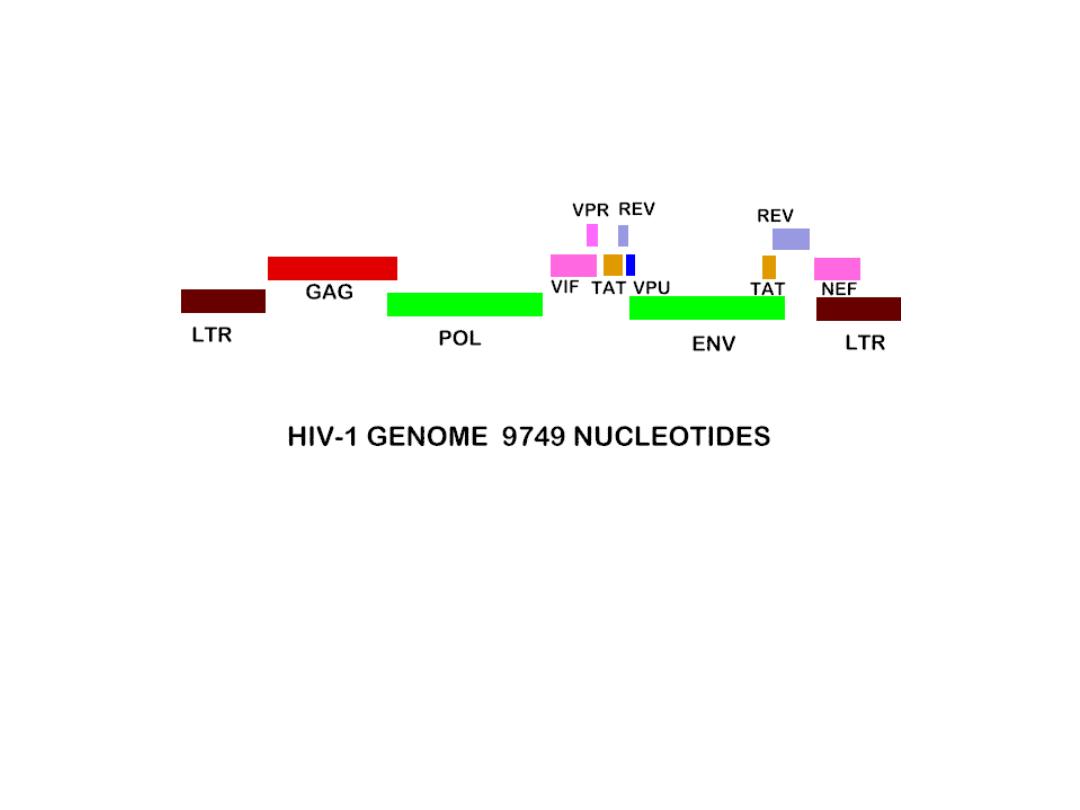
HIV Genome
env
tat
rev
vi f
vpr vpu
nef
gag
pol
• Essential
– Required for HIV
replication
– Tat - transcription
– Rev - RNA transport
– Vif - genome fidelity
• Accessory
– Enhance HIV
production
– Nef
– Vpr
– Vpu
• Universal
– Present in all
retroviruses
– Gag - structural
– Pol - replication
– Env - structural
Source Undetermined
Pathogenesis
• One of the human T-cell lymphotropic
v.(
other: HTCL v.
)
• HIV=== CD4- CMI-opportunistic inf.
=== macrophages
=== monocytes
=== dendtritic cells
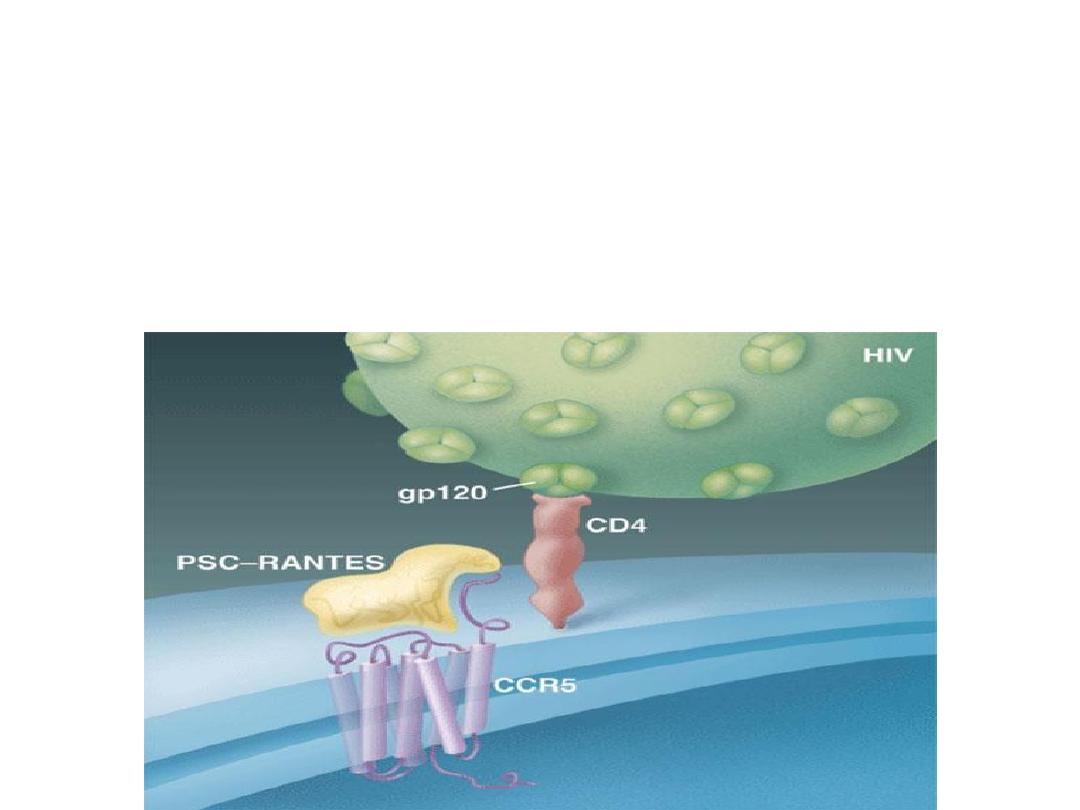
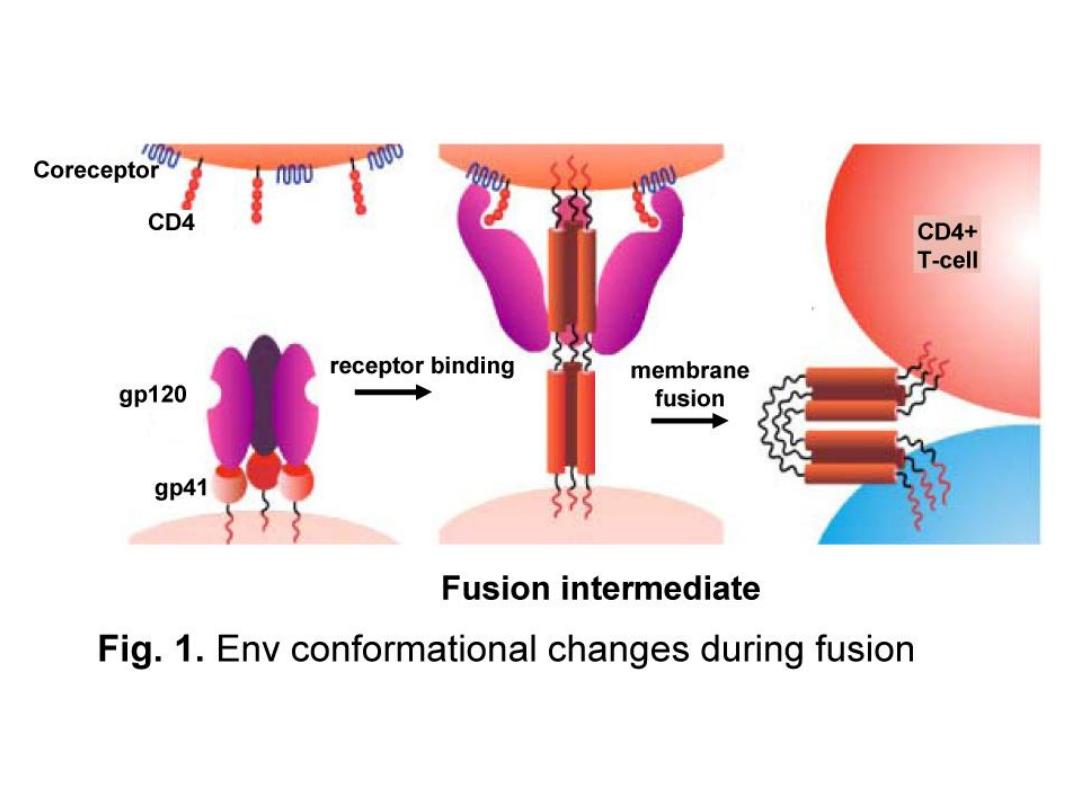
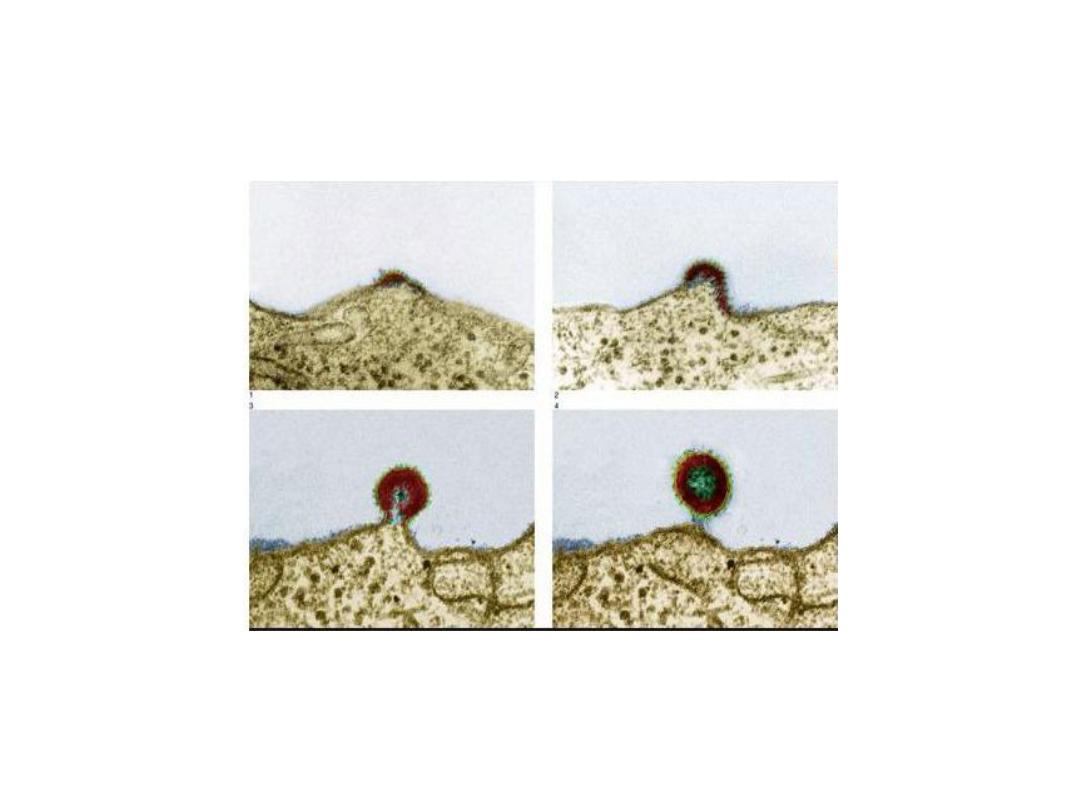
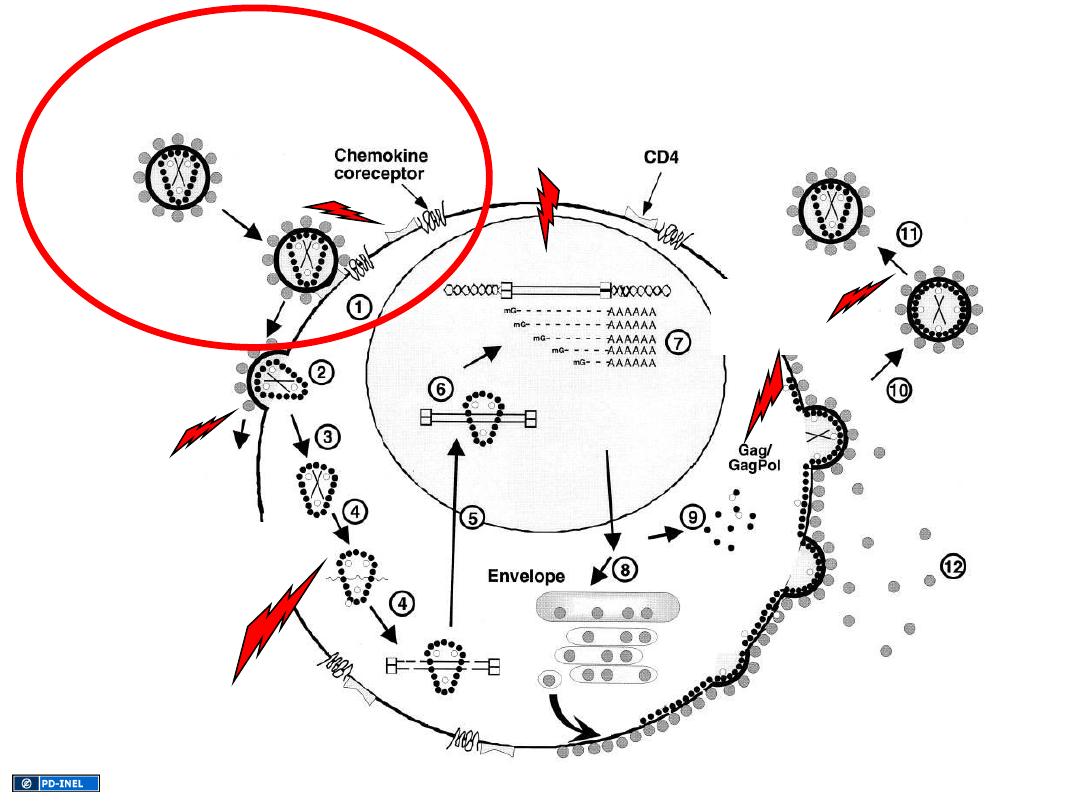
Viral Entry
•
HIV entry
requires the presence of CD4 + one of two co--‐receptors:
CCR5
or
CXCR4
• CD4 is the major determinant of viral tropism –expressed : T cells,
macrophages, monocytes and dendtritic cells
•CCR5 and CXCR4 are chemokine receptors .
CCR5
is found on both
CD4+T
cells and
macrophages
.
CXCR4
is only found on
T cells
.
•
Entry
of HIV is initially mediated by the
attachment
of the viral
envelope glycoprotein,
gp120
, to CD4.
Schematic of HIV
Replication
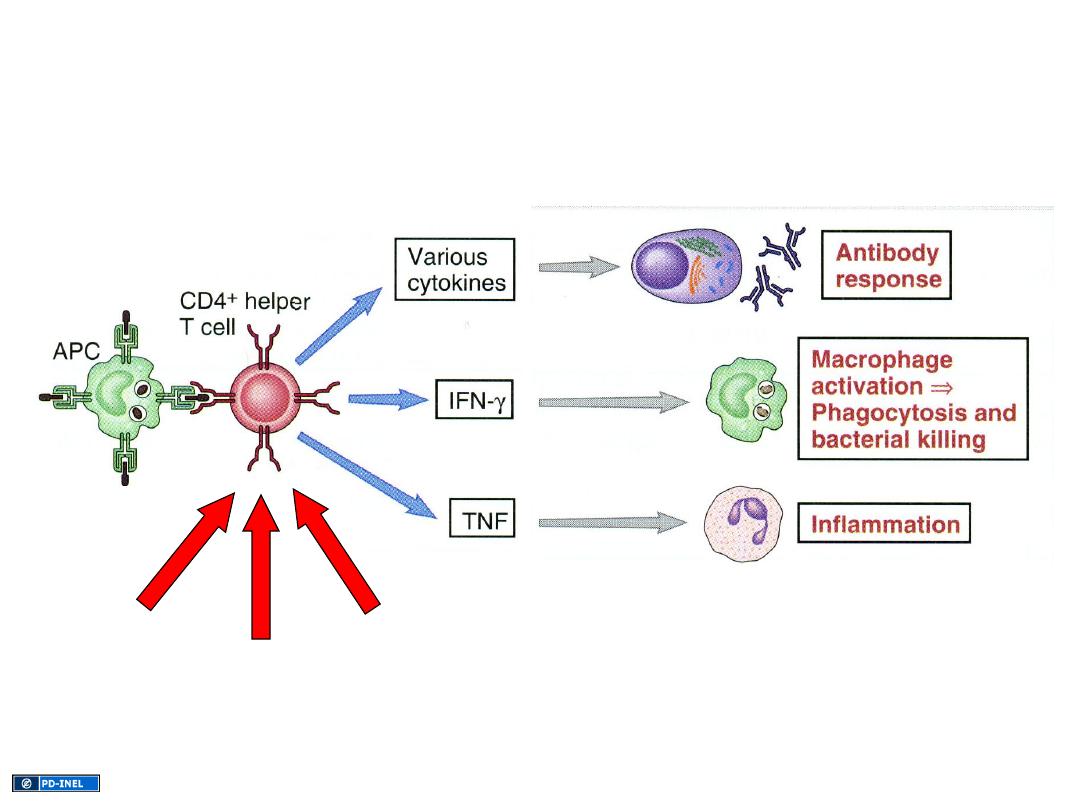
Central role of CD4+ T cell in immune
response
Direct viral
killing
Immune-
mediated
killing
“Bystander”
killing
Sources Undetermined
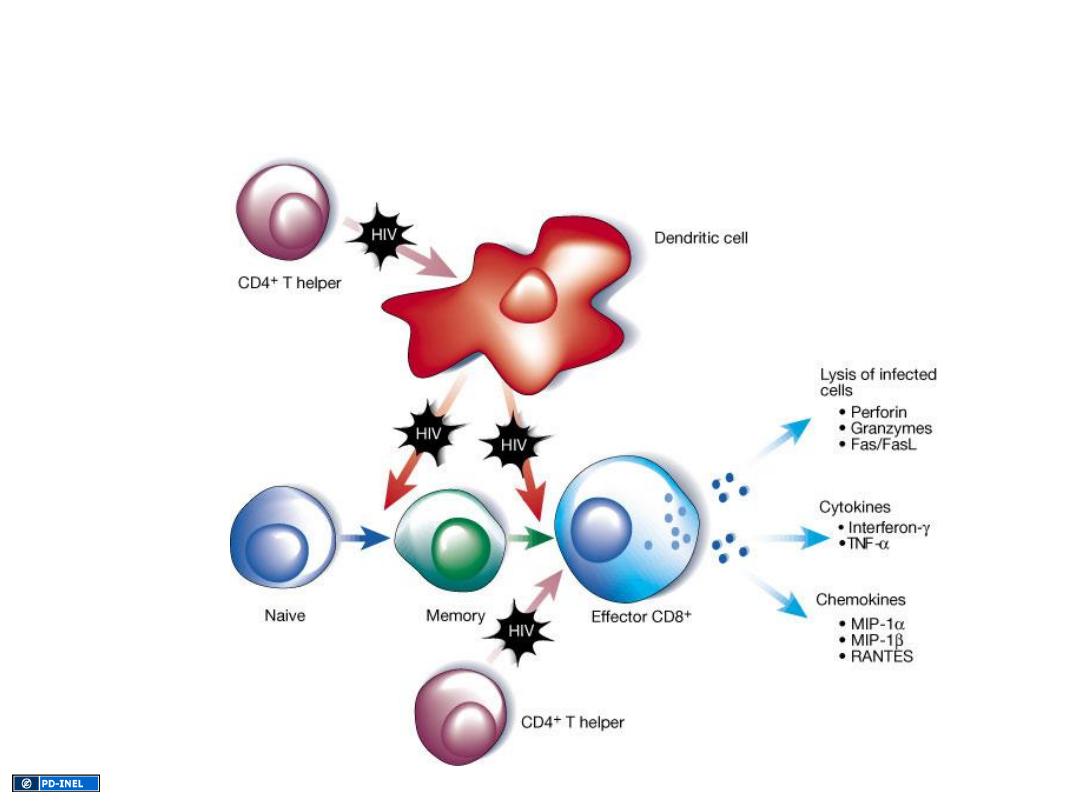
HIV-mediated disruption of CD4
+
T cell
mediated immune responses
Source Undetermined

Clinical Features
1. Early stage- infectious mononucleosis like illness.
2. Latent period - this is the period when the patient is completely
asymptomatic and may vary from a few months to a more than 10
years. The median incubation period is 8-10 years.
AIDS-related complex or persistent generalized lymphadenopathy.
4. Late- Full-blown AIDS.
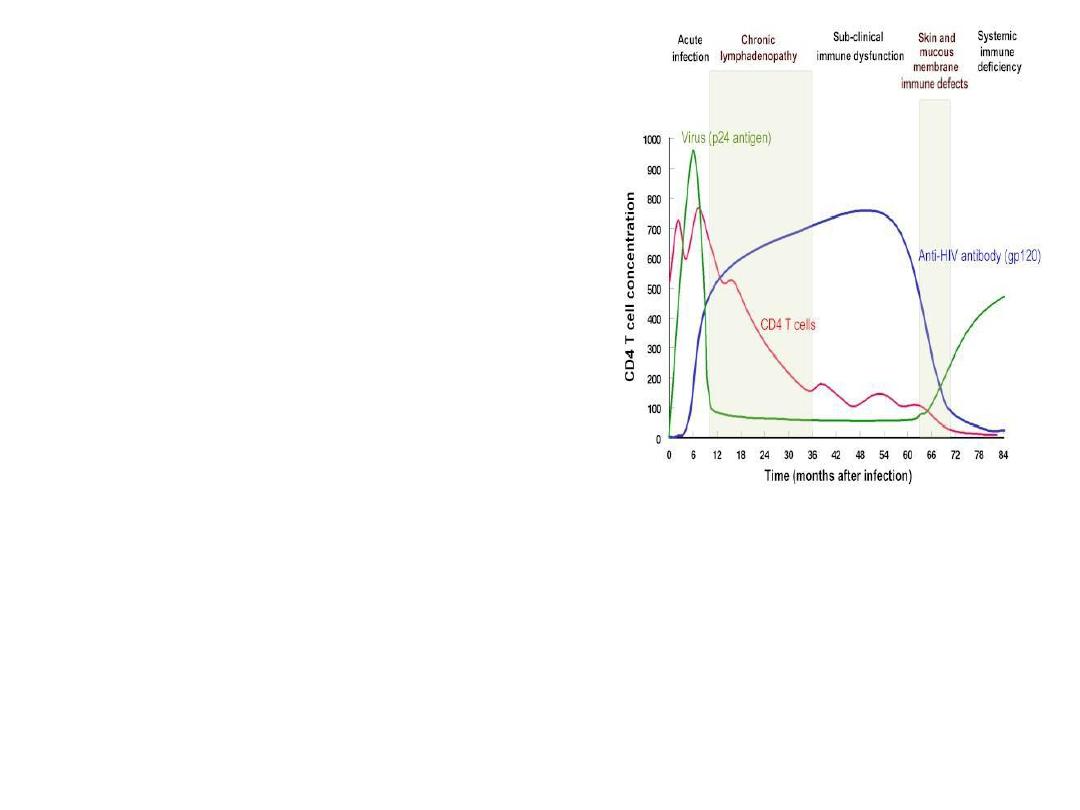
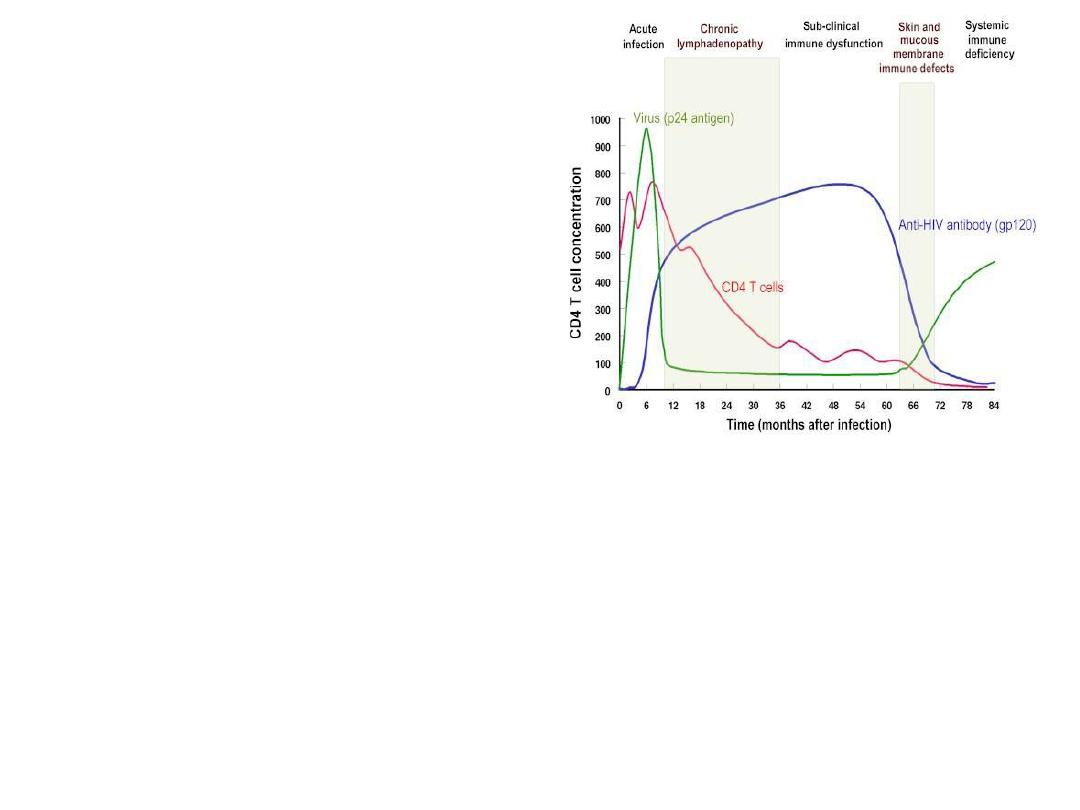
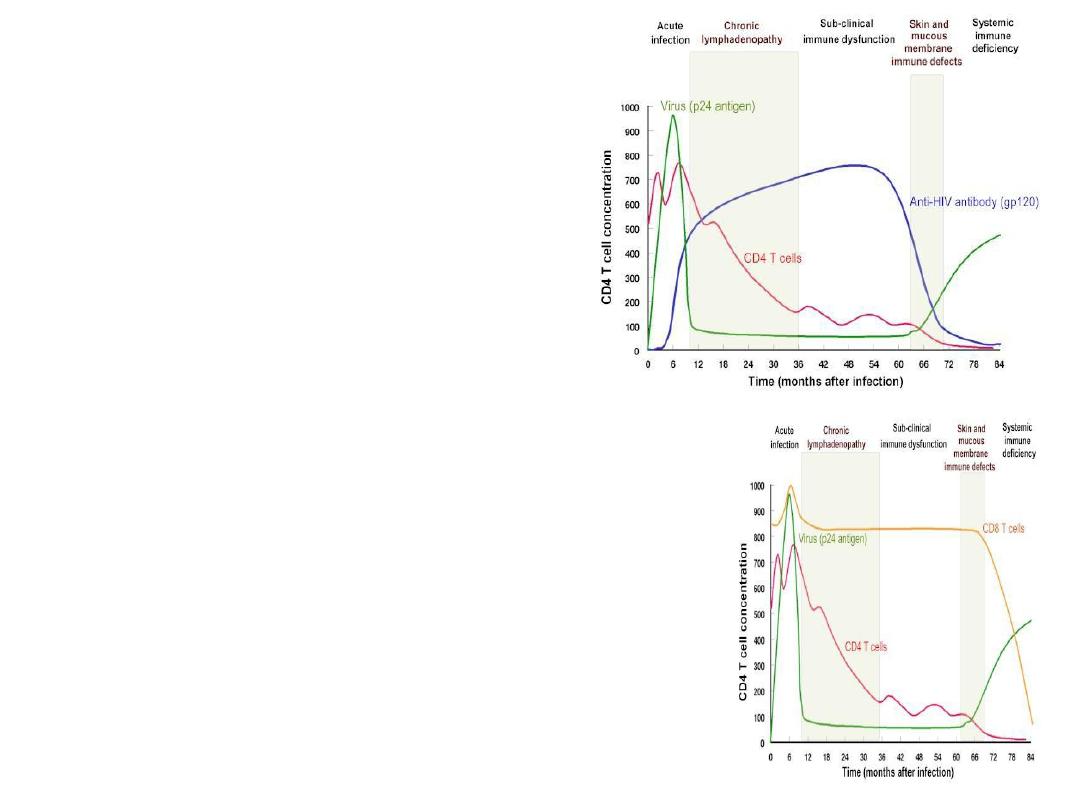
The cellular and immunological picture -The course of the disease,
virus & CD4
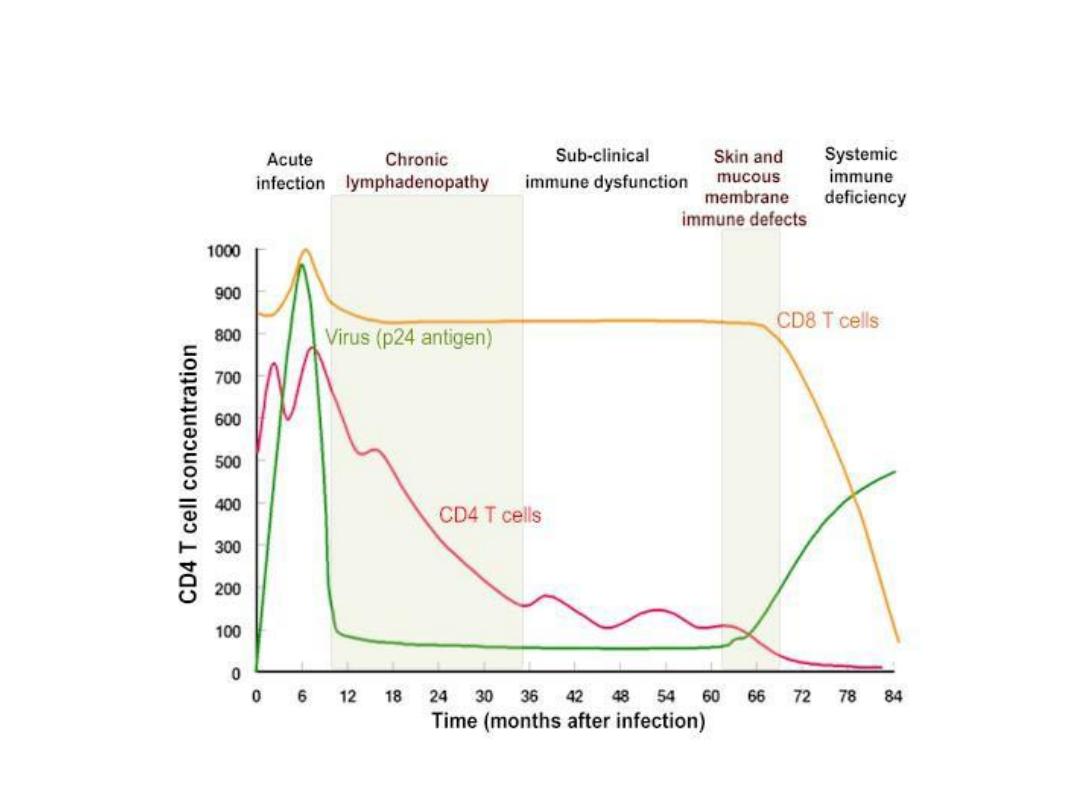
The cellular and immunological picture -The course of the diseaseCD8
• High
virus titer•Mild symptoms
•
Fall
in CD4+ cells but recovers
•
Rise
in CD8+ cells but recovers
•A
high
virus titer (up to 10 million viruses per ml
blood)
•Macrophages :
infected Macrophages bring HIV into
the body if sexually transmitted
cellular and immunological picture
The course of the disease
1. Acute Infection
Virus
almost
disappears
from circulation
•
Good
cytoxic T cell response
•Soluble antibodies
appear later
against both surface and
internal proteins
•Most virus at this stage comes from recently activated
(dividing)and infected CD4+ cells
•
CD4+
cell production
compensates
for loss due to lysis
of cells by virus production and destruction of infected
cells by CTLs
2. A strong immune response
Latency
of virus and of symptoms
•Virus
persists
in extra-vascular tissues
•
Lymph node
dendritic cells
•Resting CD4+ memory cells (last a very long
time -a very
stable
population of cells) carry
provirus
3. A latent state
Massive loss of CD4+ cells
•CD4+ cells are the targets of the virus
•Cells that proliferate to respond to the virus are
killed
by it
•Dendritic cells present antigen and virus to CD4
cells
•
Epitope variation
allows more and more HIV to
escape
from immune response just as response
wanes
•
Apoptosis
of CD4+ cells
•HIV patients with high T4 cell counts
do not
develop AIDS
4. The beginning of disease
CD8+ cells
destroy
more CD4+ cells
•CD4 cell
loss
means virus and infected cells no
longer controlled
•As CD4+ cells
fall
below 200 per cu mm virus
titer
rises
rapidly and remaining immune
response
collapses
•CD8+ cell number
collapses
•
Opp
ortunistic infections
•
Death
in ~2 years without intervention
5. Advanced disease - AIDS
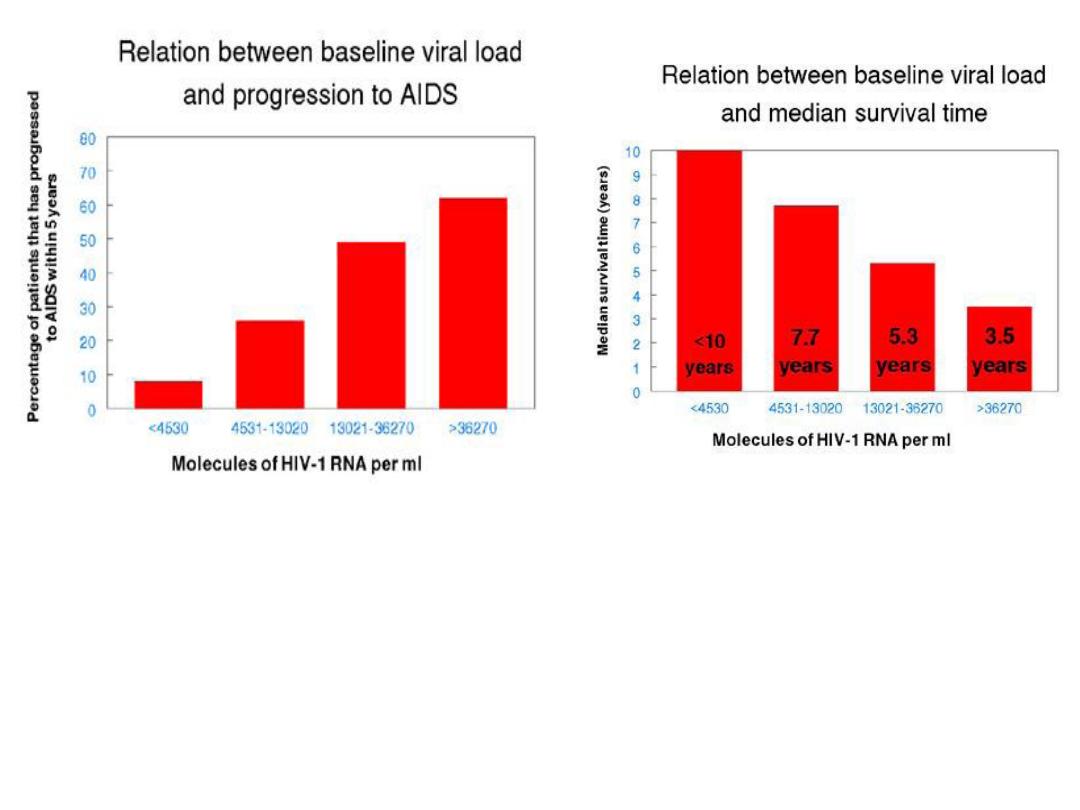
Good correlation between number of
HIV particles measured by PCR and
progression to disease
Viral load predicts survival
time
Opportunistic Infections
Protozoal
pneumocystis carinii (now thought to be a fungi),
toxoplasmosis, crytosporidosis
Fungal
candidiasis, crytococcosis
histoplasmosis, coccidiodomycosis
Bacterial
Mycobacterium avium complex, MTB
atypical mycobacterial disease
salmonella septicaemia
multiple or recurrent pyogenic bacterial infection
Viral
CMV, HSV, VZV, JCV
Opportunistic Tumours
• The most frequent opportunistic tumour,
Kaposi's sarcoma
,
is observed in 20% of patients with AIDS.
• KS is observed mostly in
homosexuals
and its relative
incidence is declining. It is now associated with a human
herpes virus 8 (HHV-8).
• Malignant lymphomas
are also frequently seen in AIDS
patients.

Other Manifestations
• It is now recognised that HIV-infected patients may
develop a number of manifestations that are
not explained
by opportunistic infections or tumours.
• The most frequent
neurological
disorder
is
AIDS
encephalopathy
which is seen in two thirds of cases.
• Other manifestations include
characteristic skin eruptions
and
persistent diarrhoea
.

Kaposi’s Sarcoma
HIV
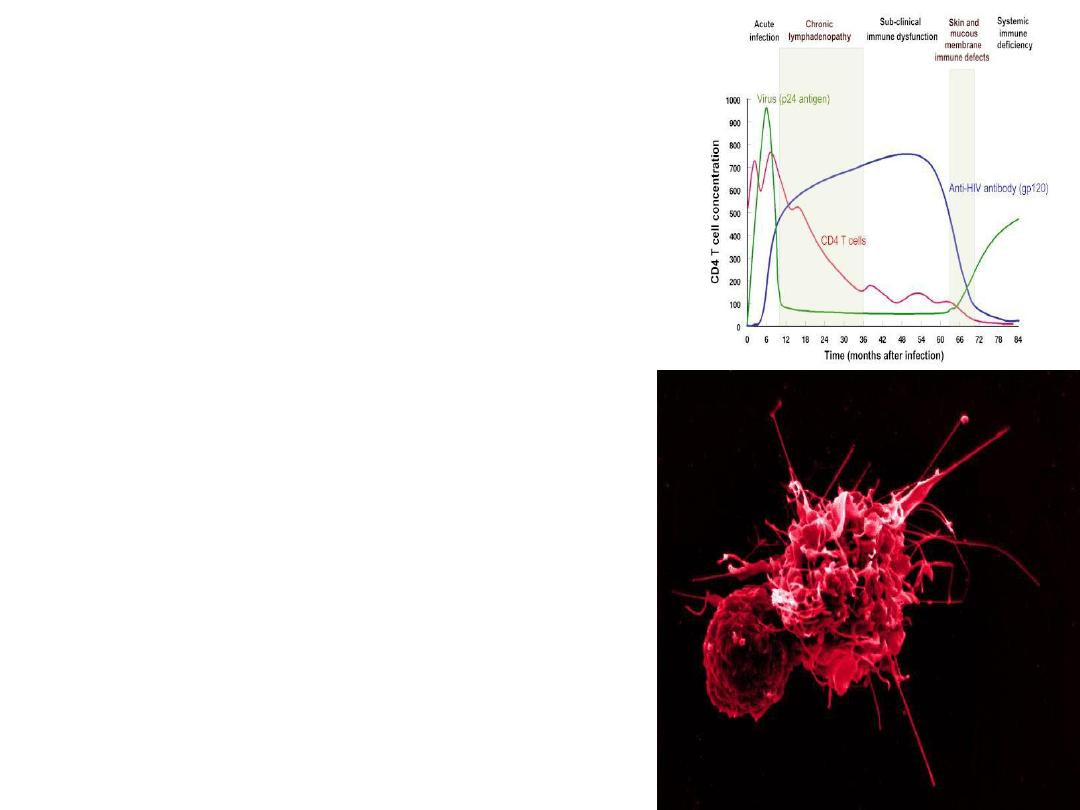
can destroy CD4 T cells in several different ways
• Accumulation
of the nonintegrated DNA copies of the viral
genome,
• increased
permeability
of the plasma membrane,
• syncytia
formation,
• induction of
apoptosis
. Or persistent
noncytocidal
infection
• CD8 T cells are important in delayed type hypersensitivity
(
DTH
) responses, which eliminate viral,fungal, and
mycobacterial infections as well as malignant cells.
• HIV-infected monocytes and microglial cells in the brain die
and release
neurotoxic
substances or chemotactic factors that
promote inflammation in the brain.
• ability to produce
antibodies
in response to an infection is
reduced
, making bacterial infections more common
• Acts as
superantigene
=activate CD4===
demise

Epidemiology
1.Sexual transmission
-
male homosexuals
= N. America
and
Western Europe.
-
heterosexual spread
= developing countries
2. Blood/blood products
-
IV drug abusers
-
Haemophiliacs
3. Vertical transmission
- from mother to the newborn , may occur:
transplacentally
,
perinatally
,
or
postnatally

HIV is
NOT
transmitted by:
casual contact
touching,
hugging,
kissing,
coughing,
sneezing,
insect bites,
water, food,
utensils, toilets,
and swimming pools or public baths.
genetic groups of HIV-1
• M (main)
highly prevalent
10
env
elope
sub
types
===
A
–
J
subtype B ===
Europe and in North and South America
subtype C ===
sub-Saharan Africa
• O (outlier)
HIV-positive persons are
infectious
during both
asymptomatic
and
symptomatic
stages of infection.

In 2003
,
4.8million
people(4.2–6.3million ) =
newly
infected
2.9 million
( 2.6–3.3 million) = death
And
˃ 20 million
since the first cases of AIDS in 1981.
Recent data
,
37.8 million
(34.6–42.3 million)
are living with HIV
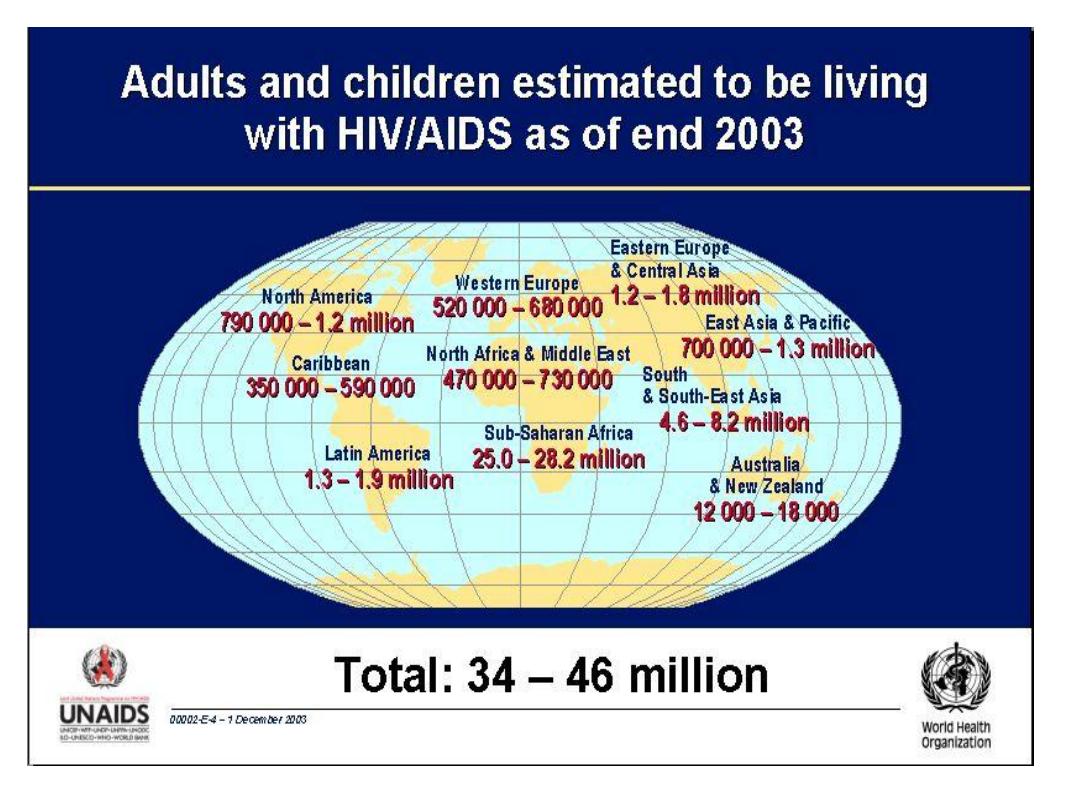
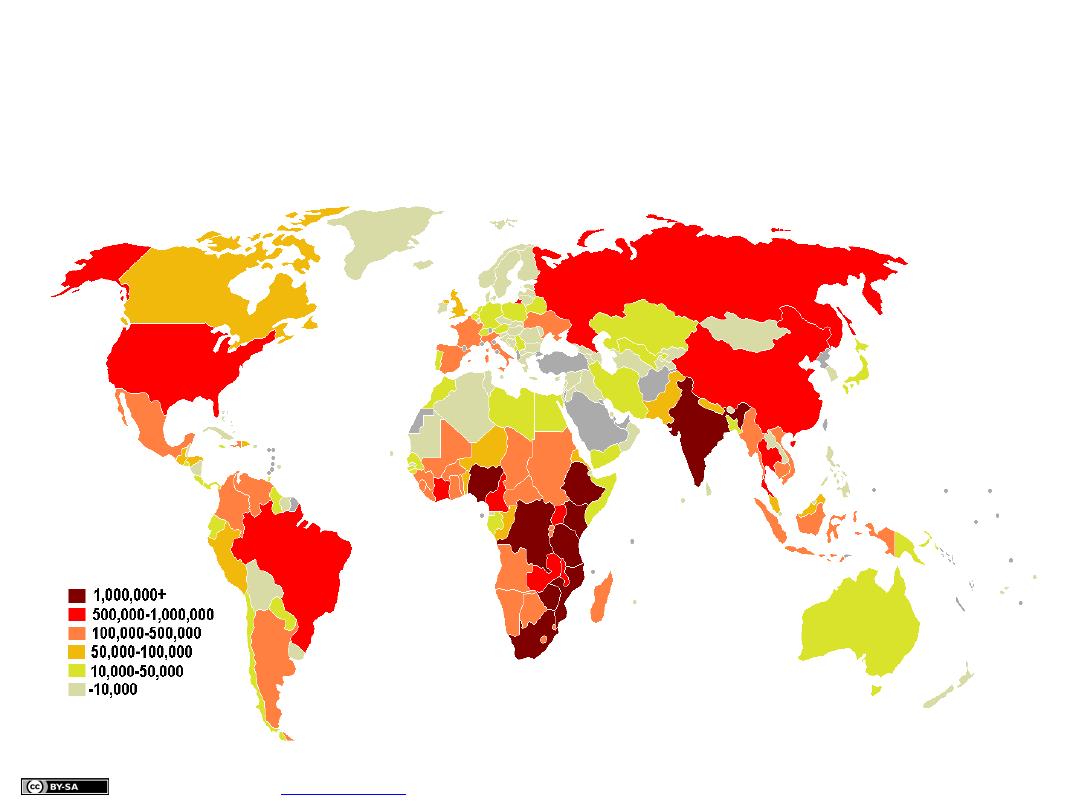
HIV/AIDS disease world-wide (2006)
People living with HIV/AIDS
Per country
UNAIDS 2006 global report,

HIV half-lives
• Activated cells
infected with HIV
produce
and
die
within
1-2 days
.
•
i.e virus present in the plasma.
•
HIV
life-cycle
=
1.5 days
.
• Resting cells
infected produce virus only after
immune stimulation
; these
cells have
a half-life
of at least
5-6 mon
ths.
• Some
cells are infected with
defective virus
that cannot complete the virus
life-cycle. Such cells are
very long lived
, and have an estimated
half-life
of
approximately
3-6 mon
ths.
• Such
long-lived cell present a
major challenge
for
anti-retroviral
therapy.
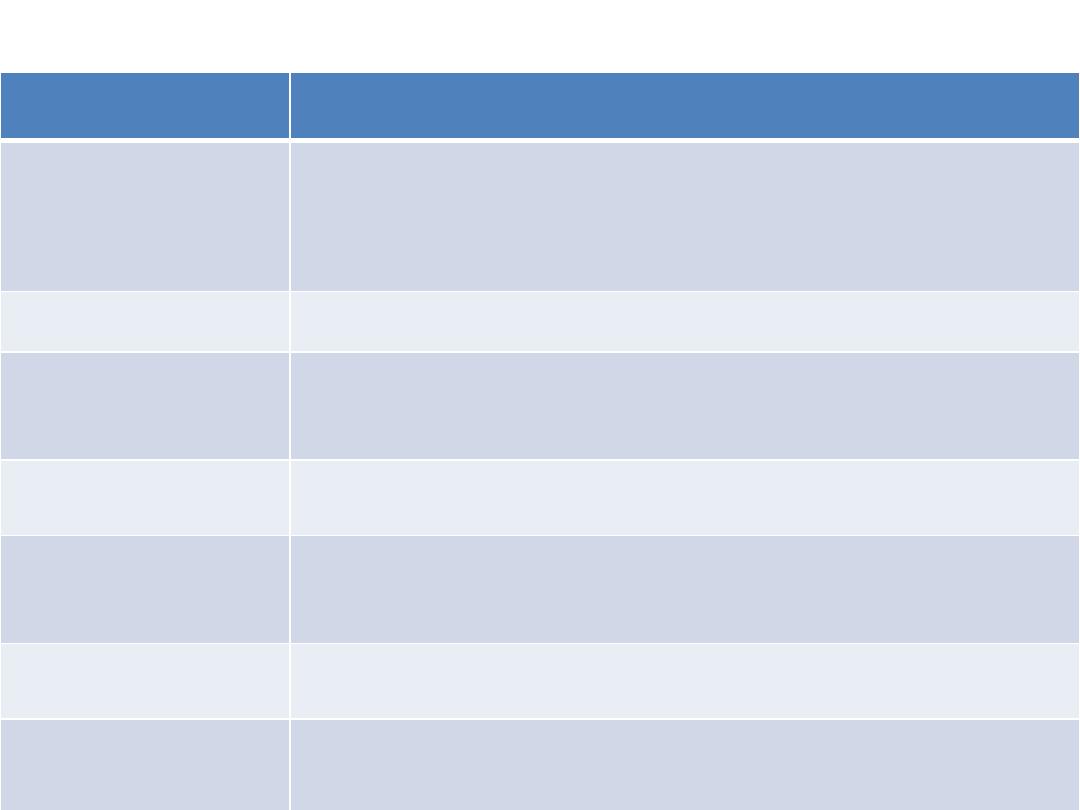
Diagnostic Tests Used to Detect HIV
Infection
tests
Purpose
ELISA
Initial screening;
two
different ELISA
results must be
positive
before a
confirmatory test
is performed
Latex agglutination
Initial screening
Western blot analysis
Confirmatory test
p24 antigen
Early
marker of infection (detection of a
recent
infection)
RT-PCR
Detection of virus
RNA
in blood(detection of
a recent
infection)
and to confirm
treatment
efficacy
CD4:CD8(T-cell ratio)
Staging
the disease and to confirm
treatment
efficacy
Isolation and culture of
virus
Only available
in research
laboratories
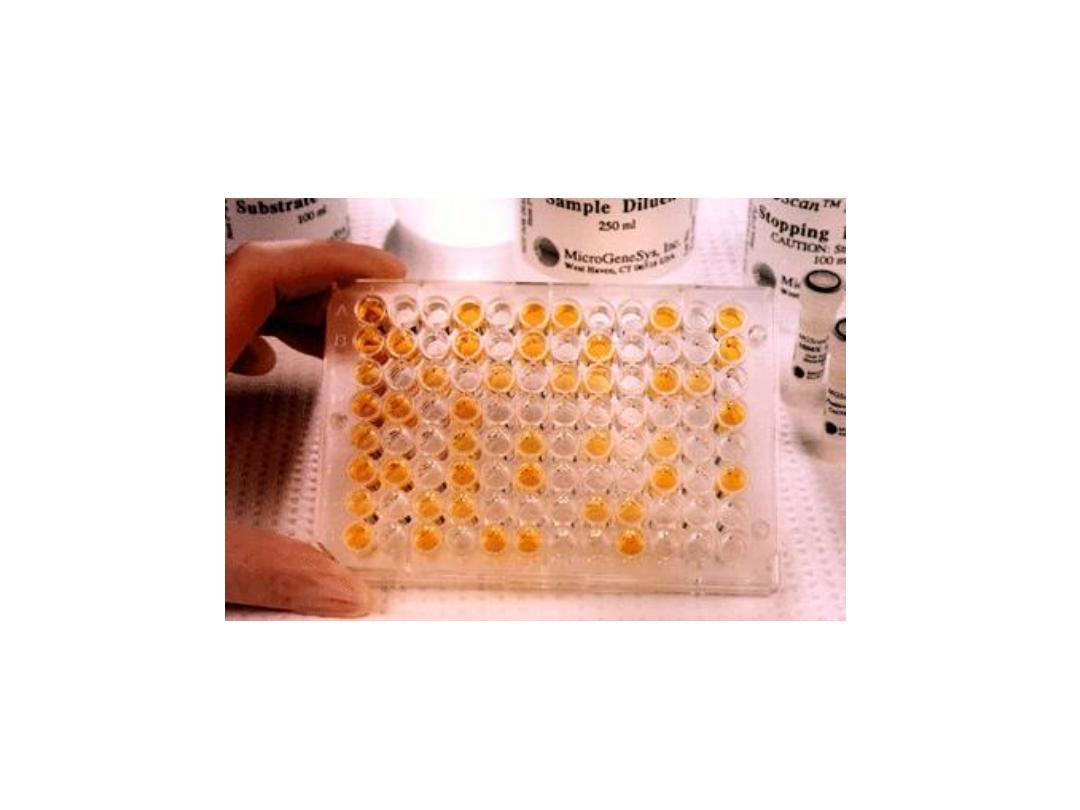
ELISA for HIV antibody
Microplate ELISA for HIV antibody: coloured wells
indicate reactivity

Prognostic tests
to monitor the patient for:
signs of disease
progression
and
response
to antiviral chemotherapy.
HIV viral load
- detect HIV-RNA e.g. RT-PCR (bad ˃10,000 copies)
HIV Antigen tests
serial CD4 counts
.
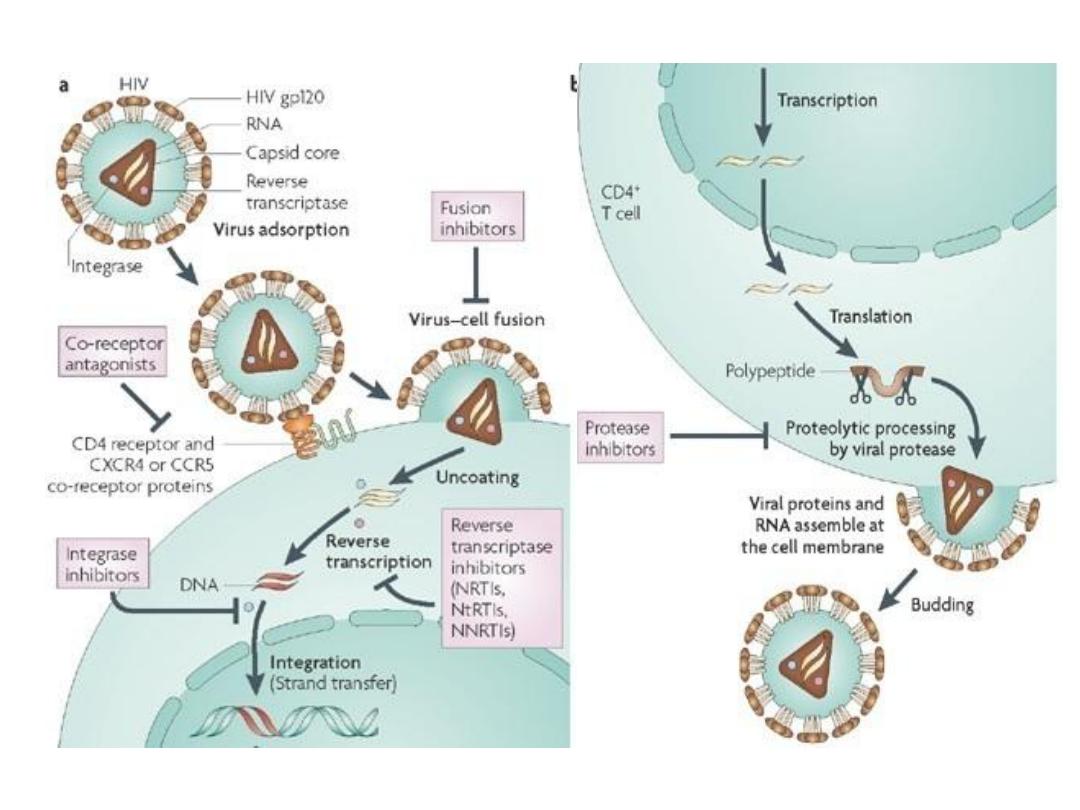
Antiretroviral Drugs Used in HAART
Class of Drug
Mechanism of Action
Name of Drug
Nucleoside or nucleotide
reverse transcriptase
inhibitors (NRTIs)
inhibit HIV reverse
transcriptase.This prevents
virus replication and
spread
zidovudine(AZT),
didanosine (DDI),
lamivudine (3TC)
Nonnucleoside reverse
transcriptase inhibitors
(NNRTIs)
=
Efavirenz (EFV),
nevirapine,
Protease inhibitors (PIs)
inhibit the retroviral
protease from cleaving the
viral proteins. slow the spread
of the virus to other
uninfected cells.
ritonavir,
indinavir
Fusion entry inhibitors
interferes with the viral gp41
and prevents fusion of HIV
with the host cell.
Enfuvirtide
CCR5 entry inhibitors
block binding of
the HIV virion to the surface of
the CD4 cells.
Maraviroc
HAART
H
ighly
A
ctive
A
nti-
R
etroviral
T
herapy
*
2
NRTI+
1
NNRTI
* *
1
or
2
PIs +
2
NRTIs
* * *
Triple
NRTI regimens
• Effective in
prolonging life
• Improving the
quality
of life
• Reduced
viral load
• Does
not cure
the chronic HIV(
latent
)
• Increased
CD4
cell
count
Attachment/
entry
Reverse
transcription
Integration
Maturation
Protease
inhibitors
Fusion
inhibitors
RT
inhibitors
Release
?
Neutralizing
antibodies
Integrase
inhibitors
Binding-
entry
inhibitors
HIV life cycle
Source Undetermined

Prevention methods
1.
safe-sex
practices (condom use),
2.blood donor
screening
in many countries
3.
safe use
of needles (no needle sharing), and
early screening for HIV infection.
4.
Circumcised
men are less likely to acquire HIV
infections
5.Treatment of HIV-1 infected
pregnant women
(
AZT
)
There is
no vaccine
currently available to
prevent HIV-1 infection or the progression
from HIV infection to AIDS.
vaccines types:
• Killed vaccine (not used)
• Live attenuated vaccine
• Synthetic peptide of env
• Subunite vaccine(env)
• Target cell protection(covering CD4)
• Gene therapy:genetically alter the target cell
make them resistant to HIV
