1
Dept.of Microbiology-Virology Dr. Shatha F Abdullah
Measles (Rubeola)
One of the most infectious childhood diseases known. Humans are the natural host. Caused
by measles v. typical paramyxovirus; envelope spikes containing H+ Fusion protein
(hemolysins) with no neuramindase activity.
In culture, produces characteristic intranuclear inclusion bodies and syncytial giant cells.
One serotype, protection after infection is lifelong.
Measles cases occur throughout the year in temperate climate. Epidemics tend to occur in
late winter and early spring.
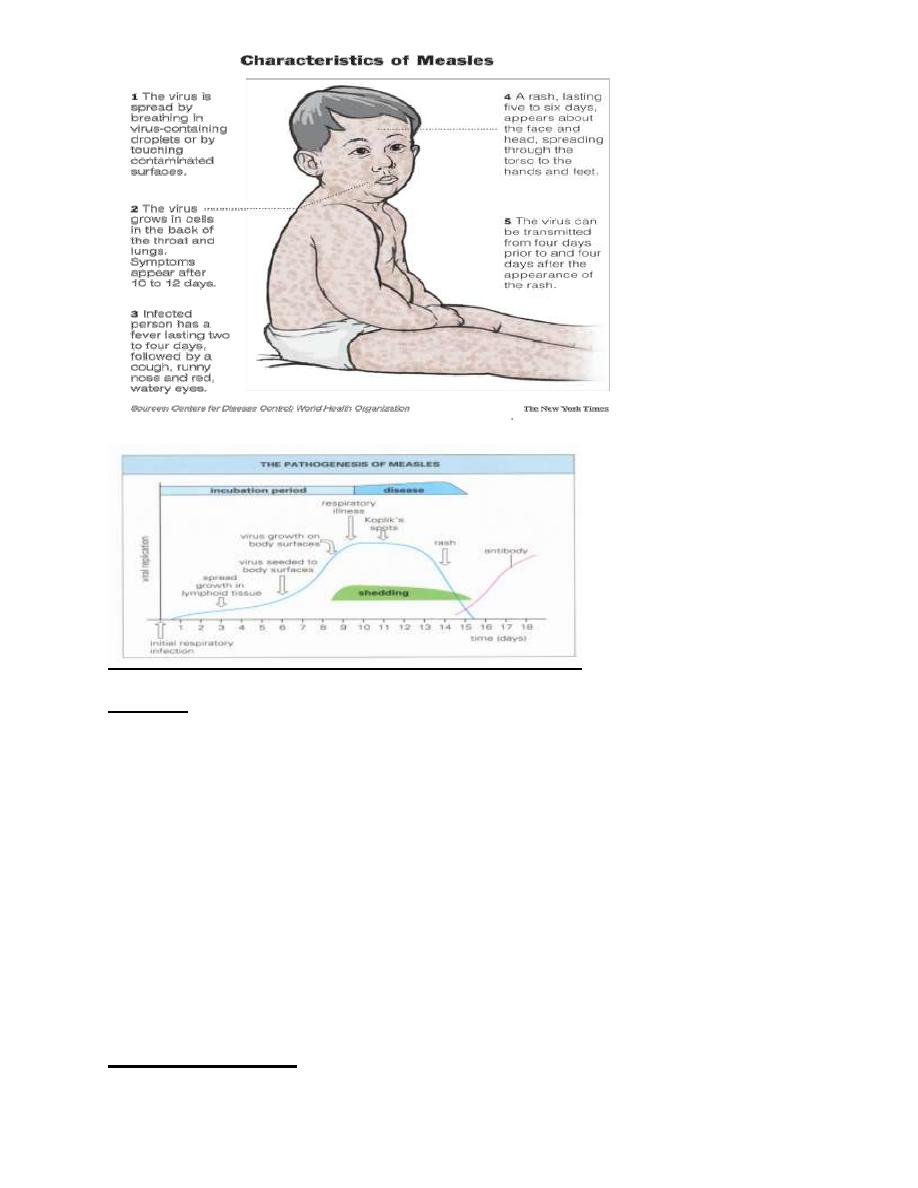
Transmission:
Measles virus transmitted through respiratory droplets but this virus can also infect via the
eye and multiply in the conjunctivae. Viremia following primary local multiplication results
in widespread distribution to many organs. Hematogenus transplacental transmission when
occur during pregnancy.
Pathogenesis & Immunity:
Virus infects URT cell lining where it multiplies locally, the infection the n spreads to the
regional lymphoid tissues &then multiply there (primary Viremia).
Secondary Viremia seeds the epithelial surfaces of the body including skin, respiratory tract,
conjunctiva where focal replication occurs. Virus replicates in certain lymphocytes which aid
in dissemination throughout the body.
Skin rash: due to *cytotoxic T cells attacking the measles virus-infected vascular endothelial
cells in the skin
**Antibody- mediated vasculitis( so that specific antibodies coincide with appearance of rash)
Virus shedding from infected person start 4days prior to and 4 days after the appearance of
rash.
Both neutralizing antibodies- IgG &cell mediated Immunity are involved during viremic
stage of measles.
Clinical findings:
1- Incubation period: 8-12 days may lasts up to3 wks in adults.
2- Prodromal phase: last for (2-4 days) this phase is characterized by high grade fever,
running nose, dry cough, sore throat, conjunctivitis (virus may be excreted during this
phase)in tears, nasal secretions, urine and blood.

2
3- Koplik's spots -raised bright red macules or ulcer with white centers on the buccal
mucosa opposite the lower molar (It’s a valuable diagnostic sign) and it appears 2 days
before the rash.
4- Eruption phase: (last for 5-8 days) a characteristic light pink, discrete maculopapules
that coalesce to form blotches, rash appear on face to the chest, the trunk and then
proceeds gradually down the limbs. Rash become brownish in 5-10 days.
The disease is more extensive in this stage with generalized virus infection in lymphoid
tissues and skin, it’s more severe in malnourished children, AIDS & TB.
Modified Measles: occur in partially immune persons,such as infant with residual
maternal anibodies. I.P is prolonged, diminished prodromal symptoms, koplik’s spots a re
usually absent and rash is mild.
Complications
1-bronchopneumonia (giant cell pneumonia,croup&bronchitis )
2- Otitis media (with or without secondary bacterial infections)
3- Conjunctivitis and corneal ulcer
4- Encephalitis ~1:1000 cases, 10% mortality rate,40% with permanent sequalae (deafness
&MR)
5-Subacute schlerosing pan encephalitis (SSPE) a rare late and fatal complication of measles
with incidence of about 1:300,000 cases occurs several years after measles, slow
viral(conventional) infection in which the virus multiplies in the brain, resulting in
neurodegenerative disease. It’s usually fatal within 1-3 years after onset.
There are a large amount of viral Ag within the inclusion bodies in infected brain cells,
there is no mature v. particle (v. lacks M protein).This is because the immune response
unable to deal with this viral infection due to immune modulation of the expressed viral
Ag on cell surface; or due to presence of defective virus particles. Patient with SSPE
exhibit high titers of measles Ab in CSF& serum with titer10-100 fold higher than those
seen in typical convalescent sera.
6-progressive measles inclusion body encephaltitis.
7-Measles in pregnant women resulting in stillbirth
3
8-Atypical measles following taken a killed vaccine, Occurs only in adult; infrequent
.
Diagnosis:
1- Clinical
2- Lab. Diagnosis:
a- Specimens: nasopharyngeal swab or washing, blood, conjunctival secretions, urine.
b- Cell culture isolation: Monkey or human kidney cells
CPE: multinucleated giant cells, intranuclear or intra cytoplasmic inclusion bodies.
Identification: IF or hemadsorption
c- Serology: ELISA,HI and Nt . IgM( appear 1-2 wks after the onset of rash =recent
infection) and IgG (4 fold rise in ab titer between acute and convalescent phase
indicate acute infection)
d- Ag and nucleic acid detection ;detection of viral RNA by using RT-PCR.
Treatment & Prevention

4
No antiviral drug, only supportive treatment; the use of vitamin A is useful to prevent blindness
due to measles.
Live attenuated vaccine, Trivalent live attenuated vaccine (MMR) usually given to 15 months
of age
Killed vaccines should not be used
Human Immunoglobulin given to modify the disease if given early in incubation period to
unimmunized pt., neonates and pregnant women.
Ribavirin; measles is susceptible in vitro to this drug with not proved clinical benefit.
Genus Henipavirus(zoonotic paramyxoviruses)
Two zoonotic paramyxoviruses were recognized in late 1990s with disease out breaks in
Australasia. Both are of public health conce rn because their high mortality, wide host range
&ability to jump species barrier and classified as Biosafty level 4 pathogen. Animal reservoir is
the fruit bat (flying fox).
1-Nipah virus: an out break of severe encephalitis was recognized in 250 cases in Malaysia
(1998-1999) with mortality rate more than 35%.
Few survivors had persistent neurological deficits and 10% with late onset encephalitis develop
months- years after initial attack.
Transmission of the disease: is through direct transmission from pig to humans.
2-Hendra virus: equine virus cause horse fatalities and few human deaths in Australia.
No available vaccine for both viruses.
Rubella (German measles)
3 days rash
Togavirus family
Composed of one piece of ss- RNA
Icosahedral nucleocapsid
Lipoprotein envelope,H-spikes
+ve strand RNA(- ve virion polymerase)
Single antigenic type
Humans are the natural host
5
Transmission
Respiratory droplets
Transplacental
Pathogenesis
Initial replication occurs in RT.: Nasopharanx & cervical L.N then after 5-7 days virus spreads
via bl. to internal organs &skin
Skin Rash: due to Ab-Ag mediated vasculitis
Rubella v. Infections confer Lifelong immunity
Clinical Findings
Rubella(post natal rubella)
I.P:12 days or longer
Prodromal period: fever& malaise at the same time Morbilliform rash start on the face then
down to extremities (lasts 3 days)
Post auricular lymphadeopathy is characteristic
Poly arthritis (due to immune complex deposit)
Lab. Diagnosis:
Clinical diagnosis is unreliable because many viral infections share the same clinical features.
Specimens: nasopharangeal swab, throat swab 3days after symptoms appear
Cell culture: Monkey kidney or baby hamster
Identification: IF or Nt
Serology: specific IgM detection using ELISA,IF, HAI &CFT
Congenital rubella syndrome
Maternal Viremia associated with rubella infection during pregnancy may result in infection of
the placenta and fetus.
*Teratogenic virus; 25% of infections are subclinical.
* Rubella infection of non- immune women during 1
st
trimester (transplacental transmission)
leads to the following consequences:
6
1- Fetal loss: Abortion, intra uterine death or still birth. If s urvive, fetus might have
2- Transient effects: growth retardation, failure to thrive,HSM,TCP, osteitis &
meningoencephalitis
3- Permanent manifestations : Congenital malformations from maternal viremia and fetal
infection are recognized at birth or during 1
st
year of life ; baby may born with:
Heart : patent ductus arteriosus
Eye: cataract, total or partial blindness
Brain: deafness &mental retardation
4- Developmental abnormalities: become obvious during childhood (pre-school-school
age) & adolescence including mental retardation, psychiatric disorders& abnormal
behavioral manifestations.
Asymptomatic baby; may shed virus for many months
Lab. Diagnosis:
Newborn infant: *IgM in cord blood= CRS
*Isolation of v. in pharyngeal secretions& other body fluids (CSF, urine,
rectal swab)
Pregnant: IgM indicate recent infection
4 –fold rise in ab titer between acute and convalescent-phase in HA & ELISA tests
1:8 or greater IgG titer=immunity & protection to fetus
Treatment & Prevention
No antiviral therapy
Live attenuated vaccine: induces respiratory IgA
- Measles Mumps Rubella vaccine (MMR) : given to
- Boys and girls at age *13-15 months
**4-5 years before school entry
-Girls aged 10-14 yrs.
Non-immunized women: sero-ve, not pregnant & should be warned to not to be pregnant at
least 3- months after vaccination.
Immune serum globulin (IG) = 1
st
trimester pregnant women, does not protect fetus but can
decrease disease severity.

7
Termination of pregnancy if sure?!
