BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
1
MYCOBACTERIA
Mycobacterium tuberculosis
Morphology and identification
A. Typical organisms: In tissue, tubercle bacilli are thin straight rods with variable
morphology from one species to another.
Mycobacteria cannot be classified as gram +ve or -ve.
They are characterized by 'acid-fastness i.e. 'acid-alcohol' quickly decolorizes
all bacteria except the mycobacteria, acid- fastness depends on the integrity of
the waxy envelope .The Ziehl-Neelsen technique of staining is employed for
identification of acid-fast bacteria.
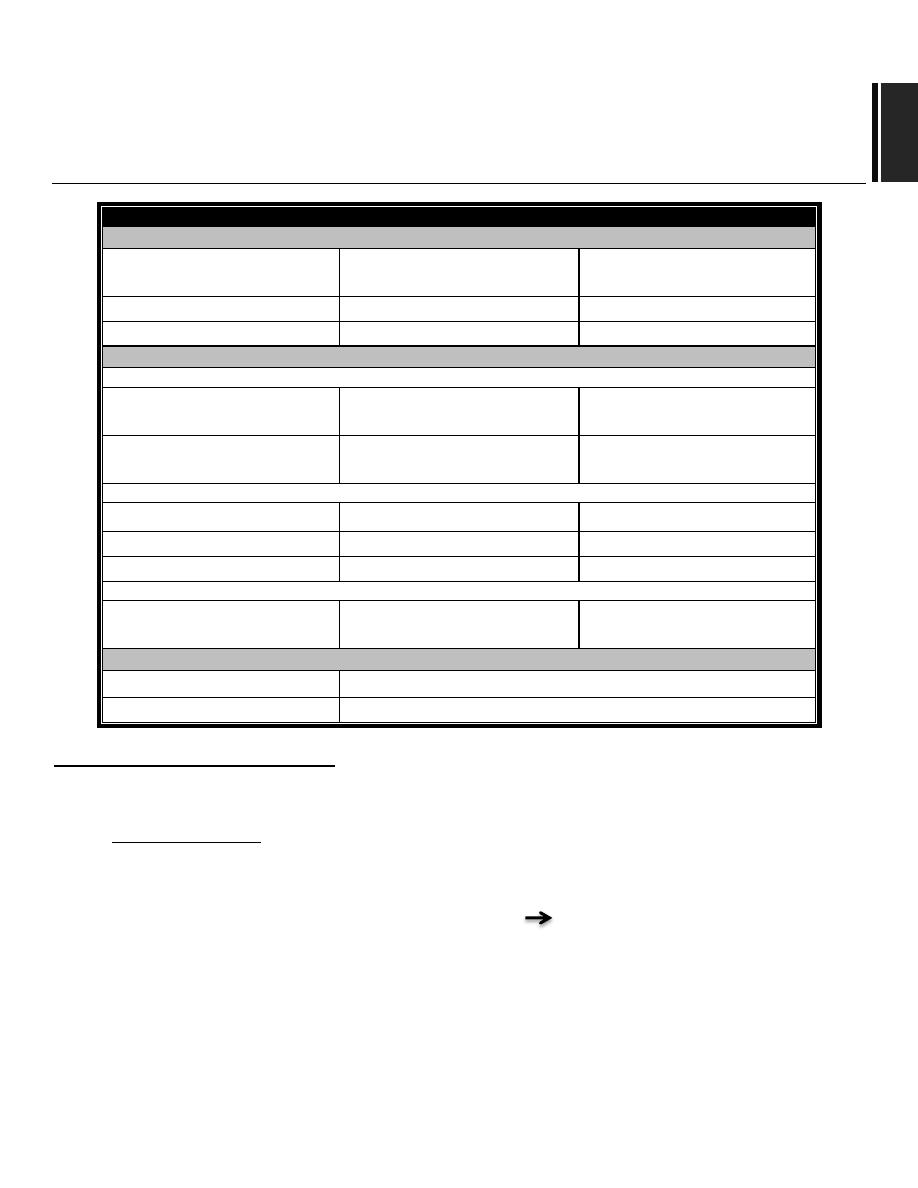
SPP.
RESERVOIR
CLINICAL MANIFESTATION
Pathogenes
M.tuberculosis
Human
Pulmonary and dissem.
T.B.
M.leprae
Human
leprosy
M.bovis
Human & cattle
T.B. like infection
Potentially pathogenic ( atypical mycobacteria)
…Moderately common
M.avium complex
Soil ,water , birds ,fowl
environment
Dissem.& pulmonary T.B.
(infects birds)
M.kansasii
Water, Soil
Pulmonary inf. Similar to
T.B.
…Uncommon
M.marinum
Fish
Subcutaneous nodules
× M.scorfulaceum
Soil ,water
Cervical lymphadenitis
× M.ulcerans
Human ,environment
Subcutaneous nodules
…Rapid growth
× M.fortuitum
× M.chlonei
Soil ,water
Cutaneous lesions
Non pathogenic
M.phlei
Enviroonment
M.smegmatous
Normal flora in sebaceous glands
BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
2
B. Culture: There are three general formulations that can be used for both the nonselective
and the selective media:-
1) Semi-synthetic agar media (eg, Middlebrook 7H10 and 7H11) contain salts,
vitamins cofactors, oleic acid, albumin, catalase, glycerol, glucose, and malachite
green. Large inocula yield growth on these media in several weeks. These media
may be less sensitive than other media for primary isolation of mycobacteria.
2) Inspissated egg media (eg, Lowenstein-Jensen) contain salts, glycerol, and complex
organic substances (eg, fresh eggs, egg yolks, potato flour, and other
ingredients).Malachite green is included to inhibit other bacteria. Small inocula in
specimens from patients will grow on these media in 3-6 weeks. These media with
added antibiotics are used as selective media.
3) Broth media: broth media (eg, Middlebrook 7H9 and 7H12) support the
proliferation of small inocula. Mycobacteria grow in clumps or masses because of
the hydrophobic character of the cell surface, and added antibiotics.
C. Growth characteristics:
1) Mycobacteria are obligate aerobes.
2) Increased Co
2
tension enhances growth.
3) Biochemical activities are not characteristics, and the growth rate is much slower
than that of most bacteria.
4) Saprophytic forms tend to grow more rapidly, to proliferate well at 22-33
c
C. To
produce more pigment, and to be less acid-fast than pathogenic forms.
D. reaction to physical and chemical agent:
Mycobacteria tend to be more resistant to chemical agents than other bacteria
because of the hydrophobic nature of the cell surface and their clumped growth.
Dyes (malachite green)or antibacterial agents (eg, penicillin)that are
bacteriostatic to other bacteria can be incorporated into media without inhibiting
the growth of tubercle bacilli.
Acids and alkalies permit the survival of some tubercle bacilli and are used to help
eliminate contaminating organisms and for 'concentration' of clinical specimens.
Tubercle bacilli are resistant to drying and survive for long periods in dried
sputum.
E. Variation.
F. Pathogenicity of Mycobacteria:
Humans and guinea pigs are highly susceptible to
M.tuberculosis
infection,
whereas fowl and cattle are resistant.

BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
3
M.tuberculosis
and
M bovis
are equally pathogenic for humans. The route of
infection (respiratory versus intestinal determines the pattern of lesions.
Some 'atypical'
mycobacteria (eg,
Mycobacterium kansasii
)
produce human disease
indistinguishable from tuberculosis, other (eg,
M.fortuitum
)
cause only surface
lesion and or act as opportunists.
Constituents of tubercle Bacilli
The constituents listed below are found mainly in cell walls. Mycobacterial cell walls can induce
delayed hypersensitivity and some resistance to infection and can replace whole mycobacterial
cells
in
Freund's adjuvant.
A. Lipid : Mycobacteria are rich in lipids. These include mycolic acids, waxes, and phosphatides.
The lipids are largely bound to proteins and polysaccharides. Lipids are to some extent
responsible for acid fastness.
Virulent strains of tubercle bacilli form microscopic "serpentine cords" in which acid-fast bacilli
are arranged in parallel chains. Cord formation is correlated with virulence. A "cord factor"
inhibits migration of leukocytes, causes chronic granulomas, and can serve as an immunologic
"adjuvant".
B. Proteins: They elicit the tuberculin reaction. They can also elicit the formation of variety of
antibodies.
C. Polysaccharides: They can induce the immediate type of hypersensitivity and can serve as
antigens in reactions with sera of infected persons.
Pathogenesis
Mycobacteria in droplets are inhaled and reach the alveoli. The disease results from
establishment and proliferation of virulent organisms and interactions with the host. Resistance
and hypersensitivity of the host greatly influence the development of the disease.
BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
4
Pathology
The production and development of lesions and their healing or progression are determined
chiefly by:
1- The number of mycobacteria in the inoculum and their subsequent multiplication.
2- The resistance and hypersensitivity of the host.
A. Two principal lesions:
1. Exudative type
this consists of an acute inflammatory reaction, with edema fluid,
polymorphonuclear leukocytes, and, later, monocytes around the tubercle bacilli. This type is
seen particularly in lung tissue. It may heal; it may lead to massive necrosis of tissue; or it may
develop into the second (productive) type of lesion. During the exudative phase, the tuberculin
test becomes positive.
2. Productive type
when fully developed it consists of three zones:
(1) a central area of large, giant cells containing tubercle bacilli;
(2) a mid-zone of pale epithelioid cells;
(3) a peripheral zone of fibroblasts, lymphocytes, and monocytes. Later the central area
undergoes caseation necrosis. Such a lesion is called a tubercle. It may break into a bronchus,
empty its contents there, and form a cavity. It may subsequently heal by fibrosis or calcification.
B.Spread of Organisms in the Host:
By direct extension through the lymphatic channels and bloodstream, and via the bronchi and
gastrointestinal tract. The bloodstream distributes bacilli to all organs (miliary distribution). If a
caseating lesion discharges its contents into a bronchus, they are aspirated and distributed to
other parts of the lungs or are swallowed and passed into the stomach and intestines.
C.Intracellular Sites of Growth:
Mycobacteria establish themselves in tissue; intracellularly in monocytes, reticuloendothelial
cells, and giant cells. That makes chemotherapy difficult and favors microbial persistence. Within
the cells of immune animals, multiplication of tubercle bacilli is greatly inhibited.
BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
5
PRIMARY INFECTION & REACTION
When a host has first contact with tubercle bacilli ,the following features are observed:
a. An acute exudative lesion develops and rapidly spreads to the lymphatics and
regional lymph nodes.
b. The lymph node undergoes massive caseation.
c. The tuberculin test becomes positive.
In primary infection, the involvement may be in any part of the lung but is most often at the
base.
The reactivation type is caused by tubercle bacilli that have survived the primary lesion.
Reactivation tuberculosis is characterized by :
a. Chronic tissue lesions.
b. Regional lymph nodes are only slightly involved. (Ghon complex).
The reactivation type almost always begins at the apex of the lung where oxygen tension (Po2)
is highest.
These differences between primary infection and reinfection or reactivation are attributed to:
1) Resistance
2) hypersensitivity induced by the first infection of the host with tubercle bacilli "Koch's
phenomena".
Immunity and Hypersensitivity
1) Development of cellular immunity during the initial infection.
2) Antibodies form against a variety of the cellular constituents of the tubercle bacilli
3) In the course of primary infection, the host develops hypersensitivity to the
tubercle bacilli.
4) This is made evident by the development of a positive tuberculin reaction.
Tuberculin Test
A-Material:
Old tuberculin is a concentrated filtrate of broth in which tubercle bacilli have grown for 6
weeks.
A Purified protein derivative ( P P D ) is obtained
It's standardized by TU "Tuberculin Units".

BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
6
Doses
5T U, 250TU according to strength required.
B. Reactions to Tuberculin:
In an individual who has not had contact with mycobacteria, there's no reaction.
An individual who has had a primary infection with tubercle bacilli develops induration,
edema, and erythema in 24-48 hours.
The skin test should be read 48 or 72 hours.
Induration 10mm or more in diameter.
Positive tests tend to persist for several days.
The tuberculin test becomes positive within 4-6 weeks after infection.
It may be negative in the presence of tuberculous infection when "anergy" develops
due to:
1) Overwhelming tuberculosis.
2) Measles
2) Hodgkin
’
s disease
3) Sarcoidosis
4) AIDS
5) Immunosuppression.
After BCG vaccination, a positive test may last for only3-7 years.
C. Interpretation of Tuberculin test
A positive tuberculin test indicates that an individual has been infected in the past or
continue to carry viable mycobacteria in some tissues. It does not imply that active disease or
immunity to disease is present .tuberculin- positive persons are at risk of developing disease
from reactivation of the primary infection
Diagnostic laboratory tests
A positive tuberculin test does not prove the presence of active disease due to tubercle bacilli.
Isolation of tubercle bacilli provides such proof:
A.Specimens: consist of fresh sputum, gastric washings, urine, pleural fluid, C5F, joint fluid,
biopsy material, blood, or other suspected material.
B.Decontamination and Concentration of Specimens:
Specimens from sputum with NaOH, neutralized with buffer, and concentrated by centrifugation
Used for acid-fast stains and for culture.
C. Smears:
• Examined for acid-fast bacilli by Ziehl-Neelsen staining.
BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
7
Fluorescence microscopy with auramine-rhodamine stain is more sensitive than acid-fast
stain.
D. Culture, Identification, and Susceptibility Testing:
A selective agar media (eg, Lowenstein-Jensen or middlebrook 7H10/7H11).
Incubation is at 37°C in 5-10% C0
2
for up to 8 weeks.
It is medically important to characterize and separate
M.tuberculosis
from all other
species of mycobacteria.
Conventional methods for identification of mycobacteria include observation of
rate of growth, colony morphology, pigmentation, and biochemical profiles.
Growth rate separates the rapid growers <7 days, from other mycobacteria.
Molecular probes provide a rapid, sensitive, and specific method for identification
of mycobacteria.
E. Antigen Detection, serology and anti-gene detection (PCR)
The polymerase chain reaction holds great promise for the rapid and direct detection of
M.
tuberculosis
in clinical specimens- the PCR test is approved for this use.
Prevention & Control
1-Prompt and effective treatment of patients with active tuberculosis
2-Drug treatment of asymptomatic tuberculin-positive persons (eg, children)-receive
immunosuppressive drugs.
3- Nonspecific factors may reduce host resistance include starvation, gastrectomy, and
suppression of cellular immunity by drugs.
4- Immunization: Various living avirulent tubercle bacilli, particularly BCG (Bacillus
Calmette-Guerinan attenuated bovine organism). Vaccination is a substitute for
primary infection with virulent tubercle bacilli without the danger inherent in the latter
given to children.
5- The eradication of tuberculosis in cattle and the pasteurization of milk have greatly
reduced
M bovis
infections.

BACTERIOLOGY::MYCOBACTERIA::Dr. Nidhal Sabry DONE BY: MAM GROUP2011
Page number
8
