Lec.1&2
IMMUNITY TO INFECTION
الاستاذة المساعدة : د وفاق محمود الوتار
_ Viral Infections
_ Bacterial Infections
_ Fungal infections
_ Protozoan Diseases & diseases Caused by Parasitic Worms (Helminthes)
_ Emerging Infectious Diseases
One of the first and most important features of host innate immunity is the barrier provided by the epithelial surfaces of the skin and the lining of the gut. The difficulty of penetrating these epithelial barriers ensures that most pathogens never gain productive entry into the host. In addition to providing
a physical barrier to infection, the epithelia also produce chemicals that are useful in preventing infection. The secretion of gastric enzymes by specialized epithelial cells lowers the pH of the stomach and upper gastrointestinal tract, and other specialized cells in the gut produce antibacterial peptides.
A major feature of innate immunity is the presence of the normal gut flora, which can competitively inhibit the binding of pathogens to gut epithelial cells. Innate responses can also block the establishment of infection. For example, the cell walls of some gram-positive bacteria contain a peptidogly can that activates the alternative complement pathway,resulting in the generation of C3b, which opsonizes bacteria and enhances phagocytosis. Some bacteria produce endotoxins such as LPS, which stimulate the production of cytokines such as TNF-_, IL-1, and IL-6 by macrophages or endothelial cells. These cytokines can activate macrophages. Phagocytosis of bacteria by macrophages and other phagocytic cells is another highly effective line of innate defense. However, some types of bacteria that commonly grow intracellularly have developed mechanisms that allow them to resist degradation within the phagocyte.
Viruses are well known for the stimulation of innate responses. In particular, many viruses induce the production of interferons, which can inhibit viral replication by inducing an antiviral response. Viruses are also controlled by NK cells. NK cells frequently form the first line of defense against viral infections. Generally, pathogens use a variety of strategies to escape destruction by the adaptive immune system. Many pathogens
reduce their own antigenicity either by growing within host cells, where they are sequestered from immune attack,or by shedding their membrane antigens. Other pathogens camouflage themselves by mimicking the surfaces of host cells, either by expressing molecules with amino acid sequences similar to those of host cell-membrane molecules or by acquiring a covering of host membrane molecules. Some pathogens are able to suppress the immune response selectively or to regulate it so that a branch of the immune system is activated that is ineffective against the pathogen. Continual variation in surface antigens is another strategy that enables a pathogen to elude the immune system. This antigenic variation may be due to the gradual accumulation of mutations, or it may involve an abrupt change in surface antigens.
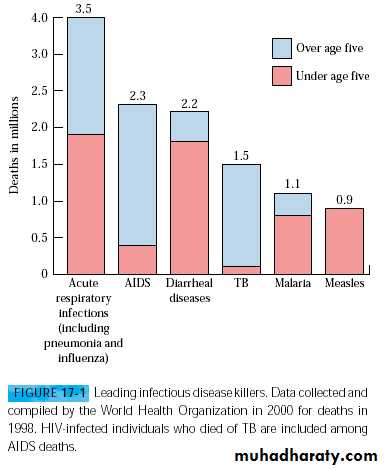
Both innate and adaptive immune responses to pathogens provide critical defense, but infectious diseases, which have plagued human populations throughout history, still cause the death of millions each year. Although widespread use of vaccines and drug therapy has drastically reduce mortality from infectious diseases in developed countries, such diseases continue to be the leading cause of death in the Third World. It is estimated that over 1 billion people are infected worldwide, resulting in more than 11 million deaths every year (Figure 17-1). some of these diseases are beginning to emerge or re-emerge in developed countries. For
example, some United States troops returned from the Persian
Gulf with leishmaniasis; cholera cases have recentlyincreased worldwide, with more than 100,000 cases reported in KwaZulu-Natal, South Africa, during the summer of 2001; and a new drug-resistant strain of Mycobacterium tuberculosis is spreading at an alarming rate in the United States. The selected infectious diseases caused by viruses, bacteria, protozoa, and helminthes ,the four main types of pathogens.
Viral Infections
A number of specific immune effectors mechanisms, together with nonspecific defense mechanisms, are called into play to eliminate an infecting virus (Table 17-1). At the same time, the virus acts to subvert one or more of these mechanisms to prolong its own survival. The outcome of the infection depends on how effectively the host’s defensive mechanism resist the virus.The innate immune response to viral infection is primarily through the induction of type I interferons (IFN-alpha_ and IFN-beta_) and the activation of NK cells. Double stranded RNA (dsRNA) produced during the viral life cycle can induce the expression of IFN-alpha _ and IFN-beta_ by the infected cell. Macrophages, monocytes, and fibroblasts also are capable of synthesizing these cytokines, but the mechanisms that induce the production of type I interferons in these cells are not completely understood. IFN-alpha_ and IFN-beta_ can induce an antiviral response or resistance to viral replication by bindingto the receptor leading to inhibition of viral replication. The binding of IFNs to NK cells induces lytic activity,making them very effective in killing virally infected cells. The activity of NK cells is also greatly enhanced by IL-12, a cytokine that is produced very early in a response to viral infection.
HUMORAL IMMUNE RESPONSE
Many Viruses are Neutralized by Antibodies ,antibodies specific for viral surface antigens are often crucial in containing the spread of a virus during acute infection and in protecting against reinfection. Antibodies are particularly effective in protecting against infection if they are localized at the site of viral entry into the body. Most viruses express surface receptor molecules that enable them to initiate infection by binding to specific host-cell membrane molecules. For example, influenza virus binds to sialic acid residues in cell membrane glycoproteins and glycolipids; rhinovirus binds to intercellular adhesion molecules (ICAMs); and Epstein-Barr virus binds to type 2 complement receptors on B cells. If antibody to the viral receptor is produced, it can block infection altogether by preventing the binding of viral particles to host cells. Secretory IgA in mucous secretions plays an important role in host defense against viruses by blocking viral attachment to mucosal epithelial cells. The advantage of the attenuated شلل الاطفالoral polio vaccine, is that it induces production of secretory IgA, which effectively blocks attachment of poliovirus along the gastrointestinal tract. Viral neutralization by antibody sometimes involves mechanisms that operate after viral attachment to host cells. also complement can agglutinate viral particles and function as an opsonizing agent to facilitate Fc- or C3b-receptor–mediated phagocytosis of the viral particles.
Cell-Mediated Immunity is Important for Viral Control and Clearance
although antibodies have an important role in containing the spread of a virus in the acute phases of infection, they are not usually able to eliminate the virus once infection has occurred—particularly if the virus is capable of entering a latent state in which its DNA is integrated into host chromosomal DNA. Once an infection is established, cell-mediated immune mechanisms are most important in host defense. Ingeneral,CD8+ TC cells and CD4+ TH1 cells are the main components of cell-mediated antiviral defense, although in some cases CD4+ TC cells have also been implicated .Activated TH1 cells produce a number of cytokines, including IL-2, IFN-a and TNF-b, that defend against viruses either directly or indirectly .IFN-gamma acts directly by inducing an antiviral state in cells. IL-2 acts indirectly by assisting in the recruitment of C TL precursors into an effector population. Both IL-2 and
IFN-gamma activate NK cells, which play an important role in host defense during the first days of many viral infections until a specific CTL response develops. In most viral infections, specific CTL activity arises within
3–4 days after infection, peaks by 7–10 days, and then declines. Within 7–10 days of primary infection, most virions have been eliminated; The viral specificity of the CTL as well can be demonstrated with IFN-α/β receptor.
How the Viruses Can Evade Host Defense Mechanisms
Despite their restricted genome size, a number of viruses have been found to encode proteins that interfere at various levels with specific or nonspecific host defenses. Presumably ,the advantage of such proteins is that they enable viruses to replicate more effectively amidst host antiviral defenses. As described above, the induction of IFN-α/β is a major innate defense against viral infection, but some viruses have developed strategies to evade the action of both. These include hepatitis C virus, which has been shown to:
overcome the antiviral effect of the interferons .Another mechanism for evading host responses, utilized in particular by herpes simplex viruses (HSV) is inhibition of antigen presentation by infected host cell by HSV-1 orHSV-2 thus preventing presentation of viral antigen to CD8+ T cells. This results in the trapping of empty class I MHC molecules in the endoplasmic reticulum and effectively shuts down a CD8+ T-cell response to HSV-infected cells.
The targeting of MHC molecules is not unique to HSV .Other viruses have been shown to down-regulate class I MHC expression shortly after infection. Two of the best characterized examples, the adenoviruses and cytomegalovirus(CMV), use distinct molecular mechanisms to reduce the surface expression of class I MHC molecules, again inhibiting antigen presentation to CD8+ T cells. Some viruses—CMV, measles virus, and HIV
Antibody-mediated destruction of viruses requires complement activation, resulting either in direct lysis of the viral particle or opsonization and elimination of the virus by phagocytic cells. A number of viruses have strategies for evading complement-mediated destruction. Vaccinia virus, for
example, secretes a protein that binds to the C4b complement component, inhibiting the classical complement pathway; and herpes simplex viruses have a glycoprotein component that binds to the C3b complement component, inhibiting both the classical and alternative pathways. can have the same effect as an antigenic shift that generates anew subtype. protection against influenza, but its specificity is strain-specific and is readily bypassed by antigenic shift&drift is responsible for our inabilityto produce an effective vaccine for colds. Now here is antigenic variation greater than in the human immunodeficiency virus (HIV), the causative agent of AIDS. Estimates suggest that HIV accumulates mutations at a rate 65 times faster than does influenza virus. .
Bacterial Infections
Immunity to bacterial infections is achieved by means of antibody unless the bacterium is capable of intracellular growth, in which case delayed-type hypersensitivity has an important role. Bacteria enter the body either through a number of natural routes (e.g., the respiratory tract, the gastrointestinal tract, and the genitourinary tract) or through normally inaccessible routes opened up by breaks in mucous membranes or skin. Depending on the number of organisms.specific immune response.Immune Responses to Extracellular
and Intracellular Bacteria
different levels of host defense are enlisted. If the inoculum size and the virulence are both low, then localized tissue phagocytes may be able to eliminate the bacteria with an innate, nonspecific defense. Larger inoculums or organisms with greater virulence tend to induce an adaptive, specific immune response.Immune Responses to extracellular and Intracellular Bacteria Can Differ
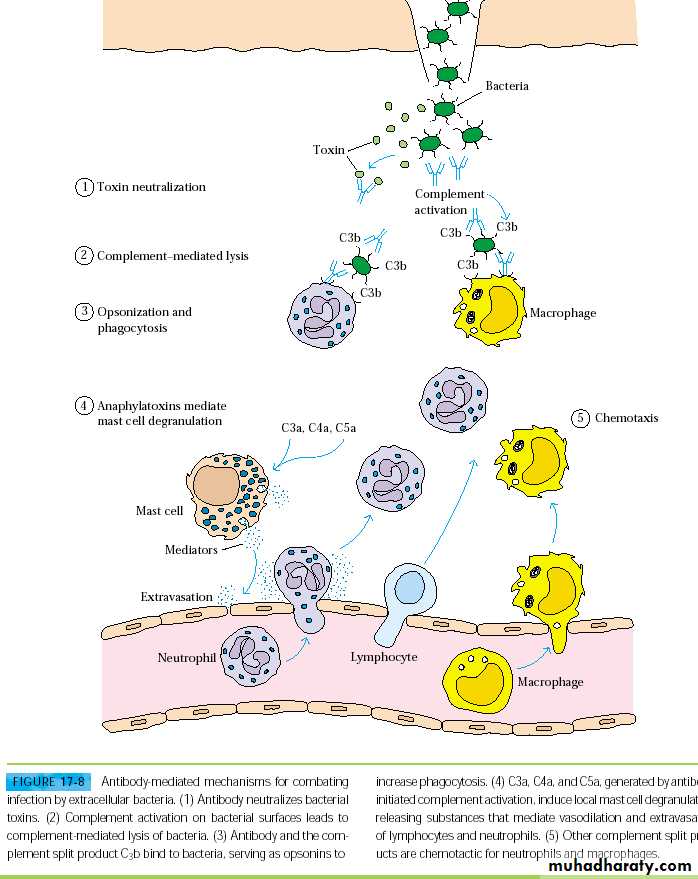
Infection by extracellular bacteria induces production of humoral antibodies, which are ordinarily secreted by plasma cells in regional lymph nodes and the submucosa of the respiratory and gastrointestinal tracts. The humoral immune response is the main protective response against extracellular bacteria. The antibodies act in several ways to protect the host from the invading organisms, including removal of the bacteria and inactivation of bacterial toxins (Figure 17-8).
Extracellular bacteria can be pathogenic because they induce a localized inflammatory response or because they produce toxins. The toxins, endotoxin or exotoxin, can be cytotoxic but also may cause pathogenesis in other ways. An excellent example of this is the toxin produced by diphtheria, which exerts a toxic effect on the cell by blocking protein synthesis.
Endotoxins, such as lipopolysaccharides (LPS), are generally components of bacterial cell walls, while exotoxins, such as diphtheria toxin, are secreted by the bacteria.
Antibody that binds to accessible antigens on the surface of a bacterium can, together with the C3b component of complement, act as an opsonin that increases phagocytosis and thus clearance of the bacterium (see Figure 17-8). In the case of some bacteria—notably, the gram-negative organism complement activation can lead directly to lysis of the organism. Antibody-mediated activation of the complement system can also induce localized production of immune effector molecules that help to develop an amplified and more effective inflammatory response. For example, the complement split products C3a, C4a, and C5a act as anaphylatoxins, inducing local mast-cell degranulation and thus vasodilation and the extravasation of lymphocytes and neutrophils from the blood into tissue space (see Figure 17-8).
Other complement split products serve as chemotactic factors for neutrophils and macrophages, thereby contributing to the buildup of phagocytic cells at the site of infection.Antibody to a bacteria toxin may bind to the toxin and neutralize it; the antibody-toxin complexes are then cleared by phagocytic cells in the same manner as any other antigen-antibody complex.
While innate immunity is not very effective against intracellular bacterial pathogens, intracellular bacteria can activate NK cells, which, in turn, provide an early defense against these bacteria. Intracellular bacterial infections tend to induce a cell-mediated immune response, specifically, delayed type hypersensitivity. In this response, cytokines secreted by
CD4+ T cells are important—notably IFN-gamma, which activates macrophages to kill ingested pathogens more effectively .
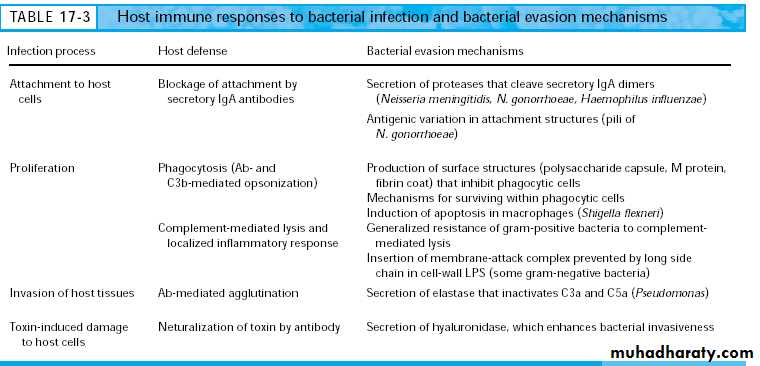
Bacteria Can Effectively Evade Host Defense Mechanisms
There are four primary steps in bacterial infection:
_ Attachment to host cells
_ Proliferation
_ Invasion of host tissue
_ Toxin-induced damage to host cells
Host-defense mechanisms act at each of these steps, and many bacteria have evolved ways to circumvent some of these host defenses. Some bacteria have surface structures or molecules that enhance their ability to attach to host cells. A number of gram-negative bacteria, for instance, have pili (long hair like projections), which enable them to attach to the membrane of the intestinal or genitourinary tract .
Other bacteria, such as Bordetella pertussis, secrete adhesion molecules that attach to both the bacterium and the ciliated epithelial cells of the upper respiratory tract. Secretory IgA antibodies specific for such bacterial structures can block bacterial attachment to mucosal epithelial cells and are the main host defense against bacterial attachment.
However, some bacteria (e.g., Neisseria gonorrhoeae,Haemophilus influenzae, and Neisseria meningitidis) evade the IgA response by secreting proteases that cleave secretory IgA at the hinge region; the resulting Fab and Fc fragments have a shortened half-life in mucous secretions and are not able to agglutinate microorganisms.
Some bacteria evade the IgA response of the host bychanging these surface antigens. In N. gonorrhoeae, for example, pilin, the protein component of the pili, has a highly variable structure ,the continual changes in the pilin sequence allow the organism to evade neutralizationby IgA.
Some bacteria possess surface structures that serve to inhibit phagocytosis. A classic example is Streptococcus pneumoniae, whose polysaccharide capsule prevents phagocytosis very effectively.
Other bacteria, such as Streptococcus pyogenes, a surface protein projection
called the M protein inhibits phagocytosis. Some pathogenic staphylococci are able to assemble a protective coat from host proteins. These bacteria secrete a coagulase enzyme that precipitates a fibrin coat around them, shielding them from phagocytic cells.Mechanisms for interfering with the complement system help other bacteria survive. In some gram-negative bacteria, resist complement mediated lysis. Pseudomonas secretes an enzyme, elastase, that inactivates both the C3a and C5a anaphylatoxins, thereby diminishing the localized inflammatory reaction.
A number of bacteria escape host defense mechanisms by their ability to survive within phagocytic cells. Some, such as Listeria monocytogenes, do this by escaping from the phagolysosome to the cytoplasm ,which is a more favorable environment for their growth. Other bacteria, such as Mycobacterium avium, block lysosomal fusion with the phagolysosome; and some mycobacteria are resistant to the oxidative attack that takes place within the phagolysosome.
Immune Responses Can Contribute to Bacterial Pathogenesis
In some cases, disease is caused not by the bacterial pathogen itself but by the immune response to the pathogen, pathogen-stimulated overproduction of cytokines leads to the symptoms of bacterial septic shock, food poisoning, and toxic-shock syndrome. For instance,cell-wall endotoxins of some gram-negative bacteria activate macrophages, resulting in release of high levels of IL-1 and TNF-, which can cause septic shock. In staphylococcal food poisoning and toxic-shock syndrome, exotoxins produced by the pathogens function as super antigens, which can activate all T cells that express T-cell receptors with a particular v- domain. The resulting overproduction of cytokines by activated TH cells causes many of the symptoms of these diseases.
The ability of some bacteria to survive intracellularly within infected cells can result in chronic antigenic activation of CD4+ T cells, leading to tissue destruction by a cell-mediated response with the characteristics of a delayed-type hypersensitivity reaction
Cytokines secreted by these activated CD4+ T cells can lead to extensive accumulation and activation of macrophages, resulting in formation of agranuloma. The localized concentrations of lysosomal enzymes in these granulomas can cause extensive tissue necrosis.
Much of the tissue damage seen with M. tuberculosis is due to a cell-mediated immune response.
Diphtheria (Corynebacterium diphtheriae) may be controlled by Immunization with Inactivated toxoid .Diphtheria is the classic example of a bacterial disease caused by a secreted exotoxin to which immunity can be induced by immunization with an inactivated toxoid.
The virulence of the organism is due completely to its potent exotoxin. The toxin causes destruction of the underlying tissue, resulting in the formation of a tough fibrinous membrane (“pseudomembrane”) composed of fibrin, white blood cells, and dead respiratory epithelial cells. The membrane itself can cause suffocation. The exotoxin also is responsible for widespread systemic manifestations. Pronounced myocardial damage and neurologic damage (ranging from mild weakness to complete paralysis) are common.
Tuberculosis (Mycobacterium tuberculosis) Is Primarily Controlled by CD4+ T Cells Tuberculosis is the leading cause of death in the world from a single infectious agent, killing about 3 million individuals every year ,roughly one-third of the world’s population, are infected with the causative agent M. tuberculosis and are at risk of developing the disease. Long thought to have been eliminated as a
Protozoan Diseases
Protozoans are unicellular eukaryotic organisms. They are responsible for several serious diseases in humans, including amoebiasis, Chagas’ disease, African sleeping sickness, malaria, leishmaniasis, and toxoplasmosis.
The type of immune response that develops to protozoan infection and the effectiveness of the response depend in part on the location of the parasite within the host. Many protozoans have life-cycle stages in which they are free within the bloodstream, and it is during these stages that humoral antibody is most effective.
Many of these same pathogens are also capable of intracellular growth; during these stages, cell-mediated immune reactions are effective in host defense. In the development of vaccines for protozoan diseases, the branch of the immune system that is most likely to confer protection must be carefully considered.
Malaria (Plasmodium Species) Infects 600 Million People Worldwide Malaria is one of the most devastating diseases in the world today, infecting nearly 10% of the world population and causing 1–2 million deaths every year. There is speculation that some of the symptoms of malaria may be caused not by Plasmodium itself but instead by excessive production of cytokines.
HOST RESPONSE TO PLASMODIUM INFECTION
In regions where malaria is endemic, the immune response to Plasmodium infection is poor. The low immune response to Plasmodium among children can be demonstrated by measuring serum antibody levels to the sporozoite stage. Only 22% of the children living in endemic areas have detectable antibodies to the sporozoite stage, whereas 84% of the adults have such antibodies. Even in adults, the degree of immunity is far from complete, however, and most people living in endemic regions have life long low-level Plasmodium infections.
A number of factors may contribute to the low levels of immune responsiveness to Plasmodium. The maturational changes from sporozoite to merozoite to gametocyte allow the organism to keep changing its surface molecules, resulting in continual changes in the antigens seen by the immune system. The intracellular phases of the life cycle in liver cells and erythrocytes also reduce the degree of immune activation generated by the pathogen and allow the organism to multiply while it is shielded from attack.
DESIGN OF MALARIA VACCINES
An effective vaccine for malaria should maximize the most effective immune defense mechanisms. Unfortunately, little is known of the roles that humoral and cell-mediated responses play in the development of protective immunity to this disease.
African Sleeping Sickness
(Trypanosoma Species)
Two species of African trypanosomes, causing meningoencephalitis and eventually the loss of consciousness. As parasite numbers increase after infection, an effective humoral antibody response develops to the glycoprotein coat, called variant surface glycoprotein (VSG), that covers
the trypanosomal surface These antibodies eliminate most of the parasites from the bloodstream, both by complement-mediated lysis and by opsonization and Millions of trypanosomes per milliliter of blood subsequent phagocytosis. However, about 1% of the organisms, which bear an antigenically different VSG, escape the initial antibody response. These surviving organisms now begin to proliferate in the bloodstream, and a new wave of parasitemia is observed. The successive waves of parasitemia reflect a unique mechanism of antigenic shift by which the trypanosomes can evade the immune response
Leishmaniasis
Is a Useful Model for Demonstrating Differences in Host Responses
The protozoan parasite Leishmania major provides a powerful and illustrative example of how host responses can differ between individuals. These differences can lead to either clearance of the parasite or fatality from the infection. Leishmania is a protozoan that lives in the phagosomes of macrophages. Resistance to the infection correlates well with the production of IFN-gamma_ and the development of a TH1 response.
Elegant studies in mice have demonstrated that strains that are resistant to Leishmania develop a TH1 response and produce IFN-gamma_ upon infection. Such strains of mice become highly susceptible to Leishmania-induced fatality if they lose either IFN-¥gamma_ or the IFN-¥_ receptor, These mice mount a TH2-type response to Leishmania infection; they produce high levels of IL-4 and essentially no IFN-¥_. Thus, one difference between an effective and an ineffective defense against the parasite is the development of a TH1 response or a TH2 response.
Diseases Caused by Parasitic Worms (Helminths)
Unlike protozoan, which are unicellular and often grow within human cells, helminthes are large, multicellular organisms that reside in humans but do not ordinarily multiply there and are not intracellular pathogens. Although helminthes are more accessible to the immune system than protozoans, most infected individuals carry few of these parasites; for this reason, the immune system is not strongly engaged and the level of immunity generated to helminths is often very poor. Parasitic worms are responsible for a wide variety of diseases in both humans and animals. More than a billion people are infected with Ascaris, a parasitic roundworm that infects the small intestine, and more than 300 million people are infected with Schistosoma, a trematode worm that causes a chronic debilitating infection. Several helminths are important pathogens of domestic animals and invade humans ingest contaminated food. These helminths include Taenia, a tapeworm of cattle and pigs, and Trichinella, the roundworm of pigs that causes trichinosis.
Several Schistosoma species are responsible for the chronic, debilitating, and sometimes fatal disease schistosomiasis(formerly known as bilharzia). Three species, are the major pathogens in humans, infecting individuals in Africa, the Middle East, South America, the Caribbean, China, Southeast Asia. A rise in the incidence of schistosomiasis in recent years has paralleled the increasing worldwide use of irrigation, which has expanded the habitat of the freshwater snail that serves as the intermediate host for schistosomes. The worms survive for up to 20 years. The schistosomules would appear to be the forms most susceptible to attack, but because they are motile, they can evade the localized cellular buildup of immune and inflammatory cells. Adult schistosome worms also have several unique mechanisms that protect them from immune defenses. The adult worm has been shown to decrease the expression of antigens on its outer membrane and also to enclose itself in a glycolipid and glycoprotein coat derived from the host, masking the presence of its own antigens. Among the antigens observed on the adult worm are the host’s own ABO blood-group antigens and histocompatibility antigens! The immune response is, of course, diminished by this covering made of the host’s self-antigens, which must contribute to the lifelong persistence of these organisms. The relative importance of the humoral and cell mediated
responses in protective immunity to schistosomiasis is controversial. These manifestations suggest that cytokines produced by a TH2-like subset are important for the immune response: IL-4, which induces B cells to class-switch to IgE production; IL-5, which induces bone-marrow precursors to differentiate into eosinophils; and IL-3, which (along with IL-4) stimulates growth of mast cells. Degranulation of mast cells releases mediators that increase the infiltration of such inflammatory cells as macrophages and eosinophils. The eosinophils express Fc receptors for IgE and IgG and bind to the antibody-coated parasite. Once bound to the parasite, an eosinophil can participate in antibody-dependent cell-mediated cytotoxicity (ADCC), releasing mediators from its granules that damage the parasite . One eosinophils mediator, called basic protein, is particularly
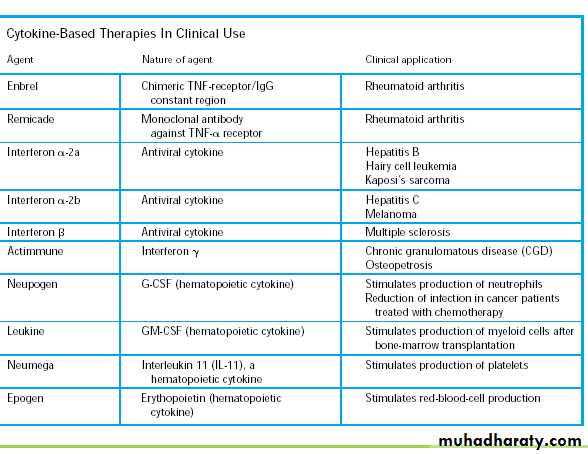
toxic to helminthes.الجدول الأخير للاطلاع فقط
THE ROLE OF CYTOKINE IN HEALTH OR DISEASES
ا م د وفاق مجمود الوتار Lec.3Cytokines are low-molecular-weight proteins that are produced and secreted by a variety of cell types. Cytokines bind to specific receptors on the membrane of target cells, triggering signal-transduction pathways that ultimately alter gene expression in the target cells The susceptibility of the target cell to a particular cytokine is determined by the presence of specific membrane receptors.
Cytokine Receptors Fall Within Five Families almost all belong to one of five families of receptor
1_ Immunoglobulin superfamily receptors
2_ Class I cytokine receptor family (also known as the
hematopoietin receptor family)
3_ Class II cytokine receptor family (also known as the
interferon receptor family)
4_ TNF receptor family
5_ Chemokine receptor family
Another feature common to most of the hematopoietin(class I cytokine) and the class II cytokine receptor families is
exaples for receptor family lignads
(a) Immunoglobulin superfamily receptors as IL-1&M-CSF
(b) Class I cytokine receptors(hematopoietin)
IL-2, IL-3, IL-4, IL-5, IL-6 ,IL-7, IL-9, IL-11 ,IL-12 ,GM-CSF
(c) Class II cytokine receptors (interferon)
IFN-α ,IFN-β, IFN-γ ,IL-10.
(d) TNF receptors TNF-α,TNF-β,CD40 ,Nerve growth factor
(e) Chemokine receptors IL-8 ,MCAF
Cytokine-Related Diseases
Defects in the complex regulatory networks governing the expression of cytokines and cytokine receptors have been implicated in a number of diseases. This section describes several diseases resulting from overexpression or underexpression of cytokines or cytokine receptors.Bacterial Septic Shock Is Common and Potentially Lethal The role of cytokine overproduction in pathogenesis can be illustrated by bacterial septic shock. This condition may develop a few hours after infection by certain gram-negative bacteria, including E. coli,Klebsiella pneumoniae, Pseudomonasaeruginosa, Enterobacter aerogenes, and Neisseria meningitidis.The symptoms of bacterial septic shock, which is often fatal, include a drop in blood pressure, fever, diarrhea, and widespread blood clotting in various organs. Bacterial septic shock apparently develops because bacterial cell-wall endotoxins stimulate macrophages to IL-1 and TNF-_ to levels that cause septic shock.
Chagas’ Disease Is Causedby a ParasiteThe protozoan Trypanosoma cruzi is the causative agent ofChagas’ disease, which is characterized by severe immune suppression. The ability of T. cruzi to mediate immune suppression
Cytokine Activity Is Implicated in Lymphoid and Myeloid Cancers
Abnormalities in the production of cytokines or their receptors have been associated with some types of cancer. For example, abnormally high levels of IL-6 are secreted by cardiac myxoma cells (a benign heart tumor),myeloma and cervical and bladder cancer cells. In myeloma cells, IL-6 appears to operate in an autocrine manner to stimulate cell proliferation.
Therapeutic Uses of Cytokines and Their Receptors
The availability of purified cloned cytokines and soluble cytokine receptors offers the prospect of specific clinical therapies to modulate the immune response. A few cytokines notably, interferons and colonystimulating factors, such as GM-CSF, have proven to be therapeutically useful. the promise of cytokines for clinical medicine is great and efforts to develop safe and effective cytokine-related strategies continue, particularly in areas such as-:1- inflammation as chronic inflamatory disease as rheumatiod arithritis,
2-cancer therapy as leukemia, lymphoma.
3- modification of the immune response during organ transplantation.
4-infectious disease,
5- allergy
6-treatment of immunodificiency.