WHO Histologic Classification of CNS tumors
• Embryonal tumors• Tumors of cranial/spinal nerves
• Mesenchymal tumors, benign
• Mesenchymal tumors, malignant
• Uncertain histogenesis
• Hemopoietic neoplasms
• Cysts/tumorlike lesions
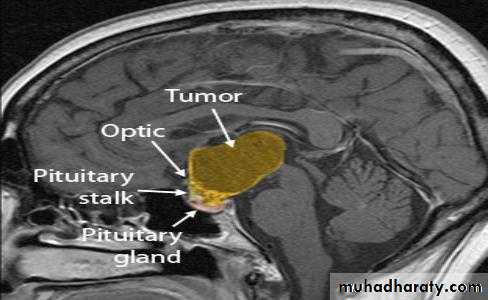
• Sellar tumors
• Neuroepithelial Tumors
• Astrocytic tumors
• Oligodemdroglial tumors
• Ependymal tumors
• Mixed gliomas
• Choroid plexus tumors
• Neurologic tumors
• Pineal parenchymal tumors
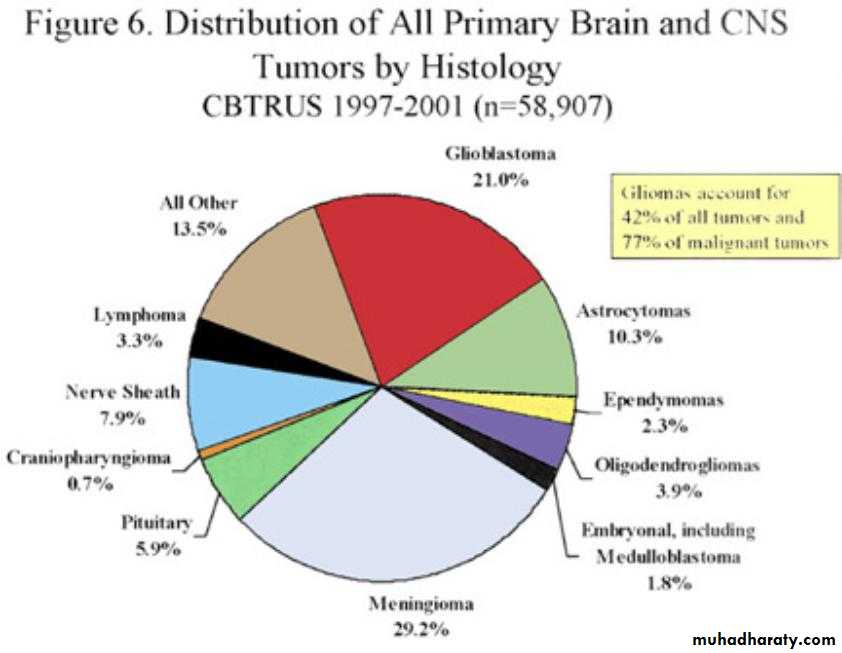
Incidence of primary brain tumors
(benign or malignant) 12.8/100,00010%–15% of cancer patients develop
brain metastases
Primary – unknown
Genetic – hereditaryMetastatic
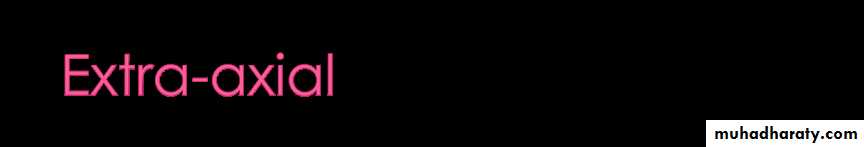
• 35% - lung
• 20% - breast
• 10% - kidney
• 5% - gastrointestinal tract
Often unknown
Under investigation:• Genetic changes
• Heredity
• Errors in fetal development
• Ionizing radiation
• Electromagnetic fields (including cellular phones)
• Environmental hazards (including diet)
• Viruses
• Injury or immunosuppression
Tissue of origin
LocationPrimary or secondary (metastatic)
Grading
Depends on location, size, and type of tumor
Neurological deficit 68%• 45% motor weakness
• Mental status changes
HA 54%
Seizures 26%
General
• Cerebral edema• Increased intracranial pressure
• Focal neurologic deficits
• Obstruction of flow of CSF
• Pituitary dysfunction
• Papilledema (if swelling around optic disk)
Cerebral Tumors
• Headache• Vomiting unrelated to food intake
• Changes in visual fields and acuity
• Hemiparesis or hemiplegia
• Hypokinesia
• Decreased tactile discrimination
• Seizures
• Changes in personality or behavior
Brainstem tumors
• Hearing loss (acoustic neuroma)• Facial pain and weakness
• Dysphagia, decreased gag reflex
• Nystagmus
• Hoarseness
• Ataxia (loss of muscle coordination) and dysarthria (speech muscle disorder) (cerebellar tumors)
Cerebellar tumors
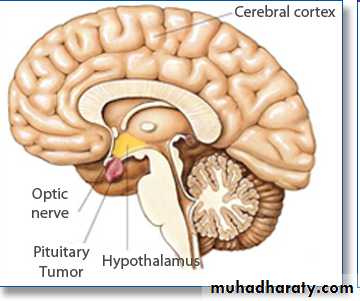
• Disturbances in coordination and equilibriumPituitary tumors
• Endocrine
• dysfunction
• Visual deficits
• Headache
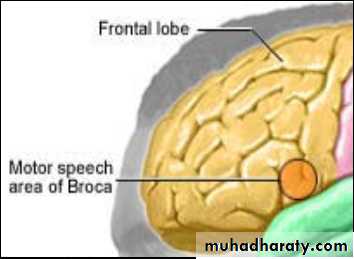
Frontal Lobe
• Inappropriate behavior• Personality changes
• Inability to concentrate
• Impaired judgment
• Memory loss
• Headache
• Expressive aphasia
• Motor dysfunctions
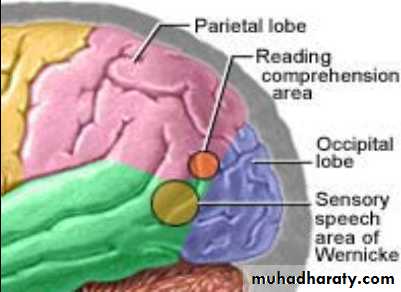
Parietal lobe
• Sensory deficits• Paresthesia
• Loss of 2 pt discrimination
• Visual field deficits
Temporal lobe
• Psychomotor seizures – temporal lobe-judgment, behavior, hallucinations, visceral symptoms, no convulsions, but loss of consciousness
Occipital lobe
• Visual disturbances
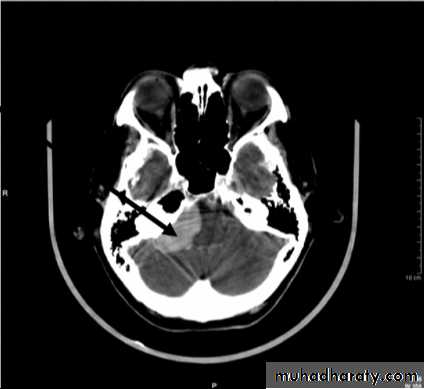
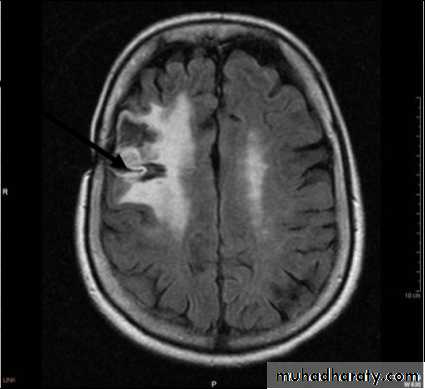
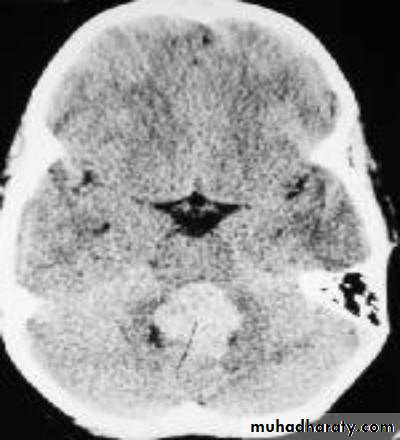
• CLASSIFICATION OF CNS TUMOURS
• Intrinsic tumours – account for virtually all tumours in children and 60% of primary CNS tumours in adults• Extrinsic tumours – arising from cranial and spinal nerves and dura.
• Tumours arising from adjacent structures i.e pituitary gland and metastatic tumours.
Gliomas
• Astrocytoma (Grades I & II)• Anaplastic Astrocytoma
• Glioblastoma Multiforme
Oligodendroglioma
Ependymomas
Medulloblastoma
CNS Lymphoma
Grade I
Non-infiltrating• Grade II
• Infiltrating• Slow growing
Grade III
InfiltratingAggressive
Grade IV
Highly infiltrativeRapidly growing
Areas of necrosis
• Grades II-IV
• Mixed astro/glio• Slow growing
• Benign• HCP/ICP
• Surgery, RT, Chemo
• Small cell embryonal neoplasms
• Malignant• HCP/ICP
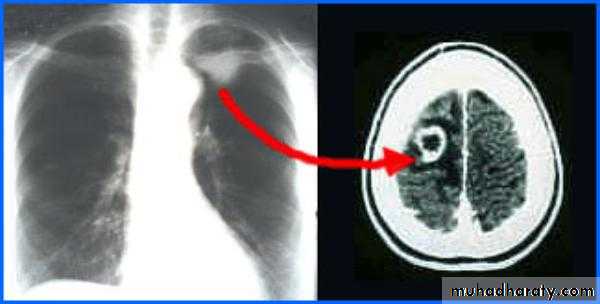
Primary CNS lymphoma
B lymphocytesIncreased ICP
Brain destruction
Meningioma
MetastaticAcoustic neuromas (Schwannoma)
Pituitary adenoma
Neurofibroma
Usually benign
Slow growing
Well circumscribed
Easily excisable
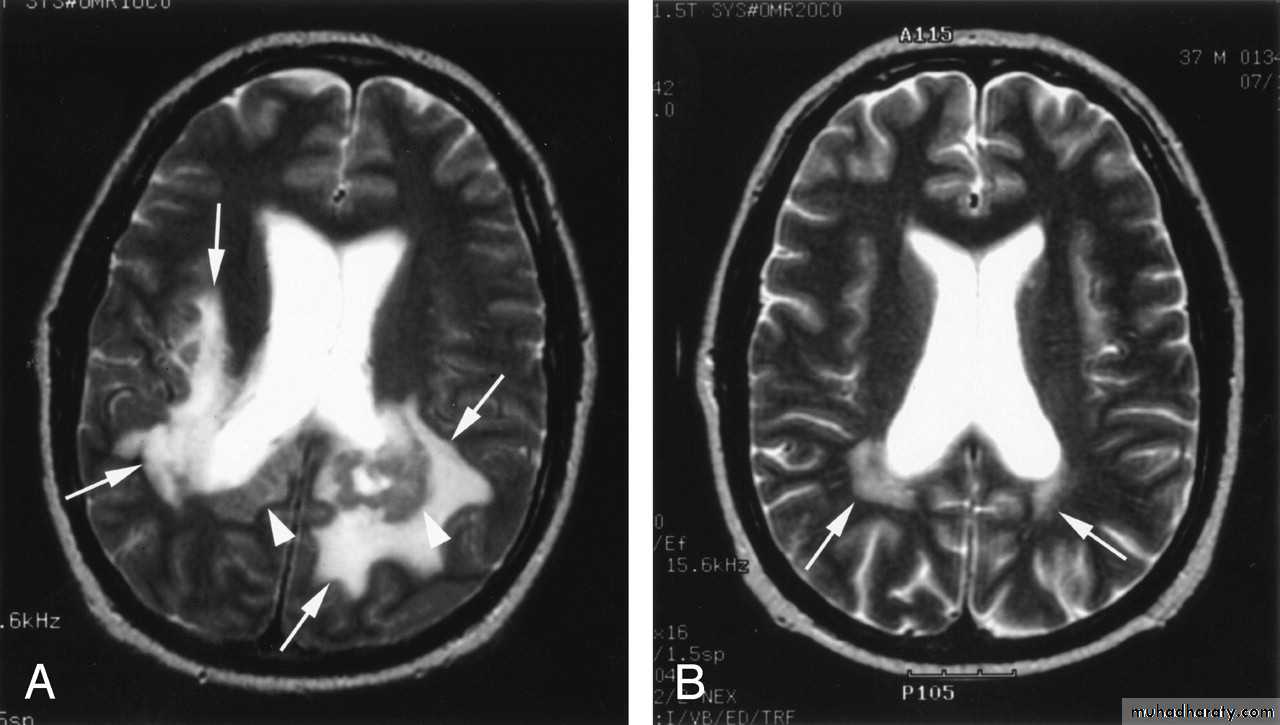
• Peritumoral edema
• Necrotic centerBenign
Schwannoma cellsCN VIII
Benign
Anterior pituitaryEndocrine dysfxn
Cystic tumor
Hypothalamic-pituitary axis dysfunctionRadiological Imaging
• Computed Tomography scan (CT scan) with/without contrast• Magnetic Resonance Imaging (MRI) with/without contrast
• Plain films
• Myelography
• Positron Emission Tomography scan (PET scan)
LP/CSF analysis
Pathology
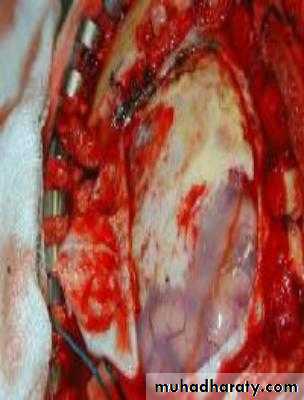
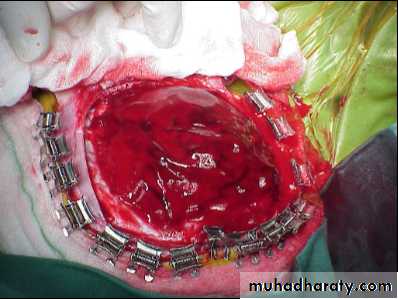
• Resection
• Craniotomy• Stereotaxis Surgery
• Biopsy
• Transsphenoidal
http://youtu.be/d95K3unaNCs
Drug therapy – Palliative
• Done for symptom treatment and to prevent complications• NSAIDs
• Analgesics – Vicodin, Lortab, MS Contin
• Steroids (Decadron, medrols, prednisone)
• Anti-seizure medications (phenytoin) Dilantin & Cerebyx
• Histamine blockers
• Anti-emetics
• Muscle relaxers (for spasms)
• Mannitol for ICP –New Hypertonic saline
Damages DNA of rapidly dividing cells
4000–6000 Gy total doseDuration of 4–8 weeks
Brachytherapy
Stereotactic radiosurgery
Roles of Radiotherapy in Brain Tumor
Incomplete surgeryDeep seated tumor: midbrain, pons
Radiosensitive tumor: medulloblastoma
Pituitary adenoma
Palliation: metastatic lesions
Slows cell growth
Cytotoxic drugs• CCNU, BCNU, PCV, Cisplatin, Etoposide, Vincristine, Temozolomide (Temodar)
Gliadel wafers
Ommaya Reservoir
Ineffective Tissue Perfusion
Ineffective Airway ClearanceImpaired Communication
Decreased Intracranial Adaptive Capacity
Activity Intolerance
Disturbed Sensory disturbance
Acute Confusion
A patient is being directly admitted to the medical-surgical unit for evaluation of a brain mass seen in the frontal lobe on a diagnostic CT scan. Which of the following signs and symptoms would the patient most likely present with?
• Personality changes
• Visual field cuts
• Difficulty hearing
• Difficulty swallowing
The nurse is evaluating the status of a client who had a craniotomy 3 days ago. The nurse would suspect the client is developing meningitis as a complication of surgery if the client exhibits
a. A positive Brudzinski’s sign
b. A negative Kernig’s sign
c. Absence of nuchal rigidity
d. A Glascow Coma Scale score of 15
AANN Core Curriculum for Neuroscience Louis, MO. Nursing, 4th Ed. 2004. Saunders. St.
Greenberg, Mark. (2006). Handbook of• Neurosurgery. Greenberg Graphics,
• Tampa, Florida.