Hussien Mohammed Jumaah
CABMLecturer in internal medicine
Mosul College of Medicine
Thursday, 24 march, 2016
Glomerular diseases
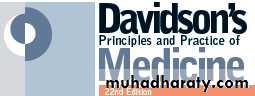
(Glomerulonephritis (GN))Bowman capsule (glomerular capsule)
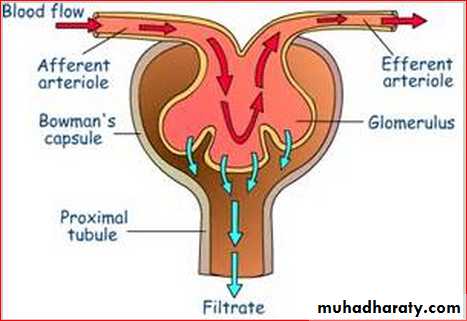
Cells of the glomerulus and targets of immunity and
autoimmunity.Antigen–antibody complexes are described according to their site of deposition: subepithelial , between podocyte and GBM; intramembranous, within the GBM; subendothelial,
between endothelial cell and GBM; and mesangial, within the mesangial matrix.
Glomerulonephritis (GN)
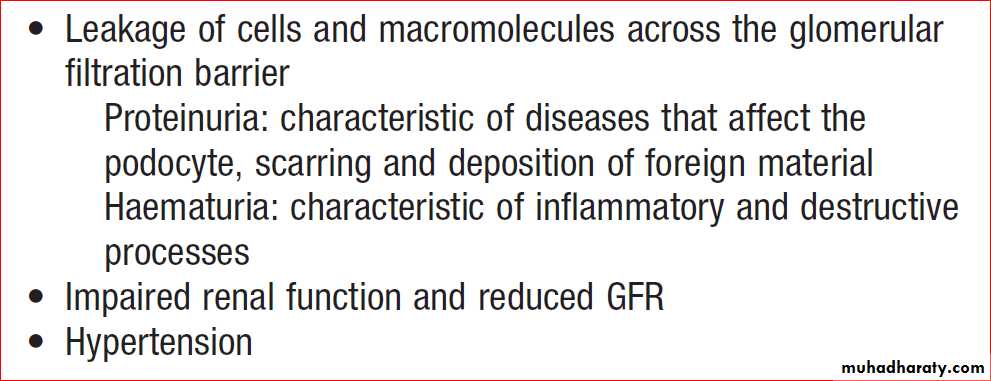
Glomerular diseases account for a significant proportion of acute and chronic kidney disease.There are many causes of glomerular damage, including immunological injury, inherited diseases such as Alport’s syndrome , metabolic diseases such as diabetes mellitus , and deposition of abnormal proteins such as amyloid in the glomeruli.
Most patients with glomerular disease are asymptomatic until abnormalities are detected on routine screening of blood or urine samples.
Clinical and laboratory features of
glomerular injuryGN
GN means ‘inflammation of glomeruli’. The term is used to describe all types, even though some (as minimal change) not associated with inflammation.
Most types are immunologically mediated and several respond to immunosuppressive drugs.
GN classified in terms of the histopathological appearances.
Minimal change, Focal segmental glomerulosclerosis (FSGS), Membranous, IgA nephropathy, Mesangiocapillary, Post-infection, Goodpasture’s disease
and Lupus nephritis (any histological type).
GN (continued)
Although deposition of circulating immune complexes was previously thought to be a common mechanism, it now seems that most granular deposits of immunoglobulin are formed ‘in situ’ by antibodies which complex with glomerular antigens, or with other extraneous antigens derived from viruses and bacteria that have become deposited in the glomeruli .Minimal change nephropathy
Occurs at all ages but accounts for nephrotic syndrome in most children and about one-quarter of adults. It is caused by reversible dysfunction of podocytes. The presentation is with proteinuria or nephrotic syndrome, typically remits with high-dose corticosteroid(CS) therapy (1 mg/kg prednisolone for 6 weeks).Some patients who respond incompletely or relapse ,frequently need maintenance CS, cytotoxic. Minimal change disease does not progress to CKD but can present with problems related to the nephrotic syndrome and complications of treatment.
Focal segmental glomerulosclerosis (FSGS)
Primary FSGS can occur in all age groups.In some patients, can have specific causes, such as HIV infection, podocyte toxins and massive obesity, but in most cases the underlying cause is unknown .
Patients with primary FSGS present with
massive proteinuria and idiopathic nephrotic syndrome. Histological analysis shows sclerosis affecting segments of the glomeruli, which may also show positive staining for
deposits of C3 and IgM on immunofluorescence.
FSGS (continued)
Since FSGS is a focal process, abnormal glomeruli may not be seen on renal biopsy if only a few are sampled, leading to an initial diagnosis of minimal change nephropathy.It can respond to high-dose CS (0.5–2.0 mg/kg/day)
but most patients show little or no response. Immunosuppressive drugs, such as ciclosporin, cyclophosphamide and mycophenolate mofetil, have been used but their efficacy is uncertain.
Progression to CKD is common and the disease frequently recurs after renal transplantation.
Membranous glomerulonephritis
Membranous GN , also known as membranous nephropathy, is the most common cause of nephrotic syndrome in adults.It is caused by antibodies (autoantibodies) directed at antigen(s) expressed on the surface of podocytes.
A proportion of cases are associated with other
causes, such as
heavy metal poisoning, drugs, infections and tumours but most are idiopathic.
Membranous GN (continued)
Approximately one-third of patients with idiopathic membranous GN undergo spontaneous remission; one-third remain in a nephrotic state, and one-third go on to develop CKD.Short-term treatment with high doses of CS and cyclophosphamide may improve both the nephrotic syndrome and the long-term prognosis.
However, because of the toxicity of these regimens, many nephrologists reserve such treatment for those with severe nephrotic syndrome or deteriorating renal function.
IgA nephropathy
This is one of the most common types of GN and can present in many ways . Haematuria is the earliest sign and is almost universal, and hypertension is also very common.Proteinuria can also occur but is usually a later feature. In many cases, there is slowly progressive loss of renal function leading to ESRD.
A particular hallmark of IgA nephropathy in
young adults is the occurrence of acute self-limiting
exacerbations, often with gross haematuria, in association with minor respiratory infections.
IgA nephropathy (continued)
It may be so acute as to resemble acute post-infectious glomerulonephritis, with fluid retention, hypertension and oliguria with dark or red urine.Characteristically, the latency from clinical infection to nephritis is short , a few days or less.
Management
directed towards the control of blood pressure in an attempt to prevent or retard progressive renal disease. There is some evidence for additional benefit from several months of high-dose CS in high-risk disease, but the response to immunosuppressive is usually poor.
Henoch–Schِnlein purpura
Most commonly occurs in children,can also be observed in adults. It is characterised by a systemic vasculitis that often arises in response to an infectious trigger. The presentation is with a characteristic petechial rash affecting buttocks and lower legs, and abdominal pain due to the occurrence of vasculitis involving the gastrointestinal tract. The presence of GN is usually indicated by the occurrence of haematuria.HenochSchِnlein purpura (continued)
When Henoch– Schِnlein purpura occurs in older children or adults, the glomerulonephritis is usually more prominent and less likely to resolve completely.Renal biopsy shows mesangial IgA deposition and appearances that are indistinguishable from acute IgA nephropathy.
Treatment is supportive in nature; in most, the prognosis is good, with spontaneous resolution, but some, particularly adults, progress to ESRD.
Mesangiocapillary glomerulonephritis (MCGN),
Also known as membranoproliferative (MPGN), is characterised by an increase in mesangialcellularity with thickening of glomerular capillary walls and subendothelial deposition of immune complexes and/or components of the complement pathway.
The typical presentation is with
proteinuria and haematuria.
MCGN classified into two main subtypes
The first is characterised by deposition of immunoglobulins within the glomeruli, (associated with chronic infections, autoimmune diseases and monoclonal gammopathy).The second is characterized by deposition of complement in the glomeruli, called ‘dense deposit disease’,
(deposition of electron-dense deposits within the GBM).
Treatment
MCGN associated with immunoglobulins deposits consists of identifying and treating the underlying disease, if possible, and the use of immunosuppressive mycophenolate mofetil or cyclophosphamide.
There is no specific treatment for dense deposit disease.
Infection-related glomerulonephritis
Occur in connection with infections of various types, including subacute bacterial endocarditis, hepatitis B, C, schistosomiasis, leishmaniasis, malaria, HIV .The most common histological pattern in bacterial infection is mesangiocapillary GN,
often associated with extensive immunoglobulin
deposition in the glomeruli with evidence of
complement consumption (low serum C3).
Post-streptococcal glomerulonephritis
It is much more common in children than adults. Thelatency is usually about 10 days after a throat infection or longer after skin infection, suggesting an immune mechanism.
Sodium retention, hypertension and oedema are particularly pronounced.
There is also reduction of GFR, proteinuria, haematuria and oliguria with a red or smoky urine appearance.
Post-streptococcal glomerulonephritis (continued)
As in other causes of post-infectious GN, serum concentrations of C3 and C4 are typically reduced, reflecting complement consumption ,and evidence of streptococcal infection may be found.Renal function begins to improve spontaneously within 10–14 days, and management by fluid and sodium restriction with diuretic and hypotensive agents is usually adequate.
Remarkably, the renal lesion in almost all children and many adults seems to resolve completely.
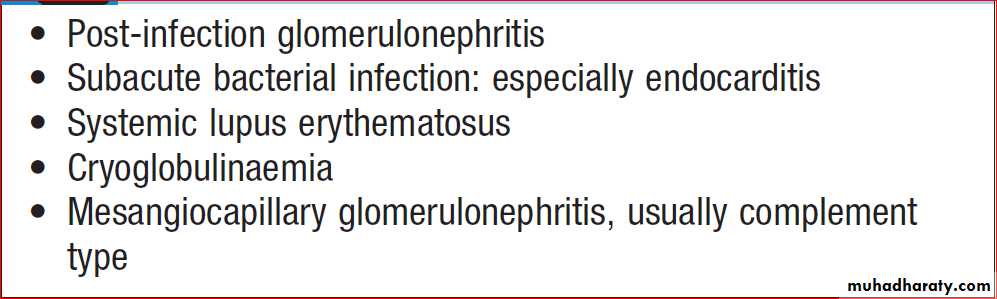
Causes of glomerulonephritis associated
with low serum complementRapidly progressive glomerulonephritis
(Crescentic GN) , characterised by rapid loss of renal function over days to weeks.Renal biopsy shows crescentic lesions, and necrotising lesions within the glomerulus, termed focal segmental (necrotising) GN. It is typically seen in Goodpasture’s disease, (anti-GBM antibodies), small-vessel vasculitides . SLE and IgA GN
Management
Immunosuppressive drugs are often required. Anti-GBM disease should be treated with plasma exchange combined with corticosteroids and immunosuppressants.